Abstract
Background
While the fear of falling is a common psychological consequence of falling, older adults who have not fallen also frequently report this fear. Fear of falling can lead to activity restriction that is self-imposed rather than due to actual physical impairments. Evidence suggests that exercise can significantly improve balance confidence, as measured by falls-related self-efficacy scales. However, there are no prospective reports that correlate change in balance confidence with changes in fall risk and physical abilities as induced by participating in a group-based exercise program.
Objective
The primary purpose of this prospective study was to examine the relationship between the change in balance confidence and the changes in fall risk and physical abilities in older women with confirmed low bone mass after 13 weeks of exercise participation. The secondary purpose of this study was to examine the relationship between the change in balance confidence and the change in physical activity level.
Methods
The sample comprised 98 women aged 75 to 85 years old women with low bone mass. Participants were randomly assigned to one of three groups: Resistance Training (n=32), Agility Training (n=34), and Stretching (sham) exercises (n=32). The 50-minute exercise classes for each study arm were held twice weekly at a local YMCA community centre.
Results
Both resistance training and agility training significantly improved balance confidence by 6% from baseline after 13 weeks. However, the change in balance confidence was only weakly correlated with improved general physical function and not significantly correlated with the changes in fall risk score, postural stability, gait speed, or physical activity level. As well, we observed balance confidence enhancement in the presence of increased fall risk or deterioration in physical abilities.
Conclusions
Two different types of exercise training improved balance confidence in older women with low bone mass. This change in balance confidence was significantly correlated with change in general physical function. Because of the observation of discordance between balance confidence change and changes in fall risk and physical abilities, those who design group-based exercise programs for community-dwelling older adults may wish to consider including an education component on factors that influence fear of falling. Objective changes in fall risk factors cannot be assumed to mirror change of fear of falling and physical abilities in older adults in the short-term.
Keywords: Balance confidence, fall risk, exercise, older women, low bone mass
INTRODUCTION
Falls are a relatively common event in older adults. Approximately 30% of individuals over 65 years of age fall at least once a year, and about half of those do so recurrently. Fall-related injuries and death in older people are a major health care problem worldwide, with the numbers continuing to rise [1].
While the fear of falling is a common psychological consequence of falling, older adults who have not fallen also frequently report this fear. Prevalence rates of fear of falling vary, but average prevalence in older adults who do not have a history of falling is 30% or more and it is double that in those older adults who have fallen [2, 3]. The prevalence of fear of falling is higher among women than men [4–6]. Fear of falling can lead to activity restriction that is self-imposed rather than due to actual physical impairments [5]. Thus, fear of falling is an independent contributor of functional decline and consequently, the loss of independence, among older adults [7].
Fear of falling has been associated with poor performance on tests of balance, including increased spontaneous sway and decreased one-leg stance time [4], reduced gait speed [8], reduced independence, poor quality of life, poor health [7], and depressed mood [6]. Fear of falling has also been identified as an independent predictor of falls in community dwelling older adults in a 20-month, population based, prospective study [9].
Considering that there is a strong association between fear of falling and physical function [3, 8], it appears that interventions, such as fall prevention programs, should attempt to simultaneously improve physical function and balance confidence. There is evidence that exercise can significantly reduce the fear of falling [10–13]. We hypothesize that participating in a group-based exercise program has the potential to augment low balance confidence (i.e. reduce fear of falling) by improving quality of life, increasing social interaction with peers, reducing anxiety and physical frailty. It is important that any enhancement of balance confidence is accompanied by an appropriate change or improvement in physical abilities. However, to our knowledge, there are no prospective reports that correlate change in balance confidence, as assessed by a falls-related self-efficacy scale, with change in physical abilities as induced by participating in a group-based exercise program. Furthermore, very little data exists on balance confidence in older people with low bone mass. As individuals with low bone mass are susceptible to sustaining fall-related fractures, their balance confidence may not be as amendable as previously reported in other populations [10, 11].
Thus, the primary purpose of this prospective study was to examine the relationship between the change in balance confidence, as measured by the Activities-Specific Balance Confidence (ABC) Scale, and the changes in fall risk and physical abilities in older women with confirmed low bone mass after 13 weeks of exercise participation. As physical activity curtailment is a common consequence of fear of falling, the secondary purpose of this study was to examine the relationship between the change in balance confidence and the change in physical activity level.
METHODS
Participants
The sample comprised 98 women aged 75 to 85 years when recruited (mean age=79, SD=3) who participated in our randomized, controlled prospective study that examined the effects of three different types of group-based exercise programs (resistance training, agility training, and general stretching) on fall risk [14] and bone health. These women were residents of greater Vancouver and in whom osteoporosis or osteopenia had been diagnosed by dual-energy x-ray densitometry (defined as a T-score at the total hip or spine at least 1.0 standard deviations below the young normal sex-matched areal bone mineral density of the Lunar reference database) [15]. Six hundred and eighty-three letters of recruitment were mailed to the women identified from various databases. Local newspaper, radio, and poster advertisements were also used to aid in recruitment.
