Abstract
Background
Frailty is considered to be a clinical syndrome characterized by decreased physiological reserves associated with a greater risk of health-related problems, hospitalization, and death. The current study examined hospitalization, falls, cognitive decline and disability between robust, prefrail and frail elderly in one year.
Methods
110 participants aged 65 or more who visited two senior welfare centers in Seoul from February 2008 to June 2008 were surveyed again from March 2009 to June 2009 with demographic characteristics, number of chronic diseases and medication, study of osteoporotic fractures (SOF) frailty index, instrumental activity of daily living (IADL), depression, mini-mental state examination-Korean version (MMSE-K), falling history and admission history within one year. These results were compared with participants' previous survey done one year ago.
Results
Among total 110 subjects, 48 (44%) robust, 30 (27%) prefrail, and 32 (29%) frail subjects changed to 26 (24%), 54 (49%), and 30 (27%) respectively over the year. There were statistical significances in age, number of chronic disease, depressive mood, MMSE, falls, hospitalization, IADL disability contributing to frailty (P < 0.05). Frailty defined by SOF frailty index was associated with greater risk of adverse outcomes. Frail subjects had a higher age-adjusted risk of cognitive function decline (odds ratio [OR], 3.57), disability (OR, 9.64), fall (OR, 5.42), and hospitalization (OR, 4.45; P < 0.005).
Conclusion
The frailty index like SOF frailty index might predict risk of falls, disability, hospitalization, and cognitive decline in the elderly, emphasizing special attention to the individuals showing frailty in outpatient examination.
Keywords: Elderly, Frailty, Adverse Outcomes Retrospective Study
INTRODUCTION
Frailty is a state of increased vulnerability to stressors that results from decreased physiological reserves and multisystem dysregulation, or a state of limited capacity to maintain homeostasis and to respond to internal and external stresses. Frailty is an aggregate expression of risk resulting from age or disease associated physiologic accumulation of subthreshold decrements affecting multiple physiologic systems resulting in adverse health outcomes.1)
Of various health outcomes, this study aims to prove frailty in relation with disability, cognitive impairment, falls and hospitalization due to following reasons. As the population ages, disability is becoming an increasingly important concept both for its public health consequences as adverse health outcomes and increasing costs and for impaired quality of life of the older population.2)
Cognitive impairment is a known risk factor of many geriatric outcomes, and the assessment of mental status is a routine part of most geriatric evaluations in the clinical setting. Functional and cognitive declines are associated not only with loss of independence and reduced quality of life for older adults, but also with increased health service use, greater risk for institutionalization and mortality.
Falls have been recognized for decades by health care professionals as an etiology of injury, but were not seen as an important independent marker of frailty until more recently. They are associated with a high mortality that is not always explainable by the fall injury itself.3) For good reason, today fall is considered a health problem on its own and a unique geriatric syndrome.4) Hospitalization has been shown to increase the risk of functional decline and disability in older adults.5)
There are many studies to elucidate the concept of frailty, aging and disability in order to increase quality of life of the elderly in developed countries. The purpose of this article is to describe frailty as an indicator of risk factors for various adverse health outcomes6) listed above in the growing population of elderly in Korea.
METHODS
1. Participants
From February 2008 to June 2008, a total of 302 outpatients of 65 years old or older who visited senior welfare centers located in Seoul and Gyeonggi province participated in the baseline examination of the frailty study. From March 2009 to June 2009, we visited 2 centers in Seoul, and 110 participants of total 178 subjects at Seoul area who participated last year and were still visiting the centers or could be reached in telephone were surveyed with a questionnaire or examination for frailty criteria and health related problems in the previous year.
2. Measurements
All participants were surveyed by 1 doctor with structured questionnaire and screening tools of depression, cognitive function, disability and, study of osteoporotic fractures (SOF) frailty index, and were asked about health status, education, economic status, smoking history, falls, hospitalization during the previous year.
1) Demographic characteristics
Age, sex, education level, religion, marital status, cohabitant, and economic status were asked.
2) Health status
Presence or absence of chronic illness (hypertension, diabetes mellitus, stroke, cancer, dementia, Parkinson's disease, dyslipidemia, coronary heart disease, chronic obstructive lung disease) and number of medication intake were asked.
