Abstract
The purpose of this study was to identify socio-economic inequalities in regular dental attendance throughout the life-course. The analyses relied on data from SHARE (waves 1 to 3 of the Survey of Health, Ageing, and Retirement in Europe), which includes retrospective information on life-course dental attendance of 26,525 persons currently aged 50 years or greater from 13 European countries (Austria, Poland, Spain, Italy, the Netherlands, Belgium, Greece, the Czech Republic, France, Denmark, Switzerland, Germany, and Sweden). Inequalities in dental attendance were assessed by means of Concentration Indices. Socio-economic disparities in regular dental attendance were identified as early as childhood. Moreover, higher educational attainment resulted in increased probabilities of regular dental attendance throughout subsequent life-years in all nations. In most countries, inequality levels remained relatively inelastic throughout the life-course. These findings suggest that a considerable proportion of inequalities in dental care use is already established at childhood and persists throughout the life-course.
Keywords: socio-economic disparities, dental care use, lifecycle analysis, elderly populations, health policy, health care economics and organizations
Introduction
Socio-economic inequalities in oral health remain a major challenge for health policy and public health (Marmot and Bell, 2011; Williams, 2011). In particular, the general demographic transition and its impact on oral health (Harford, 2009) have attached special importance to tackling inequalities among elderly generations (Tsakos, 2011). Although the existence of such inequalities has been well-documented for many years (Watt and Sheiham, 1999; Locker, 2000; Gilbert et al., 2003; Sanders et al., 2006; Watt, 2007; Holst, 2008; Tsakos et al., 2009), we still do not comprehensively understand how such inequalities can best be reduced. Strategies for tackling oral health inequalities are increasingly being discussed within the context of a ‘common-risk factor’ approach (Sheiham and Watt, 2000; Sanders et al., 2005), which aims at addressing the joint causes of multiple common diseases, oral health impairment being just one of them (Marshman and Robinson, 2009). Policy areas generally relevant to oral health promotion are use of fluoride, food and health policies to reduce sugar consumption, community approaches to improve body hygiene (including oral cleaning), smoking cessation, policies on reducing accidents, and ensuring access to appropriate preventive care (Sheiham, 1995). In relation to the latter, dental attendance patterns have been proposed as one specific pathway contributing to oral health inequalities (Newton and Bower, 2005). Despite some concern about limited effectiveness of health care interventions (Gulliford, 2009), regular dental attendance has been shown to be associated with better oral health and to be more common among individuals at the upper end of the socio-economic scale (Donaldson et al., 2008).
For health-care decision-makers, it is essential to know whether socio-economic disparities in dental attendance among late-middle-aged and elderly generations are readily responsive to contemporaneous institutional arrangements, or whether such disparities rather reflect a continuation of health behaviors acquired in early life. On the one hand, it has been suggested that accessibility features of health care systems, such as health insurance coverage, may be relevant determinants of simultaneous inequalities in health care use (van Doorslaer et al., 2004). On the other hand, the lifecycle approach provides a suitable conceptual framework for explaining a potential perseverance of socially determined dental attendance behaviors throughout the life-course. In particular, it has been proposed that, in the sense of an accumulation of risk model (Kuh and Ben-Shlomo, 2004), children growing up in a social environment in which regular dental attendance is the norm are more likely to adhere closely to a pattern of routine dental visiting in adulthood than peers growing up in settings in which an example is set of problem-oriented dental visiting (Nicolau et al., 2007). Therefore, if socio-economic disparities in adults’ dental attendance primarily reflect a continuation of earlier acquired health behaviors, such inequalities may be relatively unresponsive to contemporaneous health policy interventions.
A recent paper (Listl, 2011) has documented income-related inequalities in dental service utilization for several elderly generations in Europe. While inequalities were evident for all countries examined, these could not be explained by contemporaneous differences in health care systems. Moreover, the results of another recent study based on the same study population (Listl et al., 2011) are indicative of a potentially large impact of childhood socio-economic status on dental care use in early life. The purpose of the present paper is, therefore, to extend previous work on inequalities in dental service utilization among elderly Europeans by tracking the corresponding socio-economic disparities back into childhood and forward into the further life-course.
