Abstract
Background
Methadone-Maintained (MM) clients who engage in excessive alcohol use are at high risk for HIV and Hepatitis B virus (HBV) infection. Nurse-led Hepatitis Health Promotion (HHP) may be one strategy to decrease alcohol use in this population.
Objective
To evaluate the impact of nurse-led HHP, delivered by nurses compared to Motivational Interviewing (MI), delivered by trained therapists in group sessions or one-on-one on reduction of alcohol use.
Methods
A three-arm randomized, controlled trial, conducted with 256 MM adults attending one of five MM outpatient clinics in the Los Angeles area. Within each site, moderate-to-heavy alcohol-using MM participants were randomized into one of three conditions: 1) nurse-led hepatitis health promotion group sessions (n=87); 2) MI delivered in group sessions (MI-group; n=90), or 3) MI delivered one-on-one sessions (MI-single, n=79).
Results
Self-reported alcohol use was reduced from a median of 90 drinks/month at baseline to 60 drinks/month at six month follow-up. A Wilcoxon sign-rank test indicated a significant reduction in alcohol use in the total sample (p < .05). In multiple logistic regression analysis controlling for alcohol consumption at baseline and other covariates, no differences by condition were found.
Discussion
As compared to two programs delivered by MI specialists, a culturally-sensitive and easy to implement nurse-led HHP program produced similar reductions in alcohol use over six months. Employing nurse-led programs may allow cost savings for treatment programs as well as a greater integration of alcohol reduction counseling along with a more comprehensive focus on general health-related issues than previously conducted.
Keywords: Alcohol use, Methadone Maintained, Motivational Interviewing, nurse-led hepatitis health promotion
1.0 Introduction
Methadone-Maintained (MM) clients have reported excessive alcohol use; in fact, nearly 50% of this population has reported chronic alcohol consumption (Maremmani et al., 2007). Alcohol abuse has been associated with major health problems, including hepatic cirrhosis and hepatocellular carcinoma (Srivastava et al., 2008). Alcohol-abusing MM clients suffer from psychological impairments, including anxiety and feelings of low moods, and poor social functioning (Senbanjo et al., 2007). Alcohol use and abuse are also correlated with chronic drug use (Backmund et al., 2003); both types of substance use place individuals at risk for HIV and hepatitis (Arasteh et al., 2008). Moreover, among MM clients who have hepatitis C (HCV), reduction and/or elimination of alcohol drinking is an important treatment goal as it would decrease demand on liver enzymes and perhaps slow HCV disease progression.
To date, no studies exist which assess the impact of brief alcohol reduction among patients enrolled in methadone maintenance programs. Currently, the most popular intervention which has shown an impact on reducing alcohol use is Motivational Interviewing (MI), a ‘client-oriented counseling style’ that seeks to help clients ‘explore and resolve ambivalence’ to change (Miller and Rollnick, 2002). MI has been found to be an effective strategy in reducing alcohol use and abuse among a variety of populations, when delivered by therapists one-on-one or the less evaluated group approach (Deas, 2008; Peterson et al., 2006).
The impact of intervention directed at reducing alcohol use by health care providers who traditionally provide care and support is nevertheless of interest. In particular, nurses can have a significant potential to change behavior when interacting with addicts who are enrolled in methadone maintenance programs, as these environments provide an excellent arena for developing health promoting behaviors among high risk populations. While no research has been conducted that has focused on reducing alcohol use among the methadone population to date, nurse-led interventions have resulted in reduction of alcohol use among general hospitalized patients (Tsai et al., 2009) and among postpartum women (Fleming et al., 2008). Lock et al. (2006) believes that as one of the key roles of the nurse is to promote health, and nurses have a lower cost of employment than physicians, nurses are ideally suited to deliver brief alcohol interventions.
To date, there have been no studies specifically looking at the comparative efficacy of nurse-led intervention, nor MI, delivered either individually or in a group setting among adults receiving MM. The present study evaluates the efficacy of nurse-led Hepatitis Health Promotion (HHP) group sessions against the already established intervention MI. In addition, the study presents a unique opportunity to evaluate group MI compared to individual MI; the former of which possesses only a little, albeit growing, evidence for its efficacy compared to individual MI. Comparing these two MI interventions (Group vs individual) is also important because of the predominance of group therapy in substance abuse treatment and the fact that more studies are needed evaluating group therapy.
1.1 Theoretical Basis for Nurse-Led Intervention
The Comprehensive Health Seeking and Coping Paradigm (CHSCP; Nyamathi, 1989), originally adapted from Lazarus and Folkman’s (1984) stress and coping paradigm and Schlotfeldt’s (1981) health-seeking paradigm, proposes that a number of factors impact health outcomes of vulnerable populations with health disparities (Nyamathi et al., 2003; 2006; 2008). These factors include sociodemographic characteristics, personal and psychosocial resources and health behaviors, cognitive appraisal, coping responses, nursing strategies, and health outcomes. In this study, variables of interest include sociodemographic factors (age, ethnicity, gender, education, recruitment site), personal (physical health status factors), psychosocial factors (depressive symptomotology, poor emotional well being, social support) resources, type of intervention (MI-group, vs MI-single, vs Nurse-led HHP programs) and behavior (alcohol use, injection and non-injection drug use, traded sex, multiple partners, HBV vaccination initiation).
1.2 Nurse-Led Interventions
Several studies have demonstrated that nurse-led interventions seeking to reduce alcohol consumption among high-risk substance abusers are effective (Cummings et al., 2006; Flemming et al., 2008; Tsai et al., 2009). In a study a brief intervention delivered by nurses for problem drinkers in a Chinese hospitalized population, Tsai et al. (2009) revealed significant decreased alcohol scores at 12 month follow-up compared top a control group. Among a sample of 235 postpartum women screened as having “at-risk” drinking problem, the findings of a brief intervention offered by obstetric nurses revealed a significant reduction in mean number of drinks in the past 30 days, and number of drinking days and heavy drinking days in the past 30 days (Fleming et al., 2008).
