Abstract
Background
High density lipoprotein (HDL) cholesterol level varies with ethnicity and gender. In Korea there has not been an agreement on standards for HDL cholesterol level. Therefore, in order to establish a foundation for research on HDL cholesterol, we investigated the gender difference in HDL cholesterol level after adjusting associated factors.
Methods
The study population included 4,465 individuals (1,833 men, 2,632 women) representing 33,502,918 Koreans 20 years of age or older, who participated in the 2005 Korean National Health and Nutrition Survey. After stratifying by gender, we analyzed the HDL cholesterol level according to the general characteristics of the study population. Then we identified independent factors associated with HDL cholesterol level. After adjusting for covariates, we estimated the gender difference in HDL cholesterol level.
Results
We demonstrated that age, current smoking, body mass index, alcohol intake, triglyceride and low density lipoprotein cholesterol level have significant impact on HDL cholesterol level. In addition, educational status was also an important factor for men, while fat intake was a significant factor for women. After adjusting associated factors, the means (standard errors) of HDL cholesterol level were 43.8 (0.2) mg/dL in men and 46.3 (0.2) mg/dL in women, respectively.
Conclusion
The mean gender difference in HDL level (2.5 mg/dL) in Korean adults was, therefore, less than those observed in previous western studies.
Keywords: Cholesterol, High Density Lipoprotein, Gender Difference, Korean National Health and Nutrition Survey (KNHANES)
INTRODUCTION
High density lipoprotein cholesterol (HDL-C) is considered protective in development of cardiovascular diseases. And yet, normal HDL-C level differs among countries and guidelines. While the National Cholesterol Education Program Adult Treatment Panel (NCEP ATP) III in USA and Japan defines low HDL-C group as 40 mg/dL or less in both men and women,1,2) the American Diabetes Association (ADA) stipulates 40 mg/dL or less for men and 50 mg/dL or less for women with diabetes, respectively.3) In Europe, HDL-C level of 40 mg/dL or less in men and 45 mg/dL or less in women is suggested to increase risk of cardiovascular diseases.4) Since there is no official reference level In Korea, the USA reference level has been used in practice. Despite the need for a standard reference values, there are still no studies on the optimal target level of HDL-C in Korean adults so far.
HDL-C level varies with ethnicity and gender. In general, women have a higher level than men. However, this gender difference is less prominent5-9) in Asia, including China and Japan, than in Europe and America.6,7,9) Since this gender difference in HDL-C is also expected to be present in the Korean population, the application of the western reference values to Korean population should be done with caution without any further adjustments.
Until recently, due to relatively limited therapeutic possibilities, research on HDL-C has been neglected compared to those on low density lipoprotein cholesterol (LDL-C) and triglyceride (TG). Furthermore, this paucity of any epidemiological ground contributed to the absence of consensus on the ideal HDL-C level. By controlling known and newly identified factors that influence HDL-C level, we investigated the gender difference in HDL-C in Korean adults in hope to provide a foundation for research on HDL-C in Korean adults.
METHODS
1. Study Population
The data analyzed in this study was obtained from the 2005 Korean National Health and Nutrition Survey (KNHANES III). Eligible subjects were 4,780 individuals aged 20 years or older, who completed the Health Interview Survey, the Nutrition Survey (NS), and the Health Examination Study; which are three major components in the KNHANES III. Of the total 4,780 subjects, 116 subjects who were not clearly fasting on exam day were excluded. And 199 subjects who were taking medication for dyslipidemia were also excluded. Accordingly, 4,465 subjects (1,833 [41.1%] men, 2,632 [58.9%] women) were finally included in this present study.
2. Data Collection
1) Socioeconomic and health behavior related characteristics
Among the subjects who have smoked more than 100 cigarettes in their whole life, we defined people smoking daily or often as 'current smoker.' 'Regular exercise group' was defined as people who responded that they were exercising more than once per week. Alcohol consumption was categorized as none, less than 30 g/day in men (15 g/day in women), and more than 30 g/day in men (15 g/day in women). Past medical history such as hypertension or diabetes diagnosed by physicians was questioned. Menopausal status was also surveyed in women. Daily fat intake was estimated based on NS using one day 24 hour recall. Fat density (percent energy intake from fat) was calculated by energy intake from fat divided by total energy intake.
