Abstract
Denosumab is a breakthrough biological drug approved by the Food and Drug Administration and European Medicines Agency for the treatment of osteoporosis in 2010. It is a fully human monoclonal antireceptor activator of nuclear factor kappa-B ligand antibody, which inhibits the activity of osteoclasts, resulting in an antiresorptive effect with a significant increase in bone mineral density. The FREEDOM (Fracture Reduction Evaluation of Denosumab in Osteoporosis every 6 Months) trial, comparing denosumab with no treatment in 7868 women with postmenopausal osteoporosis, showed an important reduction of fracture risk at hip, vertebral, and nonvertebral sites in the treated group, while no statistically significant difference in the incidence of adverse events was detected between denosumab and placebo groups. The specific action of denosumab directed against a key regulator of osteoclasts makes it a valuable tool in preventing the occurrence of skeletal events caused by bone destruction in patients with advanced malignancies. The drug was approved for postmenopausal osteoporosis in women at increased risk of fracture and for the treatment of bone loss associated with androgen deprivation therapy in men with prostate cancer.
Keywords: osteoporosis, denosumab, targeted therapy, BMD, antibody, RANK-L
Introduction
The aim of osteoporosis treatment is to reduce as far as possible the risk of bone fracture. Osteoporosis, the most common metabolic bone disease, is characterized by low bone mineral density (BMD) and microarchitectural deterioration of bone tissue with a consequent increase in the susceptibility to fragility fractures. It has become an increasingly important public health problem due to the rapidly aging population. Currently, every third postmenopausal woman and every fifth man older than 50 years suffer from osteoporosis.1
It should be important to identify the possible pathological mechanisms underlying bone fragility, especially in populations at risk such as the elderly and postmenopausal women. Bone strength, ie, resistance to fracture, depends not only on bone mass, but also on its spatial distribution and the intrinsic properties of the materials that constitute the bone.1,2
Data from the National Osteoporosis Risk Assessment study revealed that only 6.4% of postmenopausal women with an osteoporotic fracture had T-score (the standard deviation difference between the patient’s BMD and the mean BMD of a female young adult reference population) of less than −2.5 (World Health Organization definition of osteoporosis) in the year preceding the fracture.3,4
More than one-half (52%) of the women with fractures were osteopenic (T-score −2.5 to −1)3,4 and, similarly, the increase in BMD achieved through the treatments for osteoporosis seemed to account for only part of the reduction of fracture risk observed.4,5
Knowledge of the molecular bases of bone metabolism would be essential to formulate drugs that act not only on BMD but also on bone quality, especially in order to reduce fracture risk. Moreover, as described below, prescription of the therapy for osteoporosis, which must be specific to the individual patient, should be the result of the evaluation of multiple factors, such as age, sex, severity of osteoporosis, bone turnover markers (bone formation or resorption), patient compliance, allergies to medications, and contraindications or side effects of drugs.
Behind the choice of the most appropriate therapy, is the concept of bone as a dynamic tissue, which has the ability to adapt its shape and size in response to mechanical loads through modeling process, and to be constantly renewed by remodeling phenomenon.1,6 Remodeling process allows the skeleton to maintain mechanical integrity through constant osteoclastic resorption of damaged bone followed by osteoblast-mediated deposition and mineralization of new matrix.
Antiosteoporosis drugs can be classified on the basis of their action on bone remodeling.7 Antiresorptive drugs (such as bisphosphonates, raloxifene – a selective estrogen receptor modulator, and denosumab) decrease bone remodeling and reduce fractures by preserving skeletal microarchitecture and moderately increasing bone mass.1 Anabolic drugs, such as teriparatide or parathyroid hormone (PTH) 1–84, on the other hand, reduce fractures by enhancing remodeling. In addition to increasing BMD, they appear to repair bone microarchitecture and improve bone geometry.1 Strontium ranelate, available for osteoporosis in Europe, decouples the two processes, inhibiting bone resorption and stimulating bone formation.1 The evidence for this suggested mechanism of action of strontium ranelate has been largely acquired from in vitro and animal studies, where doses 30 times higher than those appropriate for men were used.8 However, bone anabolic effect has not been demonstrated in animals treated with doses of strontium ranelate comparable to the marketed dose,9 nor in human paired bone biopsies by clinical studies.1
A large body of scientific evidence derives from randomized controlled trials concerning the treatment of postmenopausal osteoporosis. Three different aminobisphosphonates (alendronate, risedronate, and zoledronate), teriparatide, strontium ranelate, and hormone replacement therapy – which is no longer recommended for the prevention or treatment of osteoporosis – were shown to be effective against both vertebral and nonvertebral fractures. Evidence of efficacy against vertebral fractures is available for ibandronate (an aminobisphosphonate), raloxifene, and PTH 1–84.1,10 Table 1 shows the site of action and effect on BMD and bone turnover of the most commonly used antiosteoporosis drugs.
Table 1.
Osteoporosis therapies in use1
| Drug class | Drugs | Action on bone remodeling | Action on bone mineral density | Action on vertebral and nonvertebral fracture risk |
|---|---|---|---|---|
| Antiresorptive agents | Aminobisphosphonates | ↓↓ | ↑ | V ↓; NV ↓ |
| Raloxifene | ↓ | ↑ | V ↓ | |
| Denosumab | ↓↓↓ | ↑ | V ↓; NV ↓ | |
| Uncoupling agent | Strontium ranelate | ↓ OC, ↑OB | ↑ | V ↓; NV ↓ |
| Anabolic agents | PTH 1–84 | ↑ | ↑↑ | V ↓; NV ↓ |
| Teriparatide | ↑ | ↑↑ | V ↓; NV ↓ |
Notes: ↑ increase; ↓ decrease; ↑↑ or ↓↓ strong increase or decrease, respectively. Adapted from International Journal of Clinical Rheumatology, June 2011, Vol. 6, No. 3, Pages 359–369 with permission of Future Medicine Ltd.
Abbreviations: OB, osteoblast; OC, osteoclast; NV, nonvertebral; PTH, parathyroid hormone; V, vertebral.
In women with osteoporosis, each 1% improvement in spine BMD (measured by dual X-ray absorptiometry) is expected to reduce vertebral fracture risk by about 4%. However, randomized trials of antiresorptive agents show that 1%–6% improvements in spine BMD reduce vertebral fracture risk by 35%–50%. Less than 20% of the decreased spine fracture risk produced by alendronate or raloxifene can be explained by improvement in spine BMD. The discrepancy is even greater during the first year or two of treatment when 1%–4% improvements in BMD are associated with 65%–68% decreases in spine fracture risk. Bisphosphonates continue to increase BMD but the reduction in fracture risk wanes to 20%–45%. Dual X-ray absorptiometry underestimates the change in bone density of spinal trabecular bone, which might explain part of the discrepancy between expected and observed reductions in spine fracture risk. Even more accurate measurements of BMD would not explain the rapid onset and later waning of effect despite gradually increasing BMD.11
The effect of drugs on nonspine fracture risk is more complex and cannot be predicted from changes in dual X-ray absorptiometry BMD. Long-term use (>10 years) of estrogen, for example, has been associated with >50% reduction in risk of hip and wrist fracture, which could not be explained by improvements in BMD, and increased section modulus versus nonusers with a net increase in predicted femoral neck strength despite losing about 0.4% per year in femoral neck BMD.12 PTH reduces spine fracture risk and this effect is more completely explained by improvement in spine BMD. This suggests that sustaining increased BMD produced by PTH may maintain long-term reduction in fracture risk.
The choice of the most appropriate therapy for individual patients should be based on the level of turnover rate indicated by biochemical markers, therefore preferring an anticatabolic drug in the case of high bone turnover postmenopausal woman and an anabolic or decoupling drug in an old patient with low turnover indices or a very low spinal and/or hip BMD. Importantly, patients’ compliance with medical therapy should be considered when choosing drugs with a certain frequency of administration.1
Alendronate, risedronate, and ibandronate were marketed with administration schedules that increasingly simplified oral therapy from once daily to weekly and then to monthly. A third-generation bisphosphonate, zoledronate, is provided in the form of a brief intravenous infusion administered yearly. The therapeutic plan for PTH involves daily subcutaneous administration performed at the same time for a maximum period of 24 consecutive months overall. Denosumab, the latest one on the market, requires a subcutaneous injection every 6 months.
