SUMMARY
The relationship between voice and posture has been previously investigated. The aim of this study was to evaluate postural alterations in subjects with dysfunctional dysphonia and to analyse their variations after rehabilitation. Forty subjects with hypokinetic dysfunctional dysphonia were submitted to posturographic analysis with alternatively open and closed eyes; subjects were invited to stand upright and breath normally so that the vestibular-spinal reflex could be assessed. The following variables were considered: pressure centre coordinates on frontal and sagittal planes and standard deviations (SD), length and surface of the tract, mean velocity of the oscillations and SD, spectral frequency analysis of oscillations, statokinesigram and stabilogram. At baseline, the parameters showing the highest alterations were surface and velocity SD. All parameters improved after rehabilitation, particularly SD(X) and SD(Y), surface, velocity and relative SD; the centre of pressure shifted backwards in all patients. These results confirm that in subjects with dysfunctional dysphonia, the greater proprioceptive awareness acquired through speech therapy permits improvement in postural performance. Static stabilometry is a fundamental test for demonstrating basal postural alterations and for evaluating improvement after rehabilitation.
KEY WORDS: Posture, Posturography, Static stabilometry, Proprioception, Dysfunctional voice disorders, Speech rehabilitation
RIASSUNTO
Negli ultimi anni sono state sottolineate le correlazioni tra controllo posturale e funzione vocale. Lo scopo di questo studio è quello di valutare le alterazioni posturali in soggetti con disfonia disfunzionale e di analizzare le variazioni posturali dopo il trattamento riabilitativo. Quaranta soggetti con disfonia disfunzionale ipocinetica sono stati sottoposti ad analisi posturografica a occhi aperti e chiusi. I pazienti sono stati invitati a stare in piedi e respirare normalmente in modo da poter studiare meglio il riflesso vestibolo-spinale. Le variabili considerate sono state: coordinate del centro di pressione sul piano frontale e sagittale e le deviazioni standard relative (SD), la lunghezza e la superficie del tracciato, velocità media delle oscillazioni e la relativa deviazione standard, l'analisi spettrale di frequenza delle oscillazioni, Statokinesigramma e Stabilogramma. In condizioni basali, i parametri più alterati sono stati la superficie e la SD della velocità. Tutti i parametri sono migliorati dopo il trattamento, in particolare SD (X) e SD (Y), la superficie, la velocità e la relativa deviazione standard; il centro di pressione si è spostato indietro in tutti i pazienti. I risultati del nostro studio confermano che nei soggetti con disfonia disfunzionale, la maggiore consapevolezza propriocettiva acquisita attraverso la terapia logopedica permette un miglioramento della loro performance posturale. La stabilometria statica è un test fondamentale per dimostrare alterazioni posturali in condizioni basali e per valutare il miglioramento dopo il trattamento riabilitativo.
Introduction
There is general agreement in the literature that good, functional posture is fundamental for quality of the human voice 1-7. Furthermore, in the last 10 years or so, emphasis has been paid to the association between posture control and voice function (both for normal speech and for professional artistic performance) 8-10. As amply reported in the literature, this correlation is a reciprocal influence that can be greatly disturbed when muscular tone is altered 11 12.
Muscle tension dysphonia and muscle misuse dysphonia are disorders that corroborate the strict link between so-called dysfunctional dysphonia and postural alignment 6 13 14. In fact, dysfunctional dysphonia is generally associated with altered extra-laryngeal muscle activity, although it is still not clear whether altered extra-laryngeal tension is the cause or effect of inadequate laryngeal activity. However, modifications in postural control that emerge in these cases have an important role in the genesis and/or maintenance of dysfunctional dysphonia. The dysfunctional situation very likely creates a vicious circle in which altered extra-laryngeal tension and inadequate laryngeal activity coexist and sustain each other.