2) Anthropometric measurements
Height was measured to the nearest 0.1 cm on a stadiometer (SECA 225, Hamburg, Germany). Body weight was measured to the nearest 0.1 kg on a balance scale (GL-6000-20, Cas, Yangju, Korea) with the subject wearing a lightweight gown or underwear. Body mass index (BMI) was classified into -22.9 kg/m2, 23-24.9 kg/m2, 25 kg/m2- according to the standard of the Ministry of Health and Welfare in 2006. Blood pressure was measured manually twice with a 30-second interval in between after minimum of 5 minute rest sitting in a chair, and the mean value was taken.
3) Laboratory assessments
Blood samples were drawn from the antecubital vein after overnight fasting (longer than 10 hrs). Total cholesterol, TG, HDL-C and fasting blood sugar (FBS) were measured with enzyme method through automatic chemistry analysis device (ADVIA 1650, Bayer, Tokyo, Japan). LDL-C was calculated using the Friedewald equation in cases of TG ≤ 400.10)
3. Analysis
All analyses used 'survey data analysis' option from STATA ver. 10.0 (StataCorp., College station, TX, USA) to account for the sampling weight from the multistage, stratified, and clustered sampling of KNHANES. The basic characteristics of the study population were expressed as mean or percentages with standard error (SE). After stratification by gender, we analyzed the mean (SE) of HDL-C level according to the general characteristics and cardiovascular risk factors. Multiple linear regression model to predict HDL-C was used to find out independent factors that affect HDL-C level. Finally, we estimated the gender difference in HDL cholesterol level using generalized linear model after adjusting covariates. Statistical significance was defined as a P < 0.05.
RESULTS
When the survey weight was applied, 1,833 male participants represented 16,462,647 Korean adult men and 2,632 female participants represented 17,040,271 Korean adult women; totaling 33,502,918 adults (Data not shown).
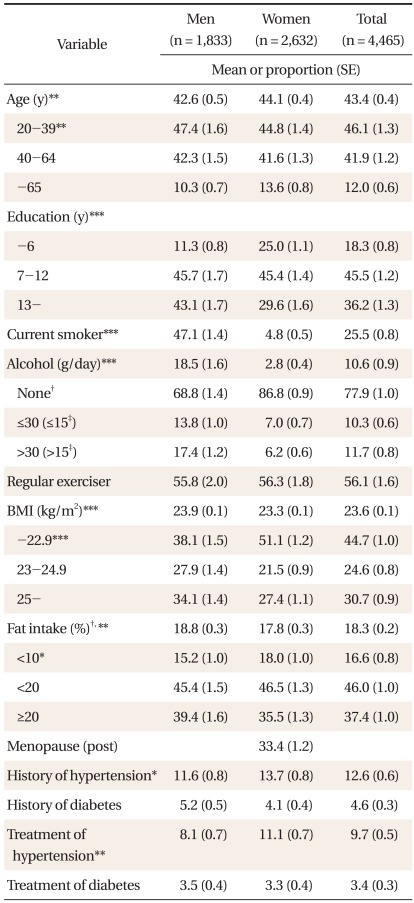
The mean age (SE) was 42.6 (0.5) years in men and 44.1 (0.4) years in women. Men had higher smoking rate and consumed more alcohol than women. Prevalence of obesity was also higher in men (34.1%) than in women (27.4%). Fat density was around 18% for both men and women. 33.4% of total women were postmenopausal (Table 1).
Table 1.
General characteristics of the study population.
Missing values were excluded.
SE: standard error, BMI: body mass index.
Significantly different between men and women group at *P < 0.05, **P < 0.01, and ***P < 0.001 by linear regression or logistic regression analysis. †As percent of total energy intake. ‡The alcohol amount of women.