Moreover, osteoporosis type (postmenopausal, senile, or secondary to pathologies or to the use of drugs), potential side effects, allergies, drug-specific contraindications, and the cost of treatment should be considered.1
The different drug classes: mechanisms of action
Bisphosphonates
Bisphosphonates are antiresorptive agents which act via the inhibition of osteoclasts, leading to reduced bone turnover, increased bone mass, and improved mineralization.13
Bisphosphonates are chemically stable analogues of inorganic pyrophosphate; publications of their biological effects began in 1969.14 Studies on the role of inorganic pyrophosphate as the body’s natural “water softener” in the control of soft tissue and skeletal mineralization led to the need to find inhibitors of calcification that would resist hydrolysis by alkaline phosphatase.14 The observation that inorganic pyrophosphate and bisphosphonates could not only retard the growth but also the dissolution of hydroxyapatite crystals prompted studies on their ability to inhibit bone resorption.14 Although inorganic pyrophosphate was unable to do this, bisphosphonates turned out to be remarkably effective inhibitors of bone resorption in both in vitro and in vivo experimental systems, and eventually in humans. As more potent bisphosphonates were synthesized and studied, it became apparent that physicochemical effects were insufficient to explain their biological effects and that cellular actions must be involved. Despite many attempts, it was not until the 1990s that their biochemical actions were elucidated. Selectively taken up and adsorbed to mineral surfaces in bone, bisphosphonates are internalized by the bone-resorbing osteoclasts and interfere with specific biochemical processes.
Bisphosphonates can be classified into at least two groups with different molecular modes of action. The simpler nonnitrogen-containing bisphosphonates (such as etidronate and clodronate) can be metabolically incorporated into non-hydrolysable analogues of adenosine triphosphate, which interfere with adenosine triphosphate-dependent intracellular pathways.14 The more potent nitrogen-containing bisphosphonates (including pamidronate, alendronate, risedronate, ibandronate, and zoledronate) are not metabolized in this way but inhibit key enzymes of the mevalonate/cholesterol biosynthetic pathway, such as farnesyl pyrophosphate synthase. They therefore interfere with geranylgeranylation (attachment of the lipid to regulatory proteins) and with the biosynthesis of isoprenoid compounds (notably farnesol and geranylgeraniol) that are required for posttranslational prenylation of small guanosine triphosphate-binding proteins (which are also guanosine triphosphatases), essential intracellular messengers, thus causing osteoclast inactivation. 13,14 Loss of geranylgeranylation leads to osteoclast apoptosis,15,16 disruption of the actin cytoskeleton, and altered membrane trafficking.13,17–19 This mechanism is responsible for nitrogen-containing bisphosphonate suppression of osteoclastic bone resorption and reduction of bone turnover, which leads to fracture prevention.13
Because of the appearance in humans of gastrointestinal adverse events after oral administration of nitrogen-containing bisphosphonates,20 the effects of oral bisphosphonates were examined in special studies in animals. Suprapharmacologic doses of alendronate administered orally to rats have been reported to induce gastric and esophageal erosions and ulcerations, as well as delay healing of indomethacin-induced gastric erosions. These effects were not attributable to changes in gastric acid secretion or prostaglandin synthesis, but are thought to be due to a topical irritant effect. Similar effects were reported with etidronate, risedronate, and tiludronate when given at pharmacologically equivalent doses.13,21–23
Accumulation of the upstream metabolite, isopentenyl pyrophosphate, as a result of inhibition of farnesyl pyrophosphate synthase may be responsible for immunomodulatory effects on gamma delta T cells, and can also lead to production of another adenosine triphosphate metabolite called ApppI, which has intracellular actions.14
Bisphosphonates are established as the treatments of choice for various diseases of excessive bone resorption, including Paget’s disease of bone, skeletal complications of malignancy, and primarily osteoporosis.
Recently, it has been suggested that in addition to inhibiting osteoclasts, bisphosphonates (specifically alendronate) may also promote osteoblast proliferation and maturation.4,24 The evidence base for bisphosphonates in the prevention of fracture in postmenopausal women is well established.4 Treatment with alendronate 10 mg/day resulted in statistically significant reductions in vertebral, nonvertebral, hip, and wrist fractures in patients with prior osteoporotic fracture or low BMD. For those patients without osteoporotic fracture or low BMD, treatment with alendronate resulted in a significant reduction in vertebral, but not other sites, fracture.4,25 Similar is the antifracture efficacy of risedronate 5 mg/day, although the reduction in wrist fractures in patients with prior fracture or low BMD was not statistically significant and there was no significant benefit in patients with normal BMD.4,26 Treatment with a once-yearly infusion of zoledronate (5 mg) significantly reduces the risk of vertebral, nonvertebral, hip, and wrist fracture in postmenopausal women with osteoporosis.4,27 In contrast, ibandronate in women with postmenopausal osteoporosis has shown a significant reduction in vertebral fracture only.4,28
Bisphosphonates improve trabecular microarchitecture; however, they have a relatively small effect on cortical bone. Trabecular microarchitecture is improved (greater bone volume, greater trabecular thickness, decreased trabecular spacing) after 2–3 years of alendronate treatment compared with placebo,29 or after 1 year of treatment with risedronate.30
In regards to the optimal treatment period, it should be considered that both alendronate and zoledronate bind strongly to the bone matrix and become internalized within bone; therefore, suppression of bone resorption continues even after treatment ends. There have been recent concerns that long-term suppression of bone remodeling and increased mineralization may result in detrimental changes to bone quality and accumulation of damage.4,31
Postmenopausal osteoporosis is a chronic disease requiring long-term management. While most antiosteoporotic treatments have been tested in 3–5-year studies, it should be crucial to assess the long-term safety and efficacy of these agents.32
Strontium ranelate
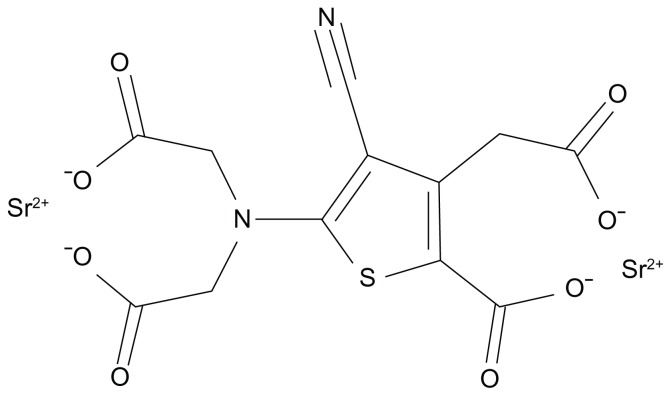
Strontium ranelate is a divalent strontium salt comprised of two molecules of stable strontium and one molecule of ranelic acid (Figure 1).33,34 It is a bone-seeking agent capable of increasing bone formation and reducing bone resorption, thereby uncoupling and rebalancing bone turnover in favor of bone formation.33–35
Figure 1.
Strontium ranelate structure.
Strontium ranelate has been shown to increase bone formation in vitro, enhancing preosteoblastic cell replication and osteoblastic differentiation and decreasing abilities of osteoblasts to induce osteoclastogenesis via the calcium-sensing receptor and an increase in the osteoprotegerin (OPG)/ receptor activator of nuclear factor kappa-B (RANK) ligand (RANKL) ratio.36 In human primary osteoblasts, strontium ranelate downregulated the expression of RANKL (which induces the differentiation of mature osteoclasts and increases osteoclast survival) and enhanced OPG expression (which inhibits RANKL-induced osteoclastogenesis), thus reducing osteoclastogenesis.34
Strontium, like calcium, acts as an agonist at the calcium-sensing receptor, promoting replication,36 differentiation,36,37 and survival36 of rodent37,38 or human36 primary osteoblasts. The drug triggers mitogenic signals, such as the activation of protein kinase C and p38 mitogen-activated protein kinase,39 and enhances the expression of c-Fos and EGR-1 genes, involved in osteoblast replication.37 The drug may act independently of the calcium-sensing receptor by protecting primary osteoblasts against apoptosis, thereby promoting osteoblastogenesis – partly via extracellular signal-related kinases 1/2 and Akt signaling – and prostaglandin E2 production.34,40
In rats,8 2 years’ treatment with strontium ranelate increased bone resistance (assessed by a compression test) and trabecular and cortical bone mass (as shown by ash weight and areal BMD in the vertebra and femur), with an improvement in bone microarchitecure.8,34 Similar effects were observed in women with postmenopausal osteoporosis in whom oral administration of strontium ranelate 2 g/day led to continued increases in BMD at all sites, proving efficacy against vertebral and nonvertebral fracture over 5 years, as demonstrated in the SOTI (Spinal Osteoporosis Therapeutic Intervention) trial41 and in the TROPOS (Treatment of Peripheral Osteoporosis) trial,42,43 though many women required longer-term treatment.32 No studies have been performed on strontium ranelate efficacy on men.
PTH
Until the advent of teriparatide (human recombinant PTH 1–34), the only available therapies for the treatment of osteoporosis worked by primarily inhibiting bone resorption (bisphosphonates, raloxifene, and estrogen), which decrease the rate of bone turnover by reducing the level of bone resorption with a subsequent reduction of bone formation activity.44,45
There is evidence from randomized controlled trials on the efficacy of anti-resorptives in reducing the risk of fracture, but none of these agents completely abolish fracture risk. Although they reduce fracture risk, particularly in the spine, there is no increase in bone formation or restoration of architectural bone tissue damage after treatment.46 Enhancement of bone formation may be provided by anabolic therapies.