These findings support the need for widespread screening and brief intervention for populations at risk for poor maternal-child outcome. In yet another nurse-delivered cluster-randomized controlled trial (Lock et al., 2006), no differences were found between the intervention and control groups. The authors contend that the high drop-out rate of over 50% may have resulted in lack of positive findings. These findings highlight the fact that nurse-led interventions have high potential for reducing substance use among at-risk populations and would be worthy of testing in a methadone-maintained population as well.
1.3 Motivational Interviewing
Although MI has been applied to various areas of health behavior change, including obesity, HIV risk factor modification and eating disorders, the broadest application of this approach has been in the area of addiction (Hettema et al., 2005). MI has been effective for the reduction of alcohol use among adults attending community health centers in Idaho (Beckham, 2007) and has been shown to effectively reduce illicit drug use among homeless adolescents (Peterson et al., 2006). Among college students, several studies have shown the effectiveness of MI in the reduction of drinking (Deas, 2008), particularly heavy drinking (Juarez et al., 2006; LaBrie et al., 2007a). However, MI has not consistently resulted in measurable improvement (Hettema et al., 2005). For example, in a recent study of homeless adolescents, MI was not associated with reduction of alcohol use (Baer et al., 2007).
Currently, there is a paucity of studies comparing outcomes when MI is delivered using individual versus group format for the management of alcohol abuse; moreover, the populations in which the studies have been conducted were quite disparate and mixed. Individually-delivered interventions using MI have been found most effective for the management of alcohol abuse among college students (Carey et al., 2007). However, brief, individual MI, delivered on a one-time basis to alcohol-abusing inpatients was not found to be associated with reductions in alcohol use (Saitz et al., 2007). Grenard et al. (2006) found that one-to-one sessions have been shown to be effective among adolescents and young adults engaged in drug-related behaviors. Group MI has also been shown to be effective in reducing alcohol use among both psychiatric inpatients with chemical dependence (Santa Ana et al., 2007) and female college students (LaBrie et al., 2007a). On the other hand, John et al. (2003) found no significant difference in amount of alcohol reduction when comparing individual to group MI among a group of alcohol-dependent inpatients.
The purpose of this trial is to evaluate the impact of a nurse-led hepatitis health promotion program in reducing alcohol use among participants receiving methadone maintenance, to an already established, empirically supported intervention (MI) and also to evaluate how the nursed-led HHP differs from either MI method.
2.0 Method
This study was a randomized controlled trial of a three-group intervention with 256 moderate and heavy alcohol-using adults receiving MM treatment in Los Angeles. After completion of a structured baseline questionnaire administered by trained research staff, all participants who self-reported moderate- to-heavy alcohol use were randomized into one of three programs: Motivational Interviewing -Single (MI-Single), Motivational Interviewing-Group (MI-Group), or Nurse-Led Hepatitis Health Promotion (HHP). MI sessions were delivered by two trained therapists specialized in the facilitation of MI. The Nurse-led HHP sessions were delivered by a research nurse in conjunction with a trained research staff member. Each program provided three sessions, as well as the HAV/HBV vaccination series for all those found to be HBV seronegative. Baseline data were collected from February 2007 to May 2008. Follow-up data were collected six months later.
2.1 Sample and Setting
MM clients met eligibility criteria if they had received methadone for at least three months, were 18–55 years of age, and reported moderate-to-heavy alcohol use based on questions from the Addiction Severity Index (ASI). Recruitment was conducted in five MM treatment sites in Los Angeles and Santa Monica. These sites included: Bay Area Addiction (BAART) clinics in the areas of Beverly, Southeast, and Lynwood, and non-BAART MM sites in Santa Monica (Matrix) and Southeast Los Angeles (TriCity).
2.2 Procedure
The study and associated materials were approved by the Human Subject Protection Committee. In addition, this study is registered with clinicaltrials.gov, registration #NCT00926146. Upon obtaining written permission from the directors to collect data at the selected sites, participants were recruited by means of posted flyers. For those interested, after informed consent for the screening had been read and signed in a private room in the sites, the outreach workers administered a brief two-minute structured questionnaire composed of socio-demographic characteristics, a screen for alcohol use and severity, and a hepatitis-related health history.
After the initial screening was completed, detailed information was provided about the study to eligible persons and a second-level consent for blood testing was requested. MM clients who met eligibility criteria and wished to participate further completed a third consent form prior to enrollment into the study.
2.3 Measures
Socio-Demographic information, collected by a structured questionnaire, included age, gender, birthdate, ethnicity, education, childhood physical abuse, history of substance abuse treatment, and history of trading sex lifetime.
HBV Vaccination Status was measured as receipt of any dose of the Twinrix vaccine. Although the vaccination was not expected to directly influence alcohol reduction, extra time and attention were required to administer it.
Perceived Health Status was measured on a 5-point scale from “excellent” to “poor” and a dichotomous item inquired about past six-month hospitalization. Health status was dichotomized at fair/poor versus better health.
Depressive Symptoms were assessed with the Center for Epidemiological Studies Depression (CES-D) scale (Radloff, 1977) and has been validated for use in homeless populations (Nyamathi et al., 2006; 2008). The 10-item self-report instrument is designed to measure depressive symptomology in the general population (Andresen et al., 1994) and measures the frequency of a symptom on a 4-point response scale from 0 “Rarely or none of the time (Less than 1 day)” to 4 “All of the time (5–7 days)”. Scale scores were dichotomized at a cutoff value of 8, a frequently used figure to suggest depressive symptomatology. The internal reliability of the scale in this sample was .80.
Emotional Well-Being was measured by the five-item mental health index (MHI-5); this scale has well-established reliability and validity (Stewart et al., 1988). Scores were linearly transformed so that they ranged from 0 to 100. A cut-point of 66 (Rubenstein et al., 1989) was used to discriminate participants’ emotional well-being. Cronbach’s alpha for the scale in this study was .79.
Social Support was measured by a 9-item scale used in the RAND Medical Outcomes Study (Sherbourne and Stewart, 1991). The items elicited information about how often respondents had friends, family or partners available to provide them with food, a place to stay, etc, on a five-point Likert scale. The instrument has demonstrated high convergent and discriminant validity; internal consistency reliability coefficients range from 0.91 to 0.97 for the subscales (Sherbourne and Stewart, 1991). Cronbach’s alpha for the scale in this study was .94. An additional question inquired about whether social support came primarily from drug users, non-drug users or both.