In the past, the majority of authors who have dealt with the association between posture and voice have focused principally on descriptive studies, such as observing the attitude of the human body at rest and during phonation, noting the position of certain areas during forced or ventilated vocalisation, or studying what happens when a microphone or a musical instrument is used at the same time 15-19. This purely 'descriptive' approach paved the way for studying the anatomical-functional relationship between postural alignment and phonation, but it encountered inevitable limitations. In the first instance, there is a certain amount of confusion regarding the definition of 'posture', the methods used for assessing it and diagnostic classification of postural disorders. This has made it difficult in the past to identify the specific causal effects on voice disorders, and consequently plan appropriate speech/rehabilitation therapy. In addition, considering postural performance prevalently from a biomechanical point of view can be inaccurate because this does not take into account the principles at the basis of the final motor output; that is, it does not consider the subcortical integration of the inputs coming from the sensorial visual-oculomotor, vestibular-cochlear and proprioceptive structures. Lastly, a study on posture during forced voice production, ventilation or singing, inevitably attributes too much importance to the voluntary component rather than to the reflex one, which is an automatic feature of the complex system of posture control. In recent years, studying posture with a stabilometric platform has helped to overcome some of the limitations mentioned above 10-12 14. In particular, this platform permits a computerized analysis of posture – offering extremely sensitive parameters – even in subjects who are not affected with primary balance disorders, such as those with pure dysfunctional dysphonia or if this is associated with secondary organic lesions. Moreover, using static stabilometry (on subjects with their eyes open, eyes closed, and eyes closed with the head bent backwards), the importance of the individual sensorial inputs (visual, vestibular and cervical proprioceptive) can be assessed, and when the test is performed during natural breathing (not forced) it is possible to study the prevalently reflex component of posture (spinal vestibular reflex: SVR). In fact, the systems controlling posture, balance and organization of body movement rely principally on the integration of specific sensorial patterns for their function, followed by the elaboration of specific motor responses that are mainly reflex ones (the most important of which is undoubtedly the SVR). In addition, postural studies carried out with static stabilometry can reveal the alterations associated with dysfunctional dysphonia in basal conditions, and then evaluate any variations in the stabilometric parameters after speech/rehabilitation therapy 10.
The aim of this work was to study postural variations in 40 subjects affected with pure hypokinetic dysfunctional dysphonia by static stabilometry in basal conditions and after a cycle of speech/rehabilitation therapy. Moreover, by performing the stabilometric test on the subjects when eyes were open and then closed, we evaluated if there was any predominating sensorial input on the maintenance of posture before and after therapy. The postural study carried out during spontaneous breathing without voice production was mainly to investigate the reflex component that controls posture alignment, namely the spinal vestibular reflex.
Materials and methods
In this study, 40 consecutive patients (all female, mean age 37.9 ± 10.9 yrs) affected with pure hypokinetic dysfunctional dysphonia and previously untreated with vocal training, were submitted to a posturographic test using a static stabilometric platform (S.Ve. P. Amplaid). The stabilometric examination with the subjects' eyes open and eyes closed was performed in basal conditions and after a cycle of vocal/rehabilitation therapy.
Each patient underwent accurate phoniatric and otorhinolaryngoiatric anamnesis, a general ENT examination, flexible fiber optic rhino-pharyngo-laryngoscopy, videolaryngostroboscopy, electro-acoustic voice tests including spectrography and analysis of vocal signal with the Multi-Dimensional Voice Program (MDVP). All patients had been suffering from chronic dysphonia for at least six months, with variable periods of deterioration that were generally associated with the voice having been abused. They all remarked that their voice disorder limited their social or working life. The subjective degree of severity of the condition was evaluated using the voice handicap index (VHI) questionnaire, which each patient filled in before therapy 20. The perceptive evaluation of voice was scored against the GIRBAS Scale 21.
Both flexible fiber optic endoscopy and videolaryngostroboscopy revealed pure dysfunctional hypokinetic dysphonia without any secondary laryngeal disorder in all subjects. None of the patients showed signs of hypertonia in the supraglottic structures or posterior phlogosis due to gastro-oesophageal reflux. In all subjects, laryngostroboscopy revealed failure of glottic closure: in 15 cases, the failure was posterior triangle-like, in 20 it was oval and in 5 it was hourglass-like with pre-contact between the anterior third and posterior two-thirds of the vocal chords. In the abduction phase in these latter five cases, no nodules or initial signs of nodules were seen on the vocal chords. In 18 cases, there was also bilateral, symmetric sub-level depression of vocal chords associated with marked hypotonia. In all cases, stroboscopic light showed that there was no deficit in chord mucosa vibration and that the glottic wave was regular and symmetric.
Pneumophonic function was uncoordinated in all patients study and the majority had various degrees of intra-rotation of the shoulders, caved-in chest and hyperextension of the neck with the jaws slightly thrust forwards. After accurate anamnesis and orthopaedic examinations, all patients with orthopaedic disorders or known postural defects (varus/valgus foot, scoliosis, previous orthopaedic surgery of any kind, etc.) were excluded from the study. In addition, the following tests were performed: accurate oto-neurological assessment, liminal tonal audiometry, investigation of spontaneous and provoked nystagmus by videonystagmography and vestibular caloric balance. Those who showed balance disorders during anamnesis and/or were classified positive upon oto/neurological examination were excluded from the study. Other exclusion criteria were: systemic disease, alcohol abuse, psychiatric disorder and vision less than 10/10.