3) SOF frailty index7)
Frailty defined according to the SOF index was identified by the presence of two or more of the following three components at the one year follow-up examination; a) Weight loss (unintentional weight loss) of 5% or more between the baseline and second examination, b) Inability to rise from a chair five times without using the arms, c) Poor energy as identified by an answer of "no" to the question "Do you feel full of energy?" on the geriatric depression scale. Participants with none of the above components were considered to be robust, and those with one component were considered to be in prefrail state.
4) Instrumental activities of daily living (IADL)
Participants indicated whether they were able to perform 10 IADLs based on K-IADL scale by Won,8) such as grooming, doing housework, preparing for own meals, doing laundry, going out, ability to use public or private transport, shopping, managing money, using a telephone, and being responsible for their own medication. Disability was defined as one or more new IADL impairments7) from the previous score.
5) Mini-mental state examination-Korean version (MMSE-K)
Mini-mental status examination developed by Folstein et al.9) in 1975 was revised and adjusted by Kwon10) in 1989. MMSE-K shows summed score of 30 that consists of orientation of time and place (10), memory (3), recall (3), calculation and concentration (5), comprehension and judgment (2), and language (7). Decrease of summed score by 3 or more compared with score of last year was defined as having had a long-term cognitive decline.11)
6) Depression
Hoyl geriatric depression scale (GDS)-512) consists of 5 items from 15-item GDS by Sheikh et al.13) which proved higher sensitivity, specificity, positive predictive value for screening compared to other short forms of GDS in study by Park et al.14) The items consist of whether the person is satisfied with life (1 on no), gets bored (1), often feels helpless (1), prefers to stay home rather than going out and doing new things (1), feels pretty worthless the way it is (1) within past one week, with scores over 2 defined as having depressive mood.
7) Falls
Asked history of any fall in the previous year (yes or no) obtained by self report.
8) Hospitalization
Asked history of any hospitalization in the previous year (yes or no) obtained by self report.
3. Statistical Analyses
SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used. Pearson's chi-square tests were used to analyze characteristics of participants by category of frailty status in correlation with age, sex, education, marital status, family income, BMI, number of chronic disease, number of current medication, presence of depressive mood, MMSE, falls, hospitalization, IADL disability and smoking. Age and sex adjusted adverse outcomes were calculated using logistic regression to analyze the association between frailty indicators and the odds of cognitive function decline, disability, fall and hospitalization in the subsequent year. The relative risk (approximated as odds ratio [OR]) of each outcome with 95% confidence intervals (CI) was estimated for participants categorized as prefrail and those as frail using robust as the referent group.
RESULTS
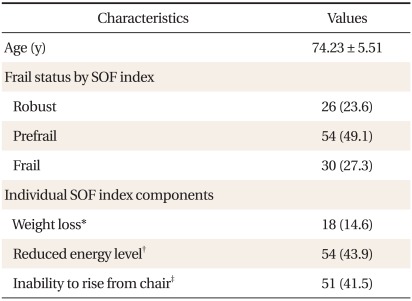
The baseline characteristics of the study participants are shown in Table 1. The mean age of 110 participants was 74.23 ± 5.51. 27.3% of participants were frail with more than 2 components by SOF frailty index criteria, 49.1% were prefrail with 1 component of SOF, and 23.6% were robust with none of the components. Of individual SOF frailty index components, reduced energy level was highest with 43.9%; inability to rise from chair and weight loss was 41.5% and 14.6% of the reply, respectively.
Table 1.
Characteristics of 110 participants.
Values are presented as mean ± SD or number (%).
SOF: study of osteoporotic fractures.
*Unintentional weight loss of 5% or more during 1 year before the examination. †Answer of "no" to the question "Do you feel full of energy?" ‡The subject's inability to rise from a chair 5 times without using the arms.