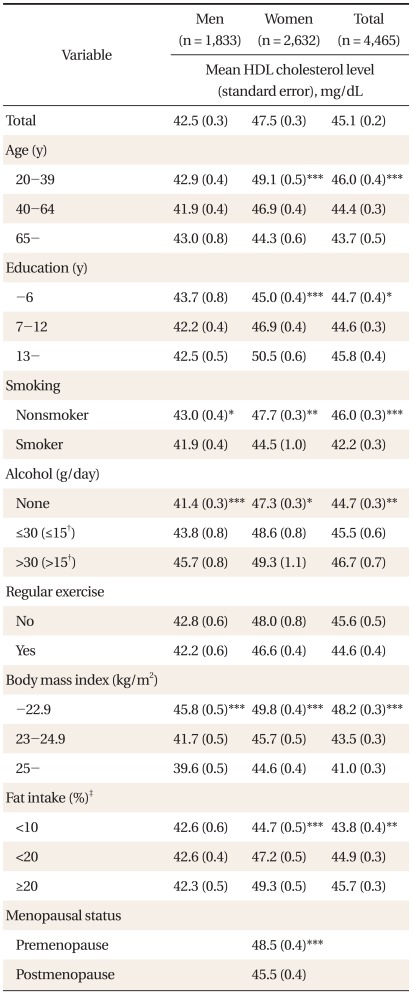
In men, mean HDL-C was significantly lower in smokers, nondrinkers and those with higher BMI. In women, HDL-C was lower in smokers, nondrinkers, postmenopausal women, women of older age, and in those with lower educational status, low fat density intake, and higher BMI (Table 2).
Table 2.
The means of high density lipoprotein (HDL) cholesterol level by general characteristics.
Significantly different between men and women group at P < 0.001 by linear regression analysis. Missing values were excluded.
Significant trend test across sex-specific categories at *P < 0.05, **P < 0.01, and ***P < 0.001 by linear regression analysis. †The alcohol amount of women. ‡As percent of total energy intake.
Mean HDL-C levels stratified by cardiovascular risk factors are shown in Table 3. Treated hypertension, FBS over 100 mg/dL, diagnosed or treated diabetes, TC more than 200 mg/dL, and TG less than 150 mg/dL were all associated with a lower HDL-C level. Additionally, blood pressure over 120/80 mmHg, diagnosed hypertension, and LDL-C less than 130 mg/day were related with lower HDL-C level in women.
Table 3.
The means of high density lipoprotein (HDL) cholesterol level by cardiovascular risk factors.
Missing values were excluded.
Significantly different between sex-specific categories at *P < 0.05, **P < 0.01, and ***P < 0.001 by linear regression analysis. †The level of total cholesterol, low density lipoprotein cholesterol, triglyceride were categorized according to the National Cholesterol Education Program Adult Treatment Panel.
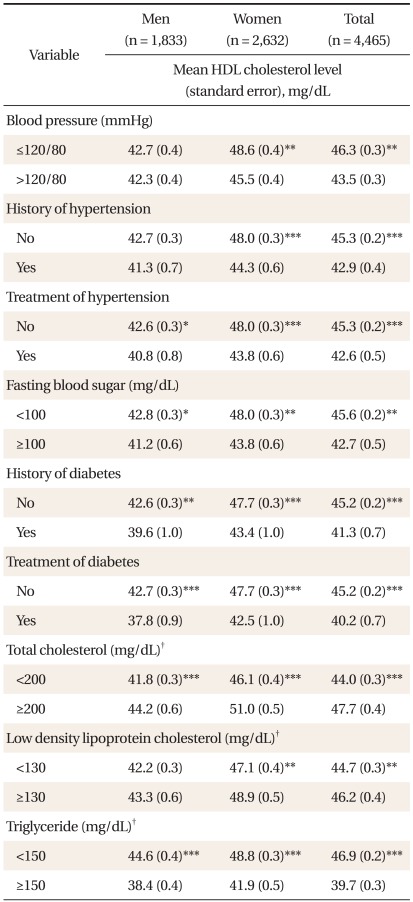
Mean HDL-C level for Korean men were 42.5 ± 0.3 mg/dL and 47.5 ± 0.3 mg/dL for Korean women. Thus the mean unadjusted HLD-C difference by sex was 5.0 mg/dL (P < 0.001) (Table 2). The distribution of HDL-C was also reviewed. The largest population proportion of high HDL-C level was 30-40 mg/dL (39.0%) for men and 40-50 mg/dL (38.3%) for women (Figure 1). The estimated prevalence of lower HDL-C group by the NCEP ATP III was 43.8% for men and 23.6% for women (P < 0.001, data not shown). Those by ADA criteria were 43.8% for men and 62.6% for women (P < 0.001, data not shown).