PTH, the major hormonal regulator of calcium homeostasis, is a potent stimulator of bone formation and can restore bone to an osteopenic skeleton when administered intermittently. 1 Osteoblasts are the primary target cells for the anabolic effects of PTH in bone tissue. Anabolic effects of PTH on bone have been demonstrated in animals and humans by numerous measurement techniques including BMD and bone histomorphometry. Recently, two-dimensional and three-dimensional assessments of cancellous bone structure have shown that PTH can reestablish lost trabecular connectivity in animals and humans by a novel mechanism in which trabeculae are first thickened and then split by longitudinal tunneling.47
These results provide new insight into the positive clinical effects of PTH in osteoporosis. In recent randomized controlled clinical trials of intermittent PTH treatment, PTH decreased incidence of vertebral and nonvertebral fractures in postmenopausal women. Thus, PTH shows strong potential as therapy for osteoporosis. However, two-dimensional and three-dimensional structural analysis of advanced osteopenia in animals has shown that there is a critical limit of trabecular connectivity and bone strength below which PTH cannot completely reverse the condition. Given that PTH treatment fails to completely restore trabecular connectivity and bone strength in animals with advanced osteopenia, early treatment of osteoporosis appears important and efficacious for preventing fractures caused by decreased trabecular connectivity.48
The beneficial effect of introducing a treatment with antiresorptives after a treatment course with teriparatide or PTH has been demonstrated and is supported by a good rationale. Teriparatide increases bone mass but, at the same time, the new bone is less mineralized. Treatment with antiresorptives after teriparatide prevents accelerated osteoclastic resorption of the new bone tissue built during teriparatide therapy, increases mineralization, and rapidly lowers cortical porosity; this leads to further increases in BMD. The cost of teriparatide treatment is considerably higher than that of antiresorptives. For this reason, its use is indicated for patients with severe osteoporosis; in Italy, for example, teriparatide is fully reimbursed in patients with a new vertebral or hip fracture while on chronic treatment with antiresorptives or in patients never treated with antiresorptives with three or more vertebral or hip fractures.1,49 Contrary to bisphosphonates, the effect of which persists for many months after drug withdrawal,50 the protective action of teriparatide on BMD vanishes with time in both genders but not up to the baseline values.51,52
Bazedoxifene
Bazedoxifene is a novel third-generation selective estrogen receptor modulator, a molecule developed to act as estrogen receptor agonists in some tissues (eg, bone) and as estrogen receptor antagonists in others, such as breast and endometrium, in order to reduce the risk of breast and endometrial cancers that would be induced by hormone replacement therapy.53,54
Two large Phase III clinical trials54,55 showed that bazedoxifene, as well as raloxifene, increased BMD, decreased levels of bone turnover markers, and significantly reduced the risk of new vertebral fractures in postmenopausal women compared with placebo. Although the incidence of nonvertebral fractures with bazedoxifene or raloxifene did not differ significantly from that with placebo, a post hoc analysis of a subgroup of women at higher fracture risk revealed that bazedoxifene significantly reduced the nonvertebral fracture risk relative to placebo and raloxifene. Bazedoxifene also improved the lipid profile by reducing the serum concentrations of total cholesterol and low-density lipoprotein cholesterol, with an increase in the serum level of high-density lipoprotein cholesterol. The incidences of vasodilatation (hot flushes), leg cramps, and venous thromboembolic events were significantly higher with bazedoxifene and raloxifene compared with placebo. There was no evidence of endometrial and breast stimulation with bazedoxifene. Taking advantage of the favorable effects of bazedoxifene on the breast and endometrium, the pairing of bazedoxifene with conjugated estrogens is under investigation for the treatment of menopausal symptoms and prevention of postmenopausal osteoporosis. A Phase III trial showed that combination therapy of bazedoxifene and conjugated estrogens significantly increased BMD and decreased bone turnover markers, with relief of hot flushes and improvement of vaginal atrophy.54
Although bazedoxifene is a promising new therapy for patients with osteoporosis, further clinical investigations of long-term treatment with this selective estrogen receptor modulator are needed to evaluate the prevention of osteoporotic fractures, breast cancers, endometrial cancers, and cardiovascular events. When treating patients with osteoporosis, estrogens and selective estrogen receptor modulators have effects not only on bone metabolism, but also on the breast, endometrium, and lipid metabolism. Before starting treatment, a risk–benefit assessment should be performed for each patient with osteoporosis.54
Denosumab
Background
The principal regulator of bone resorption is the RANKL/ RANK/OPG pathway. RANKL is a transmembrane and soluble protein that is highly expressed by osteoblasts;56,57 its receptor, RANK, is located on the cell membrane of osteoclasts and preosteoclasts.57,58 RANKL–RANK binding stimulates the formation, activity, and survival of osteoclasts, resulting in increased bone resorption.59
OPG is a naturally occurring, soluble, nonsignaling “decoy receptor” for RANKL. By binding to RANKL and preventing its interaction with RANK, OPG inhibits osteoclast formation,59,60 activity,61,62 and survival,63 thereby reducing bone resorption.57,60
An increase of RANKL in proportion to OPG is associated with the development of postmenopausal osteoporosis and other skeletal disorders that include multiple myeloma, metastatic bone disease, treatment-related bone loss, rheumatoid arthritis, and Paget’s disease of bone.57,59,64,65
Development of RANKL inhibitors
The understanding of this pathway dates back to the end of the 1990s, Amgen (Amgen Inc, Thousand Oaks, CA) researchers identified in rats a gene sequence able to influence bone metabolism.60,66 Transgenic mice in which they induced the hepatic expression of the protein derived from that sequence resulted in a profound yet nonlethal osteopetrosis, coincident with a decrease in later stages of osteoclast differentiation.60 These same effects were observed upon administration of recombinant OPG into normal mice. Recombinant OPG was shown to block osteoclast differentiation from precursor cells in vitro.60 In vivo, it stopped ovariectomy-associated bone loss in rats. In vivo and in vitro data showed that OPG could act as a soluble factor in the regulation of bone mass and be of use in the treatment of osteoporosis associated with increased osteoclast activity.60
The Amgen research group identified a protein, which they called “OPG ligand.”67 The Snow Brand (Snow Brand Milk Products Co, Ltd, Tokyo, Japan) researchers isolated the same OPG-binding protein, and by comparing gene sequences discovered that it was identical to a previously described protein named RANKL or tumor necrosis factor-related activation-induced cytokine.68 Subsequently the laboratories of Amgen analyzed osteoclast precursor cells and isolated RANK protein, which was discovered to be RANKL receptor.69
While transgenic mice knockout for RANK or RANKL developed severe osteopetrosis, the overexpression of RANKL caused an increase in osteoclasts and a reduction in bone strength, and thus caused osteoporosis.70
Several studies showed that pathological loss of bone mass, a typical example of postmenopausal osteoporosis, is associated with increased RANKL levels and the consequent hyperactivation of osteoclasts.63 Moreover, RANKL levels in postmenopausal women are directly proportional to bone turnover markers, such as serum C-telopeptide of collagen type 1 and urinary N-telopeptide of collagen type 1 (NTX) – degradation products of collagen type 1 released into circulation during resorption of bone matrix.71 Estrogen deficiency is also associated with an increment of osteoclasts and RANKL levels.71 This evidence led to the development of targeted molecules specifically interacting with RANK/RANKL/ OPG pathway.
The entry of denosumab
Denosumab is a fully human monoclonal antibody of the immunoglobulin G2 isotype with a high affinity and specificity for RANKL. By binding RANKL, denosumab prevents its interaction with RANK, in much the same way as OPG, resulting in a decrease in bone resorption.
Pharmacokinetics of denosumab
The pharmacokinetics of denosumab are nonlinear with dose, similar to other fully human monoclonal antibodies. In healthy postmenopausal women given subcutaneous denosumab in varying doses, three phases were identified: (1) a prolonged absorption phase with maximum serum concentration observed at 5–21 days postdose, increasing as dose increased; (2) a prolonged phase, with serum halflife as long as 32 days with maximum dose; and (3) a rapid terminal phase when serum concentration dropped below 1000 ng/mL.72
Efficacy and safety studies
The effect on bone remodeling of denosumab was assessed in a Phase I study72 by measurement of bone turnover markers, such as NTX, marker of bone resorption, and bone-specific alkaline phosphatase, a marker of bone formation. Forty-nine healthy postmenopausal women were treated with a single dose of subcutaneous denosumab 0.01, 0.03, 0.1, 0.3, 1.0, or 3.0 mg/kg or placebo, and followed for up to 6 months in all cohorts and as long as 9 months in the cohorts receiving the three highest doses.57,72 A reduction in NTX levels was observed that was dose-dependent, rapid (within 12 hours), profound (up to 84% decrease), sustained (for up to 6 months), and reversible with discontinuation. Reduction of bone-specific alkaline phosphatase was observed later than with NTX and was less pronounced.