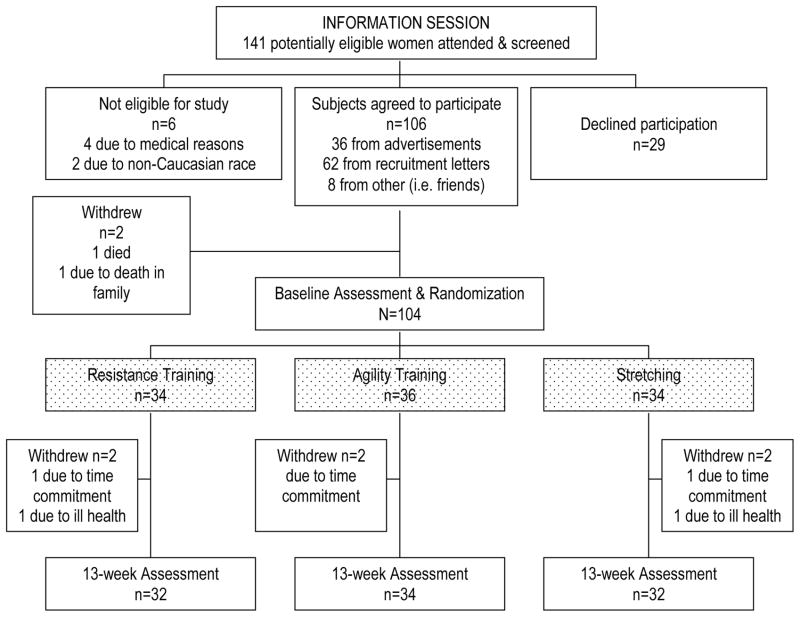
Interested individuals were screened by a standardized telephone interview, which included the revised physical activity readiness (Par-Q) questionnaire [16, 17], and were then invited to an information session where a physician (KMK) further screened all potential participants. We excluded women who were: living in care facilities, of non-Caucasian race, regularly exercising twice weekly or more, had a history of illness or a condition for which exercise may cause adverse effects, had a history of illness or a condition that would affect balance (i.e. stroke and Parkinson’s disease), or had a Mini Mental State Examination (MMSE) [18] score of ≤ 23. After baseline measurement, all participants were randomly assigned to one of three groups: Resistance Training, Agility Training, and Stretching. Randomization was stratified by baseline postural stability (total sway path in mm). Figure 1 describes the number of participants in each study arm.
Figure 1.
Flow chart outlining number of participants in each study arm.
The study was approved by the University of British Columbia Clinical Research Ethics Board and the Research Committee of the Children’s and Women’s Hospital of British Columbia. All participants gave written informed consent prior to participating in the study.
Descriptive Variables
We measured age in years, standing height in centimetres, and mass in kilograms in all participants. Cognitive state was assessed using the 30 point Mini-Mental State Examination (MMSE) [18]. Whether a participant required a walking aid was also recorded.
General health was assessed by a subset of questions from the Canadian Multicentre Osteoporosis Study (CaMOS) questionnaire [19] that relate to current medication use, the presence of associated medical conditions known to be fall risk factors (such as osteoarthritis), and fall history (in the last 4 weeks). This questionnaire was administered at baseline by trained interviewers. All participants underwent a physician review of medical history and physical examination after completing the screening questionnaire.
Outcome Measures
The outcome measures were assessed at baseline and after 13 weeks of study participation.
Fall Risk Assessment
Each participant’s fall risk was assessed by Lord’s Physiological Profile Assessment (PPA) © [20] (Prince of Wales Medical Research Institute, Randwick, Sydney, NSW, Australia). The PPA is a valid [21, 22] and reliable [23] tool for assessing fall risk in older people. Based on the performance of five key physiological tasks, the PPA computes a fall risk score (z score; standardized score) for each individual and this score has a 75% predictive accuracy for falls in older people [21, 22]. The five key components of the PPA are: postural stability, dominant quadriceps strength, dominant hand reaction time, joint position sense, and edge contrast sensitivity. The assessment methods for these components of PPA have been previously described by Lord and coworkers [20–22].
Posture Stability
Postural stability was assessed by the method described by Lord and coworkers [20]. Individuals were asked to stand as still as possible for 30 seconds on medium-density foam with their eyes open. As participants attempt to stand as still as possible for 30 seconds, total sway path in millimetres (mm) was determined from the path traced by the Lord swaymeter [22].
Gait Speed
As decreased gait speed is a significant and independent predictor of fall [22]and fracture risk in older women [24], participants were asked to walk without shoes and without the use of walking aids along an 8-meter path, first at a self-selected speed and then at a fast-paced but safe speed [25]. The test-retest reliability of gait speed in our laboratory is 0.95 (ICC). Gait speed was calculated from the mean of three trials. The cumulative distance and time of consecutive strides (i.e. from foot contact with one leg to the next foot contact with the same leg) were recorded by infrared-emitting diodes (Northern Digital) attached to the foot during the middle section (i.e. approximately a 4-meter section, representative of constant gait speed) of the 8-meter walkway.