Static stabilometry was performed using a computerised platform (S. Ve. P. Amplaid), inviting the patients to stand upright during the test and breathe normally. The test was carried out with the patients' eyes both open (OE) and closed (CE) to eliminate optical afferences and enhance proprioceptive faculties. The posturographic test was carried out in basal conditions (Pre-) and then repeated at the end of the rehabilitation therapy (Post-).
The following parameters were considered: pressure centre coordinates on the frontal (X; right-left) (minimum X, maximum X, mean X) and sagittal (Y; forwardbackward) (minimum Y, maximum Y, mean Y) areas; total length of the recording in mm (L); surface of the helix containing 90% of the points sampled (S); mean velocity and relative SD; Fourier fast transform (FFT) for oscillations on the X and Y axes separately; statokinesigram describing the area within which the centre of gravity projects with respect to the floor, and stabilogram which reveals the time taken for the pressure centre to shift on both the X and Y axis.
Rehabilitation technique used for dysphonia associated with modifications in posture
The therapy was performed five days a week for four weeks; each single session lasted 60 min. The therapeutic approach foresaw: improved awareness of the body and psychomotor self-control by supplying the patients with simple notions of physiology, and in particular the mechanics involved in breathing and speech; teaching the patient how to judge his own voice (dysphonic or progressively euphonic), which will allow him/her to regain automatic control of voice production. Therefore, therapy sessions were based on posture awareness-control and voice correction. In particular, the aim of this therapy was to facilitate global postural alignment in association with proprioceptive vocal exercises, to restore tone to the ribdiaphragm fascia, to relax the scapulohumeral girdle and facilitate projection of the voice.
Statistical analysis
All the numeric parameters are expressed in medians. A comparison was performed between several parameters at different times, before and after rehabilitation therapy. The comparison (before eyes opened vs after eyes opened; before eyes closed vs after eyes closed) was carried out considering the median of the different parameters with a Mann-Whitney non-parametric test, and considering the same parameters for the percentage of pathological patients using a chi2 test. The parameters resulting above the normal range with this instrument were considered pathological. All tests were considered significant with p < 0.05. A StatView 5 release 5.0.1 was used for processing the data.
Results
Laryngostroboscopy performed at the end of speech/rehabilitation therapy revealed an improvement in the laryngeal dysfunction in all subjects. In the 15 cases with the posterior triangle form of failed closure of the glottis, post-treatment investigation demonstrated either regular closure of the glottis or (in 2 cases) a paraphysiological small posterior triangle failure of glottic closure. After therapy, 16 of the 20 cases with oval glottic failure showed regular glottic closure during phonation and in the remaining 4 the glottic gap corresponding to the failed closure had decreased. The 5 cases with pre-contact and hourglass-type closure failure showed improved chord adduction at the control visit, where no organic lesions on the chords and no sub-level depression of the vocal chords were seen in any patient. Three of the patients with oval glottic closure failure in basal conditions showed signs of compensating hypertonia of the supraglottic structures when re-examined.
Stabilometric study
Pre-OE vs Post-OE
The comparison performed within the same group before and after rehabilitation with the patients' eyes open (Pre- OE vs Post-OE) produced the following results. Taking into account the value of the median for the parameters being studied, after speech therapy there was a statistically significant reduction in the SD (X) (0.28 vs 0.21; p = 0.02), SD (Y) (0.34 vs 0.26; p = 0.001), surface (153.30 vs 113.20 mm2; p = 0.008), velocity (9.51 vs 8.37 mm/ sec; p = 0.004) and velocity SD (5.68 vs 4.87; p = 0.001) (Mann-Whitney non-parametric test). Even the length parameter (median) decreased slightly after therapy, although the difference was not statistically significant. After treatment, the statokinesigram showed a slight backward shift in all patients when their eyes were open, in spite of the fact that the medians of sagittal plane shifting (Ymin, Ymax, Ymed; pre- vs post-therapy) showed no statistically significant difference. When the percentage of pathological patients was evaluated for individual parameters, and the data obtained in eyes-open mode before and after therapy were compared (Pre-OE vs Post-OE), there was a statistically significant difference for Ymax (12.5% vs 0; p = 0.02), S (17.5% vs 2.5%; p = 0.03) and velocity SD (27.5% vs 2.5%; p = 0.008) (chi2 test). Even Xmin and Xmax showed improvement after therapy, although these differences were not statistically significant. In fact, while there were 6 subjects (15%) who were pathological for Xmin in basal conditions, after treatment these dropped to 3 (7.5%). In the case of Xmed, there were 3 (7.5%) subjects who were pathological in basal conditions and only one (2.5%) outside the range after therapy. The data referring to the Pre-OE vs Post-OE comparison are summarized in Table I.
