Abstract
A history of severe allergic reaction to iodine contrast leading to anaphylactic shock presents a dilemma in patients requiring cardiac catheterization. As an alternative, gadolinium has been an interesting and potentially useful agent. However, gadolinium produces poor image quality and has been associated with significant arrhythmias in small case series. Furthermore, there is no consensus about the maximal allowable dose that can be administered to a patient. In the present report, a successful combination of gadolinium contrast with a power injector that produced adequate image quality in a patient with severe allergy to iodine contrast is described. The case was complicated by the occurrence of ventricular fibrillation when damping occurred during injection of contrast into the right coronary artery. This complication has been reported previously with intracoronary gadolinium injection. The report is followed by a brief literature review.
Keywords: Angiography, Complication, Gadolinium use, Iodine contrast allergy, PCI complication, Percutaneous coronary intervention, Stenting, Ventricular fibrillation
Coronary artery angiography remains an indispensible technique in patients with cardiac disease. However, its use is associated with side effects and limitations. Severe allergy to iodine contrast agents, as well as deterioration of renal function in patients with renal insufficiency, remain the main problems with iodine-based contrast media. As an alternative, gadolinium has been an interesting and potentially useful replacement for iodine contrast for coronary and peripheral arteriography. However, randomized trials have shown worsening renal failure with the use of gadolinium. Furthermore, image quality is poor and significant arrhythmias have been reported. In the present report, we describe a patient with severe allergic reaction to iodine contrast requiring coronary angiography. To improve image quality, we used gadolinium combined with a power injector.
CASE PRESENTATION
A 73-year-old man with ischemic cardiomyopathy, coronary artery disease, diabetes, hypertension and hyperlipidemia presented with progressive angina and dyspnea on exertion. Over the previous several months, he was hospitalized multiple times for congestive heart failure and non-ST elevation myocardial infarction. Sequential echocardiography showed a deterioration of left ventricular function, with a decrease in ejection fraction from near normal to 35% with regional wall motion abnormalities. Given the patient’s serial ischemic events, progressive angina and decrease in systolic function, cardiac catheterization was warranted. Cardiac catheterization had never been performed due to a severe, life-threatening allergy to iodinated contrast, during which he once required endotracheal intubation for respiratory distress. After extensive discussion with the patient, the decision was made to pursue coronary angiography using gadolinium. To improve image quality, a decison was made to use a power injector during the procedure with standard undiluted gadolinium, which has previously been reported to be safe. While not of excellent quality, the cine images were adequate and provided clinically relevant data. No arrhythmias or hemodynamic changes occurred during three power injections of 8 mL of undiluted gadolinium per injection (total of 24 mL) in the left coronary arteries. However, during power injection into the right coronary artery, sudden damping of the pressure occurred at the beginning of the injection due to deep seeding of the catheter tip triggering ventricular fibrillation, which successfully responded to a third defibrillation attempt using 360 J after the first two attempts failed.
The patient was found to have chronic total occlusion of his left circumflex artery (Figures 1 to 3), a 40% lesion in the mid right coronary artery (Figure 4) and multiple mild irregularities in the left anterior descending artery. There was no evidence of left main coronary artery disease. Therefore, aggressive medical therapy was believed to be appropriate, with optimization of the patient’s heart failure and coronary artery disease treatment, and modification of his risk factors.
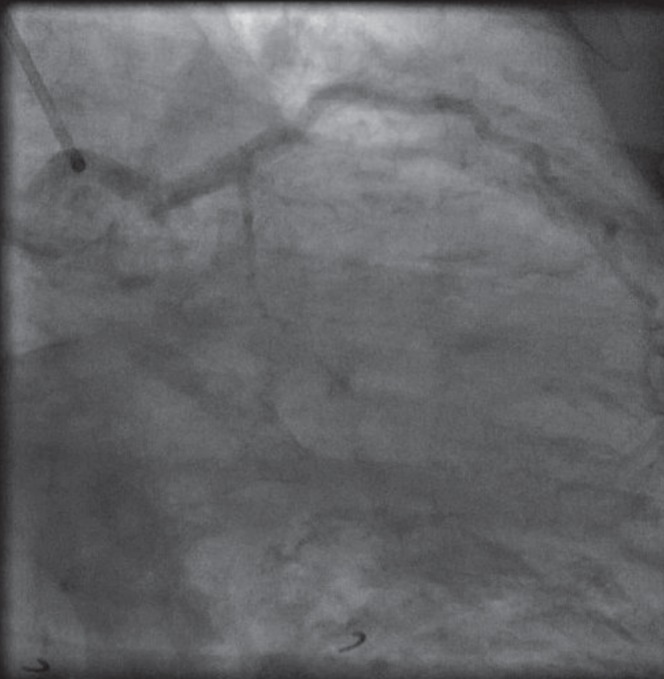
Figure 1).

Left anterior oblique caudal view showing 100% occlusion of the circumflex artery from its origin
Figure 3).