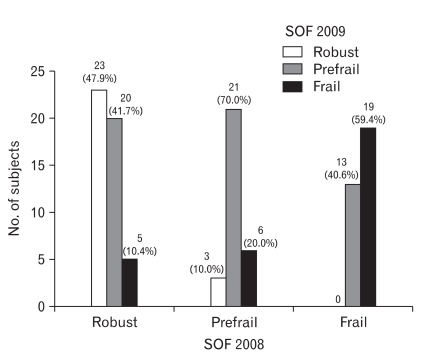
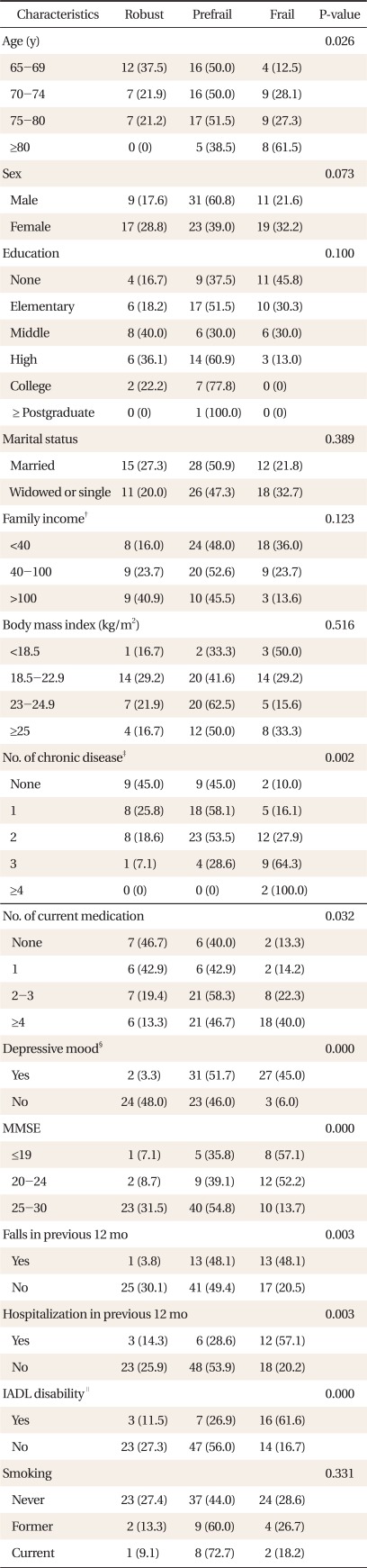
Among total 110 subjects, 48 (44%) robust, 30 (27%) prefrail, and 32 (29%) frail elderly identified in the previous year changed to 26 (24%), 54 (49%), and 30 (27%) respectivey during follow-up of 12 months (Figure 1). There were statistical significances in age, number of chronic disease, depressive mood, MMSE, falls, hospitalization, IADL disability contributing to frailty (P < 0.05). On the contrary, sex, education, marital status, family income, BMI, and smoking appeared not to be in close association with frailty status (P > 0.05) (Table 2).
Figure 1.
Change of frailty status in 12 months. SOF: study of osteoporotic fractures.
Table 2.
Characteristics of participants by category of frailty status as defined by the study of osteoporotic fractures (SOF) index.*
Values are presented as number (%). P-value from x2 test for outcomes comparing a difference between any of the 3 study groups.
MMSE: mini-mental state examination, IADL: instrumental activity of daily living.
*Analyzed with chi-square test. †To be expressed in ten thousand Won in Korean currency. ‡History of 1 or more selected medical conditions including stroke, cancer (excluding skin cancer), dementia, hypertension, parkinsonism, diabetes mellitus, dyslipidemia, coronary heart disease, and chronic obstructive lung disease. §Score over 2 by Hoyl geriatric depression scale (GDS)-5 indicates depressive mood. ∥Having difficulties in or inability to perform IADL tasks.
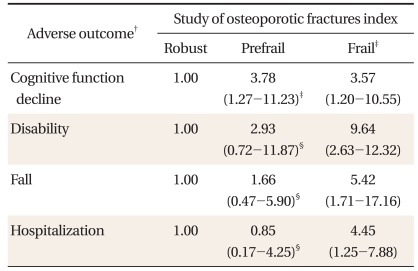
During an average follow-up of 12 months, compared with robust participants, participants in prefrail group (OR, 3.78; 95% CI, 1.27 to 11.23) and frail group (OR, 3.57; 95% CI, 1.20 to 10.55) had an increased age adjusted risk of cognitive function decline. Compared with robust participants, frail group (OR, 9.64; 95% CI, 2.63 to 12.32) had an increased risk of disability, whereas the associations were diminished in magnitude in prefrail group. The risk of hospitalization was significant in frail group (OR, 4.45; 95% CI, 1.25 to 7.88) whereas it did not reach statistical significance in prefrail group. The associations between frailty indicators and fall appeared significant in frail group (OR, 5.42; 95% CI, 1.71 to 17.16) which again showed diminished relationship in prefrail group (Table 3).