General Physical Function
General physical function was assessed using the Howe et al.’s [26] Community Balance and Mobility Scale. This scale is a performance-based balance and mobility measure consisting of 13 items each rated at a 5-point scale (maximum of 85 points). It includes items such as timed single leg stand, tandem walking, and stair mobility. This novel scale was chosen because present balance and mobility measures do not adequately assess high-level function [27, 28]. Initial test-retest reliability for the Community Balance Mobility Scale indicates a high agreement between tests with an ICC of 0.975. The internal consistency of the scale is also very high (Cronbach’s alpha=0.96) [26].
Balance Confidence
The 16-item Activities-specific Balance Confidence Scale [29] assessed balance confidence, with each item rated from 0% (no confidence) to 100% (complete confidence). The maximum score achievable is 1600, which is then averaged over the 16 items to provide a score out of 100. This scale has a two-week test-retest reliability of ICC=0.92 and internal consistency Cronbach’s alpha of 0.96. The ABC score is correlated with other measures of self-efficacy, distinguishes between individuals of low and high mobility, and corresponds with balance performance measures [8, 10].
Physical Activity Level
Each participant’s current level of physical activity was determined by the Physical Activities Scale for the Elderly (PASE) questionnaire[30, 31]. The PASE questionnaire is valid and reliable for older adults [30, 31]. Its score is significantly associated with physiologic and performance characteristics [31].
Exercise Intervention
The exercise intervention began one week after baseline measures were completed. Participants were required to attend their assigned exercise class twice weekly. All classes were held at a YMCA community centre and led by certified fitness instructors. The classes were 50 minutes in duration. The head instructor of each class recorded attendance daily. Adherence with the assigned exercise program was recorded for each participant and compliance is expressed as the percentage of the 48 classes (maximum number of classes) attended.
Resistance Training
The protocol for the Resistance Training group was progressive and high-intensity in nature with the aims of increasing muscle strength in the extremities and trunk. Both a Keiser® Pressurized Air system (Keiser Corporation, Fresno, CA, USA) and free weights were used to provide the training stimulus. Participants were given a 2-week period for familiarisation with the equipment and the exercises. The Resistance Training exercises included: biceps curls, triceps extension, seated row, latissmus dorsi pull downs, mini-squats, mini-lunges, hamstring curls, calf raises, and gluteus maximus extensions on a mat.
The intensity of the training stimulus was initially set at 50% to 60% of 1RM (repetition maximum) as determined at week two, with a work range of two sets of 10–15 repetitions and progressed to 75% to 85% of 1RM at a work range of six to eight repetitions (two sets) by week four. The training stimulus was increased using the 7RM method [32], when two sets of six to eight repetitions were completed with proper form and without pain or discomfort. Squats, lunges, and gluteus maximum extensions, however, did not follow the above guideline. These three exercises were performed initially with body weight and loading was increased only when proper form was maintained for two sets of 10 repetitions. The number of sets completed and the load lifted for each exercise were recorded every class for each participant.
Agility Training
The aims of the Agility Training protocol were to challenge: 1) hand-eye coordination, 2) foot-eye coordination, 3) dynamic balance, 4) static balance and 5) psychomotor performance (reaction time). Ball games, relay races, dance movements, and obstacle courses were used to achieve these goals. A logbook was maintained detailing the content of each week’s classes and is available from the first author (TLA). Due to the potential risk of falls in the Agility Training class, participants were given KPH® (Tampere, Finland) hip protectors and all instructors provided very close supervision and ‘spotting’ as in gymnastics training.
Stretching
The content of the Stretching class consisted of stretching exercises, deep breathing and relaxation techniques, and general posture education. There is no evidence that these exercises reduce fall risk [33]. This group served to control for confounding variables such as physical training received by traveling to the community centre for twice-weekly classes, social interaction and changes in lifestyle secondary to study participation.
Data Analyses
Data were analyzed using SPSS (Windows Version 11.0). Descriptive data are reported for variables of interest (i.e. mean, standard deviation, and range).
Comparisons of group characteristics and baseline scores were undertaken using a Chi Square test for differences in proportions and ANOVA for differences in means. A repeated measures analysis of variance model was constructed to determine the between- and within-group differences in balance confidence after 13 weeks of exercise participation.
We determined the level of association between change in balance confidence and the following variables for the entire cohort (N=98) using the Spearman rank correlation coefficients: change in fall risk score, change in postural stability, change in gait speed, change in general physical function, and change in physical activity level. Change was calculated as the post-intervention value minus the baseline value. The use of the Spearman rank correlation coefficient was warranted, as the distribution of the change scores for balance confidence was not normally distributed. The overall alpha error was set at p≤0.05.
Effect size (ES; delta index) and percent change were also calculated for fall risk score, postural stability, gait speed, general physical function, balance confidence, and physical activity level. Effect size was calculated by subtracting the mean baseline value from the mean post-intervention value and dividing the result by the baseline standard deviation [34]. Percent change was calculated by subtracting the mean baseline value from the mean post-intervention value, dividing by the mean baseline value, and multiplying by 100.