The efficacy and safety of denosumab were evaluated in a Phase II randomized placebo-controlled study in postmenopausal women with low BMD, defined as lumbar spine T-score of −1.8 to −4.0 or total hip or femoral neck T-score of −1.8 to −3.5.57,73–74 A total of 412 women were randomized to receive subcutaneous denosumab 6, 14, or 30 mg every 3 months or 14, 60, 100, or 210 mg every 6 months, open-label oral alendronate 70 mg once a week, or placebo. The primary endpoint was the percentage change in lumbar spine BMD at 12 months compared to baseline. Other endpoints included the percentage change from baseline in BMD at the total hip, femoral neck, distal one-third radius, and assessment of bone turnover with serum C-telopeptide of collagen type 1, urinary NTX, and bone-specific alkaline phosphatase. At 12 months, denosumab treatment was associated with a significant lumbar spine BMD increase of 3.0%–6.7%, depending on the dose and dosing interval, with smaller significant BMD increases observed at other skeletal sites.73 BMD increases at the total hip and distal one-third radius with subcutaneous denosumab 30 mg every 3 months and 60 mg every 6 months were greater than with open-label alendronate.
Treatment with denosumab resulted in a dose-dependent, rapid, sustained, and reversible suppression of bone turnover markers.57 The data at 24 months supported and extended the findings at 12 months, with continuing increases in BMD and suppression of bone turnover markers.74
The study was extended for 24 months beyond the initial 24 months.75 Patients originally randomized to denosumab were treated with subcutaneous denosumab 60 mg every 6 months, placebo, or placebo for 12 months followed by retreatment with subcutaneous denosumab 60 mg every 6 months for 12 months. Open-label alendronate patients discontinued alendronate therapy after 24 months and received no additional drug therapy. The original placebo group was maintained for the entire 48 months. Continuous denosumab treatment for 48 months increased BMD at the lumbar spine (9.4%–11.8% compared with baseline) and total hip (4.0%–6.1% compared with baseline), with consistent suppression of bone turnover markers for the duration of the study. Discontinuation of denosumab after 24 months of treatment was associated with a BMD decrease of 6.6% at lumbar spine and 5.3% at total hip within 12 months of discontinuation.57
Retreatment with denosumab 12 months after discontinuation increased BMD to an extent similar to what was observed with initial treatment (BMD at lumbar spine increased 9.0% and at total hip increased by 3.9% compared with original baseline values).
Bone turnover marker levels increased with discontinuation of denosumab and decreased with retreatment. Discontinuation of alendronate at 24 months resulted in a modest decrease in BMD at lumbar spine by 48 months, with a greater decrease in BMD at total hip and distal one-third radius; bone turnover marker levels increased, but remained below baseline at 48 months. The initial 4-year study was extended an additional 4 years to evaluate the efficacy and safety of denosumab with up to 8 years of continuous exposure. A preliminary interim analysis after 2 years of the extension study (total of 6 years of denosumab therapy), with all patients switched to open-label denosumab at a dose of 60 mg subcutaneously every 6 months, showed that BMD at lumbar spine increased 13.3% compared with baseline, with sustained reductions in serum C-telopeptide of collagen type 1 and bone-specific alkaline phosphatase.75 No patient developed neutralizing antibodies to denosumab.57
FREEDOM (Fracture Reduction Evaluation of Denosumab in Osteoporosis every 6 Months) was a large 3-year Phase III clinical trial in 7868 postmenopausal women with osteoporosis who were randomized to receive either subcutaneous denosumab 60 mg (n = 3902) or placebo (n = 3906) every 6 months.76 The primary efficacy endpoint was new vertebral fractures at 36 months, with secondary endpoints that included time to first hip and non-vertebral fractures. Study subjects, between the ages of 60 and 90 years, had a baseline T-score at lumbar spine or total hip between −2.5 and −4.0, with approximately 23% having at least one prevalent vertebral fracture at time of entry into the study. Treatment with denosumab was associated with a statistically significant 68% reduction in the risk of new vertebral fractures compared with placebo (2.3% denosumab versus 7.2% placebo, P < 0.0001), 40% reduction in the risk of hip fractures (0.7% denosumab versus 1.2% placebo, P = 0.036), and 20% reduction in the risk of nonvertebral fractures (6.5% denosumab versus 8.0% placebo, P = 0.011).57,76 There was no increase in the risk of cancer, infection, cardiovascular disease, delayed fracture healing, or hypocalcemia, and there were no cases of osteonecrosis of the jaw and no adverse reactions to the injection of denosumab.
DEFEND (Denosumab Fortifies Bone Density) was a Phase III trial evaluating the efficacy and safety of denosumab in 332 postmenopausal women with low bone mass (osteopenia). Postmenopausal women with lumbar spine T-scores between −1.0 and −2.5 were randomized to receive subcutaneous denosumab 60 mg every 6 months or placebo. 77 The primary efficacy endpoint was percentage change from baseline in lumbar spine BMD measured by dual X-ray absorptiometry at 24 months compared to placebo. Denosumab significantly increased BMD at lumbar spine compared with placebo at 24 months (denosumab 6.5% versus placebo −0.6%, P < 0.0001), as well as at total hip, distal one-third radius, and total body (P < 0.0001 for each compared with placebo), with a significant decrease in bone turnover markers compared with placebo. The safety profile was similar to placebo, except for a slightly higher incidence of cellulitis and exanthema. Eczema was reported in 3.0% of denosumab-treated patients compared with 1.7% in the placebo group (P < 0.001); cellulitis as a serious adverse event was more common with denosumab (0.3%) than placebo (<0.1%).
DECIDE (Determining Efficacy: Comparison of Initiating Denosumab Versus Alendronate) was a 1-year Phase III double-blind, double-dummy noninferiority trial in 1189 postmenopausal women with lumbar spine or total hip T-score of −2.0 or less who were randomized to receive subcutaneous denosumab 60 mg every 6 months plus weekly oral placebo or oral alendronate 70 mg weekly plus placebo subcutaneous injections every 6 months.78 The primary endpoint was percentage change from baseline of total hip BMD at 12 months in subjects treated with denosumab compared with alendronate. At 12 months, there was a significantly greater BMD increase with denosumab compared with alendronate at total hip (denosumab 3.5% versus alendronate 2.6%, P < 0.0001) and all other measured skeletal sites, with treatment difference 0.6% at femoral neck, 1.0% at trochanter, 1.1% at lumbar spine, and 0.6% at distal one-third radius (P < 0.0002 for all sites). There was a statistically significant greater reduction in bone turnover markers with denosumab compared with alendronate.
STAND (Study of Transitioning from Alendronate to Denosumab) was a 1-year Phase III double-blind, active-controlled, double-dummy study in 504 postmenopausal women being treated with alendronate, with lumbar spine or total hip T-score between −2.0 and −4.0.79 Subjects were randomized to receive subcutaneous denosumab 60 mg every 6 months or continuing oral alendronate 70 mg weekly. The primary endpoint was percentage change in BMD at total hip at 12 months for denosumab compared to alendronate. At 12 months, there was a statistically significant greater increase in BMD with denosumab compared with continuing alendronate at total hip (denosumab 1.90%, alendronate 1.05%, P < 0.0001), lumbar spine, and distal one-third radius. Discontinuing denosumab (at a dose of 210 mg) after 24 months resulted in a decrease in BMD in the following year comparable to the gains in BMD with 24 months of therapy.75 Denosumab has a declining residual effect over 1 year, a period called offset time.80
Table 2 provides a summary of the principal randomized controlled trials conducted with denosumab.
Table 2.
Phase III clinical trials of denosumab for the treatment of postmenopausal osteoporosis or osteopenia58
| Study | Aim | Control group | Mean age at baseline (years) | Mean lumbar spine T-score at baseline | Primary endpoint | Sample size (subjects) | Study period (years) | Efficacy | Safety: adverse events and serious adverse events |
|---|---|---|---|---|---|---|---|---|---|
| FREEDOM | Treatment of PMO | Placebo | 72.3 | −2.8 | New vertebral fractures at 36 months | 7868 | 3 | ↓ vertebral fracture risk | >cellulitis and eczema |
| DEFEND | Prevention of PMO | Placebo | 59.4 | −1.6 | Lumbar spine BMD at 24 months | 332 | 2 | ↑ BMD | >infections |
| DECIDE | Comparison of denosumab and alendronate | Alendronate | 64.4 | −2.6 | Total hip BMD at 12 months | 1189 | 1 | > ↑ BMD | – |
| STAND | Switch from alendronate to denosumab | Continuing alendronate | 67.6 | −2.6 | Total hip BMD at 12 months | 504 | 1 | ↑ BMD with switch to denosumab | – |
Note:>: more in the denosumab group than in the other group. Data from Hsu H, Lacey DL, Dunstan CR, et al. Tumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligand. Proc Natl Acad Sci U S A. 1999;96(7):3540–3545.
Abbreviations: BMD, bone mineral density; PMO, postmenopausal osteoporosis.