Table 3.
Risks of cognitive decline, disability, fall and hospitalization for one year according to frailty status.*
Values are presented as odds ratio (95% confidence interval).
*Analyzed with logistic regression model. †Age and sex adjusted. ‡P < 0.05. §P > 0.05.
DISCUSSION
Adverse health-related outcomes in an elderly person can be crucial for the individual and their families that are strongly linked to quality of life and future mortality. In this study, frailty, as defined by validated phenotype at baseline, was associated with the likelihood of developing cognitive function decline, falls, hospitalization and disability in 12 months follow-up. There are various means of assessing frailty in the elderly. Ma et al.15) used Cardiovascular Health Study (CHS) index based on 5 domains and SOF frailty index based on 3 domains in previous study. These two indices of frailty showed similar odds ratios between frailty and disability and prevalence of frail patient in senior welfare centers in Korea as resulted previous our study.
As SOF frailty index with only three components (weight loss, inability to rise from a chair, and poor energy) is very simple, measurement of frailty using this index can seem to be insufficient to provide useful operationalization to frailty, but Ensrud et al.6) suggested that there was no difference between the SOF index and the CHS index in discriminating falls, disability, nonspine fracture or death.
In spite of former results that the SOF index is useful in the evaluation of frailty in the elderly, it seems to lack confidence in longitudinal characterization of change in frailty status over time because a change of at least 1 component can fluctuate frailty status within 3 categories as seen in Figure 1.
Of the participants, reduced energy level was the most answered component in frail and prefrail group. Hoyl GDS-5 is to be answered assuming that the symptom appeared in the past one week, whereas SOF index applied to the past one year. The variance might have occurred in these two different measures of depression although most of the participants who had depressive mood answered "no" to the question "Do you feel full of energy?"
Nevertheless, as frailty is a dynamic process involving change over time, longitudinal multiple assessments of the different components are often necessary and 3 components of SOF index could change each status in fluctuation. This means the frail status of older person at just assessment time is important for application of intervention to improve health status of the elderly.
We used IADL instead of basic ADL (BADL) to predict the disability in frail status. Of the two measures of physical disability included in the study of Ravaglia et al.,16) difficulty with IADL rather than ADL was an independent predictor of mortality. This may reflect the fact that the ADL index, taken as predictor of functional decline, is weaker than IADL because it captures disability only at the extreme end of the disabling process.
Hoyl GDS-517) showed the highest sensitivity (97.9%) over other depression scales compared to the 15-item GDS and we used this scale with supporting evidence of shorter time with similar results to GDS scales of more items.
As frailty status deteriorates, each adverse outcome incremented in risk factor and frailty has considerable value as a clinical concept. Frailty predicts 3 year incidence or progression of disability in both mobility and activities of daily living, independent of comorbid diseases, health behaviors, and psychosocial characteristics.18) The risk of individual mortality can be predicted better by frailty than by chronological age.19) Not surprisingly, frail people seem to have a significant lower quality of life.20) On the basis of US studies, it appears that frailty affects about 7% of people aged ≥ 65 years, and about 25-40% of those aged ≥ 80 years.21) Frailty leads to recurrent hospitalization, institutionalization, and death.
From study by Ma et al.,15) frail individuals tended to have lower education level, family income, and BMI, and tended to be living alone which was different from this study whereas age, number of chronic diseases, depressive symptoms, MMSE and fall showed concordance. These differences occurred from smaller number of participants in the follow-up study, and especially the subjects of our study are 110 persons who continue active participation in welfare program during past year among total 178 persons. This means the possibility that persons with lower education, family income, BMI would have high tendency to be lost during follow-up period.
Frailty study in association with increased risks of adverse health outcomes including falls, fractures, and mortality in elderly Caucasian women in the United states by Ensrud et al.22,23) suggests several reasons for this result. It suggests that frailty has been linked to declines in circulation levels of gonadal hormones,24) 25-hydroxyvitamin D, growth hormone, and insulin-like growth factor-1 (IGF-1),25) elevations in proinflammatory cytokines and coagulation factors,26) subclinical anemia,27) renal insufficiency,28) atherosclerosis, anorexia and malnutrition. Alternatively, frailty may be a marker of other conditions that increase the risk of falls, fractures, and mortality.