Figure 1.
Distribution of high density lipoprotein cholesterol (HDL-C) level in men and women.
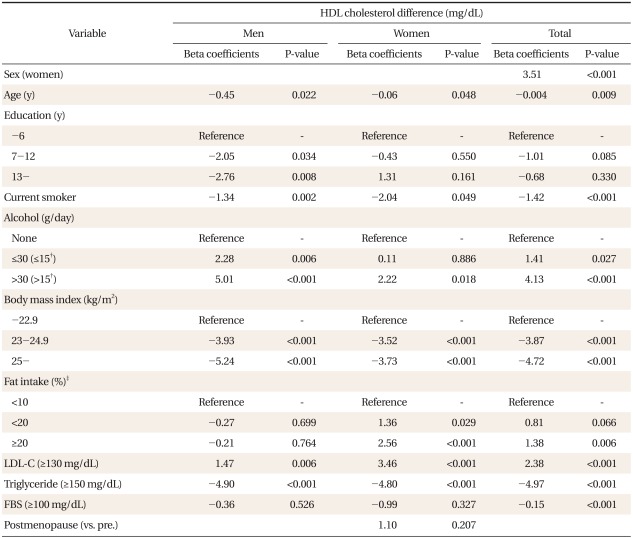
Multiple regression analysis was carried out to identify independent factors that affect HDL-C level (Table 4). While older age, smoking, overweight or obesity, and TG over 150 mg/dL were significantly associated with lower HDL-C level, alcohol drinking more than 30 g/day (15 g/day for female) and LDL-C more than 130 mg/dL (P < 0.001) were associated with higher HLD-C level. Education level was related to a lower level of HDL-C only in men, and higher fat intake was related to a higher HDL-C level only in women.
Table 4.
Estimated effects on HDL cholesterol level* associated with differences in other factors.
HDL: high density lipoprotein, LDL-C: low density lipoprotein cholesterol, FBS: fasting blood sugar.
*By multiple regression analysis. †The alcohol amount of women. ‡As percent of total energy intake.
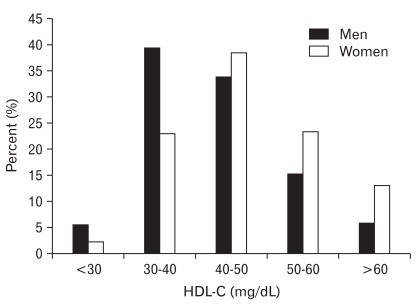
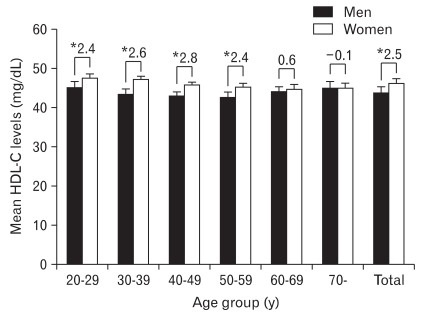
Mean HDL-C according to gender and age was estimated after controlling the following factors: educational level, current smoking status, alcohol intake quantity, BMI, fat density quantity, LDL-C and TG levels (Figure 2). Mean HDL-C level of Korean men and women were 43.8 ± 0.2 mg/dL and 46.3 ± 0.2 mg/dL respectively. Mean gender difference was 2.5 mg/dL (P < 0.001). However, this gender difference disappeared after 60 years-old and older.