Materials & Methods
Data Source
The present study is based on data from waves 1 to 3 of the Survey of Health, Ageing, and Retirement in Europe (SHARE). SHARE represents the first European dataset with detailed cross-national information about health, socio-economic conditions, and family backgrounds of the elderly population. The initial wave of SHARE included 11 countries and was conducted in 2004, followed by wave 2 in 2006-2007, which incorporated three additional countries. Wave 3 (referred to as SHARELIFE) was designed to collect detailed retrospective life-histories during 2008-2009. SHARE data are collected on the basis of computer-assisted personal interviews and self-completed paper & pencil questionnaires. Study participants are representative of the European population aged 50 and over in Scandinavia (Denmark and Sweden), Central Europe (Austria, France, Germany, Switzerland, Belgium, and the Netherlands), and the Mediterranean (Spain, Italy, and Greece), as well as two transition countries (the Czech Republic and Poland). Eligible as study participants are all household members aged 50 yrs and over. A detailed description of the SHARE and SHARELIFE methodology is available in the literature (Börsch-Supan et al., 2008; Schröder, 2008) and on the SHARE Web site (www.share-project.org).
Measures of Dental Attendance
SHARELIFE provides retrospective information about regular dental attendance throughout the life-course of 26,525 persons from 13 European countries. Based on the questions (see Appendix for details), a series of variables was constructed for depicting whether respondents had or had not regularly visited a dentist throughout their life history. These are:
regular dental attendance between life-years 0 and 15 (childhood);
regular dental attendance between life-years 16 and 25;
regular dental attendance between life-years 26 and 40;
regular dental attendance between life-years 41 and 55;
regular dental attendance between life-years 56 and 65;
regular dental attendance between life-years 66 and 75;
regular dental attendance from life-year 76 onward.
Measures of Socio-economic Conditions
Two frequently applied socio-economic measures are income and education. While SHARE contains information about respondents’ current income at the time of interview, i.e., at age 50+, the information in SHARELIFE about the income situation in earlier life-years is relatively limited. However, SHARE provides detailed information about respondents’ education. Importantly, educational attainment has been shown to have a strong impact on income level (Ashenfelter and Krueger, 1994). In accordance with human capital theory, education provides the skills and knowledge needed in the workplace. The more human capital an individual obtains, the more valuable (s)he is in the labor market, which then results in higher earnings (Mincer, 1958; Schultz, 1961).
In SHARE, respondents were asked about their highest educational attainment upon their first participation in the survey, i.e., either in wave 1 or in wave 2. Thereby, educational attainment was measured according to the International Standard Classification of Education [ISCED] (UNESCO, 1997; see Appendix for the definition of ISCED levels). Using educational attainment as a socio-economic measure is particularly appealing within a lifecycle framework. Its informative content already applies to the age at which education is usually completed, i.e., late adolescence and early adulthood. Moreover, it holds effective throughout the subsequent life-course, particularly due to its strong associations with income (see above). However, ‘educational attainment accomplished’ does not directly apply to socio-economic conditions in childhood and early adolescence.
SHARELIFE, fortunately, provides information about the number of books per household during childhood. As suggested in the social science literature, the number of books per household is a powerful proxy for the educational, social, and economic background during childhood and adolescence (Schütz et al., 2008). Moreover, the number of books at home has been shown to be the single most important predictor of educational attainment (Wößmann, 2003). In SHARELIFE, the relevant socio-economic measure was evaluated by asking “Approximately how many books were there in the place you lived in when you were 10?” With the additional reference that magazines, newspapers, or school books should not be counted, respondents could answer this question according to the following categories: “None or very few (0-10 books)”, “Enough to fill one shelf (11-25 books)”, “Enough to fill one bookcase (26-100 books)”, “Enough to fill two bookcases (101-200 books)”, and “Enough to fill two or more bookcases (more than 200 books)”.
Identification of Socio-economic Inequalities
Inequalities in dental attendance were identified by means of the Concentration Index (CI). The CI quantifies the degree of relative socio-economic inequality in a health variable and is increasingly being used in the dental literature (Perera and Ekanayake, 2008; Somkotra and Detsomboonrat, 2009; Do et al., 2010; Listl, 2011). The construct of the CI relates directly to the so-called ‘concentration curve’ (see Appendix for a detailed explanation). Formally, the CI can be expressed with reference to the covariance between a health sector variable and the fractional rank within the socio-economic distribution (Kakwani et al., 1997). An according formal definition of the CI for purpose of this study, i.e., identification of socio-economic inequalities in dental attendance, is given in formula 1 (Appendix). Generally note that the value of the CI is bounded between – 1 and +1, and a positive (negative) value of the CI means dental attendance is higher among the better (worse) off.