Clinical applications of denosumab
Denosumab has been approved for treatment of postmenopausal osteoporosis, as the data of clinical trials showed antifracture efficacy of denosumab to be at least as good as current therapeutic agents in the treatment of postmenopausal osteoporosis and is associated with excellent tolerability. It may be particularly important for patients with gastrointestinal contraindications or side effects with oral bis phosphonates and for patients with malabsorption.57 The long dosing interval of 6 months is likely to be attractive to patients who have difficulty with the more frequent and sometimes bothersome requirements for oral bisphosphonate therapy. The subcutaneous route of administration expands the potential locations for drug administration to any physician’s office, as compared with intravenous bisphosphonates, which are typically given at an infusion center or office with staff trained in infusion therapy.57
The clinical significance of the observation of statistically significant differences in some individual adverse events (eg, sore throat, rash) and serious adverse events (eg, cellulitis, infections requiring hospitalization) is unclear, but has raised concern regarding possible adverse effects on the immune system. RANKL inhibition might increase the risk of infection or malignancy, since RANKL, RANK, and/or OPG are expressed in activated T and B lymphocytes, dendritic cells, and CD4/CD8 thymocytes,81,82 and RANKL and RANK knockout mice have a deficiency of splenic B cells and fail to develop lymph nodes.83,84 However, inhibition of RANKL in adult humans has not been shown to adversely affect measured parameters of immune function.57
No evidence of adverse clinical consequences due to bone turnover suppression, eg, increased fracture risk or impaired fracture healing, were observed with denosumab.57 Iliac crest bone biopsy data has shown normal bone quality with significant decreases in bone turnover parameters in denosumab-treated patients,85,86 consistent with the observed effects on bone turnover markers. All placebo-treated patients were found to have double label, while 36% of patients treated with denosumab had no detectable tetracycline label and 25% had only a single label.
The clinical significance of the absence of tetracycline label in denosumab-treated patients is uncertain. While denosumab appears to be an excellent option as the primary treatment of postmenopausal osteoporosis, it is most likely to be used in patients with a contraindication to oral bisphosphonates, gastrointestinal intolerance, malabsorption, or poor response to therapy.57
A validated Markov microsimulation model was used to estimate the cost (€2009) per quality-adjusted life year gained of a 3-year denosumab treatment compared with no treatment.80 The model was populated with cost and epidemiological data for Belgium from a health-care perspective and the base–case population was defined from the FREEDOM trial.80 This study suggests, on the basis of currently available data, that denosumab is cost-effective compared with no treatment for postmenopausal Belgian women with low bone mass and who are similar to patients included in the FREEDOM trial. In addition, denosumab was found to be cost-effective at the commonly accepted threshold of €30,000 per quality-adjusted life year gained in a population currently reimbursed in Europe with T-score −2.5 or less or prevalent vertebral fracture, aged 60 years and above.80
As well as in postmenopausal osteoporosis, denosumab has been examined in rheumatoid arthritis, multiple myeloma, breast cancer, prostate cancer, and other solid tumors.87
Androgen deprivation therapy is the cornerstone treatment for metastatic prostate cancer. The profound hypogonadal state is associated with metabolic changes including decreased BMD and an increased risk of fracture.87
In postmenopausal women, a single administration of denosumab resulted in rapid (within 12 hours), marked (80%), and sustained (6 months) suppression of osteoclast activity.71 In patients with multiple myeloma or bone metastasis from breast or prostate cancer, denosumab was well tolerated and achieved rapid and sustained suppression of osteoclast activity,88,89 and has proven efficacy in fracture prevention in men on initial androgen deprivation therapy.
Denosumab was superior to zoledronate in treatment of bone metastatic disease in castration resistant prostate cancer, the one setting in which a bisphosphonate is approved for prostate cancer.87 Ongoing Phase III studies will address other important unmet medical needs including metastasis prevention.87
In patients receiving methotrexate for erosive rheumatoid arthritis, denosumab provided protection against erosion, not only preventing bone loss but increasing hand BMD as measured by dual X-ray absorptiometry.90
Safety information on denosumab
Data is summarized in Table 3 and available in the leaflet information of denosumab.
Table 3.
Safety information on denosumab
| Hypocalcemia | Denosumab is contraindicated in patients with hypocalcemia, which may worsen – especially in patients with severe renal impairment. In patients predisposed to hypocalcemia and disturbances of mineral metabolism, clinical monitoring of calcium and mineral levels is required, and an adequate supplement of calcium and vitamin D. |
| Serious infections | In a clinical trial (N = 7808),76 serious infections leading to hospitalization were reported more frequently in the denosumab group than in the placebo group. Serious skin infections, as well as infections of the abdomen, urinary tract, and ear, were more frequent in patients treated with denosumab. Endocarditis was also reported more frequently in denosumab-treated subjects. The incidence of opportunistic infections was balanced and the overall incidence of infections was similar between the treatment groups. Patients should be advised to seek prompt medical attention if they develop signs or symptoms of severe infection, including cellulitis.76 Patients on concomitant immunosuppressant agents or with impaired immune systems may be at increased risk for serious infections. |
| Dermatologic adverse reactions | Epidermal and dermal adverse events (eg, dermatitis, eczema, and rashes) occurred at a significantly higher rate in the denosumab group compared to the placebo group. Most of these events were not specific to the injection site.76 Discontinuing denosumab if severe symptoms develop should be considered. |
| Osteonecrosis of the jaw | Osteonecrosis of the jaw, which can occur spontaneously, is generally associated with tooth extraction and/or local infection with delayed healing, and has been reported in patients receiving denosumab. An oral exam should be performed by the prescriber prior to initiation of denosumab. A dental examination with appropriate preventive dentistry should be considered prior to treatment in patients with risk factors for osteonecrosis of the jaw. Good oral hygiene practices should be maintained during treatment with denosumab. For patients requiring invasive dental procedures, clinical judgment should guide the management plan of each patient. Patients who are suspected of having or who develop osteonecrosis of the jaw should receive care by a dentist or an oral surgeon. Extensive dental surgery to treat osteonecrosis of the jaw may exacerbate the condition. Discontinuation of denosumab should be considered based on individual benefit–risk assessment. |
| Suppression of bone turnover | Denosumab resulted in significant suppression of bone remodeling as evidenced by markers of bone turnover and bone histomorphometry. The significance of these findings and the effect of long-term treatment are unknown. Monitor patients for consequences, including osteonecrosis of the jaw, atypical fractures, and delayed fracture healing. |
Denosumab and osteonecrosis of the jaw (ONJ)
The FREEDOM trial reported no cases of ONJ in either denosumab or placebo group.76 As ONJ and atypical femoral subtrochanteric fracture associated with long-term bisphosphonate use are rare, there might be an advantage (albeit small, given the rarity of these events) to the use of denosumab. Moreover, since bisphosphonates are cleared by the kidney and contraindicated in patients with renal insufficiency, denosumab (which is cleared by non-renal metabolism) may prove to be a safe drug in these patients, although studies that directly address this issue need to be done.91
All denosumab randomized controlled trials published to date include a dosing interval longer than 3 months and a cumulative dose of not more than 210 mg per 6 months.92,93 None of these studies report any cases of ONJ. On the contrary, preliminary results of two randomized controlled trials studying denosumab for the treatment of bone metastases in cancer patients include a monthly dosing interval and a dose of 120 mg per month.94,95 Denosumab-related ONJ could be a dose-related adverse effect.93
ONJ has been reported to be a much more common event in patients receiving bisphosphonates for the treatment and prevention of cancer-related skeletal events (mainly intravenously) rather than in those patients receiving bisphosphonates (mainly orally) for nonmalignancy indications.96,97
Similar to bisphosphonate-related ONJ pharmacosurveillance and reporting history,98 broad introduction of denosumab into clinical practice would allow for the recognition of denosumab-related ONJ adverse effect. Common plausible mechanisms for the etiopathogenesis of both denosumab- and bisphosphonate-related ONJ would encompass defective osteoclast differentiation, function, survival, and “fatigue.”99 When compared to bisphosphonates, denosumab exhibits the advantage of short clearance time. Thus, more feasible treatment and earlier healing of denosumab-related ONJ when compared to bisphosphonate-related ONJ could be anticipated.93
Denosumab and atypical fractures
Research from the first 3 years of an open-label extension of the pivotal Phase III FREEDOM trial, presented at the American College of Rheumatology 2011 Annual Meeting, showed that long-term use of the antiresorptive agent denosumab in postmenopausal women with osteoporosis continues to increase bone density and reduce markers of bone turnover, with no increased risk for the atypical fractures seen with long-term use of bisphosphonates.100
Further clinical investigations of long-term treatment with denosumab are needed to evaluate the possible occurrence of atypical fractures.
Conclusion
Denosumab is a promising emerging drug for the prevention and treatment of postmenopausal osteoporosis. Human monoclonal antibody to RANK, denosumab 60 mg given subcutaneously every six months has shown to increase BMD and reduce bone turnover and fracture risk in all the fragile sites. It is simple to administer and well tolerated, with a safety profile generally similar to placebo, except for a slightly higher incidence of cellulitis and exanthema.