Table I.
Pre-OE and Post-OE: values of each parameter in the eyes-open mode study, before and after rehabilitation (median). Pre-OE N (%) and Post-OE N (%): number of pathological patients and the relative percentage for each parameter. p1: statistical significance of the pre- vs post-therapy comparison referring to the median (Mann-Whitney). p2: statistic significance of the pre- vs post-therapy comparison referring to the number of pathological patients (Chi2).
| Pre-OE | Post-OE | p1 | Pre-OE N (%) | Post-OE N (%) | p2 | |
|---|---|---|---|---|---|---|
| Xmin | -11.20 | -9.66 | NS | 6 (15%) | 3 (7.5%) | NS |
| Xmax | 4.78 | 1.44 | NS | 4 (10%) | 4 (10%) | NS |
| Xmed | -4.11 | -3.55 | NS | 3 (7.5%) | 1 (2.5%) | NS |
| SD (X) | 0.28 | 0.24 | 0.02 | - | - | - |
| Ymin | -44.40 | -45.20 | NS | 2 (5%) | 0 | NS |
| Ymax | -24.30 | -30.00 | NS | 5 (12.5%) | 0 | 0.02 |
| Ymed | -35.95 | -36.27 | NS | 0 | 0 | - |
| SD (Y) | 0.34 | 0.26 | 0.001 | - | - | NS |
| L | 235.55 | 231.80 | NS | 1 (2.5%) | 1 (2.5%) | NS |
| S | 153.30 | 113.20 | 0.008 | 7 (17.5%) | 1 (2.5%) | 0.03 |
| FFTx | 0.08 | 0.08 | NS | - | - | - |
| FFTy | 0.08 | 0.04 | NS | - | - | - |
| VEL | 9.51 | 8.37 | 0.004 | - | - | - |
| SD (VEL) | 5.68 | 4.87 | 0.001 | 11 (27.5%) | 1 (2.5%) | 0.008 |
Pre-CE vs Post-CE
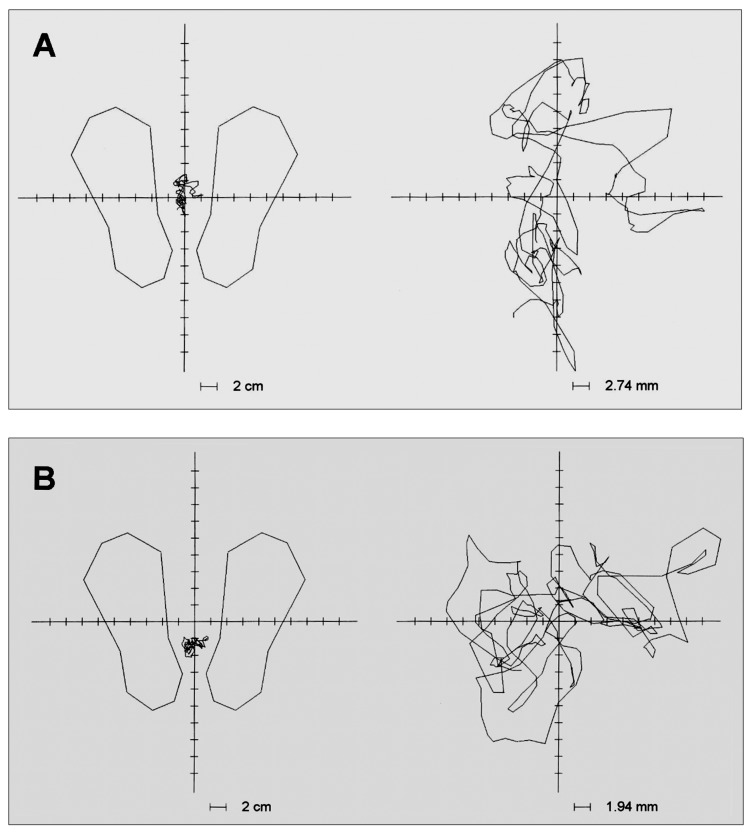
Comparison within the same group before and after treatment with the patients' eyes closed (Pre-CE vs Post-CE) gave the following results. Taking into consideration the median value of all parameters in the study, there was a statistically significant reduction in SD (X) (0.40 vs 0.31; p = 0.0008) and SD (Y) (0.40 vs 0.35; p = 0.02) after therapy. The surface and length (medians) were also lower after treatment, although these differences were not statistically significant. Even in this case, the statokinesigram revealed a slight shift backwards after therapy in all subjects, in spite of the fact that the medians corresponding to the shift on the sagittal plane (Ymin, Ymax, Ymed) showed no statistically significant difference (Fig. 1). When the percentage of pathological patients was evaluated for each parameter and the data obtained before and after rehabilitation treatment with their eyes closed was compared, there was a statistically significant difference in the case of Ymin (10% vs 0; p = 0.04) and Ymax (10% vs 2,5%; p = 0.04), S (17.5% vs 2.5%; p = 0.03) and velocity SD (27.5% vs 2.5%; p = 0.008) (chi2 test). It is worth noting is that while no statistically significant difference was seen, even the Xmin (15% vs 7.5%), Xmed (10% vs 7.5%), Ymed (10% vs 2.5%), surface (20% vs 10%) and velocity SD (22.5% vs 17.5%) parameters decreased in pathological patients. The data referring to the Pre-EC vs Post-EC comparison are provided in Table II.