In the present paper, CIs were first calculated for all countries and for all different life periods. Statistically significant differences in CIs between different life periods and between countries were then identified by means of pairwise t tests. Moreover, cross-country socio-economic influences on CI level were assessed by means of linear regression. All data analysis in the present study was carried out with the software package STATA/SE 11 (StataCorp, College Station, TX, USA). The level of statistical significance was generally set at 5%.
Results
Table 1 shows summary statistics for population proportions of persons who have ever visited the dentist regularly throughout the life-course, and for the distribution of socio-economic stratification variables by respondents’ country of residence. Data in column 1 indicate considerable cross-country differences in the level of regular dental attendance. Similar variations between nations are displayed for socio-economic status, i.e., for number of books in household during childhood (column 2), and for highest educational attainment (column 3). Countries exhibiting relatively high levels of socio-economic status are shown to have higher levels of dental attendance in comparison with nations representing lower socio-economic status.
Table 1.
Summary Statistics – Population Proportions of Persons Who Have Ever Visited the Dentist Regularly, Number of Books per Household during Childhood, and Educational Attainment (ISCED levels)
| Number of Books in Household during Childhood |
Highest Educational Attainment (ISCED levels) |
||||||
|---|---|---|---|---|---|---|---|
| Ever Visited the Dentist Regularly | 0-10 | 11-100 | ➣100 | level 0-1 | level 2-3 | level 4-6 | |
| >Austria | 74.8% | 45.8% | 46.4% | 7.8% | 19.6% | 57.6% | 22.8% |
| Germany | 80.2% | 31.2% | 53.8% | 15.0% | 0.8% | 71.4% | 27.8% |
| Sweden | 95.4% | 20.0% | 56.2% | 23.8% | 34.8% | 35.4% | 29.8% |
| Netherlands | 85.0% | 31.1% | 53.6% | 15.3% | 16.1% | 62.2% | 21.7% |
| Spain | 43.1% | 63.6% | 30.0% | 6.4% | 64.1% | 28.0% | 7.4% |
| Italy | 47.4% | 75.2% | 21.2% | 3.6% | 53.2% | 38.2% | 8.6% |
| France | 71.0% | 45.8% | 40.9% | 13.3% | 42.9% | 37.8% | 19.3% |
| Denmark | 90.4% | 21.6% | 52.1% | 26.3% | 15.9% | 48.6% | 35.5% |
| Greece | 41.7% | 63.3% | 34.8% | 1.9% | 48.9% | 32.6% | 18.5% |
| Switzerland | 81.0% | 30.2% | 48.8% | 21.0% | 15.8% | 55.3% | 28.9% |
| Belgium | 65.1% | 46.3% | 41.3% | 12.4% | 26.5% | 49.7% | 23.8% |
| Czech Republic | 88.8% | 16.8% | 66.9% | 16.3% | 18.1% | 69.6% | 12.2% |
| Poland | 43.8% | 60.8% | 33.6% | 5.6% | 47.2% | 40.4% | 12.4% |
NB: For reasons of clarity and comprehensibility of the Table, “number of books” and “ISCED levels” are consolidated into three categories each.
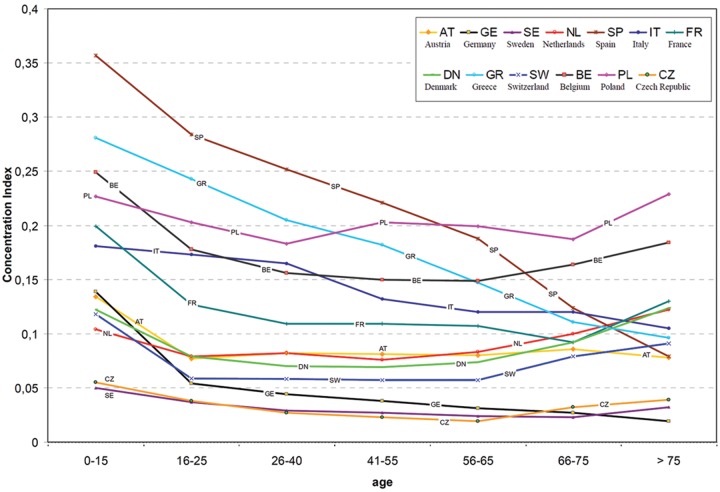
Table 2 presents CIs for inequalities in regular dental attendance throughout the respondents’ life-course and according to country of residence. The according CIs are also visualized in the Fig. CIs are generally positive and statistically significant throughout the full age range, the only exception being Germany, which displays a non-significant CI for age 75+. As indicated by pairwise t tests (Appendix Table 1), the majority of within-country comparisons of CIs between different life periods is statistically non-significant. In Poland, CI differences are statistically non-significant throughout the full age range. In Austria, Germany, Sweden, France, Switzerland, and Belgium, CIs at ages 0-15 are significantly higher than in later life periods, but no significant within-country differences exist after childhood. A similar pattern is found for the Czech Republic, where, additionally, CIs at ages 16-25 are significantly higher than at ages 56-65. The Netherlands and Denmark display CIs in childhood and late life periods which are significantly higher than in middle life. Spain, Italy, and Greece are the only countries displaying a gradual CI decline throughout the entire life-course, though corroboration of statistical significance is mostly lagged by at least one life period.