Approved by the Food and Drug Administration and European Medicines Agency for the treatment of postmenopausal osteoporosis in women at high risk of fracture and for the bone loss associated with androgen deprivation therapy in men with prostate cancer, denosumab may be particularly useful in clinical practice for the treatment of patients who have failed or are intolerant to other available osteoporosis therapy, eg, patients with gastrointestinal contraindications, side effects with oral bisphosphonates, or malabsorption.
Denosumab has also shown promising skeletal effects in the treatment of cancer and rheumatoid arthritis.
Footnotes
Disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. No writing assistance was utilized in the production of this manuscript.
References
- 1.Cavalli L, Brandi ML. Age- and gender-related macro and microarchitecture changes in bone structure and implications for treatment. Int J Clin Rheumatol. 2011;6(3):359–369. [Google Scholar]
- 2.Bouxsein ML. Determinant of skeletal fragility. Best Pract Res Clin Rheumatol. 2005;19(6):897–911. doi: 10.1016/j.berh.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Siris ES, Chen YT, Abbott TA, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. 2004;164(10):1108–1112. doi: 10.1001/archinte.164.10.1108. [DOI] [PubMed] [Google Scholar]
- 4.Gallacher SJ, Dixon T. Impact of treatments for postmenopausal osteoporosis (bisphosphonates, parathyroid hormone, strontium ranelate, and denosumab) on bone quality: a systematic review. Calcif Tissue Int. 2010;87(6):469–484. doi: 10.1007/s00223-010-9420-x. [DOI] [PubMed] [Google Scholar]
- 5.Chen P, Miller PD, Recker R, et al. Increases in BMD correlate with improvements in bone microarchitecture with teriparatide treatment in postmenopausal women with osteoporosis. J Bone Miner Res. 2007;22(8):1173–1180. doi: 10.1359/jbmr.070413. [DOI] [PubMed] [Google Scholar]
- 6.Brandi ML. Microarchitecture, the key to bone quality. Rheumatology (Oxford) 2009;48(Suppl 4):iv3–iv8. doi: 10.1093/rheumatology/kep273. [DOI] [PubMed] [Google Scholar]
- 7.Riggs BL, Parfitt AM. Drugs used to treat osteoporosis: the critical need for a uniform nomenclature based on their action on bone remodeling. J Bone Miner Res. 2005;20(2):177–184. doi: 10.1359/JBMR.041114. [DOI] [PubMed] [Google Scholar]
- 8.Ammann P, Shen V, Robin B, Mauras Y, Bonjour JP, Rizzoli R. Strontium ranelate improves bone resistance by increasing bone mass and improving architecture in intact female rats. J Bone Miner Res. 2004;19(12):2012–2020. doi: 10.1359/JBMR.040906. [DOI] [PubMed] [Google Scholar]
- 9.Fuchs RK, Allen MR, Condon KW, et al. Strontium ranelate does not stimulate bone formation in ovariectomized rats. Osteoporos Int. 2008;19(9):1331–1341. doi: 10.1007/s00198-008-0602-6. [DOI] [PubMed] [Google Scholar]
- 10.Pietschmann P, Rauner M, Sipos W, Kerschan-Schindl K. Osteoporosis: an age-related and gender-specific disease – a mini-review. Gerontology. 2009;55(1):3–12. doi: 10.1159/000166209. [DOI] [PubMed] [Google Scholar]
- 11.Cummings SR. How drugs decrease fracture risk: lessons from trials. J Musculoskelet Neuronal Interact. 2002;2(3):198–200. [PubMed] [Google Scholar]
- 12.Beck TJ, Stone KL, Oreskovic TL, et al. Effects of current and discontinued estrogen replacement therapy on hip structural geometry: the study of osteoporotic fractures. J Bone Miner Res. 2001;16(11):2103–2110. doi: 10.1359/jbmr.2001.16.11.2103. [DOI] [PubMed] [Google Scholar]
- 13.Reszka AA, Rodan GA. Bisphosphonates mechanism of action. Curr Osteoporos Rep. 2003;1(2):45–52. doi: 10.1007/s11914-003-0008-5. [DOI] [PubMed] [Google Scholar]
- 14.Russell RG. Bisphosphonates: the first 40 years. Bone. 2011;49(1):2–19. doi: 10.1016/j.bone.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Coxon FP, Helfrich MH, Van’t Hof R, et al. Protein geranylgeranylation is required for osteoclast formation, function, and survival: inhibition by bisphosphonates and GGTI-298. J Bone Miner Res. 2000;15(8):1467–1476. doi: 10.1359/jbmr.2000.15.8.1467. [DOI] [PubMed] [Google Scholar]
- 16.Reszka AA, Halasy-Nagy JM, Masarachia PJ, Rodan GA. Bisphosphonates act directly on the osteoclast to induce caspase cleavage of mst1 kinase during apoptosis. A link between inhibition of the mevalonate pathway and regulation of an apoptosis-promoting kinase. J Biol Chem. 1999;274(49):34967–34973. doi: 10.1074/jbc.274.49.34967. [DOI] [PubMed] [Google Scholar]
- 17.Halasy-Nagy JM, Rodan GA, Reszka AA. Inhibition of bone resorption by alendronate and risedronate does not require osteoclast apoptosis. Bone. 2001;29(6):553–559. doi: 10.1016/s8756-3282(01)00615-9. [DOI] [PubMed] [Google Scholar]
- 18.Rogers HL, Marshall D, Rogers MJ. Effects of bisphosphonates on osteoclasts in vitro, studies by scanning electron microscopy. Bone. 2002;30(3):43S. [Google Scholar]
- 19.Alakangas A, Selander K, Mulari M, et al. Alendronate disturbs vesicular trafficking in osteoclasts. Calcif Tissue Int. 2002;70(1):40–47. doi: 10.1007/s002230010047. [DOI] [PubMed] [Google Scholar]
- 20.de Groen PC, Lubbe DF, Hirsch LJ, et al. Esophagitis associated with the use of alendronate. N Engl J Med. 1996;335(14):1016–1021. doi: 10.1056/NEJM199610033351403. [DOI] [PubMed] [Google Scholar]
- 21.Blank MA, Ems BL, Gibson GW, et al. Nonclinical model for assessing gastric effects of bisphosphonates. Dig Dis Sci. 1997;42(2):281–288. doi: 10.1023/a:1018849415297. [DOI] [PubMed] [Google Scholar]
- 22.Elliott SN, McKnight W, Davies NM, et al. Alendronate induces gastric injury and delays ulcer healing in rodents. Life Sci. 1998;62(1):77–91. doi: 10.1016/s0024-3205(97)01040-0. [DOI] [PubMed] [Google Scholar]
- 23.Peter CP, Kindt MV, Majka JA. Comparative study of potential for bisphosphonates to damage gastric mucosa of rats. Dig Dis Sci. 1998;43(5):1009–1015. doi: 10.1023/a:1018826600877. [DOI] [PubMed] [Google Scholar]
- 24.Xiong Y, Yang HJ, Feng J, Shi ZL, Wu LD. Effects of alendronate on the proliferation and osteogenic differentiation of MG-63 cells. J Int Med Res. 2009;37(2):407–416. doi: 10.1177/147323000903700216. [DOI] [PubMed] [Google Scholar]
- 25.Wells GA, Cranney A, Peterson J, et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;1:CD001155. doi: 10.1002/14651858.CD001155.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Wells GA, Cranney A, Peterson J, et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev. 2008;1:CD004523. doi: 10.1002/14651858.CD004523.pub3. [DOI] [PubMed] [Google Scholar]
- 27.Black DM, Delmas PD, Eastell R, et al. HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356(18):1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 28.Chesnut CH, III, Skag A, Christiansen C, et al. Oral Ibandronate Osteoporosis Vertebral Fracture Trial in North America and Europe (BONE) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res. 2004;19(8):1241–1249. doi: 10.1359/JBMR.040325. [DOI] [PubMed] [Google Scholar]
- 29.Recker R, Masarachia P, Santora A, et al. Trabecular bone microarchitecture after alendronate treatment of osteoporotic women. Curr Med Res Opin. 2005;21(2):185–194. doi: 10.1185/030079904X20259. [DOI] [PubMed] [Google Scholar]
- 30.Dufresne TE, Chmielewski PA, Manhart MD, Johnson TD, Borah B. Risedronate preserves bone architecture in early postmenopausal women in 1 year as measured by three-dimensional microcomputed tomography. Calcif Tissue Int. 2003;73(5):423–432. doi: 10.1007/s00223-002-2104-4. [DOI] [PubMed] [Google Scholar]
- 31.Seeman E. To stop or not to stop, that is the question. Osteoporos Int. 2009;20(2):187–195. doi: 10.1007/s00198-008-0813-x. [DOI] [PubMed] [Google Scholar]
- 32.Reginster JY, Bruyère O, Sawicki A, et al. Long-term treatment of postmenopausal osteoporosis with strontium ranelate: results at 8 years. Bone. 2009;45(6):1059–1064. doi: 10.1016/j.bone.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 33.European Medicines Agency. Protelos: scientific discussion. [Accessed October 12, 2009]. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000560/human_med_000999.jsp&jsenabled=true.