For this study, alcohol use was assessed by the Time Line Follow Back that assessed the number of standard drinks consumed per day over the last 30 days.
Drug use was measured by the Addiction Severity Index – Lite Version. This measure is a shortened version of the ASI (5th edition – McClellan et al., 1992). Drug use was dichotomized at its median for clarity of presentation in this study.
2.4 Intervention
Nurse-Led Hepatitis Health Promotion (HHP) Program. At baseline, a nurse and Hepatitis-trained research assistant conducted three time-equivalent (60 minute) HHP group sessions. These staff were well trained on the integration of the CHSCP into their education delivery. Each session was spaced two weeks apart; thus, the three sessions were delivered within six weeks of entry into the program. The average number of participants was six; however groups ranged from 5–7 in number.
The HHP sessions focused on hepatitis education, specifically, the progression of HCV infection and the culturally-sensitive strategies that infected individuals can adopt to prevent or reduce accumulated damage to liver functioning. Utilizing the principles of the CHSCP, this intervention by nursing integrated strategies which included discussing the dangers of alcohol use on hepatitis (cognitive factors), discussing ways to avoid alcohol and other drugs, eating a balanced diet, dangers of reinfection of HCV by resuming injection drug use (IDU), receiving unsafe tattoos and body piercing, having unprotected sexual behavior, and being consistent in engaging in other health-related behaviors, such as regular medical check-ups (behavioral factors). Additional health promoting activities included strategies in enhancing coping (coping factors), such as seeking social support of a positive nature, getting support from religion and building self esteem (personal and psychosocial factors) when afflicted with a history of drug and alcohol addiction. The HHP program was directed by a detailed protocol to maintain fidelity of the program and prevent the HHP team from moving into MI-type approaches. While the didactic delivery style was utilized, the sessions were interactive as the group raised questions about the content.
Motivational Interviewing Program (Individual vs Group). After completion of the baseline questionnaire, eligible participants randomized into the MI group were offered three, 60-minute sessions that were delivered (one-on-one or via group format) by trained MI specialists with the same delivery timing and number of clients in the group session as the HHP sessions. The MI specialists included a PhD-prepared psychologist who conducted primarily the MI-group sessions and a MSW-prepared researcher who conducted primarily the individual MI sessions. The psychologist was trained by experts in MI and has had over 15 years experience in facilitating MI in clinical practice with drug addicted clients. The MSW-prepared researcher had over two years training in MI facilitation by a MI-trained psychologist. MI sessions included MI spirit (e.g., collaboration, evocation, autonomy), MI principles (e.g., empathy, rolling with resistance, developing discrepancy, enhancing self-efficacy) and MI microskills (e.g., eliciting change talk, reflections and affirmations). MI sessions were focused on exploring the impact alcohol use had on health and risky behaviors, and working through ambivalence to reduce alcohol use while focusing on subsequent life goals. Content in the group vs one-on-one MI sessions were identical and the delivery of each session was guided by a detailed protocol and bi-weekly meetings with the investigator and therapists which enhanced treatment adherence and fidelity by the therapists. The sessions were open; thus allowing participants who had not completed their three sessions with their original cohort to complete with a later cohort.
Regardless of group, both HHP and MI Single or Group sessions were preceded by a needs assessment and included referrals and appointments as needed for medical and mental health services. All participants received a small incentive for each of three sessions ($5); and a Local Community Resource Guide. For both HHP and MI programs, subsequent to the sessions, the three-series HAV/HBV vaccine was administered by the research nurse, if the participant was eligible for the vaccine (HBV sero-negative and no history of allergies) and desired to be vaccinated. All participants also received referrals to 12-step alcohol treatment programs in the community. Moreover, participants were notified to return for their six-month follow-up questionnaire and the last vaccine dose, for those receiving the vaccine series.
2.5 Data Analysis
All analyses were intent-to-treat. The primary outcome was at least 50% reduction in alcohol use by six-month follow-up. Additionally, we examined abstinence from alcohol use at six months. Preliminary analyses, including chi-square tests, t tests, analysis of variance and correlations, were used to assess comparability of the three programs at baseline and to examine unadjusted correlates of a 50% or greater reduction in alcohol use. Multiple logistic regression modeling was used to assess program effects on 50% alcohol reduction, controlling for potential confounders. Six people reporting no alcohol use at baseline, despite moderate-to-heavy alcohol use on the screener were excluded from this analysis; as were a few participants with mixed or “other” ethnicity. Stepwise backward multiple logistic regression analysis was used to create a model of alcohol reduction; predictors included variables that were associated with 50% alcohol use reduction at the 0.15 level in preliminary analyses. Indicators for MI-single and MI-group assignment and baseline alcohol use, categorized into quartiles due to non-normality, were included in all models; other covariates were retained if they were significant at the .10 level.
Multicollinearity was assessed and model fit was examined with the Hosmer-Lemeshow test. More specifically, we addressed the lack of independence by using the “fixed effects approach to clustering”, as recommended by Snijders and Bosker (1999), among others, when the number of clusters (sites) is small (e.g., <10). To control for differences among the means of the 5 sites, we tested dummy variables for 4 of the sites in a final regression model. Since the results did not differ substantively, we present the more parsimonious model. Statistical analyses were performed with SAS/STAT.