Table 2.
Concentration Indices (CI) for Inequalities in Regular Dental Attendance throughout the Life-course
| Age (yrs) |
||||||||
|---|---|---|---|---|---|---|---|---|
| 0-15 | 16-25 | 26-40 | 41-55 | 56-65 | 66-75 | > 75 | ||
| Country | AT | 0.134 | 0.077 | 0.082 | 0.081 | 0.080 | 0.086 | 0.078 |
| (0.101; 0.166) | (0.049; 0.105) | (0.054; 0.110) | (0.053; 0.108) | (0.052; 0.108) | (0.050; 0.121) | (0.024; 0.132) | ||
| GE | 0.139 | 0.054 | 0.044 | 0.038 | 0.031 | 0.027 | 0.019 | |
| (0.114; 0.164) | (0.035; 0.073) | (0.028; 0.060) | (0.023; 0.053) | (0.015; 0.046) | (0.006; 0.049) | (–0.019; 0.058) | ||
| SE | 0.050 | 0.037 | 0.029 | 0.027 | 0.024 | 0.023 | 0.032 | |
| (0.036; 0.060) | (0.026; 0.048) | (0.020; 0.039) | (0.018; 0.035) | (0.015; 0.032) | (0.013; 0.034) | (0.014; 0.049) | ||
| NL | 0.104 | 0.079 | 0.082 | 0.076 | 0.083 | 0.100 | 0.122 | |
| (0.088; 0.119) | (0.065; 0.093) | (0.069; 0.096) | (0.063; 0.089) | ( 0.068; 0.097) | (0.078; 0.121) | (0.089; 0.155) | ||
| SP | 0.357 | 0.284 | 0.252 | 0.221 | 0.188 | 0.124 | 0.079 | |
| (0.295; 0.419) | (0.236; 0.332) | (0.212; 0.292) | (0.186; 0.256) | (0.153; 0.224) | (0.079; 0.170) | (0.006; 0.153) | ||
| IT | 0.181 | 0.173 | 0.165 | 0.132 | 0.120 | 0.120 | 0.105 | |
| (0.136; 0.225) | (0.137; 0.209) | (0.133; 0.196) | (0.105; 0.159) | (0.093; 0.147) | (0.086; 0.154) | (0.042; 0.167) | ||
| FR | 0.199 | 0.127 | 0.109 | 0.109 | 0.107 | 0.092 | 0.130 | |
| (0.173; 0.224) | (0.105; 0.148) | (0.089; 0.128) | (0.090; 0.128) | (0.086; 0.127) | (0.065; 0.119) | (0.091; 0.168) | ||
| DN | 0.122 | 0.079 | 0.070 | 0.069 | 0.074 | 0.092 | 0.124 | |
| (0.107; 0.138) | (0.066; 0.091) | (0.059; 0.082) | (0.057; 0.080) | (0.061; 0.086) | (0.072; 0.111) | (0.092; 0.156) | ||
| GR | 0.281 | 0.243 | 0.205 | 0.182 | 0.147 | 0.111 | 0.096 | |
| (0.243; 0.320) | (0.209; 0.278) | (0.173; 0.236) | (0.153; 0.211) | (0.117; 0.178) | (0.067; 0.156) | (0.035; 0.158) | ||
| SW | 0.118 | 0.059 | 0.058 | 0.057 | 0.057 | 0.079 | 0.091 | |
| (0.097; 0.138) | (0.039; 0.079) | (0.040; 0.076) | (0.039; 0.074) | (0.038; 0.076) | (0.051; 0.106) | (0.046; 0.136) | ||
| BE | 0.249 | 0.178 | 0.156 | 0.150 | 0.149 | 0.164 | 0.184 | |
| (0.224; 0.274) | (0.157; 0.200) | (0.136; 0.176) | (0.131; 0.169) | (0.129; 0.170) | (0.135; 0.193) | (0.141; 0.227) | ||
| CZ | 0.055 | 0.038 | 0.027 | 0.023 | 0.019 | 0.032 | 0.039 | |
| (0.043; 0.066) | (0.027; 0.048) | (0.017; 0.038) | (0.013; 0.034) | (0.008; 0.030) | (0.013; 0.050) | (0.002; 0.076) | ||
| PL | 0.227 | 0.203 | 0.183 | 0.203 | 0.199 | 0.187 | 0.229 | |
| (0.194; 0.261) | (0.169; 0.237) | (0.149; 0.218) | (0.167; 0.238) | (0.160; 0.240) | (0.124; 0.250) | (0.127; 0.331) | ||
NB: 95% confidence intervals in parentheses; values in bold indicate statistical significance at the 5% level; socio-economic stratification relies on number of books per household during childhood (age group 0-15) and on educational attainment according to the International Standard Classification of Education; results are weighted (adjustment for age & sex); AT = Austria, GE = Germany, SE = Sweden, NL = Netherlands, SP = Spain, IT = Italy, FR = France, DN = Denmark, GR = Greece, SW = Switzerland, BE = Belgium, CZ = Czech Republic, PL = Poland.
Figure.
Inequalities in regular dental attendance throughout the lifecycle.