Fig. 1.
Statokinesigram in a patient before (A) and after (B) rehabilitation. The centre of pressure shift backwards and the surface parameter after therapy shows less dispersion of the oscillations on the platform, particularly on the sagittal plane.
Table II.
Pre- and Post considering the parameters in the eyes-closed mode (CE).
| Pre-CE | Post-CE | p1 | Pre-CE N (%) | Post-CE N (%) | p2 | |
|---|---|---|---|---|---|---|
| Xmin | -15.20 | -11.70 | NS | 6 (15%) | 3 (7.5%) | NS |
| Xmax | 6.35 | 5.20 | NS | 1 (2.5%) | 3 (7.5%) | NS |
| Xmed | -2.80 | -4.65 | NS | 4 (10%) | 3 (7.5%) | NS |
| SD (X) | 0.40 | 0.31 | 0.0008 | - | - | - |
| Ymin | -47.95 | -54.00 | NS | 4 (10%) | 0 | 0.04 |
| Ymax | -29.35 | -29.60 | NS | 4 (10%) | 0 | 0.04 |
| Ymed | -38.05 | -40.98 | NS | 4 (10%) | 1 (2.5%) | NS |
| SD (Y) | 0.40 | 0.35 | 0.02 | - | - | - |
| L | 390.09 | 356.56 | NS | 0 | 0 | - |
| S | 252.91 | 241.75 | NS | 8 (20%) | 4 (10%) | NS |
| FFTx | 0.08 | 0.08 | NS | - | - | - |
| FFTy | 0.08 | 0.08 | NS | - | - | - |
| VEL | 15.57 | 13.64 | NS | - | - | - |
| SD (VEL) | 9.51 | 8.61 | NS | 9 (22.5%) | 7 (17.5%) | NS |
Discussion
In order to understand the anatomical and functional relationship between voice and posture, the structures associated with the larynx must be considered; the jaws and the hyoid bone are very important in this respect 22. In fact, since the larynx is suspended from the hyoid bone, it can vary its position according to how the hyoid bone itself moves, or, indirectly, when the head, jaws (and thus temporo- mandibular articulation), cervical spine and scapular girdle move 23. If one considers the muscle-tendon and ligament connections of the hyoid bone with these parts of the skeleton, the anatomical-functional relationship between the larynx and posture becomes clear 24. Any nonalignment or torsional imbalance of the entire spine and the cervical area, in particular, directly influences the position of the hyoid bone because of the above-mentioned anatomical connections and, indirectly, the position (and functioning, of course) of the larynx as well.