Ensrud et al.7) also provided a similar result on study of frailty indexes predicting falls, disability, fractures, and mortality in elderly men in the United States suggesting that the CHS index has been linked to specific alterations in physiological and biological pathways that may lead to multisystem impairment underlying the development of the clinical frailty syndrome.
In Samper-Ternent et al.29) study on relationship between frailty and cognitive decline over a 10-year period in older Mexican Ame ricans, a statistically significant association was found between frailty and subsequent decline in cognitive function. Also, they found that the risk of developing Alzheimer' s disease was 2.5 times as high when frailty was present at baseline in a short term follow-up of 3 years.30)
This study has several limitations. The participants were restricted to only 2 senior welfare center visitors that can be biased to a limited pool of the elderly. Of the participants, there were no cases of mortality which could be overcome by longer follow-up period. In each adverse outcome, prefrail group showed diminished correlation compared to the frail group, which suggests that longer observation time and more participants are necessary.
The major strength of our study is that is is the first attempt in Korea to find adverse outcomes after 1-year follow-up with relationships of frailty. It was hypothesized based on other studies conducted with different race and ethnicity and reached a result that the hypothesis could apply to Asians, especially elderly Koreans with age and sex adjustments.
In conclusion, the frailty status as evaluated by SOF frailty index predicts risk of falls, disability, hospitalization, and cognitive decline in the elderly, indicating that frail elderly should be identified in clinical practice with interventions to reduce the adverse geriatric consequences.
References
- 1.Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 2.Freedman VA, Crimmins E, Schoeni RF, Spillman BC, Aykan H, Kramarow E, et al. Resolving inconsistencies in trends in old-age disability: report from a technical working group. Demography. 2004;41:417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence: unifying the approach to geriatric syndromes. JAMA. 1995;273:1348–1353. [PubMed] [Google Scholar]
- 4.Soriano TA, DeCherrie LV, Thomas DC. Falls in the community-dwelling older adult: a review for primary-care providers. Clin Interv Aging. 2007;2:545–554. doi: 10.2147/cia.s1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyd CM, Xue QL, Guralnik JM, Fried LP. Hospitalization and development of dependence in activities of daily living in a cohort of disabled older women: the Women's Health and Aging Study I. J Gerontol A Biol Sci Med Sci. 2005;60:888–893. doi: 10.1093/gerona/60.7.888. [DOI] [PubMed] [Google Scholar]
- 6.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Cawthon PM, Stone KL, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168:382–389. doi: 10.1001/archinternmed.2007.113. [DOI] [PubMed] [Google Scholar]
- 7.Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57:492–498. doi: 10.1111/j.1532-5415.2009.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Won JW. Korea activities of daily living scale and Korea instrumental activities of daily living scale. J Korean Geriatr Soc. 2002;6(s1):93–104. (Korean text) [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Kwon YC, Park JH. Korean version of mini-mental state examination (MMSE-K) part I: development of the test for the elderly. J Korean Neuropsychiatr Assoc. 1989;28:125–135. [Google Scholar]
- 11.Williams-Russo P, Sharrock NE, Mattis S, Szatrowski TP, Charlson ME. Cognitive effects after epidural vs general anesthesia in older adults: a randomized trial. JAMA. 1995;274:44–50. [PubMed] [Google Scholar]
- 12.Hoyl MT, Alessi CA, Harker JO, Josephson KR, Pietruszka FM, Koelfgen M, et al. Development and testing of a five-item version of the Geriatric Depression Scale. J Am Geriatr Soc. 1999;47:873–878. doi: 10.1111/j.1532-5415.1999.tb03848.x. [DOI] [PubMed] [Google Scholar]