- 34.Deeks ED, Dhillon S. Strontium ranelate: a review of its use in the treatment of postmenopausal osteoporosis. Drugs. 2010;70(6):733–759. doi: 10.2165/10481900-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 35.Marie PJ, Ammann P, Boivin G, Rey C. Mechanisms of action and therapeutic potential of strontium in bone. Calcif Tissue Int. 2001;69(3):121–129. doi: 10.1007/s002230010055. [DOI] [PubMed] [Google Scholar]
- 36.Brennan TC, Rybchyn MS, Green W, Atwa S, Conigrave AD, Mason RS. Osteoblasts play key roles in the mechanisms of action of strontium ranelate. Br J Pharmacol. 2009;157(7):1291–1300. doi: 10.1111/j.1476-5381.2009.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhu LL, Zaidi S, Peng Y, et al. Induction of a program gene expression during osteoblast differentiation with strontium ranelate. Biochem Biophys Res Commun. 2007;355(2):307–311. doi: 10.1016/j.bbrc.2007.01.120. [DOI] [PubMed] [Google Scholar]
- 38.Chattopadhyay N, Quinn SJ, Kifor O, Ye C, Brown EM. The calcium-sensing receptor (CaR) is involved in strontium ranelate-induced osteoblast proliferation. Biochem Pharmacol. 2007;74(3):438–447. doi: 10.1016/j.bcp.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 39.Caverzasio J. Strontium ranelate promotes osteoblastic cell replication through at least two different mechanisms. Bone. 2008;42(6):1131–1136. doi: 10.1016/j.bone.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 40.Fromiguè O, Hay E, Barbara A, et al. Calcium sensing receptor-dependent and receptor-independent activation of osteoblast replication and survival by strontium ranelate. J Cell Mol Med. 2009;13(8B):2189–2199. doi: 10.1111/j.1582-4934.2008.00673.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meunier PJ, Roux C, Seeman E, et al. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Eng J Med. 2004;350(5):459–468. doi: 10.1056/NEJMoa022436. [DOI] [PubMed] [Google Scholar]
- 42.Reginster JY, Seeman E, De Vernejoul MC, et al. Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab. 2005;90(5):2816–2822. doi: 10.1210/jc.2004-1774. [DOI] [PubMed] [Google Scholar]
- 43.Reginster JY, Felsenberg D, Boonen S, et al. Effects of long term strontium ranelate treatment on the risk of nonvertebral and vertebral fractures in postmenopausal osteoporosis: results of a 5-year randomized, placebo-controlled trial. Atrthritis Rheum. 2008;58(6):1687–1695. doi: 10.1002/art.23461. [DOI] [PubMed] [Google Scholar]
- 44.Delmas PD. Treatment of postmenopausal osteoporosis. Lancet. 2002;359(9322):2018–2026. doi: 10.1016/S0140-6736(02)08827-X. [DOI] [PubMed] [Google Scholar]
- 45.Recker RR, Marin F, Ish-Shalom S, et al. Comparative effects of teriparatide and strontium ranelate on bone biopsies and biochemical markers of bone turnover in postmenopausal women with osteoporosis. J Bone Miner Res. 2009;24(8):1358–1368. doi: 10.1359/jbmr.090315. [DOI] [PubMed] [Google Scholar]
- 46.Riggs BL, Parfitt AM. Drugs used to treat osteoporosis: the critical need of a uniform nomenclature based on their action on bone remodeling. J Bone Miner Res. 2005;20(2):177–184. doi: 10.1359/JBMR.041114. [DOI] [PubMed] [Google Scholar]
- 47.Recker RR, Bare SP, Smith SY, et al. Cancellous and cortical bone architecture and turnover at the iliac crest of postmenopausal osteoporotic women treated with parathyroid hormone 1–84. Bone. 2009;44(1):113–119. doi: 10.1016/j.bone.2008.09.019. [DOI] [PubMed] [Google Scholar]
- 48.Miyakoshi N. Effects of parathyroid hormone on cancellous bone mass and structure in osteoporosis. Curr Pharm Des. 2004;10(21):2615–2627. doi: 10.2174/1381612043383737. [DOI] [PubMed] [Google Scholar]
- 49.Adami S, Brandi ML, Canonico PL, Minisola G, Minisola S, Tarantino U. Appropriate use of anabolic treatment for severe osteoporosis. Clin Cases Miner Bone Metab. 2010;7(2):114–122. [PMC free article] [PubMed] [Google Scholar]
- 50.Bone HG, Hosking D, Devogelaer JP, et al. Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med. 2004;350(12):1189–1199. doi: 10.1056/NEJMoa030897. [DOI] [PubMed] [Google Scholar]
- 51.Finkelstein JS, Wyland JJ, Leder BZ, et al. Effects of teriparatide retreatment in osteoporotic men and women. J Clin Endocrinol Metab. 2009;94(7):2495–2501. doi: 10.1210/jc.2009-0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eastell R, Nickelsen T, Marin F, et al. Sequential treatment of severe postmenopausal osteoporosis after teriparatide: final results of the randomized, controlled European study of Forsteo (EUROFORS) J Bone Miner Res. 2009;24(4):726–736. doi: 10.1359/jbmr.081215. [DOI] [PubMed] [Google Scholar]
- 53.Kawate H, Takayanagi R. Efficacy and safety of bazedoxifene for postmenopausal osteoporosis. Clin Interv Aging. 2011;6:151–160. doi: 10.2147/CIA.S15711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Silverman SL, Christiansen C, Genant HK, et al. Efficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo- and active-controlled clinical trial. J Bone Miner Res. 2008;23(12):1923–1934. doi: 10.1359/jbmr.080710. [DOI] [PubMed] [Google Scholar]
- 55.Miller PD, Chines AA, Christiansen C, et al. Effects of bazedoxifene on BMD and bone turnover in postmenopausal women: 2-yr results of a randomized, double-blind, placebo-, and active-controlled study. J Bone Miner Res. 2008;23(4):525–535. doi: 10.1359/jbmr.071206. [DOI] [PubMed] [Google Scholar]
- 56.Collin-Osdoby P. Regulation of vascular calcification by osteoclast regulatory factors RANKL and osteoprotegerin. Circ Res. 2004;95(11):1046–1057. doi: 10.1161/01.RES.0000149165.99974.12. [DOI] [PubMed] [Google Scholar]
- 57.Lewiecki EM. Treatment of osteoporosis with denosumab. Maturitas. 2010;66(2):182–186. doi: 10.1016/j.maturitas.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 58.Hsu H, Lacey DL, Dunstan CR, et al. Tumor necrosis factor receptor family member RANK mediates osteoclast differentiation and activation induced by osteoprotegerin ligand. Proc Natl Acad Sci U S A. 1999;96(7):3540–3545. doi: 10.1073/pnas.96.7.3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lacey DL, Timms E, Tan HL, et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell. 1998;93(2):165–176. doi: 10.1016/s0092-8674(00)81569-x. [DOI] [PubMed] [Google Scholar]
- 60.Simonet WS, Lacey DL, Dunstan CR, et al. Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell. 1997;89(2):309–319. doi: 10.1016/s0092-8674(00)80209-3. [DOI] [PubMed] [Google Scholar]
- 61.Burgess TL, Qian Y, Kaufman S, et al. The ligand for osteoprotegerin (OPGL) directly activates mature osteoclasts. J Cell Biol. 1999;145(3):527–538. doi: 10.1083/jcb.145.3.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mosekilde L, Sogaard CH, Danielsen CC, Torring O. The anabolic effects of human parathyroid hormone (hPTH) on rat vertebral body mass are also reflected in the quality of bone, assessed by biomechanical testing: a comparison study between hPTH-1–34 and hPTH-1–84. Endocrinology. 1991;129(1):421–428. doi: 10.1210/endo-129-1-421. [DOI] [PubMed] [Google Scholar]
- 63.Lacey DL, Tan HL, Lu J, et al. Osteoprotegerin ligand modulates murine osteoclast survival in vitro and in vivo. Am J Pathol. 2000;157(2):435–448. doi: 10.1016/S0002-9440(10)64556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hofbauer LC, Schoppet M. Clinical implications of the osteoprotegerin/RANKL/RANK system for bone and vascular diseases. JAMA. 2004;292(4):490–495. doi: 10.1001/jama.292.4.490. [DOI] [PubMed] [Google Scholar]
- 65.Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423(6937):337–342. doi: 10.1038/nature01658. [DOI] [PubMed] [Google Scholar]
- 66.Yasuda H, Shima N, Nakagawa N, et al. Identity of osteoclastogenesis inhibitory factor (OCIF) and osteoprotegerin (OPG): a mechanism by which OPG/OCIF inhibits osteoclastogenesis in vitro. Endocrinology. 1998;139(3):1329–1337. doi: 10.1210/endo.139.3.5837. [DOI] [PubMed] [Google Scholar]