In this regard, it is easy to understand how posture and muscular-skeletal dysfunctions can influence the position of the larynx and its phonic function. Nevertheless, it is still not clear how primary laryngeal dysfunctions can influence posture and how these two conditions (laryngeal and extra-laryngeal dysfunction) can withstand and sustain each other. The fact that dysfunctional dysphonia, whether pure or associated with secondary laryngopathy, is associated with modified respiratory dynamics and a particular conformation, was acknowledged many years ago 25. The posture of a subject affected with dysfunctional dysphonia accompanied by hypotonia and hypokinesis often shows the typical forward shift of the centre of pressure, due to hollow of the chest and forward flexion of the thoracic spine; deflexion of the neck and forward thrust of the jaws are also present. Hence, the relationship between posture and voice appears to move in a two-way direction: modification in posture secondary to exogenous stimulation can affect the voice, while alterations to the voice production mechanism can cause modifications in posture. The fundamental processes of postural compensation exerted by the different parts of the skeleton are to be considered essentially reflex phenomena, generated in response to the various patterns of specific sensorial inputs. In this respect, over and above the SVR, there are tonic reflexes in the neck, local static reactions, tonic reflexes of the labyrinth, optical reflexes and plantar reflexes. Using these reflexes, the CNS regulates the 'entire motor mechanism' rather than just the activity of individual muscles. As a consequence, even the simplest motor responses have to be interpreted as a complex motor action, in which the different synergies involved in muscular-skeletal activation are organized differently by CNS control, which is exerted through the continuous uptake of proprioceptive and exterioceptive information sent to the CNS by the different receptor systems 26. In phoniatrics, these neurophysiological principles permit greater comprehension of the relationship between posture and voice. In fact, there is continuous comparison among the following: proprioceptive signals that represent the state of laryngeal activation (muscular, fascial, ligamentous, articular), specific sensorial signals generated by sub-glottic pressure, proprioceptive and exterioceptive signals that derive from extra-laryngeal muscular-skeletal structures (diaphragm, spine, scapular and pelvic girdle) and acoustic signals that supply information concerning the results of phonic activity. Therefore, it is clear that when there is incorrect control over laryngeal muscles, the information relayed will be incongruent and the consequent motor output will be inadequate. This way, when the CNS tries to correct the 'complex motor activity' it enables laryngeal and extralaryngeal compensation procedures that are prevalently reflex and can cause functional alterations in the voice and in posture, maintaining them over time. Likewise, when primary alterations occur in the extra-laryngeal muscletendon and muscle-skeleton structures (distortive trauma in the cervical spine, temporo-mandibular articulation dysfunctions, skull-mandibular or skull-cervical imbalance, poorly elastic surgical scarring), reflex dysfunctions can appear even in the laryngeal muscles and cause dysfunctional dysphonia and dysodia.
Some authors suggest that the geometric representation of the human body mainly depends upon information supplied by the proprioceptive afferences, and they stress the fact that since proprioception comes from all parts of the body it obviously plays a fundamental role in maintaining static posture 27 28. Hence, proprioception (in the sense of perception of articular position, of muscle strength and spatial and temporal cutaneous discrimination), appears to be the most important element in the management of posture, at least under static conditions 29.
It is clear, therefore, that rehabilitation treatment for dysfunctional dysphonia should not ignore postural alterations. Using static stabilometry in this study in patients affected with dysfunctional dysphonia, we were able to demonstrate not only the postural alterations in basal conditions but also how many of the postural parameters can vary after rehabilitation speech therapy. The parameters that were altered most prior to the treatment were surface, velocity and velocity SD. After therapy, the improvement in these parameters in the eyes-open mode was statistically significant. Regarding the surface parameter after therapy, there was less dispersion of the oscillations on the platform due to greater precision of the postural system; the decrease in the velocity values and its SD means that less energy is spent by the system and that the oscillations are more homogeneous. The fact that these alterations and their improvement are more evident in the eyesopen mode shows that the visual input in these patients is unable to stabilize the postural system, unlike what happens in balance disorders of a peripheral nature (labyrinth deficit). Other parameters that showed statistically significant improvement, both in eyes-open and eyes-closed modes, were SD(X) and SD(Y), demonstrating that there was greater homogeneity in the oscillations on both planes after speech therapy. Considering the percentage of pathological patients, the Ymax parameter (maximum shifting on the sagittal plane) also showed significant improvement both in the eyes-open and eyes-closed mode because of fewer oscillations on the sagittal plane after treatment. Moreover, the Statokinesigram showed that the centre of pressure was more or less shifted backwards in all patients after rehabilitation. We can also say that even the parameters referring to lateral plane shifting (Xmax, Xmed, Xmin) improved with the therapy, and while this was not statistically significant, it confirmed that the oscillation on all the planes was less.