Figure 2.
Covariates-adjusted age group specific gender difference in level of high density lipoprotein cholesterol (HDL-C) (mean ± SD). *Significantly different between men and women at P < 0.001 by general linear models. Data were adjusted for education level (-6 y, 7-12 y, 13 y-), current smoking status (yes or no), the amount of alcohol intake (men: no, ≤30 g/day, >30 g/day; women: no, ≤15 g/day, >15 g/day), body mass index (-22.9 kg/m2, 23-24.9 kg/m2, 25 kg/m2-), fat intake (% of total energy intake; <10%, <20%, ≥20%), low density lipoprotein cholesterol (<130 mg/dL, ≥130 mg/dL), triglyceride (<150 mg/dL, ≥150 mg/dL). Age (y; continuous) was further adjusted for total group.
DISCUSSION
In this study, we assessed factors that affect HDL-C level after stratifying by gender and estimated the gender difference in the HDL-C level after adjusting the relevant factors. HDL-C level was associated with age, smoking, BMI, alcohol consumption, TG and LDL-C in both sexes. In addition, educational status was a risk factor in men, while fat intake was in women. The unadjusted gender difference in HDL-C level of 5 mg/dL decreased to 2.6 mg/dL after adjusting relevant factors. The final estimated mean HDL-C level of Korean adult men and women were 43.8 ± 0.2 mg/dL, and 46.3 ± 0.2 mg/dL, respectively. HDL-C level was higher in women until their 50s. Sex difference in HDL-C was less than those of westerns countries. However, Korean data showed a similar tendency.10-13)
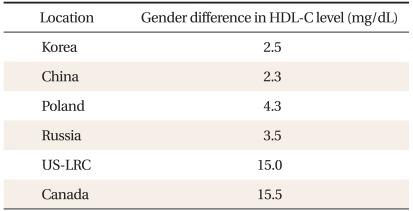
HDL-C distribution differed by ethnicity and gender.5,6,13,14) Davis et al.6) assessed the sex difference in HDL-C level of six countries and showed that women had higher HDL-C level than men; the difference was the highest in Canada and USA at as high as 15.5 mg/dL, and the lowest in China at as low as 2.3 mg/dL. Kesteloot et al.14) also demonstrated that gender difference was higher in Belgium as compared to China, confirming previous findings. The unadjusted sex difference of 5.0 mg/dL resulted from factors such as educational level, smoking, alcohol consumption, age, fat intake, BMI, LDL-C, and TG level. Although the difference is attenuated after adjustment of these factors, there still remained significant difference of 2.5 mg/dL. This result was similar to the difference in China but far less than those expected in USA or Europe (Table 5).
Table 5.
Covariates-adjusted gender difference in HDL-C level from six countries.6)
US-LRC, US Lipid Research Clinics.
The results of other countries (except Korea) were based on reference.6) As for other countries, data were adjusted for age (years), body mass index (kg/m2), current smoking status (yes or no), the amount of alcohol intake (20 g/day), centered heart rate (20 beats/min), and hormone use (yes or no). As for Korea, data were adjusted for education level (years; -6, 7-12, 13-), current smoking status (yes or no), the amount of alcohol intake (men; no, ≤30 g/day, >30 g/day, women; no, ≤15 g/day, >15 g/day), body mass index (-22.9 kg/m2, 23-24.9 kg/m2, 25 kg/m2-), fat intake (% of total energy intake; <10%, <20%, ≥20%), low density lipoprotein cholesterol (<130 mg/dL, ≥130 mg/dL), triglyderide (<150 mg/dL, ≥150 mg/dL), fasting blood sugar (<100 mg/dL, ≥100 mg/dL) and age (years; continuous).
