Abstract
Context: Few population-based studies have examined the relationship between psychiatric and somatic or biomedical disorders.
Objective: We examined the effect of the presence or absence of any psychiatric disorder on somatic or biomedical diagnosis disorder costs. Guided by the Kaiser Permanente and Centers for Disease Control and Prevention Adverse Childhood Experiences (ACE) Study, we examined our administrative data to test if psychiatric disorder is associated with a higher level of somatic disorder.
Design: A dataset containing registration data for 205,281 patients younger than age 18 years was randomly selected from administrative data based on these patients never having received any specialized, publicly funded ambulatory, emergency or inpatient admission for treatment of a psychiatric disorder. All physician billing records (8,724,714) from the 16 fiscal years April 1993 to March 2009 were collected and grouped on the basis of presence or absence of any International Classification of Diseases (ICD) psychiatric disorder.
Main Outcome Measures: We compared 2 groups (with or without any psychiatric disorder: dependent variable) on the cumulative 16-year mean cost for somatic (biomedical, nonpsychiatric) ICD diagnoses (independent variable).
Results: Billing costs related to somatic and biomedical disorders (nonpsychiatric costs) were 1.8 times greater for those with psychiatric disorders than for those without psychiatric disorders. Somatic costs peaked before the age of 6 years and remained higher than the groupings without psychiatric disorders in each age range.
Conclusion: In support of the ACE study, ICD psychiatric disorders (as an index of developmental adversity) are associated with substantially greater ICD somatic disorders. The findings have implications for health care practice.
Introduction
The association between general health care costs and mental problems is emerging as an important topic in policy development related to reducing the burden of mental illness on society. Seligman1 proposed in 1989 that an epidemic of depression was on the horizon. A published study in our catchment indicates that psychiatric disorder is indeed epidemic.2 Furthermore, the health care cost reductions associated with health improvement are better for those with somatic or biomedical problems (eg, asthma) than in those with mental problems.3,4
As individuals develop, those with early adversity (eg, abuse and neglect) have a greater likelihood in adulthood of using health services more frequently—an effect modulated by psychiatric status.5 Childhood psychiatric conditions such as depression and substance abuse have a long-term economic cost and are estimated to reduce subsequent lifetime family income by $300,000 US, at a national cost of $1.2 trillion US.6 Felitti et al7 have studied extensively the association between childhood adversity and adult health status, with the finding that adversity-affected adults are at considerably higher risk of having serious health concerns. Here, we present population-based results that support the findings of Felitti et al's Adverse Childhood Experiences (ACE) study.
Materials and Methods
Health care in Canada is primarily universal. Medically necessary health services in each province include family physician visits and access to specialized ambulatory, emergency, and inpatient health treatment, including mental health, and are covered under public provincial health plans. In addition, family physicians serve as gatekeepers for specialty care. Most people who require mental health care are first served by their family physicians. For each patient visit, physicians bill the provincial health plan directly to receive payment for the services they deliver. Each billing includes at minimum a unique patient identifier, an International Classification of Diseases (ICD) diagnosis, and an associated visit cost.
The April 1993 through March 2009 data used in this study consisted of physician billings (Calgary Research Ethics Board ID 21695) for patients from the Calgary Zone in Alberta who were younger than age 18 years on their index visit. Physician billing data represented the records of all health services rendered to all individuals from the catchment sample who sought health care on a specified date for a specified problem and were assigned an ICD diagnosis.
The group under study consisted of those who had physician health care billings and did not have a personal health number associated with treatment by specialized, publicly funded ambulatory, emergency, or inpatient mental health services. The randomly selected files of physician billing data consisted of 205,281 unique individuals having 8,724,714 billing records submitted by regional physicians. These records included billing data related to somatic or biomedical and psychiatric diagnoses assigned by physicians. All diagnoses were based on ICD-9 or ICD-10 mental health diagnostic codes. The data formed two natural groups of individuals: those with a psychiatric diagnosis and those without any physician-assigned psychiatric diagnoses (no psychiatric diagnosis). Each of these groups had physical biomedical or somatic disorders that formed the basis for comparison.
Diagnosis-related costs were recorded in the dataset as the total amount paid by the provincial health plan to the physician for each visit. Physical (somatic and/or biomedical) diagnosis costs were summed across each group and did not include visit costs related to any psychiatric disorder billings. Psychiatric diagnosis costs were totaled separately.