Statistical significance regarding cross-country differences in CIs is presented in Appendix Table 2. For the majority of comparisons between countries, pairwise t tests indicate significant CI differences, albeit the number of significant cross-country differences is reduced in late life. Finally, Appendix Table 3 presents parameter estimates from regression analyses for cross-country socio-economic influences on CI level. The results show that inequality decreases with increasing socio-economic status. Coefficients are highest for childhood and decline incrementally throughout subsequent life periods. Statistical significance corroborates until age yrs 56-65 but not thereafter.
Discussion
The findings of the present paper indicate disproportionate concentrations regarding regular dental attendance throughout the life-course among the better-off individuals in Spain, Greece, Poland, Italy, Belgium, the Netherlands, France, Denmark, Austria, Switzerland, the Czech Republic, Germany, and Sweden.
In comparison with the magnitude of cross-country variations, within-country variations in inequalities throughout the life-course appeared to be relatively low. The inequalities in most nations may, accordingly, be considered comparatively inelastic throughout the lifecycle. Moreover, the described cross-country differences in inequalities were shown to be associated with cross-country variations in socio-economic status. That is, countries with comparably high standards in terms of number of books in household during childhood and in terms of highest educational attainment turned out to have smaller inequality levels than nations with lower socio-economic standards, and vice versa. The observation that such an association between socio-economic and inequality measures is statistically significant until age yrs 65+ but not thereafter may, at least partially, be attributable to the age-related inequality decline in Spain, Greece, and Italy. One explanation for the specific inequality pattern in these countries could rest on a potentially increased appreciation of oral health care during the past decades. Given the high early-life disparities in dental attendance between the better- and worse-off, such a temporal trend may have had a particularly strong impact on inequalities in these countries.
In comparison with previous literature about relative income-related inequalities in dental service use by elderly Europeans (Listl, 2011), there are notable congruities. Above all, both income-related inequalities at age 50+ and socio-economic inequalities throughout the lifecycle were evident for many European countries. It should be noted, however, that the analyses are not directly comparable, because they are based on different socio-economic and utilization measures. Further limitations of the present paper should be mentioned. First, SHARELIFE data are based on a retrospective survey, and this may raise some concern of recall bias. However, a recent paper (Mazzonna and Havari, 2011) suggests that respondents well remember their health status and living conditions in early life. Second, educational attainment was used as a measure of socio-economic status at different life stages. But in the absence of more accurate socio-economic variables throughout the lifecycle, this appears to be a suitable approximation. Third, the number of observations became relatively small for older age groups, which is due to survey design. Therefore, the results may be interpreted with caution. Nevertheless, SHARE and SHARELIFE have the unique advantage of being representative of many European countries and, thus, of enabling cross-country comparisons to be made on the basis of a standardized survey.