The higher HDL-C level in women partly explained the lower mortality from cardiovascular disease in women.8,15) Furthermore, countries with lower gender difference in HDL-C level have a lower cardiovascular mortality and a lower gender difference in mortality.6,9,15) Mascitelli and Pezzett15) suggested that the same level of HDL-C in men would not only reduce the gender differences in cardiovascular mortality, but also lower the overall mortality. Gender difference in HDL-C is partly explained by estrogen. Estrogen is known to reduce the metabolic activity of macrophage by lipid accumulation, while testosterone promotes it.16,17) In this study, HDL-C level remained higher in women even after menopause, confirming our previous finding that menopause and HDL-C level were independent from each other.18) Therefore, the gender difference in HDL-C level is not a simple result of sex hormones and other unknown factors need to be investigated.
An increase in HDL-C level by 6% reduces the incidence of cardiovascular disease by 22-24%, which is similar to the effect of reduced LDL-C level decreasing cardiovascular disease by 28%.19,20) In addition, low HDL-C level has been blamed as the main cause of recent increasing prevalence dyslipidemia in Korea.21) Though pharmacological treatment options to increase HDL-C such as cholesterol ester transfer protein (CETP) inhibitor and apo A1 mimetic peptide are under development, basic epidemiological evidences required to define HDL-C cut-off levels are still not sufficient in Korea. If the study subjects are categorized by the NCEP ATP III guideline, 43.8% of men and 23.6% of women belong to the low HDL-C group. When the ADA guideline is used, 43.8% of men and 62.6% of women have low HDL-C group; resulting in a markedly higher prevalence of low HDL-C level in women. Musha et al.5) from Japanproposes a higher cut-off value of HDL-C of 50 mg/dL so that the prevalence of cardiovascular diseases in men and women become similar. Although the ideal methodology to determine the cut-off value of HDL-C should be based on incidence or mortality of cardiovascular diseases from longitudinal studies; there are few large scale prospective studies to give us answers. In this situation, the second best option would be to adopt existing foreign guidelines as reference and modify those reflecting Korean situations. In fact, in the year 2009, the Korean Society of Lipidology and Atherosclerosis set cut-off values of 40 mg/dL for lower HDL-C level for both male and female by using existing guidelines of USA as reference, but no target treatment level was suggested. Given the current Korean situation of scarce basic epidemiological studies, our study would be highly meaningful.
Since serum lipids are closely related to each other,22) it is quite difficult to define independent factors that influence the level of each lipid subsets. This close correlation between serum lipids was shown in our study. For an example, the mean HDL-C was significantly lower for both sexes in the high TG group (≥150 mg/dL). This is in part explained by the fact that TG increases CETP action on HDL-C disintegration.23) Inverse relationship between TG and HDL-C has already been reported in various studies.12,24,25) The tendency of increasing HDL-C along with an increase in LDL-C was also reported.25) We also confirmed that mean HDL-C is high in the normal or above normal LDL-C group. Fat consumption also affects HDL-C level. High fat diet is known to increase HDL-C by increasing the apoA-1 synthesis.26) Kim et al.11) suggested that mean HDL-C increased in women with higher fat intake, which is similar to the result of our study. This finding partially explains the reasons for low HDL-C in Koreans who consume less than 20% of total energy intake from fat, which is far lower than westerners.21)
Our limitations include the following. Although the KNHANES III is a large scale data that represents the entire Korean population, detailed measurement of behavioral factors is not possible for large number of subjects. This could be the reason why factors such as exercise, which had been found to be related to HDL-C in the previous studies, failed to prove significant relevance in our study.27) In addition, we could not fully assess and adjust lifestyle behavioral factors partly because of factors that we could not identify and partly because of crude measurements. For example, lower education level was associated with a higher HDL-C level in our study. We do not think that educational level influence HDL-C level directly; rather it may affect behavioral risk factors related with HDL-C and in turn affect HDL-C level (confounding effect).28) Many subjects of our group with less than 6 years of schooling are of old age (mean age of 64.6 year), not obese (mean BMI of 23.2 kg/m2), and non-smokers (average smoking rate of 44.6%). These characteristic are all favorable factors of high HDL-C level. Accordingly, HDL-C was higher in the lower educational level group even after statistical adjustments, which suggest the remaining confounding effect.