3.0 Results
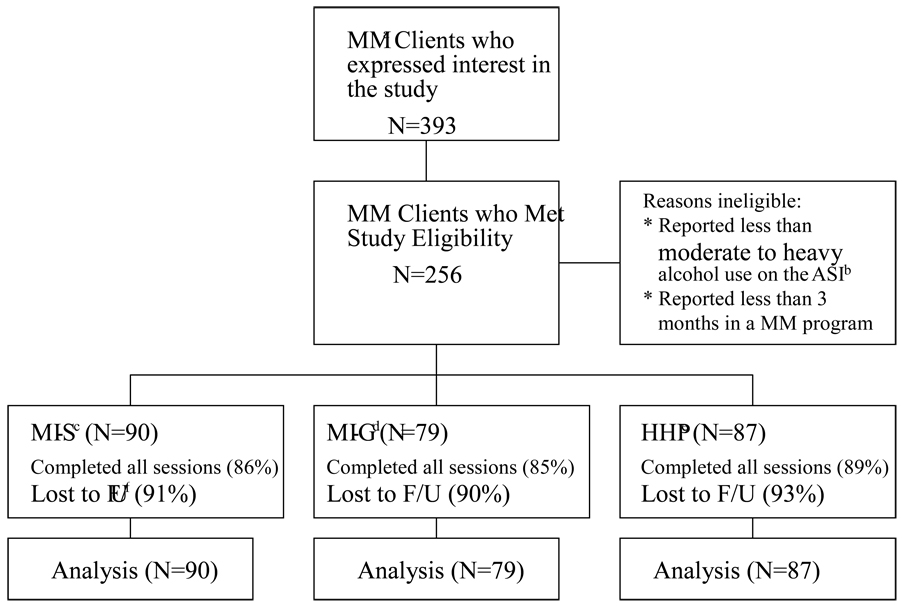
Compilation of the sample is as described in Table 1. A total of 256 MMT participants were randomized into the MI-S (n = 90), MI-G (n = 79) or Nurse-led HHP (n = 87) group. A few participants (n = 6) reported no alcohol use in the past month at baseline. As shown on Table 1, more than half the sample (59%) was male and predominantly African American (45%) or Latino (27%). About one-third of participants received social support from both drug-users and non-drug users, while almost half reported social support from primarily non drug users. A total of 86.7% of participants completed all three sessions and 91.3% completed the six month follow-up (Figure 1).
Table 1.
Baseline Sample Characteristics of Methadone Maintained Clients by Program
| Characteristics | ||||||||
|---|---|---|---|---|---|---|---|---|
| MI-Single | MI-Group | HHP | Total | |||||
| (N = 90) | (N = 79 ) | (N = 87 ) | (N = 256 ) | |||||
| Background | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Mean Age | 51.9 | (7.9) | 50.0 | (7.4) | 51.8 | (8.8) | 51.2 | (8.4) |
| % | % | % | % | |||||
| Male | 60.0 | 58.2 | 59.3 | 59.2 | ||||
| Ethnicity: | ||||||||
| African American | 46.7 | 44.3 | 44.2 | 45.1 | ||||
| White | 21.1 | 24.1 | 11.6 | 18.8 | ||||
| Latino | 25.6 | 25.3 | 29.1 | 26.7 | ||||
| Other | 6.7 | 6.3 | 15.1 | 9.4 | ||||
| High School Grad | 62.2 | 59.5 | 52.3 | 58.0 | ||||
| Partnered | 51.7 | 55.7 | 55.8 | 54.3 | ||||
| Employed | 18.0 | 12.7 | 20.9 | 17.3 | ||||
| Recruitment Site: | ||||||||
| Beverly | 16.9 | 21.8 | 23.8 | 20.7 | ||||
| Southeast | 31.5 | 37.2 | 28.6 | 32.3 | ||||
| Lynwood | 9.0 | 9.0 | 8.3 | 8.8 | ||||
| Matrix | 28.0 | 23.1 | 23.8 | 24.7 | ||||
| TriCity | 15.7 | 9.0 | 15.7 | 13.6 | ||||
| Fair/poor health | 58.9 | 63.3 | 59.3 | 60.4 | ||||
| Childhood Physical Abuse | 23.3 | 27.9 | 24.4 | 25.1 | ||||
| Lifetime Trade Sex | 31.8 | 46.7 | 32.9 | 36.7 | ||||
| Substance Use | ||||||||
| Recent +Alcohol Use at Baseline |
||||||||
| 0–40++ | 23.3 | 27.9 | 24.4 | 25.1 | ||||
| 41–89 | 21.1 | 22.8 | 30.2 | 24.7 | ||||
| 90–180 | 32.2 | 22.8 | 24.4 | 26.7 | ||||
| > 180 | 23.3 | 26.6 | 20.9 | 23.5 | ||||
| Recent+ marijuana use | 17.8 | 25.3 | 5.8 | 16.0 | ||||
| Recent+ IDU | 37.8 | 45.6 | 37.2 | 40.0 | ||||
| Smoke ≥ 1 pack/day | 52.2 | 64.6 | 52.3 | 56.1 | ||||
| Recent+ Self-Help | 23.3 | 25.3 | 15.1 | 21.2 | ||||
| Program | ||||||||
| ≥ 50% reduction in alcohol use at six months |
46.6 | 54.0 | 49.4 | 49.8 | ||||
| No recent+ alcohol use at six months |
22.2 | 20.3 | 23.3 | 22.0 | ||||
| Psychological Resources | ||||||||
| Depressive Sxsa | 81.1 | 81.1 | 80.2 | 80.8 | ||||
| Poor Emotional Well | 73.3 | 65.8 | 62.8 | 67.5 | ||||
| Beingb | ||||||||
| Social Support From: | ||||||||
| Primarily Drug Users | 7.8 | 12.7 | 17.4 | 12.6 | ||||
| Primarily Non Drug | 51.1 | 45.6 | 48.8 | 48.6 | ||||
| Users | ||||||||
| Both | 34.4 | 38.0 | 32.6 | 34.9 | ||||
| No One | 6.7 | 3.8 | 1.2 | 3.9 | ||||
recent refers to past month
denotes number of drinks consumed over the last 30 days
Based on a CES-D short form (10 items) score of 8 or more
Based on a score of 65 or less on a 0–100 scale
Figure 1.
Description of the Sample. a. Methadone Maintained. b. Alcohol Severity Index. c. Motivational Interviewing – Single. d. Motivational Interviewing – Group. e. Nurse-led Hepatitis Health Promotion. f. Follow-up.
At baseline, half of the sample reported 90 standard alcoholic drinks or more in the past month. In terms of drug use, 40% reported current IDU; only about one in five reported attending recent self-help programs. There were no group differences in subject characteristics at baseline with respect to program type. Health and health behaviors in this sample were found to be suboptimal. One quarter of the sample reported physical abuse in childhood and over a third said they had participated in sex trade. Symptoms of mental illness were common, with 80% reporting depressive symptoms and over two-thirds reporting poor emotional well being.