Data Analysis
Groupings based on the presence or absence or any psychiatric disorder represented the dependent or outcome variable. Costs and visits for somatic or biomedical diagnoses represented the main independent variables. Age and sex represented covariates of analysis. Descriptive statistics were calculated as the mean per patient for visits and costs related to somatic or biomedical diagnoses (eg, subtracting billing costs for psychiatric diagnoses) by patient age and sex for each outcome group (those with or without psychiatric diagnoses). In the data shown in the results section, costs related to a somatic diagnosis were calculated independently of psychiatric diagnosis costs.
Results
Age ranged from younger than age 1 year to age 17 years. The sample consisted of 150,380 individuals with no psychiatric diagnosis and 54,901 with any psychiatric diagnosis. Approximately half of the sample was female (49%). There were no differences in the distribution of age or sex between the two groups.
Thirty-seven percent of the sample had a psychiatric disorder over the 16-year study period. The mean number of visits related to somatic or biomedical diagnoses for unique individuals in each grouping was as follows: no psychiatric diagnosis, 28; psychiatric diagnosis, 47. Those with a psychiatric disorder had between 1.7 times more visits for somatic disorders on average than those without a psychiatric disorder. Individual patients had an average of 5 visits during the study period related to treatment of psychiatric disorders, at an average cost of $380 per patient.
Figure 1 represents the mean cost of physician billing for somatic or biomedical diagnoses per unique individual for the 2 study groups. For those with any psychiatric disorder, the somatic or biomedical diagnosis costs were 1.8 times higher than those without psychiatric disorders.
Figure 1.
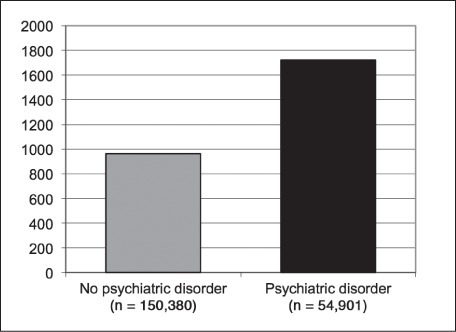
Mean physician billing cost related to a somatic or biomedical disorder.
There was, however, an age effect (Figure 2). Even though the relative ratios of cost in each age category were approximately the same, overall costs decreased as age increased and were greatest for preschool children. The decrease occurred because the sample was truncated when any patient reached the age of 18 years, thereby representing only pediatric physician visits.
Figure 2.
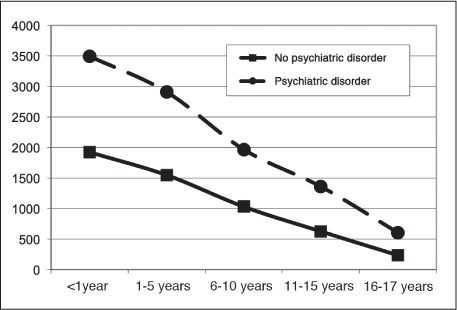
Mean somatic/biomedical disorder billing cost (Canadian dollars) per unique patient by age group for groups with and without any psychiatric diagnosis over the 16-year period.
Discussion
The ACE Study (www.acestudy.org) has described the relationship between health status in adulthood and reported adverse childhood experiences.8–10 The ACE Study has provided a great deal of information related to the reporting of adversity, present health status, and health economy. We are currently seeking how to implement the ACE survey in our publicly funded health system because of substantial health expenditure savings reported with the use of this survey. For example, at Kaiser Permanente in a sample of 125,000 adult patients in one department using such a questionnaire, routinely gathering this information was associated with a 35% reduction in doctor office visits in the subsequent year (Vincent Felitti, MD, personal communication; 2012 Apr 1).a
Furthermore, a recent study has identified the effect of psychiatric morbidity on mortality, noting that the burden of psychiatric illness goes on largely unattended and unnoticed.10 To our knowledge, no population-based studies to date have provided information about the relationship between psychiatric disorder and health status over time. However, in terms of developmental psychopathology, childhood adversity has long been considered a harbinger of psychiatric disturbance and disorder.