RESULTS
The key results were in the change in balance confidence over time and the correlation between balance confidence and objective measures. The objective measures included fall risk score, postural stability, gait speed, general physical function and physical activity level. Descriptive Variables, Baseline Values, and Compliance
The three groups did not differ in any of the descriptive variables (Table 1). Based on the physician’s findings, the participants had normal neurological and musculoskeletal function. Table 2 provides the baseline values for the outcome measures. In the group as a whole, the adherence to the exercise classes was 83.3%. The Resistance Training group had an average compliance of 85.4%, the Agility Training group 87.3%, and the Stretching group 78.8%.
Table 1.
Descriptive statistics for descriptors (N=98).
| Variable* | Resistance (n=32) | Agility (n=34) | Stretching (n=32) | Entire Cohort (N=98) |
|---|---|---|---|---|
| Mean (SD); Range | Mean (SD); Range | Mean (SD); Range | Mean (SD); Range | |
| Age† (yr) | 79.6 (2.1); 75 to 86 | 78.9 (2.8); 75 to 86 | 79.5 (3.2); 75 to 86 | 79.3 (2.7); 75 to 86 |
| Height (cm) | 160.1 (6.0); 148.0 to 172.0 | 157.0 (6.2); 144.0 to 167.2 | 158.3 (8.4); 139.6 to 178.9 | 158.5 (7.0); 139.6 to 178.9 |
| Weight (kg) | 59.9 (9.4); 47.2 to 83.2 | 62.5 (9.3); 47.2 to 89.2 | 65.2 (12.6); 36.6 to 96.2 | 62.5 (10.77); 36.6 to 96.2 |
| Medications | 2.6 (2.3); 0 to 9 | 3.2 (2.1); 0 to 7 | 4.1 (3.3); 0 to 17 | 3.3 (2.6); 0 to 17 |
| MMSE (max 30 pts) | 28.7 (1.4); 25 to 30 | 28.6 (1.4); 24 to 30 | 28.3 (1.9); 23 to 30 | 28.6 (1.6); 23 to 30 |
| Fall in Last 4 Wks‡ | 5 (15.6) | 1 (2.9) | 2 (6.3) | 8 (8.2) |
| Osteoarthritis‡ | 11 (34.4) | 13 (38.2) | 17 (53.1) | 41 (41.8) |
| Knee | 5 (15.6) | 6 (17.6) | 6 (18.8) | 17 (17.3) |
| Osteoarthritis‡ |
There were no significant differences between the groups for any measure.
Age at baseline measurement. All participants were 75–85 years at recruitment, but several participants turned 86 years between recruitment and baseline measurement.
Count (%). Count=Number of “yes” cases within each group. % =Percent of “yes” cases within each group.
Table 2.
Descriptive statistics for outcome measures at baseline and after 13-weeks of exercise training (N=98).
| Variable | Resistance (n=32) | Agility (n=34) | Stretching (n=32) |
|---|---|---|---|
| Mean (SD); 95% CI | Mean (SD); 95% CI | Mean (SD); 95% CI | |
| Baseline | |||
| Fall Risk Score (SD)* | 2.22 (0.70); 1.94 to 2.52 | 2.40 (0.86); 2.12 to 2.67 | 1.92 (0.83); 1.64 to 2.20 |
| Postural Stability (mm) | 230.1 (93.1); 199.1 to 265.6 | 219.0 (80.3); 187.5 to 250.9 | 217.0 (104.7); 184.3 to 249.7 |
| Gait Speed: Normal (m/s) | 1.02 (0.25); 0.95 to 1.10 | 1.02 (0.19); 0.95 to 1.09 | 0.91 (0.20); 0.83 to 0.98 |
| Gait Speed: Fast (m/s) | 1.47 (0.35); 1.37 to 1.58 | 1.39 (0.26); 1.29 to 1.49 | 1.27 (0.27); 1.17 to 1.37 |
| General Physical Function† | 44.6 (21.6); 37.1 to 50.7 | 39.9 (17.5); 33.4 to 46 4 | 40.4 (18.3); 33.7 to 47.1 |
| Physical Activity Level‡ | 98.0 (51.8); 82.0 to 110.3 | 83.3 (35.1); 69.8 to 96.8 | 76.3 (30.0); 62.4 to 90.2 |
| Balance Confidence§ | 76.3 (22.7); 68.4 to 83.1 | 78.3 (14.5); 71.3 to 85.3 | 75.6 (23.7); 68.3 to 82.8 |
| Final | |||
| Fall Risk Score (SD)* | 1.39 (0.98); 1.07 to 1.76 | 1.49 (0.97); 1.17 to 1.82 | 1.50 (0.95); 1.16 to 1.84 |
| Postural Stability (mm) | 183.6 (123.2); 145.5 to 227.7 | 179.5 (98.1); 140.2 to 218.7 | 196.6 (122.9); 156.2 to 237.0 |
| Gait Speed: Normal (m/s) | 1.11 (0.22); 1.03 to 1.18 | 1.09 (0.19); 1.02 to 1.16 | 1.00 (0.19); 0.92 to 1.07 |
| Gait Speed: Fast (m/s) | 1.52 (0.33); 1.42 to 1.62 | 1.55 (0.27); 1.45 to 1.65 | 1.41 (0.28); 1.31 to 1.52 |
| General Physical Function† | 49.5 (20.7); 42.4 to 55.3 | 51.5 (15.5); 45.3 to 57.7 | 45.8 (17.8); 39.4 to 52.1 |
| Physical Activity Level‡ | 108.7 (44.3); 88.0 to 130.2 | 116.6 (70.2); 96.4 to 136.7 | 115.1 (58.1); 94.4 to 135.8 |
| Balance Confidence§ | 80.9 (17.1); 74.8 to 86.1** | 83.2 (12.2); 77.9 to 88.6** | 76.3 (17.6); 70.7 to 81.8 |
Measured by the Physiological Profile Assessment (PPA) where lower values indicate lower risk of falling.