Within the limitations of the present study, the findings suggest that a considerable proportion of inequalities in regular dental attendance is already established in childhood and persists throughout the life-course. Inequalities in later life-years may, thus, be relatively unresponsive to contemporaneous health policy interventions.
Supplementary Material
Footnotes
The present paper uses data from SHARELIFE release 1, as of November 24, 2010, and SHARE release 2.5.0, as of May 24, 2011. The SHARE data collection has been primarily funded by the European Commission through the 5th framework program (project QLK6-CT-2001-00360 in the thematic program Quality of Life), through the 6th framework program (projects SHARE-I3, RII-CT- 2006-062193, COMPARE, CIT5-CT-2005-028857, and SHARELIFE, CIT4-CT-2006-028812), and through the 7th framework program (SHARE-PREP, 211909 and SHARE-LEAP, 227822). Additional funding from the US National Institute on Aging (U01 AG09740-13S2, P01 AG005842, P01 AG08291, P30 AG12815, Y1-AG-4553-01 and OGHA 04-064, IAG BSR06-11, R21 AG025169) as well as from various national sources is gratefully acknowledged (see www.share-project.org for a full list of funding institutions). The author is fully funded through a Postdoctoral Fellowship by the Medical Faculty of the University of Heidelberg.
The author declares no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is published electronically only at http://jdr.sagepub.com/supplemental.
References
- Ashenfelter O, Krueger AB. (1994). Estimates of the economic return to schooling from a new sample of twins. Am Econ Rev 84:1157-1173 [Google Scholar]
- Börsch-Supan A, Brugiavini A, Jürges H, Kapteyn A, Mackenbach J, Siegrist J, et al. (2008). First results from the Survey of Health, Ageing, and Retirement in Europe (2004-2007) – Starting the longitudinal dimension. Mannheim: MEA; URL accessed on 3/8/2012 at: http://share-dev.mpisoc.mpg.de/fileadmin/pdf_documentation/FRB2/FRB2_all_chapters.pdf [Google Scholar]
- Do LG, Spencer AJ, Slade GD, Ha DH, Roberts-Thomson KF, Liu P. (2010). Trend of income-related inequality of child oral health in Australia. J Dent Res 89:959-964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson AN, Everitt B, Newton T, Steele J, Sherriff M, Bower E. (2008). The effects of social class and dental attendance on oral health. J Dent Res 87:60-64 [DOI] [PubMed] [Google Scholar]
- Gilbert GH, Duncan RP, Shelton BJ. (2003). Social determinants of tooth loss. Health Serv Res 38(6 Pt 2):1843-1862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliford M. (2009). Health services as determinants of population health. In: Oxford textbook of public health. 5th ed. Detels R, Beaglehole R, Lansang MA, Gulliford M, editors. Oxford: Oxford University Press [Google Scholar]
- Harford J. (2009). Population ageing and dental care. Community Dent Oral Epidemiol 37:97-103 [DOI] [PubMed] [Google Scholar]
- Holst D. (2008). Oral health equality during 30 years in Norway. Community Dent Oral Epidemiol 36:326-334 [DOI] [PubMed] [Google Scholar]
- Kakwani NC, Wagstaff A, Van Doorslaer E. (1997). Socioeconomic inequalities in health: measurement, computation and statistical inference. J Econometrics 77:87-104 [Google Scholar]
- Kuh D, Ben-Shlomo Y. (2004). The life course approach to chronic disease epidemiology. 2nd ed. Oxford: Oxford University Press [Google Scholar]
- Listl S. (2011). Income-related inequalities in dental service utilization by Europeans aged 50+. J Dent Res 90:717-723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Listl S, Moran V, Maurer J, Faggion CM., Jr (2012). Dental service utilization by Europeans aged 50 plus. Community Dent Oral Epidemiol 40: 164-74 [DOI] [PubMed] [Google Scholar]
- Locker D. (2000). Deprivation and oral health: a review. Community Dent Oral Epidemiol 28:161-169 [DOI] [PubMed] [Google Scholar]
- Marmot M, Bell R. (2011). Social determinants and dental health. Adv Dent Res 23:201-206 [DOI] [PubMed] [Google Scholar]