Hence, our data demonstrate how rehabilitation treatment can improve postural performance. Previous studies have suggested that labyrinth inputs can prevalently influence the surface parameter, while proprioceptive ones influence velocity 30 31. All the same, other authors stress that when a healthy subject with no vestibular deficit stands erect on a flat surface (like a stabilometric platform), both shifting of the body and the speed of this shift can be monitored through the proprioceptive afferences 32.
The results of our study, which agree with the latest reports in the literature 10, confirm that in subjects affected with dysfunctional dysphonia the greater proprioceptive awareness acquired through speech therapy permits improvement in the majority of postural parameters evaluated with static stabilometry, including the surface parameter. It is likely, therefore, that when there is no pathological vestibular input, the majority of the postural parameters studied (including the surface) are controlled mainly by the proprioceptive system.
Conclusions
When static stabilometry is used for studying a series of numeric parameters and graphic representations, it can demonstrate postural alterations in the basal condition present in subjects affected with dysfunctional dysphonia and, consequently, the postural changes that can be obtained with appropriate speech-rehabilitation therapy. These results appear to be related to the greater precision in postural performance, which is probably due to the fact that rehabilitation made the subjects more aware of the proprioceptive structure of their body. In fact, the speech therapy performed revealed that in the majority of cases there was a chain reaction, in which better control over voice and breathing led to improvement in posture, and vice-versa, through a reciprocal activation-stimulation mechanism. The results of our study, which are in agreement with the latest reports in the literature, show how rehabilitation therapy should not be focused exclusively on the larynx, but should also involve postural performance 10 33. To confirm this, further studies on a larger population of patients with different types of dysphonia must be performed.
References
- 1.McKinney JC. Diagnosis and correction of vocal faults: a manual for teachers of singing and for choir directors. Revised edition. Nashville. TN: Genevox Music Group; 1994. [Google Scholar]
- 2.Brown OL. Discover your voice: how to develop healthy voice abits. San Diego. CA: Singular; 1996. [Google Scholar]
- 3.Dennehy C, Saxon K, Schneider C. Exercise physiology principles applied to voice performance: the improvement of postural alignment. J Voice. 1997;11:332–333. doi: 10.1016/s0892-1997(97)80012-4. [DOI] [PubMed] [Google Scholar]
- 4.Peckham A. The contemporary singer: elements of vocal technique. Boston. MA: Berklee Press; 2000. [Google Scholar]
- 5.Rubin JS, Mathieson L, Blake A. Posture and voice. J Singing. 2004 Jan;60:271–275. January/February. [Google Scholar]
- 6.Behrman A. Common practices of voice therapists in the evaluation of patients. J Voice. 2005;19:454–469. doi: 10.1016/j.jvoice.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Herman-Ackah YD. Physiology of voice production: considerations for the vocal performer. J Singing. 2005 Nov;62:173–176. November/December. [Google Scholar]
- 8.Kooijman PG, Jong FI, Oudes MJ, et al. Muscular tension and body posture in relation to voice handicap and voice quality in teachers with persistent voice complaints. Folia Phoniatr Logop. 2005;57:134–147. doi: 10.1159/000084134. [DOI] [PubMed] [Google Scholar]
- 9.Koufman JA, Radomski TA, Joharii GM, et al. Laryngeal biomechanics of the singing voice. Otolaryngol Head Neck Surg. 1996;115:527–537. doi: 10.1016/S0194-59989670007-4. [DOI] [PubMed] [Google Scholar]
- 10.Bruno E, Padova A, Napoletano B, et al. Voice disorders and posturography: variables to define the success of rehabilitative treatment. J Voice. 2009;23:71–75. doi: 10.1016/j.jvoice.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Grini MN, Ouaknine M, Giovanni A. Contemporary postural and segmental modification of forced voice. Rev Laryngol Otol Rhinol. 1998;4:253–257. [PubMed] [Google Scholar]