Difference in HDL-C level by gender in Korean adults was much less than those from western countries. When considering the importance of HDL-C, it is necessary to modify low HDL-C level by actively managing modifiable factors such as smoking and high BMI. Further studies are needed to find out the meaning of the racial and gender differences of HDL-C level in terms of cardiovascular disease prevalence and mortality using longitudinal study designs. We hope our results be used as basic evidence for establishing standards for HDL-C management for Korean adults.
References
- 1.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 2.Teramoto T, Sasaki J, Ueshima H, Egusa G, Kinoshita M, Shimamoto K, et al. Diagnostic criteria for dyslipidemia. Executive summary of Japan Atherosclerosis Society (JAS) guideline for diagnosis and prevention of atherosclerotic cardiovascular diseases for Japanese. J Atheroscler Thromb. 2007;14:155–158. doi: 10.5551/jat.e537. [DOI] [PubMed] [Google Scholar]
- 3.Haffner SM American Diabetes Association. Dyslipidemia management in adults with diabetes. Diabetes Care. 2004;27(Suppl 1):S68–S71. doi: 10.2337/diacare.27.2007.s68. [DOI] [PubMed] [Google Scholar]
- 4.Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary: fourth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (Constituted by representatives of nine societies and by invited experts) Eur Heart J. 2007;28:2375–2414. doi: 10.1093/eurheartj/ehm316. [DOI] [PubMed] [Google Scholar]
- 5.Musha H, Hayashi A, Kida K, Takahashi E, Suzuki K, Kawasaki K, et al. Gender difference in the level of high-density lipoprotein cholesterol in elderly Japanese patients with coronary artery disease. Intern Med. 2006;45:241–245. doi: 10.2169/internalmedicine.45.1528. [DOI] [PubMed] [Google Scholar]
- 6.Davis CE, Williams DH, Oganov RG, Tao SC, Rywik SL, Stein Y, et al. Sex difference in high density lipoprotein cholesterol in six countries. Am J Epidemiol. 1996;143:1100–1106. doi: 10.1093/oxfordjournals.aje.a008686. [DOI] [PubMed] [Google Scholar]
- 7.Kesteloot H, Lee CS, Park HM, Kegels C, Geboers J, Claes JH, et al. A comparative study of serum lipids between Belgium and Korea. Circulation. 1982;65:795–799. doi: 10.1161/01.cir.65.4.795. [DOI] [PubMed] [Google Scholar]
- 8.Barrett-Connor E. Sex differences in coronary heart disease. Why are women so superior? The 1995 Ancel Keys Lecture. Circulation. 1997;95:252–264. doi: 10.1161/01.cir.95.1.252. [DOI] [PubMed] [Google Scholar]
- 9.Klimis D, Gnardellis C, Trichopoulou A. Gender differences in blood lipids in a Greek island population: the EPIC study. Nutr Res. 2000;20:35–45. [Google Scholar]
- 10.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 11.Kim SM, Han JH, Park HS. Prevalence of low HDL-cholesterol levels and associated factors among Koreans. Circ J. 2006;70:820–826. doi: 10.1253/circj.70.820. [DOI] [PubMed] [Google Scholar]
- 12.Goh VH, Tong TY, Mok HP, Said B. Differential impact of aging and gender on lipid and lipoprotein profiles in a cohort of healthy Chinese Singaporeans. Asian J Androl. 2007;9:787–794. doi: 10.1111/j.1745-7262.2007.00294.x. [DOI] [PubMed] [Google Scholar]
- 13.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, et al. Trends in serum lipids and lipoproteins of adults, 1960-2002. JAMA. 2005;294:1773–1781. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 14.Kesteloot H, Huang DX, Yang XS, Claes J, Rosseneu M, Geboers J, et al. Serum lipids in the People's Republic of China: comparison of Western and Eastern populations. Arteriosclerosis. 1985;5:427–433. doi: 10.1161/01.atv.5.5.427. [DOI] [PubMed] [Google Scholar]
