Abstract
Eosinophilic esophagitis (EoE) is a chronic esophageal disease increasingly recognized in adults for its gastrointestinal manifestations. This paper discusses a young woman with EoE who presented with persistent hiccups and intermittent dyspepsia. The patient was initially treated with trials of both H2 blocker and proton pump inhibitor. However, her hiccups resolved only after treatment with topical fluticasone. A repeat upper endoscopy while on steroid treatment demonstrated both histologic remission of EoE and resolution of esophageal trachealization. Our patient's clinical course supports an association between hiccups and EoE, suggesting that EoE be considered in the differential diagnosis of patients with refractory hiccups.
Key Words: Eosinophilic esophagitis, Esophagitis, Eosinophils, Esophagus, Hiccups
Introduction
Eosinophilic esophagitis (EoE) is a commonly recognized pediatric condition that has emerged as a disorder increasingly affecting adults. Although EoE has been documented in all ages, races and genders, the typical EoE patient is an adult male with prior history of atopy. EoE is characterized by chronic, immune/antigen-mediated esophageal dysfunction with eosinophil-predominant inflammation. Incidence rates of EoE have increased over the past decade beyond what would be expected by increased recognition alone [1, 2]. Recent studies have reported prevalences approaching 1:1,000 in adults [3]. Solid-food dysphagia is the most common presenting symptom in adults [4]. Food impaction, chest pain, upper abdominal pain, symptoms of gastroesophageal reflux disease (GERD) and globus have also been reported in some adults with EoE [5, 6]. However, hiccups have not been previously reported.
New consensus recommendations released in 2011 established a minimum peak value of 15 eosinophils/hpf as a requirement for a diagnosis of EoE with few exceptions [6]. Additionally, due to an increasing prevalence of proton pump inhibitor-responsive esophageal eosinophilia, therapeutic trials of proton pump inhibitor or pH monitoring were recommended to aid in distinguishing EoE from GERD.
Treatment of EoE incorporates both dietary and medical-based modalities. Studies have demonstrated both clinical and histologic response to (1) strict elemental diet, (2) diet restriction based on allergy testing, and (3) diet restriction based on eliminating the more common food allergens [6]. Corticosteroids have also been proven to be effective in treating EoE, however clinical and histologic features are known to return with discontinuation of therapy. Here we report the case of a 24-year-old female who was diagnosed with EoE with an atypical presentation.
Case Report
A 24-year-old woman was referred to our care in March 2011 with a 3-year history of persistent hiccups and mild, intermittent dyspepsia. Her symptoms began with episodic mild chest discomfort lasting one minute followed by bouts of hiccups. Over time, the hiccups progressed to up to 10 episodes per day. She had no prior medical history other than one admission for renal calculi, and her only prescription was birth control pills. She had no history of allergy and no known family history of illness as she was adopted.
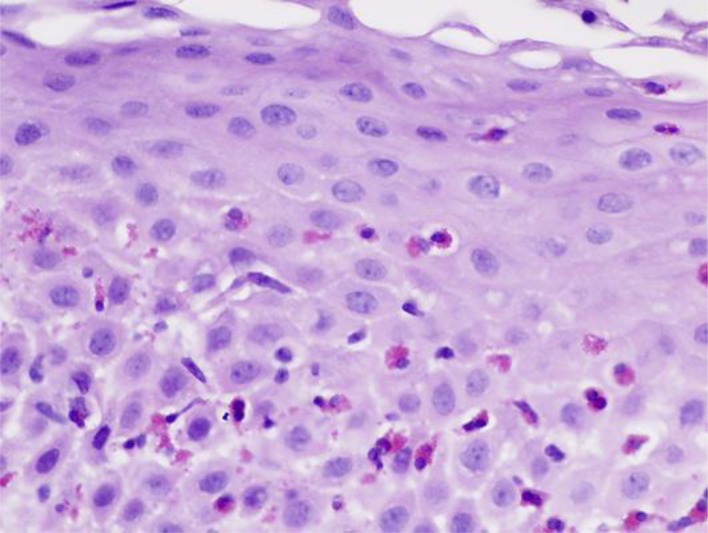
Six months before our evaluation she was treated empirically with ranitidine with no relief of her symptoms. She underwent esophagogastroduodenoscopy (EGD), which demonstrated trachealization of the esophagus, and biopsies from the distal esophagus showed significant eosinophilic infiltration. She was subsequently placed on a 6-week course of high-dose omeprazole (40 mg twice daily), with minimal relief of her symptoms. A follow-up EGD showed persistent trachealization and esophageal eosinophilia (peak eosinophil count of 23/hpf) consistent with a diagnosis of EoE (fig. 1).
Fig. 1.