Measured by the Community Balance and Mobility Scale (CB&M) where higher values indicate better physical function.
Measured by the PASE questionnaire where higher values indicate higher physical activity levels.
Measured by the ABC Scale where higher values indicate lower levels of fear of falling.
p<0.05 compared with baseline value (paired t-test).
Balance Confidence
Baseline balance confidence was not significantly different between the three groups (p=0.855). There was a significant main effect of time (within group effect) for balance confidence after 13 weeks of exercise intervention (p=0.002). Subsequent analysis (paired t-tests) indicated that while both the Resistance Training group and the Agility Training group improved balance confidence after the 13-week intervention period (p≤0.031), the Stretching group did not (p=0.729) (Table 2). Both groups significantly improved balance confidence by 6% from baseline.
Spearman Rank Correlation Coefficients
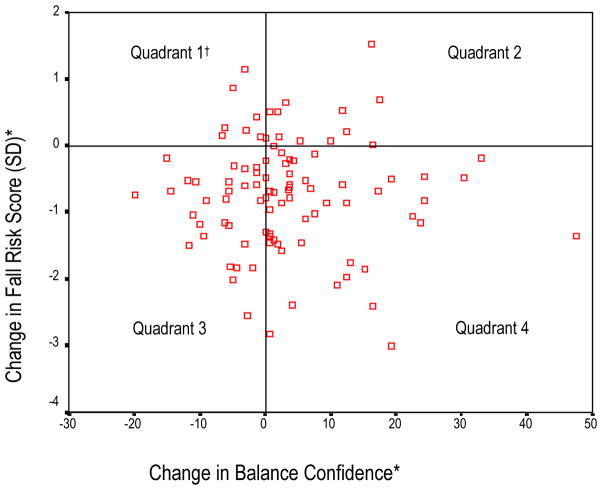
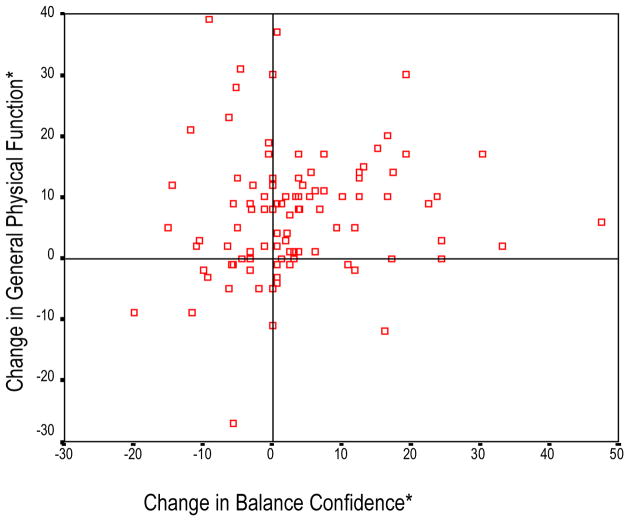
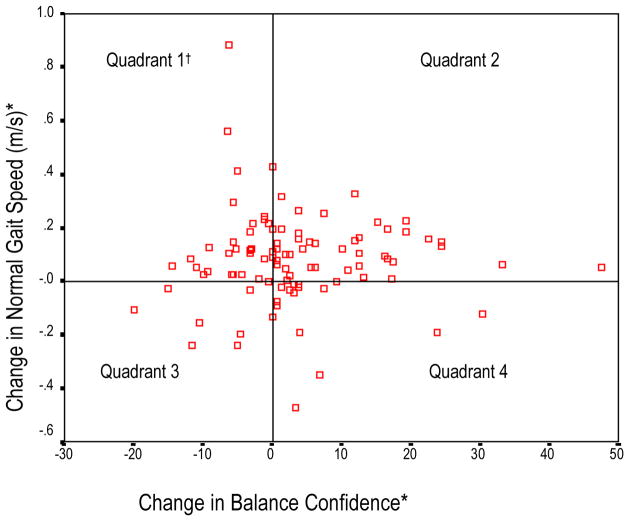
Correlations between the (change) variables of interest are shown in Table 3. Change in balance confidence after 13 weeks of exercise intervention was not significantly correlated with change in fall risk score, postural stability, gait speed, or physical activity level. Although change in balance confidence was significantly associated with change in general physical function, it was a weak association (rho=0.207). Figures 2 to 4 illustrate the relationship between change in balance confidence and change in fall risk score, gait speed, and general physical function.