3.1 Alcohol Use Reduction
As shown in Table 1, about half the sample reported at least a 50% reduction in alcohol use and slightly more than one in five reported no alcohol use at six month follow-up. However, there were no statistically significant condition differences in either 50% reduction in alcohol use or abstinence from alcohol at six months follow-up. Compared to their counterparts who failed to reduce alcohol use by 50%, those who were able to reduce successfully were more likely to be African American (40% vs 52%, p < .05) and more likely to be the highest quartile of baseline drinking (14% vs 35%, p < .001) (Table 2).
Table 2.
Associations between Baseline Characteristics and Reduction of Alcohol Use by At Least 50%
| Characteristic | 50% Reduction in Drinking | |||
|---|---|---|---|---|
| No | Yes | |||
| (N = 126) | (N = 124) | |||
| Background | ||||
| Mean Age (SD) | 51.5 | 8.3 | 50.0 | 8.6 |
| Male | 65.1 | 53.2 | ||
| Ethnicity* | ||||
| African American | 39.7 | 51.6 | ||
| White | 18.3 | 18.6 | ||
| Latino | 29.4 | 24.2 | ||
| Other | 12.7 | 5.7 | ||
| High School Grad | 54.8 | 62.9 | ||
| Employed | 17.6 | 16.9 | ||
| Recruitment Site: | ||||
| Beverly | 24.8 | 14.1 | ||
| Southeast | 29.6 | 35.5 | ||
| Lynwood | 11.2 | 7.4 | ||
| Matrix | 22.4 | 27.3 | ||
| TriCity | 12.0 | 15.7 | ||
| Fair/poor health | 55.4 | 61.8 | ||
| Childhood Physical Abuse | 20.6 | 28.2 | ||
| Lifetime Traded Sex | 31.8 | 41.5 | ||
| Alcohol-Abusing | 38.4 | 41.1 | ||
| Partner | ||||
| Drug-Abusing Partner | 33.9 | 25.0 | ||
| Quartiles for Baseline Alcohol Use*** |
||||
| 0–40 | 27.0 | 20.2 | ||
| 41–89 | 31.0 | 19.4 | ||
| 90–180 | 28.6 | 25.8 | ||
| > 180 | 13.5 | 34.7 | ||
| Baseline ASI Drug High | 31.5 | 33.1 | ||
| Recent Marijuana use | 19.8 | 11.3 | ||
| Recent + IDU | 43.7 | 35.5 | ||
| Recent+ Self-help Prog | 19.8 | 22.6 | ||
| Smoke ≥ 1 pack/day | 50.0 | 61.1 | ||
| Multiple Sex Partners | 20.6 | 16.9 | ||
| Psychosocial Resources | ||||
| Depressive Sxs | 13.6 (6.3) | 12.9 (6.0) | ||
| Emotional Well-Being | 49.7 (24.1) | 54.5 (21.5) | ||
| Social Support | ||||
| Primary Drug User | 14.3 | 5.7 | ||
| Primary Non Drug | 45.2 | 52.4 | ||
| User | ||||
| Both | 37.3 | 33.1 | ||
| No one | 3.2 | 4.8 | ||
| Completed Vaccine | 64.1 | 74.4 | ||
recent refers to past six-month period
p < .05, chi-square or t test
p < .01, chi-square or t test
3.2 Multivariate Results
Adjusting for potentially confounding characteristics did not affect the preliminary findings of no condition differences in alcohol reduction (Table 3). Baseline alcohol use was the most important correlate of 50% alcohol reduction. Women had greater odds of reducing their alcohol use by at least 50% than men. More education and having received at least one dose of the HBV vaccine, with concomitant time and attention, were also associated with alcohol use reduction. Participants with drug-using partners and those who reported using marijuana on at least two days in the last 30 had lower odds of 50% alcohol reduction than their counterparts.
Table 3.
Logistic Regression Results for 50% Reduction of Alcohol Use (N = 249)
| Adjusted Odds Ratio | 95% CI | P Value | |
|---|---|---|---|
| Intervention Programs (vs HHP) | |||
| MI-Single | 0.91 | 0.47, 1.73 | .765 |
| MI-Group | 1.53 | .76, 3.09 | .231 |
| Female | 1.95 | 1.11, 3.44 | .021 |
| Education | 1.16 | 1.00, 1.33 | .045 |
| Baseline Alcohol Use | 1.68 | 1.30, 2.17 | .001 |
| Drug-Using Partner | 0.56 | 0.30, 1.02 | .058 |
| Recent+ Marijuana Use | 0.34 | 0.14, 0.80 | .013 |
| HBV Vaccination | 1.84 | 1.06, 3.18 | .013 |
recent refers to the past month
4.0 Discussion
As a result of high rates of chronic consumption of alcohol use among methadone maintained persons, the need to assess programs which focus on brief alcohol reduction at the program site is great. This study was designed to study the effectiveness of a nurse-led intervention as compared to an already established intervention, MI. In addition, this study presented a unique opportunity to evaluate group MI compared to individual MI, as little is known of the efficacy of group MI when compared to the larger evidence base that individual MI possesses. Comparing these two MI interventions is also important because of the predominance of group therapy in substance abuse treatment and that more studies are needed evaluating group MI.
The major finding of this study was that all three interventions resulted in significant reductions in drinking behavior at six-month follow-up. Specifically, over a six-month period of intervention, about half of the total sample reported at least a 50% reduction in alcohol use and about 20% reported no alcohol use at six month follow-up. There were no significant differences found among treatment groups with respect to drinking reduction. While MI has been shown to be effective for the management of problem drinking among college students (Deas, 2008; White et al., 2007; LaBrie et al., 2007b), and homeless persons (Baer et al., 2007; Peterson et al., 2006), we found no evidence of differential efficacy of one-on-one vs group-delivered MI over a nurse-led intervention in reducing alcohol drinking. Nurse-led interventions have been found to be effective for the management of alcohol-related problems among adults (Lock et al., 2006; Smith et al., 2003). Although there have been no studies designed to investigate the effectiveness of the same intervention, delivered by different practitioners such as nurses, physicians, social workers or clinical psychologists (Finfgeld-connett, 2005), Littlejohn and Holloway (2008) believe that nursing interventions are highly warranted for the prevention of alcohol abuse.