- 15.Mascitelli L, Pezzetta F. High-density lipoprotein cholesterol and sex difference in coronary heart disease risk. Am J Med. 2006;119:e17. doi: 10.1016/j.amjmed.2005.10.044. [DOI] [PubMed] [Google Scholar]
- 16.Rossouw JE. Hormones, genetic factors, and gender differences in cardiovascular disease. Cardiovasc Res. 2002;53:550–557. doi: 10.1016/s0008-6363(01)00478-3. [DOI] [PubMed] [Google Scholar]
- 17.Suh MS, Lee HG, Yoon YS, Sunwoo S, Park HS. Factors associated low HDL cholesterol in adults. J Korean Acad Fam Med. 2001;22:1214–1223. [Google Scholar]
- 18.Park HA, Park JK, Park SA, Lee JS. Age, menopause, and cardiovascular risk factors among Korean middle-aged women: the 2005 Korea National Health and Nutrition Examination Survey. J Womens Health (Larchmt) 2010;19:869–876. doi: 10.1089/jwh.2009.1436. [DOI] [PubMed] [Google Scholar]
- 19.Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 20.Rubins HB, Robins SJ, Collins D, Fye CL, Anderson JW, Elam MB, et al. Veterans Affairs High-Density Lipoprotein Cholesterol Intervention Trial Study Group. Gemfibrozil for the secondary prevention of coronary heart disease in men with low levels of high-density lipoprotein cholesterol. N Engl J Med. 1999;341:410–418. doi: 10.1056/NEJM199908053410604. [DOI] [PubMed] [Google Scholar]
- 21.Korea Centers for Disease Control and Prevention. The Third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005. Seoul: Korea Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 22.Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al. Harrison's principles of internal medicine. 17th ed. New York: McGraw-Hill; 2008. [Google Scholar]
- 23.Kwiterovich PO., Jr The metabolic pathways of high-density lipoprotein, low-density lipoprotein, and triglycerides: a current review. Am J Cardiol. 2000;86(12A):5L–10L. doi: 10.1016/s0002-9149(00)01461-2. [DOI] [PubMed] [Google Scholar]
- 24.Hansel B, Kontush A, Giral P, Bonnefont-Rousselot D, Chapman MJ, Bruckert E. One third of the variability in HDL-cholesterol level in a large dyslipidaemic population is predicted by age, sex and triglyceridaemia: The Paris La Pitie Study. Curr Med Res Opin. 2006;22:1149–1160. doi: 10.1185/030079906X104821. [DOI] [PubMed] [Google Scholar]
- 25.Kolovou GD, Anagnostopoulou KK, Damaskos DS, Bilianou HI, Mihas C, Milionis HJ, et al. Gender differences in the lipid profile of dyslipidemic subjects. Eur J Intern Med. 2009;20:145–151. doi: 10.1016/j.ejim.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 26.Wolf G. High-fat, high-cholesterol diet raises plasma HDL cholesterol: studies on the mechanism of this effect. Nutr Rev. 1996;54:34–35. doi: 10.1111/j.1753-4887.1996.tb03772.x. [DOI] [PubMed] [Google Scholar]
- 27.Teramoto M, Golding LA. Regular exercise and plasma lipid levels associated with the risk of coronary heart disease: a 20-year longitudinal study. Res Q Exerc Sport. 2009;80:138–145. doi: 10.1080/02701367.2009.10599547. [DOI] [PubMed] [Google Scholar]
- 28.Muennig P, Sohler N, Mahato B. Socioeconomic status as an independent predictor of physiological biomarkers of cardiovascular disease: evidence from NHANES. Prev Med. 2007;45:35–40. doi: 10.1016/j.ypmed.2007.04.005. [DOI] [PubMed] [Google Scholar]