- Marshman Z, Robinson PG. (2009). Dental public health. In: Oxford textbook of public health. 5th ed. Detels R, Beaglehole R, Lansang MA, Gulliford M, editors. Oxford: Oxford University Press [Google Scholar]
- Mazzonna F, Havari E. (2011): Can we trust older people’s statements on their childhood circumstances? Evidence from SHARELIFE. SHARE Working Paper Series 05-2011. URL accessed on 3/8/2012 at: http://mea.mpisoc.mpg.de/uploads/user_mea_discussionpapers/1203_recall_bias13_MEA%20%281%29.pdf
- Mincer J. (1958). Investment in human capital and personal income distribution. J Polit Econ 66:281-302 [Google Scholar]
- Newton JT, Bower EJ. (2005). The social determinants of oral health: new approaches to conceptualizing and researching complex causal networks. Community Dent Oral Epidemiol 33:25-34 [DOI] [PubMed] [Google Scholar]
- Nicolau B, Thomson WM, Steele JG, Allison PJ. (2007). Lifecourse epidemiology: concepts and theoretical models and its relevance to chronic oral conditions. Community Dent Oral Epidemiol 35:241-249 [DOI] [PubMed] [Google Scholar]
- Perera I, Ekanayake L. (2008). Social gradient in dental caries among adolescents in Sri Lanka. Caries Res 42:105-111 [DOI] [PubMed] [Google Scholar]
- Sanders AE, Spencer AJ, Stewart JF. (2005). Clustering of risk behaviours for oral and general health. Community Dent Health 22:133-140 [PubMed] [Google Scholar]
- Sanders AE, Slade GD, Turrell G, Spencer A, Marcenes W. (2006). The shape of the socioeconomic-oral health gradient: implications for theoretical explanations. Community Dent Oral Epidemiol 34:310-319 [DOI] [PubMed] [Google Scholar]
- Schröder M. (2008). Retrospective data collection in the Survey of Health, Ageing and Retirement in Europe – SHARELIFE methodology. Mannheim: MEA; URL accessed on 3/8/ 2012 at: http://share-dev.mpisoc.mpg.de/fileadmin/pdf_sharelife/Publications/FRB-Methodology_2011_Ch.1.pdf [Google Scholar]
- Schütz G, Ursprung H, Wößman L. (2008). Education policy and equality of opportunity. Kyklos 61:279-308 [Google Scholar]
- Schultz T. (1961). Investment in human capital. Am Econ Rev 51:1-17 [Google Scholar]
- Sheiham A. (1995). Development of oral health promotion strategies In: Turning strategy into action. Kay E, editor. Manchester: Eden Bianchi Press [Google Scholar]
- Sheiham A, Watt RG. (2000). The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol 28:399-406 [DOI] [PubMed] [Google Scholar]
- Somkotra T, Detsomboonrat P. (2009). Is there equity in oral healthcare utilization: experience after achieving Universal Coverage. Community Dent Oral Epidemiol 37:85-96 [DOI] [PubMed] [Google Scholar]
- Tsakos G. (2011). Inequalities in oral health of the elderly: rising to the public health challenge? J Dent Res 90:689-690 [DOI] [PubMed] [Google Scholar]
- Tsakos G, Sheiham A, Ilife S, Kharicha K, Harari D, Swift CG, et al. (2009). The impact of educational level on oral health-related quality of life in older people in London. Eur J Oral Sci 117:286-292 [DOI] [PubMed] [Google Scholar]
- UNESCO (1997). International Standard Classification of Education (ISCED 1997). URL accessed on 3/8/2012 at: http://www.unesco.org/education/information/nfsunesco/doc/isced_1997.htm
- Van Doorslaer E, Masseria C, OECD Health Equity Research Group Members (2004). Income-related inequality in the use of medical care in 21 OECD countries. OECD Health Working Paper 14. URL accessed on 3/8/2012 at: http://www.oecd.org/dataoecd/14/0/31743034.pdf
- Watt R, Sheiham A. (1999). Inequalities in oral health: a review of the evidence and recommendations for action. Br Dent J 187:6-12 [DOI] [PubMed] [Google Scholar]
- Watt RG. (2007). From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dent Oral Epidemiol 35:1-11 [DOI] [PubMed] [Google Scholar]
- Williams DM. (2011). Global oral health inequalities – The research agenda. J Dent Res 90:549-551 [DOI] [PubMed] [Google Scholar]
- Wößmann L. (2003). Schooling resources, educational institutions and student performance: the international evidence. Oxford B Econ Stat 65:117-170 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.