Our study also showed that MI, delivered by trained therapists, either in group sessions or via one-on-one sessions did not differ in effectiveness from each other, and neither were more effective than a nurse-led HHP program, for the reduction of alcohol use. While there is a paucity of studies which have examined relative effect of one-to-one MI sessions compared to group MI sessions, both methods have been found to be effective in the management of alcohol abuse. In particular, one-to-one MI has been shown to be an effective intervention among medical inpatients (Saitz et al, 2007), and group MI has been found to be beneficial among college women (LaBrie et al, 2007a) and psychiatric inpatients (Santa Ana et al., 2007). However, the majority of trials have compared MI (delivered in a group or on a one-to-one basis) to other interventions such as cognitive behavioral therapy, and therapies based on social-cognitive, self-regulation, and self-determination theories (Carey et al., 2007). To date, we do not know of any study comparing one-to-one MI with group MI in the management of problem drinking for methadone maintained clients. Moreover, no studies have compared these two types of MI delivery styles with nurse-led programs. Our study is the first to compare MI delivery (one-to-one versus group) with a nurse-led intervention. As the nurse-led HHP sessions were found to be as effective as MI sessions, further studies of the efficacy and cost-effectiveness of nurse-led management of problem alcohol use is highly warranted.
We also found that African Americans were more likely to reduce alcohol consumption by at least 50% compared to their ethnic counterparts. While ethnic differences were not previously reported among MM populations who attempted to reduce their alcohol consumption, these findings are consistent with those from a study which showed that African American college students more regularly employed drinking reduction strategies (with the exception of choosing a designated driver), compared with White college students (Siebert et al., 2003). Further investigation is warranted to assess whether ethnic differences are important in enabling further reduction of alcohol among a diverse sample of MM clients.
Logistic regression findings revealed that heavier alcohol drinkers were more likely to reduce alcohol use by 50%. Our results are concordant with those reported by Walton et al. (2008) where participants who were most ready to reduce their alcohol intake had higher pre-intervention alcohol intake, compared with those who consumed less. Clearly, participants who used higher amounts may have been more able to reduce alcohol use rather than to stop drinking completely. However, among individuals affected by or at high risk for hepatitis, total cessation of alcohol use is recommended. Thus, strategies to enhance the cessation of any amount of alcohol use is needed.
Our results also showed that being female and having higher levels of education were associated with greater reduction in alcohol consumption. Consistent with other findings, males have been found to be higher consumers of alcohol compared with women (Livingston and Room, 2009). While there are no studies showing that females respond more effectively than males to MI therapy, or to nurse-led interventions in the management of alcohol abuse, gender differences have been found with respect to the risk factors and consequences of alcohol abuse (Nolen-Hoeksema, 2004). Men and women with histories of abuse (sexual, emotional or physical) have also been found to experience different rates of recovery, with respect to substance abuse treatment (Branstetter et al., 2008). We believe that the results of our study, in conjunction with the findings from the studies cited above, suggest that women may respond differently to therapy than men.
Another important finding was that participants who had one or more of the three series Twinrix hepatitis vaccine were more likely to reduce alcohol use by at least 50%. While this finding has never been reported in the literature, we believe that the extra time and attention taken to explain the vaccine and to administer the injection was an important factor resulting in alcohol reduction. Kaminer et al (2008) reported that programs of aftercare, which consisted of multiple in-person or telephonic follow-up slowed post-treatment relapse among adolescents. Programs of aftercare and interventions such as ours, both involve extra time and attention on the part of therapists and this may lead to better client outcomes.
In our study, recent marijuana users were least likely to reduce alcohol use. This is consistent with the findings from another study showing that alcohol use, in conjunction with marijuana use, was associated with poorer outcomes, compared with alcohol use alone (Rhodes et al., 2008).
One study limitation was that our interventions, one-to-one MI, group-MI, and a nurse-led hepatitis prevention program were delivered by a heterogeneous group of practitioners. The internal validity of our study could have been enhanced if we compared nurse-led MI to nurse-led hepatitis prevention. Another study limitation was the fact that we recruited volunteers into our study who may have been motivated for treatment as well as used self-report to measure treatment effect. Self-report can be subject to bias which may threaten the validity of the study. Finally, while we did not audio-tape the sessions or utilize a checklist to assess for fidelity, a detailed treatment protocol was followed and bi-weekly meetings were held with the investigator and therapists throughout the study to provide feedback and supervision to maintain the treatment protocol and its delivery.
In summary, this study is the first to compare nurse-led HHP to two methods of MI (one-to-one and group) for the management of problem drinking, among people undergoing MM therapy. All three interventions resulted in significant reductions in alcohol drinking behavior. Implications of employing MI group vs MI individual clearly may result in cost savings for treatment programs. More importantly, employing nurse-led programs may not only allow cost savings as well but also allow a greater integration of alcohol reduction counseling along with a more comprehensive focus on general health-related issues than previously conducted. It has been suggested that nurses can play a significant role in management of alcohol abuse (Littlejohn and Holloway, 2008). We have been able to demonstrate that nurses can be as effective as other practitioners in the management of excessive alcohol use. We believe that further studies of the efficacy and cost-effectiveness of nurse-led management of problem alcohol use is highly warranted.
Acknowledgements
The authors would like to thank Cindy James for her assistance with the manuscript preparation.
Role of Funding:
Funding for this study was provided by NIAAA Grant AA015759. The NIAAA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors:
Barbara Greengold and Steve Shoptaw contributed to writing the review of literature and introduction. Adeline Nyamathi, and Mary Marfisee contributed to the methods and discussion. Allan Cohen, Kamala Nyamathi, Viviane de Castro and Daniel George contributed to the editing and final review of the manuscript. Barbara Leake provided the statistical analysis. All authors approved the final paper.
Conflict of Interest:
All authors declare that they have no conflicts of interest.
Contributor Information
Adeline Nyamathi, University of California, Los Angeles, School of Nursing, 2-250 Factor, Box 951702, Los Angeles, CA 90095-1702, (310) 825-8405, (310) 206-7433, anyamath@sonnet.ucla.edu.
Steven Shoptaw, University of California, Los Angeles, Department of Family Medicine and Psychiatry, 10880 Wilshire Blvd., Los Angeles, CA 90095-7087, (310) 794-0619x225, sshoptaw@mednet.ucla.edu.