Of the randomly selected study group, 37% had a physician billing for a psychiatric disorder. Prior analysis of a 9-year and 16-year dataset, including adult and geriatric data, indicated that 46% of the randomly selected comparison group had a physician billing for a psychiatric disorder.2 Somatic and biomedical disorder costs among those in the psychiatric disorder group were higher than in the group with no psychiatric disorder.2 Furthermore, the psychiatric disorder rate was higher overall (46%) in the sample that included all ages,2 indicating that the somatic morbidity associated with psychiatric disorder increased with age. In our study, we observed that across childhood and adolescence the rate of contact with regional physicians decreased up to the age of 18 years (Figure 2). The psychiatric disorder group had a consistently higher proportion of biomedical and somatic disorder-related costs at each age. The age-related decrement represents the result of truncating all visit dates when any patient reached age 18 years. Hence, a patient who was age 17 years at the index visit would have accumulated fewer visits before his/her 18th birthday than a patient who was 1 year old at the index visit in the first year of the study (1994). Data inclusion was truncated for all patients when they turned 18 years old because this directly reflects the organization of our health care system, especially in psychiatry.
The results of the present large population-based study demonstrated the physical (somatic or biomedical) liability of having a psychiatric disorder in childhood and adolescence. The cost related to somatic or biomedical disorders, given any psychiatric diagnosis, were 1.8 times as high compared with the group with no psychiatric disorder. Similarly, the burden of a somatic or biomedical disorder given the presence of a psychiatric diagnosis also increased in proportion with age to 3.3 times higher in the previously reported sample that included all ages.2
The burden of somatic or biomedical disorders in the psychiatric disorder group emerged early in life (Figure 2) and much earlier than the investment we make in psychiatric care. Considering that the sample size in this study was approximately two thirds of the total base population of those younger than age 18 years in the catchment, the somatic or biomedical diagnosis-related cost burden having any psychiatric disorder becomes paramount, especially given the early-life onset of physical (somatic or biomedical) disorders. Our current dataset holds the potential to examine patterns of emergence and co-occurrence of somatic and psychiatric disorders over time. For example, preliminary results (unpublished data, 2010) indicate that neurotic and anxiety disorders are much more prevalent in the sample and, therefore, have the highest direct (psychiatric) and indirect (physical) physician billing costs in total, even though their per capita cost is comparatively less than other psychiatric diagnoses, such as organic brain syndromes and mental retardation.
There were several limitations of the study. Any physician billing could include costs associated with up to three diagnoses. If any one of these diagnoses was a psychiatric diagnosis, the total cost of that visit was assigned to the total mental health costs for that unique individual. As a result, the total health costs for each unique individual were marginally underestimated if there were additional somatic or biomedical diagnoses associated with a psychiatric diagnosis for a given visit. Multiple diagnoses, however, were associated with a minority of the physician billings. A second limitation was associated with the reliability and validity of the assignment of psychiatric diagnoses by the billing physicians. Compared with specialists, family physicians have limited psychiatric training (given the large number of unspecified psychiatric diagnoses). However, the same threats to validity and reliability were present in the assignment of all psychiatric diagnoses in each of the study groups. We acknowledge that diagnostic precision may be an issue in some instances. Finally, by excluding in the sampling process patients known to have received publicly funded, specialized ambulatory, inpatient, or emergency psychiatric services, the possible differences between the psychiatric and nonpsychiatric groups in this study have been minimized. We were not able to account for additional privately funded health care in either group, however, where available, privately funded health care is not the norm in Canada.
Psychiatric assessment and treatment, if required, should always include assessment and treatment of physical conditions.
Conclusion
The association between general somatic and biomedical health costs and the health care costs of psychiatric disorder is emerging as an important topic in policy development related to understanding and reducing the burden of mental illness on society.11 However, there have been few systematic population-based health care utilization studies. We examined the health costs in a pediatric population over a 16-year period. The main finding was that health costs of individuals with a psychiatric diagnosis were about twice as high on average per unique patient given any psychiatric diagnosis compared with those without a psychiatric diagnosis. Psychiatric billing costs independently added on to the costs of somatic or biomedical diagnoses. The physical (somatic and biomedical) disorders were directly comparable between the study groups with and without psychiatric disorders, and the ratio of the average costs per individual between these 2 groups over the 16-year period was the main finding of this study. This ratio (2:1) was lower than the ratio observed in the previous study of the 9-year period for a sample of all ages,2 including child, adult, and geriatric populations, suggesting that the physical burden of psychiatric disorder increases with age.