- 13.Sheikh JI, Yesavage JA, Brooks JO, 3rd, Friedman L, Gratzinger P, Hill RD, et al. Proposed factor structure of the Geriatric Depression Scale. Int Psychogeriatr. 1991;3:23–28. doi: 10.1017/s1041610291000480. [DOI] [PubMed] [Google Scholar]
- 14.Park HS, Deung Jung YJ, Lee CI, Oh JE, Hong SH, Cho CY. Comparing various short-form geriatric depression scales in elderly patients. J Korean Acad Fam Med. 2006;27:364–369. [Google Scholar]
- 15.Ma SH, Jeung KY, Hong SH, Shim EY, Yoo SH, Kim MY, et al. Correlation between frailty level and disability of the elderly and frailty related factors. Korean J Fam Med. 2009;30:588–597. [Google Scholar]
- 16.Ravaglia G, Forti P, Lucicesare A, Pisacane N, Rietti E, Patterson C. Development of an easy prognostic score for frailty outcomes in the aged. Age Ageing. 2008;37:161–166. doi: 10.1093/ageing/afm195. [DOI] [PubMed] [Google Scholar]
- 17.Weeks SK, McGann PE, Michaels TK, Penninx BW. Comparing various short-form Geriatric Depression Scales leads to the GDS-5/15. J Nurs Scholarsh. 2003;35:133–137. doi: 10.1111/j.1547-5069.2003.00133.x. [DOI] [PubMed] [Google Scholar]
- 18.Puts MT, Lips P, Deeg DJ. Static and dynamic measures of frailty predicted decline in performance-based and self-reported physical functioning. J Clin Epidemiol. 2005;58:1188–1198. doi: 10.1016/j.jclinepi.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 19.Mitnitski AB, Mogilner AJ, MacKnight C, Rockwood K. The mortality rate as a function of accumulated deficits in a frailty index. Mech Ageing Dev. 2002;123:1457–1460. doi: 10.1016/s0047-6374(02)00082-9. [DOI] [PubMed] [Google Scholar]
- 20.Puts MT, Shekary N, Widdershoven G, Heldens J, Lips P, Deeg DJ. What does quality of life mean to older frail and non-frail community-dwelling adults in the Netherlands? Qual Life Res. 2007;16:263–277. doi: 10.1007/s11136-006-9121-0. [DOI] [PubMed] [Google Scholar]
- 21.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 22.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Cawthon PM, Stone KL, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168:382–389. doi: 10.1001/archinternmed.2007.113. [DOI] [PubMed] [Google Scholar]
- 23.Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62:744–751. doi: 10.1093/gerona/62.7.744. [DOI] [PubMed] [Google Scholar]
- 24.Morley JE, Kaiser FE, Sih R, Hajjar R, Perry HM., 3rd Testosterone and frailty. Clin Geriatr Med. 1997;13:685–695. [PubMed] [Google Scholar]
- 25.Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol A Biol Sci Med Sci. 2002;57:M772–M777. doi: 10.1093/gerona/57.12.m772. [DOI] [PubMed] [Google Scholar]
- 26.Walston J, McBurnie MA, Newman A, Tracy RP, Kop WJ, Hirsch CH, et al. Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: results from the Cardiovascular Health Study. Arch Intern Med. 2002;162:2333–2341. doi: 10.1001/archinte.162.20.2333. [DOI] [PubMed] [Google Scholar]
- 27.Leng S, Chaves P, Koenig K, Walston J. Serum interleukin-6 and hemoglobin as physiological correlates in the geriatric syndrome of frailty: a pilot study. J Am Geriatr Soc. 2002;50:1268–1271. doi: 10.1046/j.1532-5415.2002.50315.x. [DOI] [PubMed] [Google Scholar]
- 28.Shlipak MG, Stehman-Breen C, Fried LF, Song X, Siscovick D, Fried LP, et al. The presence of frailty in elderly persons with chronic renal insufficiency. Am J Kidney Dis. 2004;43:861–867. doi: 10.1053/j.ajkd.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 29.Samper-Ternent R, Al Snih S, Raji MA, Markides KS, Ottenbacher KJ. Relationship between frailty and cognitive decline in older Mexican Americans. J Am Geriatr Soc. 2008;56:1845–1852. doi: 10.1111/j.1532-5415.2008.01947.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buchman AS, Boyle PA, Wilson RS, Tang Y, Bennett DA. Frailty is associated with incident Alzheimer's disease and cognitive decline in the elderly. Psychosom Med. 2007;69:483–489. doi: 10.1097/psy.0b013e318068de1d. [DOI] [PubMed] [Google Scholar]