Allan Cohen, Director of Research and Training, Bay Area Addiction, Research and Treatment, Inc., 1926 W. Beverly Blvd. Los Angeles, CA 90057, (213) 607-0210, (310) 607-1434, allanjcohen@aol.com.
Barbara Greengold, University of California, Los Angeles, School of Nursing, 3-133 Factor, Box 956917, Los Angeles, CA 90095-6917, (310) 794-4814, (310) 267-0413, Barby3ann@yahoo.com.
Kamala Nyamathi, University of California, Davis, School of Medicine, One Shields Avenue, Davis, California 95616.
Mary Marfisee, University of California, Los Angeles, David Geffen School of Medicine, 1920 Colorado Avenue, Los Angeles, CA 90095-7087, (818) 947-4095, mmarfisee@mednet.ucla.edu.
Viviane de Castro, University of California, Los Angeles, School of Nursing, 3-133 Factor, Box 956917, Los Angeles, CA 90095-6917, (310) 794-4814, (310) 267-0413, viviane.pecanha@yahoo.com.
Farinaz Khalilifard, University of California, Los Angeles, School of Nursing, 3-133 Factor, Box 956917, Los Angeles, CA 90095-6917, (310) 794-4814, (310) 267-0413, farinazfard@yahoo.com.
Daniel George, Director, Matrix Institute on Addictions, 12304 Santa Monica Blvd., Los Angeles, CA 90025, ddgeorge_74@yahoo.com.
Barbara Leake, University of California, Los Angeles, School of Nursing, 3-669 Factor, Box 956917, Los Angeles, CA 90095-1702, Barbara@ucla.edu.
References
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short-form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- Arasteh K, Des Jarlais DC, Perlis T. Alcohol and HIV sexual risk behaviors among injection drug users. Drug Alcohol Depend. 2008;95:54–61. doi: 10.1016/j.drugalcdep.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backmund M, Schutz CG, Meyer K, Eichenlaub D, Soyka M. Alcohol consumption in heroin users, methadone-substituted and codeine-substituted patients- Frequency and correlates of use. Eur Addict Res. 2003;9:45–50. doi: 10.1159/000067733. [DOI] [PubMed] [Google Scholar]
- Branstetter SA, Bower E, Kamien J, Amass L. A history of sexual, emotional, or physical abuse predicts adjustment during opioid maintenance treatment. J Subst Abuse Treat. 2008;34:208–214. doi: 10.1016/j.jsat.2007.03.009. [DOI] [PubMed] [Google Scholar]
- Baer JS, Garrett SB, Beadnell B, Wells E, Peterson PL. Brief motivational intervention with homeless adolescents: evaluating effects on substance use and service utilization. Psych Addict Behav. 2007;21(4):582–586. doi: 10.1037/0893-164X.21.4.582. [DOI] [PubMed] [Google Scholar]
- Beckham N. Motivational interviewing with hazardous drinkers. J Am Acad Nurse Pract. 2007;19:103–110. doi: 10.1111/j.1745-7599.2006.00200.x. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon L, Carey M, Demartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addict Behav. 2007;32(11):2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings GE, Francescutti LH, Predy G, Cummings G. Health promotion and disease prevention in the emergency department: a feasibility study. Can J Emerg Med. 2006;8(2):100–105. doi: 10.1017/s1481803500013543. [DOI] [PubMed] [Google Scholar]
- Deas D. Evidence-based treatments for alcohol use disorders in adolescents. Pediatrics. 2008;121 Suppl. 4:S348–S354. doi: 10.1542/peds.2007-2243G. [DOI] [PubMed] [Google Scholar]
- Finfgeld-connett D. Alcohol brief interventions. Ann Rev Nurs Res. 2005;23:363–388. [PubMed] [Google Scholar]
- Fleming MF, Lund MR, Wilton G, Landry M, Scheets D. The healthy moms study: The efficacy of brief alcohol intervention in postpartum women. Alcohol Clin Exp Res. 2008;32(9):1600–1606. doi: 10.1111/j.1530-0277.2008.00738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grenard JL, Ames SL, Pentz M, Sussman S. Motivational interviewing with adolescents and young adults for drug-related problems. Int J Adolesc Med Health. 2006;18(1):53–67. doi: 10.1515/ijamh.2006.18.1.53. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller W. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- John U, Veltrup C, Driessen M, Wetterling T, Dilling H. Motivational intervention: an individual counseling vs. a group treatment approach for alcohol-dependent in-patients. Alcohol Alcohol. 2003;38(3):263–269. doi: 10.1093/alcalc/agg063. [DOI] [PubMed] [Google Scholar]
- Juarez P, Walters ST, Daugherty M, Radi C. A randomized trial of motivational interviewing and feedback with heavy drinking college students. J Drug Educ. 2006;36(3):233–246. doi: 10.2190/753N-8242-727T-G63L. [DOI] [PubMed] [Google Scholar]
- Kaminer Y, Burleson JA, Burke RH. Efficacy of outpatient aftercare for adolescents with alcohol use disorders: A randomized controlled study. J Am Acad Child Adolesc Psychiatry. 2008;47(12):1405–1412. doi: 10.1097/CHI.0b013e318189147c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Thompson AD, Huchting K, Lac A, Buckley K. A group motivational interviewing intervention reduces drinking and alcohol-related negative consequences in adjudicated college women. Addict Behav. 2007a;32:2549–2562. doi: 10.1016/j.addbeh.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Pedersen ER, Lamb TF, Quinlan T. A campus-based motivational enhancement group intervention reduces problematic drinking in freshmen male college students. Addict Behav. 2007b;32:889–901. doi: 10.1016/j.addbeh.2006.06.030. [DOI] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. pp. 117–180. [Google Scholar]
- Littlejohn C, Holloway A. Nursing interventions for preventing alcohol-related harm. Subst Misuse. 2008;17(1):53–59. doi: 10.12968/bjon.2008.17.1.28062. [DOI] [PubMed] [Google Scholar]