Table 3.
Spearman rank correlation coefficient matrix between balance confidence and variables of interest. Balance confidence (ABC Scale score), postural stability (mm), normal gait speed (m/s), fast gait speed (m/s), general physical function (Community Balance and Mobility Scale), and physical activity level (PASE score)*.
| Δ Fall Risk Score | Δ Stability | Δ Normal Gait | Δ Fast Gait | Δ Function | Δ Activity | |
|---|---|---|---|---|---|---|
| Δ Balance Confidence | −0.006 | −0.019 | 0.058 | −0.031 | 0.207* | 0.047 |
Significantly correlated at p≤0.05.
Figure 2. Scatterplot of change in fall risk score versus change in balance confidence.
*Negative change value in fall risk score indicates improvement. Positive value in balance confidence indicates improvement.
†Quadrants 2 and 3 indicate discord between changes in Fall Risk Score and balance confidence.
Figure 4. Scatterplot of change in general physical function versus change in balance confidence.
*Positive change in general function and in balance confidence indicates improvement.
†Quadrants 1 and 4 indicate discord between changes in gait speed and balance confidence.
Effect Size & Percent Change
The largest effect size was observed in fall risk score (−0.81) and the smallest effect size was observed in balance confidence (0.19). Table 4 lists the effects sizes and percent changes for the variables of interest.
Table 4.
Effect sizes (delta index) and percent changes observed for balance confidence, Fall Risk Score, postural stability, gait speed, general physical function, and physical activity level (N=98).
| Variable | Effect Size* | % Change* |
|---|---|---|
| Fall Risk Score (SD) | −0.81 | −33.12 |
| Postural Stability (mm) | −0.34 | −16.04 |
| Normal Gait Speed (m/s) | 0.38 | 8.25 |
| Fast Gait Speed (m/s) | 0.40 | 8.65 |
| General Physical Function† | 0.40 | 17.92 |
| Physical Activity Level‡ | 0.58 | 33.60 |
| Balance Confidence§ | 0.19 | 4.50 |
Negative effect sizes and percent changes in fall risk score and postural stability indicate improvement. Positive effect sizes and percent changes in gait speed, general physical function, physical activity level, and balance confidence indicate improvement.
Measured by the Community Balance and Mobility Scale.
Measured by the PASE questionnaire.
Measured by the ABC Scale.
Thus, our results showed an improvement in balance confidence in both the Agility Training and the Resistance Training groups, but not the Stretching group. This was weakly correlated with change in general physical function, but not with fall risk score or other objective measures of physical abilities.
DISCUSSION
We found that both resistance training and agility training, but not general stretching, significantly enhanced balance confidence in older women with confirmed low bone mass. The mean ABC scores for the Resistance Training group and the Agility Training group were 80 and 83, respectively, after 13 weeks of training. According to Meyers and coworkers [10], ABC scores 80 and above are indicative of highly functioning, physically active older adults. To our knowledge, this is the first study that has examined the effect of different types of exercise programs on balance confidence in older adults. It is noteworthy that resistance training alone improved balance confidence. This has not been demonstrated before as previous exercise interventions that enhanced balance confidence all encompassed balance training [10–13]. Furthermore, the enhancement of balance confidence with exercise in a population of individuals at high risk of sustaining fall-related fractures and of falls is an important and new finding.
Importantly, we also observed that change in balance confidence, as assessed by the ABC scale, did not significantly correlate with change in fall risk, postural stability, gait speed, or physical activity level after 13 weeks of participating in resistance training, agility training, or general stretching. Change in balance confidence was, however, significantly associated with change in general physical function. While previous prospective exercise intervention studies [10, 11, 13] have reported improvement in physical abilities with a concomitant reduction in the fear of falling, these studies did not report change score correlations.
We found that the influence of exercise on balance confidence was of a much lower magnitude than that of exercise on fall risk, postural stability, gait speed, general physical function, and physical activity level. This finding may be due to the disparity between the variables of interest in their potential for change or improvement. For instance, the mean baseline ABC score for the cohort was 77. This is comparable to the scores (low 80s) obtained in a previous study involving individuals with osteoporosis [10]. According to Myers et al. [10], individuals who score in the mid-80s or better on the ABC are unlikely to show further improvement in balance confidence while there is room for improvement for those scoring below 80. Thus, the potential for improvement in balance confidence in our cohort may have been limited. In contrast, the mean baseline fall risk score for our entire cohort was 2.18 (Table 2), which represents a net performance of 2.18 standard deviations inferior to the age-matched mean. This indicates this group was at marked risk of falling and thereby, likely possessed a greater potential for improvement.
Our scatterplot data (Figures 2–4) indicate that an individual’s change in balance confidence can be discordant with change in fall risk, postural stability, gait speed, general physical function, or physical activity level. This underscores that balance confidence is not a measure of postural stability – and it was never designed to be one. The observation of balance confidence enhancement in the presence of increased fall risk or deterioration in physical ability is of particular concern as it implies that such an individual may partake in activities that are beyond her physical abilities, and consequently, increase her risk of falling. Thus, although fear of falling is a pervasive and serious problem in older adults, our data suggest that caution needs to be exercised when implementing strategies to enhance balance confidence so that it does not become elevated beyond actual physical abilities.