- 12.Giovanni A, Assalante C, Galmiche A, et al. Forçage vocale et posture: ètudes expérimentales chez le sujet sain. Rev Laryngol Otol Rhinol. 2006;5:285–291. [PubMed] [Google Scholar]
- 13.Angsuwaramgess T, Morrison M. Extrinsic laryngeal muscular tension in patients with voice disorders. J Voice. 2002;16:333–343. doi: 10.1016/s0892-1997(02)00105-4. [DOI] [PubMed] [Google Scholar]
- 14.Giovanni A, Akl L, Ouakine M. Postural dynamics and vocal effort: preliminary experimental analysis. Folia Phoniatr Logop. 2008;60:80–85. doi: 10.1159/000114649. [DOI] [PubMed] [Google Scholar]
- 15.Hoit JD, Plassman BL, Lansing RW, et al. Abdominal muscle activity during speech production. J Appl Physiol. 1988;6:2656–2664. doi: 10.1152/jappl.1988.65.6.2656. [DOI] [PubMed] [Google Scholar]
- 16.Hoit JD. Influence of body position on breathing and its implications for the evaluation and treatment of speech and voice disorders. J Voice. 1995;9:341–347. doi: 10.1016/s0892-1997(05)80196-1. [DOI] [PubMed] [Google Scholar]
- 17.Manchester RA. Musculoskeletal problems of adolescent instrumentalist. Med Probl Perform Art. 1997;12:72–74. [Google Scholar]
- 18.Zetterberg C, Backlund H, Karlsson J, et al. Musculoskeletal problems among male and female music students. Med Probl Perform Art. 1998;13:160–166. [Google Scholar]
- 19.Cayreyre F, Akl L, Amy de la Bretèque B, et al. Augmentation des mouvements respiratoires abdominaux lors du passage soudain de la voix conversationnelle à la voix forte. Rev Laryngol Otol Rhinol. 2005;5:347–351. [PubMed] [Google Scholar]
- 20.Jacobson BH, Johnson A, Grywalsky C, et al. The voice handicap index (VHI): development and validation. Am J Speech Lang Pathol. 1997;6:66–70. [Google Scholar]
- 21.Dejonckere PH, Remacle M, Fresnel-Elbaz E, et al. Differentiated perceptual evaluation of pathological voice quality: reliability and correlations with acoustic measurements. Rev Laryngol Otol Rhinol. 1996;117:219–224. [PubMed] [Google Scholar]
- 22.Gray H. Gray's Anatomy. The Anatomical Basis of Clinical Practice. 40th ed. Philadelphia: Ed. Churchill Livingstone/ Elsevier; 2008. [Google Scholar]
- 23.Miyaoka S, Hirano H, Miyaoka Y, et al. Head movement associated with performance of mandibular tasks. J Oral Rehabil. 2004;31:843–850. doi: 10.1111/j.1365-2842.2004.01387.x. [DOI] [PubMed] [Google Scholar]
- 24.Jaïs L, Grelet F. Influence de la position de la langue sur la posture. Etude en stabilométrie statique. In: Lacour M, editor. Contrôle postural: pathologies et traitements, innovations et rééducation. Marseille: Solal Editeurs; 2001. pp. 63–79. [Google Scholar]
- 25.Huche F. La voix: pathologie vocale. Paris: Masson; 1990. [Google Scholar]
- 26.Bricot B. La reprogrammation posturale global. Montpellier: Ed. Sauramps Medical; 1996. [Google Scholar]
- 27.Roll JP, Roll R. From eye to foot: a proprioceptive chain involved in postural control. In: Amblard B, Berthoz A, Clarac F, editors. Posture and gait: development adaptation and modulation. Amsterdam: Elsevier; 1988. pp. 155–164. [Google Scholar]
- 28.Lackner JR. Some proprioceptive influences on the perceptual representation of body shape and orientation. Brain. 1988;111:281–297. doi: 10.1093/brain/111.2.281. [DOI] [PubMed] [Google Scholar]
- 29.Gilman S. Joint position sense and vibration sense: anatomical organisation and assessment. J Neurol Neurosurg Psych. 2002;73:473–477. doi: 10.1136/jnnp.73.5.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nagakawa H, Ohashi N, Watanabe Y, et al. The contribution of proprioception to postural control in normal subjects. Acta Otolaryngol (Stockh) 1993;(Suppl 504):112–116. doi: 10.3109/00016489309128134. [DOI] [PubMed] [Google Scholar]
- 31.Yasuda T, Nagakawa T, Inoue H, et al. The role of the labyrinth, proprioception and plantar mechanosensor in the maintenance of an upright posture. Eur Arch Otorhinolaryngol. 1999;256:527–532. doi: 10.1007/pl00014149. [DOI] [PubMed] [Google Scholar]
- 32.Roll JP, Popov K, Gurfinkel V, et al. Sensorimotor and perceptual function of muscle proprioception in microgravity. J Vestib Res. 1993;3:259–273. [PubMed] [Google Scholar]
- 33.Wilson Arbleda BM, Frederick AL. Consideration for maintenance of postural alignment for voice production. J Voice. 2008;22:90–99. doi: 10.1016/j.jvoice.2006.08.001. [DOI] [PubMed] [Google Scholar]