- 67.Khosla S. Minireview: the OPG/RANKL/RANK system. Endocrinology. 2001;142(12):5050–5055. doi: 10.1210/endo.142.12.8536. [DOI] [PubMed] [Google Scholar]
- 68.Yasuda H, Shima N, Nakagawa N, et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci U S A. 1998;95(7):3597–3602. doi: 10.1073/pnas.95.7.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anderson DM, Maraskovsky E, Billingsley WL, et al. A homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell function. Nature. 1997;390(6656):175–179. doi: 10.1038/36593. [DOI] [PubMed] [Google Scholar]
- 70.Mizuno A, Kanno T, Hoshi M, et al. Transgenic mice overexpressing soluble osteoclast differentiation factor (sODF) exhibit severe osteoporosis. J Bone Miner Metab. 2002;20(6):337–344. doi: 10.1007/s007740200049. [DOI] [PubMed] [Google Scholar]
- 71.Eghbali-Fatourechi G, Khosla S, Sanyal A, Boyle WJ, Lacey DL, Riggs BL. Role of RANK ligand in mediating increased bone resorption in early postmenopausal women. J Clin Invest. 2003;111(8):1221–1230. doi: 10.1172/JCI17215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bekker PJ, Holloway DL, Rasmussen AS, et al. A single-dose placebo-controlled study of AMG 162, a fully human monoclonal antibody to RANKL, in postmenopausal women. J Bone Miner Res. 2004;19(7):1059–1066. doi: 10.1359/JBMR.040305. [DOI] [PubMed] [Google Scholar]
- 73.McClung MR, Lewiecki EM, Cohen SB, et al. Denosumab in postmenopausal women with low bone mineral density. N Engl J Med. 2006;354(8):821–831. doi: 10.1056/NEJMoa044459. [DOI] [PubMed] [Google Scholar]
- 74.Lewiecki EM, Miller PD, McClung MR, et al. Two-year treatment with denosumab (AMG 162) in a randomized phase 2 study of postmenopausal women with low BMD. J Bone Miner Res. 2007;22(12):1832–1841. doi: 10.1359/jbmr.070809. [DOI] [PubMed] [Google Scholar]
- 75.Miller PD, Bolognese MA, Lewiecki EM, et al. Effect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trial. Bone. 2008;43(2):222–229. doi: 10.1016/j.bone.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 76.Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–765. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]
- 77.Bone HG, Bolognese MA, Yuen CK, et al. Effects of denosumab on bone mineral density and bone turnover in postmenopausal women. J Clin Endocrinol Metab. 2008;93(6):2149–2157. doi: 10.1210/jc.2007-2814. [DOI] [PubMed] [Google Scholar]
- 78.Brown JP, Prince RL, Deal C, et al. Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trial. J Bone Miner Res. 2009;24(1):153–161. doi: 10.1359/jbmr.0809010. [DOI] [PubMed] [Google Scholar]
- 79.Kendler DL, Roux C, Benhamou CL, et al. Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Miner Res. 2010;25(1):72–81. doi: 10.1359/jbmr.090716. [DOI] [PubMed] [Google Scholar]
- 80.Hiligsmann M, Reginster JY. Potential cost-effectiveness of denosumab for the treatment of postmenopausal osteoporotic women. Bone. 2010;47(1):34–40. doi: 10.1016/j.bone.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 81.Clowes JA, Riggs BL, Khosla S. The role of the immune system in the pathophysiology of osteoporosis. Immunol Rev. 2005;208:207–227. doi: 10.1111/j.0105-2896.2005.00334.x. [DOI] [PubMed] [Google Scholar]
- 82.Xing L, Schwarz EM, Boyce BF. Osteoclast precursors, RANKL/ RANK, and immunology. Immunol Rev. 2005;208:19–29. doi: 10.1111/j.0105-2896.2005.00336.x. [DOI] [PubMed] [Google Scholar]
- 83.Dougall WC, Glaccum M, Charrier K, et al. RANK is essential for osteoclast and lymph node development. Genes Dev. 1999;13(18):2412–2424. doi: 10.1101/gad.13.18.2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kong YY, Yoshida H, Sarosi I, et al. OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature. 1999;397(6717):315–323. doi: 10.1038/16852. [DOI] [PubMed] [Google Scholar]
- 85.Reid IR, Benhamou CL, Bolognese M, et al. Effects of denosumab on bone histology and histomorphometry: the FREEDOM and STAND studies [abstract] J Bone Miner Res. 2009;24(Suppl 1):S9. doi: 10.1002/jbmr.149. [DOI] [PubMed] [Google Scholar]
- 86.United States Food and Drug Administration, Amgen Inc. Briefing information for the August 13, 2009 meeting of the Reproductive Health Drugs Advisory Committee. 2009. [Accessed October 30, 2009]. Available from: http://www.fda.gov/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ReproductiveHealth-DrugsAdvisoryCommittee/ucm176584.htm.
- 87.Lee RJ, Saylor PL, Smith MR. Treatment and prevention of bone complication from prostate cancer. Bone. 2011;48(1):88–95. doi: 10.1016/j.bone.2010.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Body JJ, Facon T, Coleman RE, et al. A study of the biological receptor activator of nuclear factor-kappaB ligand inhibitor, denosumab, in patients with multiple myeloma or bone metastases from breast cancer. Clin Cancer Res. 2006;12(4):1221–1228. doi: 10.1158/1078-0432.CCR-05-1933. [DOI] [PubMed] [Google Scholar]
- 89.Lipton A, Steger GG, Figueroa J, et al. Randomized active-controlled phase II study of denosumab efficacy and safety in patients with breast cancer-related bone metastases. J Clin Oncol. 2007;25(28):4431–4437. doi: 10.1200/JCO.2007.11.8604. [DOI] [PubMed] [Google Scholar]
- 90.Deodhar A, Dore RK, Mandel D, et al. Denosumab-mediated increase in hand bone mineral density associated with decreased progression of bone erosion in rheumatoid arthritis patients. Arthritis Care Res (Hoboken) 2010;62(4):569–574. doi: 10.1002/acr.20004. [DOI] [PubMed] [Google Scholar]
- 91.Khosla S. Increasing options for the treatment of osteoporosis. N Engl J Med. 2009;361(8):818–820. doi: 10.1056/NEJMe0905480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Anastasilakis AD, Toulis KA, Goulis DG, et al. Efficacy and safety of denosumab in postmenopausal women with osteopenia or osteoporosis: a systematic review and a meta-analysis. Horm Metab Res. 2009;41(10):721–729. doi: 10.1055/s-0029-1224109. [DOI] [PubMed] [Google Scholar]
- 93.Kyrgidis A, Toulis KA. Denosumab-related osteonecrosis of the jaws. Osteoporos Int. 2011;22(1):369–370. doi: 10.1007/s00198-010-1177-6. [DOI] [PubMed] [Google Scholar]
- 94.Henry D, von Moos R, Vadhan-Raj S, et al. A double-blind, randomized study of denosumab versus zoledronic acid for the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. Eur J Cancer Suppl. 2009;7(3):12. doi: 10.1200/JCO.2010.31.3304. [DOI] [PubMed] [Google Scholar]
- 95.Stopeck A, Body JJ, Fujiwara Y, et al. Denosumab versus zoledronic acid for the treatment of breast cancer patients with bone metastases: results of a randomized phase 3 study. Eur J Cancer Suppl. 2009;7(3):2–3. [Google Scholar]
- 96.Hess LM, Jeter JM, Benham-Hutchins M, Alberts DS. Factors associated with osteonecrosis of the jaw among bisphosphonate users. Am J Med. 2008;121(6):475–483. doi: 10.1016/j.amjmed.2008.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kyrgidis A, Vahtsevanos K. Osteonecrosis of the jaw in patients receiving oral bisphosphonates. Osteoporos Int. 2010;21(3):535–536. doi: 10.1007/s00198-009-1089-5. [DOI] [PubMed] [Google Scholar]
- 98.Edwards BJ, Gounder M, McKoy JM, et al. Pharmacovigilance and reporting oversight in US FDA fast-track process: bisphosphonates and osteonecrosis of the jaw. Lancet Oncol. 2008;9(12):1166–1172. doi: 10.1016/S1470-2045(08)70305-X. [DOI] [PubMed] [Google Scholar]
- 99.Kyrgidis A, Vahtsevanos K. “Fatigue” having a role in the pathogenesis of osteonecrosis of the jaws. Clin Oral Investig. 2009;13(4):479–480. doi: 10.1007/s00784-009-0319-8. [DOI] [PubMed] [Google Scholar]
- 100.Gordon D. Denosumab increases bone density, no atypical fracture risk. Medscape Medical News [website on the Internet] Nov 10, 2011. [Accessed January 17, 2012]. Available from: http://www.medscape.com/viewarticle/753389.
- 101.Reszka AA, Rodan GA. Bisphosphonate mechanism of action. Curr Rheumatol Rep. 2003;5(1):65–74. doi: 10.1007/s11926-003-0085-6. [DOI] [PubMed] [Google Scholar]