There are several possible reasons for the observed discourse between balance confidence change and changes in fall risk and physical abilities. One reason may be this study’s cohort. Our cohort consisted of older women with confirmed low bone mass, individuals who are at a greater risk of sustaining fall-related fractures compared with age-matched healthy counterparts. Assuming that our cohort is cognisant of this elevated risk of fracture, their balance confidence may be more resistant to change compared with their physical abilities and participation in physical activity. We acknowledge that some degree of fear of falling may be prudent in those at risk of sustaining fall-related fractures. The issue of what is the ‘appropriate’ amount of fear of falling, or an optimal confidence to mobility ratio, as well as what might constitute a ‘gold-standard’ for this psychological variable warrants further research.
Second, our exercise intervention programs did not include any education specifically targeting fear of falling in our study. As fear of falling is a psychological entity and multifactorial in etiology, a multidimensional approach to decrease fear of falling, such as the combination of exercise intervention and falls education, may have been more efficacious than exercise alone in enhancing balance confidence in our cohort. Third, the lack of specificity between our training programs and the 16 items of the ABC Scale may have decreased the efficacy of the intervention. The exercise programs did not specifically “train” our participants in the activities of the ABC Scale (i.e. riding an escalator holding onto the rail), but perceived self-efficacy will only generalize to highly similar situations [35].
Fourth, balance confidence may have been falsely elevated in our participants secondary to increased socialization and support with study participation. Balance confidence may also have been positively affected the by the sense of personal accomplishment associated with successfully participating in the weekly exercise classes.
Finally, the mismatch observed between change in balance confidence and the changes in fall risk and physical abilities may be due to psychosocial factors of fear of falling. Both the fear of social embarrassment and concerns about damage to social identity are feared consequences of falling [36, 37]. As we did not assess these factors in our study, we are unable to determine the contribution of these factors to the mismatch observed between the variables of interest but we recommend these behavioural determinants be given further research attention.
Our results highlight that partaking in exercise alone may increase balance confidence in the absence of improved physical abilities in older women with low bone mass. A clinical corollary of this study is that those (e.g. fitness instructors and physical therapists) who design group-based exercise programs for community-dwelling older adults should consider including an education component on factors that influence fear of falling.
CONCLUSIONS
Both resistance training and agility training significantly improved balance confidence in community-dwelling older women with low bone mass after 13 weeks of participation. This change in balance confidence was significantly correlated with change in general physical function. However, the change in balance confidence did not significantly correlate with changes in fall risk, physical abilities, and physical activity level. This may due to differences in the potential for change in the variables of interest, the cohort examined, the need for a multidimensional approach to decrease fear of falling, and training specificity. Of particular concern, is the observation of discordance between balance confidence change and changes in fall risk and physical abilities. Future studies are needed to determine interventions that would achieve concordance between the fear of falling and physical abilities in older adults.
Figure 3. Scatterplot of change in normal gait speed versus change in balance confidence.
*Positive change in gait speed and in balance confidence indicates improvement.
†Quadrants 1 and 4 indicate discord between changes in gait speed and balance confidence.
Acknowledgments
Funding: Provided by the Vancouver Foundation (BCMSF).
The Vancouver Foundation (BCMSF) and the BC Women’s Hospital Osteoporosis Program supported this project. The South Slope YMCA was a partner of this research project. Drs. Khan and Eng are Canadian Institutes of Health Research (Institute of Musculoskeletal Health and Arthritis) New Investigators. Dr. Eng received a salary support from Canadian Institutes of Health Research (MSH-63617). Drs. McKay and Eng are Michael Smith Foundation for Health Research Career Scholars. Ms. Liu-Ambrose is a Michael Smith Foundation for Health Research Doctoral Trainee and a Killam Pre-Doctoral Fellow.