Hematoxylin and eosin slide from esophageal biopsy shows large numbers of intraepithelial eosinophils as well as multiple degranulated eosinophils. Magnification = 40×.
The patient was started on topical swallowed fluticasone (440 μice daily). Her symptoms improved substantially within 1 week, with hiccups occurring fewer than 2 times per week. After 6 weeks her chest discomfort and hiccups had resolved completely. A repeat EGD while on treatment demonstrated resolution of trachealization, and biopsies showed histologic remission of EoE (peak eosinophil count of 5/hpf). Fluticasone was subsequently discontinued, but the patient developed recurrent hiccups within a few days. The hiccups resolved 2 weeks after reintroduction of fluticasone.
Discussion
Hiccups are common and usually resolve spontaneously. They are an involuntary spasmodic contraction of the diaphragm and intercostal muscles, resulting in sudden inspiration and closure of the glottis [7]. Multiple causes of hiccups have been described, including gastric or esophageal distention due to overeating or carbonated beverages, phrenic nerve irritation, central nervous system disorders, metabolic, postoperative and psychogenic disorders, medication side effects and reflux esophagitis [8]. The pathogenesis is unclear, but one proposed mechanism suggests that esophageal receptors send impulses via the vagal nerve to respiratory motor neurons, resulting in hiccups [9].
EoE is a chronic, immune/antigen-mediated esophageal disease characterized histologically by eosinophil-predominant inflammation and clinically by symptoms related to esophageal dysfunction [6]. Due to overlapping clinical features, the diagnosis of EoE requires distinction from GERD with a trial of a proton pump inhibitor or with pH monitoring. The most common presenting symptom in adults is dysphagia to solids [4]. Food impaction occurs in 33–54% of adults with EoE [10]. Hiccups have not been previously reported.
In our patient, symptoms and esophageal eosinophilia led to the initial suspicion of GERD and the initiation of acid-modifying therapy. Our patient achieved minimal relief with an H2 blocker or proton pump inhibitor, suggesting that hiccups were unlikely related solely to GERD. By contrast, the patient's clinical, endoscopic and histologic response to topical steroid therapy supports an association between hiccups and EoE and suggests that EoE be considered in the differential diagnosis of patients with refractory hiccups.
Grant Support
The International Gastrointestinal Eosinophil Researchers (TIGERS) Concept Award (support to P.A.B. and J.L.).
Disclosure Statement
The authors have no conflicts of interest.
References
- 1.Straumann A, Simon HU. Eosinophilic esophagitis: escalating epidemiology? J Allergy Clin Immunol. 2005;115:418–419. doi: 10.1016/j.jaci.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Hruz P, Straumann A, Bussmann C, et al. Escalating incidence of eosinophilic esophagitis: a 20-year prospective, population-based study in Olten County, Switzerland. J Allergy Clin Immunol. 2011;128:1349–1350. doi: 10.1016/j.jaci.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 3.Bonis P. Putting the puzzle together: epidemiological and clinical clues in the etiology of eosinophilic esophagitis. Immunol Allergy Clin North Am. 2009;29:41–52. doi: 10.1016/j.iac.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Mackenzie SH, Go M, Chadwick B, et al. Eosinophilic oesophagitis in patients presenting with dysphagia – a prospective analysis. Aliment Pharmacol Ther. 2008;28:1140–1146. doi: 10.1111/j.1365-2036.2008.03795.x. [DOI] [PubMed] [Google Scholar]
- 5.Dellon ES, Gibbs WB, Fritchie KJ, et al. Clinical, endoscopic, and histologic findings distinguish eosinophilic esophagitis from gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2009;7:1305–1313. doi: 10.1016/j.cgh.2009.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liacouras CA, Furuta GT, Hirano I, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011;128:3–20. doi: 10.1016/j.jaci.2011.02.040. [DOI] [PubMed] [Google Scholar]
- 7.Kolodzik PW, Eilers MA. Hiccups (singultus): review and approach to management. Ann Emerg Med. 1991;20:565–573. doi: 10.1016/s0196-0644(05)81620-8. [DOI] [PubMed] [Google Scholar]
- 8.Kahrilas PJ, Shi G. Why do we hiccup? Gut. 1997;41:712–713. doi: 10.1136/gut.41.5.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher MJ, Mittal RK. Hiccups and gastroesophageal reflux: cause and effect? Dig Dis Sci. 1989;34:1277–1280. doi: 10.1007/BF01537278. [DOI] [PubMed] [Google Scholar]
- 10.Desai TK, Stecevic V, Chang CH, et al. Association of eosinophilic inflammation with esophageal food impaction in adults. Gastrointest Endosc. 2005;61:795–801. doi: 10.1016/s0016-5107(05)00313-5. [DOI] [PubMed] [Google Scholar]