- Livingston M, Room R. Variations by age and sex in alcohol-related problematic behavior per drinking volume and heavier drinking occasion. Drug Alcohol Depend. 2009;101:169–175. doi: 10.1016/j.drugalcdep.2008.12.014. [DOI] [PubMed] [Google Scholar]
- Lock C, Kaner E, Heather N, Doughty J, Crawshaw A, McNamee P, Purdy S, Pearson P. Effectiveness of nurse-led brief alcohol intervention: a cluster randomized controlled trial. J Adv Nurs. 2006;54:426–439. doi: 10.1111/j.1365-2648.2006.03836.x. [DOI] [PubMed] [Google Scholar]
- Maremmani I, Pani PP, Mellini A, Pacini M, Marini G, Lovrecic M, Perugi G, Shinderman M. Alcohol and cocaine use and abuse among opioid addicts engaged in a methadone maintenance treatment program. J Addict Dis. 2007;26(1):61–70. doi: 10.1300/J069v26n01_08. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- McClellan AT, Kushner H, Metzger D, Peters R, Smith L, Grissom G, Pettinati H, Argerious M. The fifth edition of the addiction severity index. J Subst Abuse Treat. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in risk factors and consequences for alcohol use and problems. Clin Psych Rev. 2004;24:981–1010. doi: 10.1016/j.cpr.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Nyamathi A. Comprehensive health seeking and coping paradigm. J Adv Nurs. 1989;14:281–290. doi: 10.1111/j.1365-2648.1989.tb03415.x. [DOI] [PubMed] [Google Scholar]
- Nyamathi A, Christiani A, Nahid P, Gregerson P, Leake B. A randomized controlled trial of two treatment programs for homeless adults with latent tuberculosis infection. Int J Tuberc Lung Dis. 2006;10(7):775–782. [PubMed] [Google Scholar]
- Nyamathi A, Nahid P, Berg J, Burrage J, Christiani A, Aqtash S, Morisky D, Leake B. Efficacy of nurse case-managed intervention for latent tuberculosis among homeless subsamples. Nurs Res. 2008;57(1):33–39. doi: 10.1097/01.NNR.0000280660.26879.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Stein J, Dixon E, Longshore D, Galaif E. Predicting positive attitudes about quitting drug and alcohol use among homeless women. Psych Addict Behav. 2003;17(1):32–41. doi: 10.1037/0893-164x.17.1.32. [DOI] [PubMed] [Google Scholar]
- Peterson PL, Baer JS, Wells E, Ginzler JA, Garrett SB. Short-term effects of a brief motivational intervention to reduce alcohol and drug risk among homeless adolescents. Psych Addict Behav. 2006;20(3):254–264. doi: 10.1037/0893-164X.20.3.254. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rhodes WA, Peters RJ, Perrino CS, Bryant S. Substance use problems reported by historically Black college students: combined marijuana and alcohol use versus alcohol alone. J Psychoactive Drugs. 2008;40(2):201–205. doi: 10.1080/02791072.2008.10400631. [DOI] [PubMed] [Google Scholar]
- Rubenstein LV, Calkins DR, Young RY, Cleary P, Fink A, Kosecoff J, Jette AM, Davies AR, Delbanco TL, Brook RH. Improving patient function: A randomized trial of functional disability screening. Ann Intern Med. 1989;111:836–842. doi: 10.7326/0003-4819-111-10-836. [DOI] [PubMed] [Google Scholar]
- Saitz R, Palfai T, Cheng DM, Horton NJ, Freedner N, Dukes K, Kraemer KL, Roberts MS, Guerriero RT, Samet JH. Brief intervention for medical inpatients with unhealthy alcohol use: a randomized, controlled trial. Ann Intern Med. 2007;146:167–176. doi: 10.7326/0003-4819-146-3-200702060-00005. [DOI] [PubMed] [Google Scholar]
- Santa Ana E, Wulfert E, Nietert PJ. Efficacy of group motivational interviewing (GMI) for psychiatric inpatients with chemical dependence. J Consult Clin Psych. 2007;75(5):816–822. doi: 10.1037/0022-006X.75.5.816. [DOI] [PubMed] [Google Scholar]
- Schlotfeldt R. Nursing in the future. Nursing Outlook. 1981;29:295–301. [PubMed] [Google Scholar]
- Senbanjo R, Wolff K, Marshall J. Excessive alcohol consumption is associated with reduced quality of life among methadone patients. Addiction. 2007;102:257–263. doi: 10.1111/j.1360-0443.2006.01683.x. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Siebert DC, Wilke DJ, Delva J, Smith MP, Howell R. Differences in African American and White college student’s drinking behaviors: consequences, harm reduction strategies, and health information sources. J Am College Health. 2003;52(3):123–129. doi: 10.1080/07448480309595734. [DOI] [PubMed] [Google Scholar]
- Snijders T, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. London: Sage; 1999. [Google Scholar]
- Srivastava A, Kahan M, Ross S. The effect of methadone maintenance treatment on alcohol consumption: A systematic review. J Subst Abuse Treat. 2008;34:215–223. doi: 10.1016/j.jsat.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Smith AJ, Hodgson K, Bridgeman K, Shepherd JP. A randomized controlled trial of a brief intervention after alcohol-related facial injury. Addiction. 2003;98:43–52. doi: 10.1046/j.1360-0443.2003.00251.x. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26:724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- Tsai Y, Tsai M, Lin Y, Chen C. Brief intervention for problem drinkers in a Chinese population: A randomized controlled trial in a hospital setting. Alcohol Clin Exp Res. 2009;33(1):95–101. doi: 10.1111/j.1530-0277.2008.00815.x. [DOI] [PubMed] [Google Scholar]
- Walton MA, Goldstein AL, Chermack ST, McCammon RJ, Cunningham RM, Barry KL, Blow FC. Brief alcohol intervention in the emergency department: moderators of effectiveness. J Stud Alcohol Drugs. 2008;69:550–560. doi: 10.15288/jsad.2008.69.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Mun EY, Pugh L, Morgan TJ. Long-term effects of brief substance use interventions for mandated college students: Sleeper effects of an in-person personal feedback intervention. Alcohol Clin Exp Res. 2007;31(8):1380–1391. doi: 10.1111/j.1530-0277.2007.00435.x. [DOI] [PubMed] [Google Scholar]