References
- 1.Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348:42–49. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 2.Tinetti M, Speechley M, Ginter S. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol. 1994;49:M140–147. doi: 10.1093/geronj/49.3.m140. [DOI] [PubMed] [Google Scholar]
- 4.Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol. 1991;46:M123–131. doi: 10.1093/geronj/46.4.m123. [DOI] [PubMed] [Google Scholar]
- 5.Howland J, Lachman ME, Peterson EW, Cote J, Kasten L, Jette A. Covariates of fear of falling and associated activity curtailment. Gerontologist. 1998;38:549–555. doi: 10.1093/geront/38.5.549. [DOI] [PubMed] [Google Scholar]
- 6.Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84:565–570. doi: 10.2105/ajph.84.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55:M299–305. doi: 10.1093/gerona/55.5.m299. [DOI] [PubMed] [Google Scholar]
- 8.Myers A, Powell L, Maki B, Holliday P, Brawley L, Sherk W. Psychological indicators of balance confidence: Relationship to actual and perceived abilities. J Gerontol. 1996;51A:M37–M43. doi: 10.1093/gerona/51a.1.m37. [DOI] [PubMed] [Google Scholar]
- 9.Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 10.Myers A, Fletcher P, Myers A, Sherk W. Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) scale. J Gerontol. 1998;53:M287–294. doi: 10.1093/gerona/53a.4.m287. [DOI] [PubMed] [Google Scholar]
- 11.Taggart HM. Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older women. Appl Nurs Res. 2002;15:235–242. doi: 10.1053/apnr.2002.35975. [DOI] [PubMed] [Google Scholar]
- 12.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 13.Yates S, Dunnagan T. Evaluating the effectiveness of a home-based fall risk reduction program for rural community-dwelling older adults. J Gerontol. 2001;56A:M226–M230. doi: 10.1093/gerona/56.4.m226. [DOI] [PubMed] [Google Scholar]
- 14.Liu-Ambrose T, Khan K, Eng J, Janssen P, Lord S, McKay H. Both resistance and agility training reduce fall risk in 75–85 year old women with low bone mass: A six-month randomized controlled trial. J Am Geriatr Soc. 2004:000–000. doi: 10.1111/j.1532-5415.2004.52200.x. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO Study Group. WHO Technical Report Series. Geneva: World Health Organization; 1994. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis; p. 843. [PubMed] [Google Scholar]
- 16.Chisholm D, Collins M, Kulak L, Davenport W, Gruber N. Physical activity readiness. Br Col Med J. 1975;17:375–378. [Google Scholar]
- 17.Canadian Society for Exercise Physiology. Par-Q and You. Gloucester, Ontario, Canada: Canadian Society of Exercise Physiology; 1994. [Google Scholar]
- 18.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 19.Krieger N, Tenenhouse A, Joseph L, Mackenzie M, Poliquin S, Brown J, et al. The Canadian Multicentre Osteoporosis Study. Can J Aging. 1999;18:376–387. [Google Scholar]
- 20.Lord S, Menz H, Tiedemann A. A physiological profile approach to falls risk assessment and prevention. Phys Ther. 2003;83:237–252. [PubMed] [Google Scholar]
- 21.Lord S, Clark R, Webster I. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc. 1991;39:1194–1200. doi: 10.1111/j.1532-5415.1991.tb03574.x. [DOI] [PubMed] [Google Scholar]
- 22.Lord S, Ward J, Williams P, Anstey K. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42:1110–1117. doi: 10.1111/j.1532-5415.1994.tb06218.x. [DOI] [PubMed] [Google Scholar]
- 23.Lord S, Castell S. Physical activity program for older people. Effect on balance, strength, neuromuscular control, and reaction time. Arch Phys Med Rehabil. 1994;75:648–652. doi: 10.1016/0003-9993(94)90187-2. [DOI] [PubMed] [Google Scholar]
- 24.Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott A, Hausherr E, et al. Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996;348:145–149. doi: 10.1016/s0140-6736(96)01440-7. [DOI] [PubMed] [Google Scholar]
- 25.Lord S, Lloyd D, Nirui M, Raymond J, Williams P, Stewart R. The effect of exercise on gait patterns in older women: A randomized controlled trial. J Gerontol. 1996;51A:M64–M70. doi: 10.1093/gerona/51a.2.m64. [DOI] [PubMed] [Google Scholar]
- 26.Howe J, Inness E, Verrier M, Williams J. American Congress of Rehabilitation Medicine. 1999. Development of the Community Balance and Mobility Scale (CB&M) for the Traumatic Brain Injury (TBI) [Google Scholar]
- 27.Wallmann H. Comparison of elderly nonfallers and fallers on performance measures of functional reach, sensory organization, and limit of stability. J Gerontol. 2001;56A:M580–583. doi: 10.1093/gerona/56.9.m580. [DOI] [PubMed] [Google Scholar]
- 28.Briggs R, Gossman M, Birch R, Drews J, Shaddeau S. Balance performance among noninstituionalized elderly women. Physical Activity. 1989;69:748–756. doi: 10.1093/ptj/69.9.748. [DOI] [PubMed] [Google Scholar]
- 29.Powell L, Myers A. The Activities-specific Confidence (ABC) scale. J Gerontol. 1995;50A:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 30.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 31.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 32.Braith RW, Graves JE, Leggett SH, Pollock ML. Effect of training on the relationship between maximal and submaximal strength. Med Sci Sports Exerc. 1993;25:132–138. doi: 10.1249/00005768-199301000-00018. [DOI] [PubMed] [Google Scholar]
- 33.Province MA, Hadley EC, Hornbrook MC, Lipsitz LA, Miller JP, Mulrow CD, et al. The effects of exercise on falls in elderly patients. A preplanned meta- analysis of the FICSIT Trials. Frailty and Injuries: Cooperative Studies of Intervention Techniques. JAMA. 1995;273:1341–1347. [PubMed] [Google Scholar]
- 34.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. Appleton and Lange; Norwalk: 1993. [Google Scholar]
- 35.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 36.Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-dwelling older people. The Gerontologist. 2002;42:17–23. doi: 10.1093/geront/42.1.17. [DOI] [PubMed] [Google Scholar]
- 37.Yardley L. Fear of imbalance and falling. Reviews in Clinical Gerontology. 1998;8:23–29. [Google Scholar]