The type of physical problems and the relationship between patterns of biomedical or somatic disorders and specific types of psychiatric disorder remain to be examined. Whereas a specific pattern of association is beyond the scope of the present report, what has been established is the fundamental relationship between the biologic substratum and psychiatric disorder in a form that may be examined exhaustively in a population. The implications for policy and practice are self evident. Psychiatric assessment and treatment, if required, should always include assessment and treatment of physical conditions. Segregated systems of care may, in fact, be detrimental in terms of long-term outcome and more costly in managed health care.
The present dataset holds the potential to reveal the relationships among specific diagnostic groupings that develop and are observed over time. The order of costs by psychiatric diagnoses provides a logical point of entry to examine the patterns of psychiatric and concurrent or prodromal somatic burden that develop over time. Profiles and patterns may emerge from the combinations and permutations in these data, which permit the identification of standard clinical pathways together with their associated costs. Such analysis represents a classic roadmap problem, and given the large numbers of permutations and combinations, it would take many researchers many years to unravel. Hence, we are developing a standardized algorithm to make the time-dependent results from these data accessible to investigators. This information is beginning to form the empirical basis on which to study and measure future innovation related to optimization of clinical pathways.
The main policy implication of the study's results points to the universal integration of psychiatric and health care structures and processes. Our findings bring to the fore the call to action embodied in the 1977 observation by Engles,12 the father of biopsychosocial theory:
The dominant model of disease today is biomedical, and it leaves no room within this framework for the social, psychological, and behavioral dimensions of illness. A biopsychosocial model is proposed that provides a blueprint for research, a framework for teaching, and a design for action in the real world of health care.
Although Engle's theory has been refined and advanced over the years, it is our hope that the present study will facilitate detailed examination of the relationships among the “biopsycho” spheres of a representative population.
Disclosure Statement
This study was funded, in part, by the Norlien Foundation. The author(s) have no other conflicts of interest to disclose.
Acknowledgments
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
a Co-Principal Investigator, The Adverse Childhood Experiences (ACE) Study; San Diego, CA
References
- 1.Seligman MEP. Vol 9. Washington, DC: The G Stanley Hall Lecture Series; 1989. Why is there so much depression today? The waxing of the individual and the waning of the commons; pp. 77–96. p. [Google Scholar]
- 2.Cawthorpe D, Wilkes TC, Guyn L, Li B, Lu M. Association of mental health with health care use and cost: a population study. Can J Psychiatry. 2011;56(8):490–4. doi: 10.1177/070674371105600807. [DOI] [PubMed] [Google Scholar]
- 3.Wu P, Katic BJ, Liu X, Fan B, Fuller CJ. Mental health service use among suicidal adolescents: findings from a US national community survey. Psychiatr Serv. 2010 Jan;61(1):17–24. doi: 10.1176/ps.2010.61.1.17. [DOI] [PubMed] [Google Scholar]
- 4.Wade TJ, Guo JJ. Linking improvements in health-related quality of life to reductions in Medicaid costs among students who use school-based health centers. Am J Public Health. 2010 Sep;100(9):1611–6. doi: 10.2105/AJPH.2009.185355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yanos PT, Czaja SJ, Widom CS. A prospective examination of service use by abused and neglected children followed up into adulthood. Psychiatr Serv. 2010;61(8):796–802. doi: 10.1176/ps.2010.61.8.796. [DOI] [PubMed] [Google Scholar]
- 6.Smith JP, Smith GC. Long-term economic costs of psychological problems during childhood. Soc Sci Med. 2010 Jul;71(1):110–5. doi: 10.1016/j.socscimed.2010.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998 May;14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 8.Felitti VJ. Adverse childhood experiences and adult health. Acad Pediatr. 2009 May–Jun;9(3):131–2. doi: 10.1016/j.acap.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Brown DW, Anda RF, Edwards VJ, Felitti VJ, Dube SR, Giles WH. Adverse childhood experiences and childhood autobiographical memory disturbance. Child Abuse Negl. 2007 Sep;31(9):961–9. doi: 10.1016/j.chiabu.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 10.Brown DW, Anda RF, Felitti VJ, et al. Adverse childhood experiences are associated with the risk of lung cancer: a prospective cohort study. BMC Public Health. 2010 Jan 19;(10):20. doi: 10.1186/1471-2458-10-20. Erratum in: BMC Public Health 2010;10:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawrence D, Kisely S, Pais J. The epidemiology of excess mortality in people with mental illness. Can J Psychiatry. 2010;55(12):752–60. doi: 10.1177/070674371005501202. [DOI] [PubMed] [Google Scholar]
- 12.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–36. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]