Cranial right anterior oblique view showing 100% occlusion of the circumflex artery without any significant left anterior descending artery disease
Figure 4).
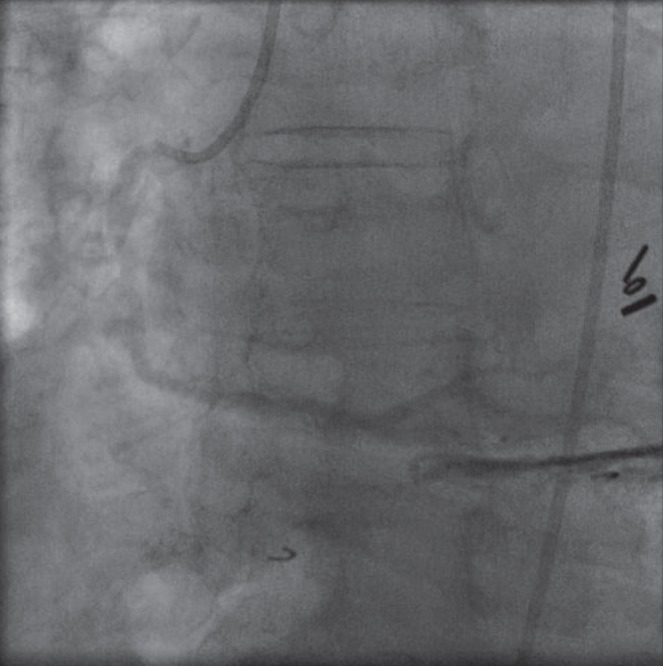
Left anterior oblique view showing the right coronary artery with mild disease
DISCUSSION
Side effects as a result of iodinated contrast media have occurred less frequently since the introduction of nonionic agents; however, allergy to iodinated agents remain an important complication of coronary angiography. In a large-scale study by Katayama et al (1), nonionic contrast media significantly reduced the prevalence of all degrees of adverse reactions when compared with ionic contrast media. This was true for milder adverse and potentially life-threatening reactions.
Gadolinium is a chemical element that has been routinely used as a contrast agent in magnetic resonance imaging. It has also been used in multiple diagnostic and interventional vascular procedures. When used in recommended doses, gadolinium has been shown to be safe, well-tolerated and not nephrotoxic in patients with normal renal function (2–5). The use of gadolinium-based agents has also been described in interventional procedures with good image quality and satisfactory results (2,5–7). Its reported safety encouraged us to use it for coronary angiography in a patient with severe allergic reaction to iodine-based contrast media (2–5,7). Furthermore, we infused the gadolinium-based agent using a power injector, which improved image quality and, to our knowledge, has not been previously described in coronary angiography.
Multiple studies have shown satisfactory results and safe outcomes with the use of gadolinium as mentioned above. In patients with baseline renal insufficiency, gadolinium produced no deterioration of renal function when complemented with standard renal protective measures including intravenous fluid hydration and oral N-acetylcysteine (8,9). One study showed no effect on renal function when gadolinium was mixed 1:1 with nonionic hypo-osmolar iodine medium (9). However, there are data suggesting that gadolinium mixed with low-dose iso-osmolar iodinated contrast medium is associated with similar or higher rates of contrast-associated nephrotoxicity (10). Even when administered without iodinated media, gadolinium caused acute renal insufficiency in high doses (0.6 mmol/kg and 0.9 mmol/kg) in two cases reported by Giozzet et al (11). In a retrospective, single-centre study, Sam et al (12) showed that gadolinium use was associated with acute renal failure in seven of 195 (3.5%) patients with chronic renal insufficiency; no impairment in renal function occurred in patients with normal creatinine levels. This emphasizes the importance of not exceeding the limit of 0.4 mmol gadolinium/kg body weight. The safe dose is 40 mL to 70 mL per examination per patient (2,11,13).
In one study (8), three of 19 patients (21%) developed potentially life-threatening cardiac arrhythmias after intracoronary gadolinium injection, requiring defibrillation or emergency medical treatment. However, in another study using undiluted gadolinium (7), no significant adverse event occurred. In our patient, ventricular fibrillation occurred during right coronary artery angiography, most likely secondary to the combination of pressure damping and hyperosmolar gadolinium contrast. Based on our experience and other case series, ventricular arrhythmias can occur in significant number of patients during gadolinium injection. Therefore, physicians need to be aware of this potential life-threatening complication when using gadolinium. We recommend placing defibrillation patches on the patient connected to a defibrillator at the highest 360 J energy setting before cardiac catheterization is performed with gadolinium-based agents. This could optimize shock delivery in the case of serious ventricular arrhythmias that require immediate cardioversion. Furthermore, we strongly suggest avoiding gadolinium injection if damping occurs during coronary angiography to decrease the risk of ventricular arrhythmias.
CONCLUSION
It is becoming more evident that gadolinium is a reasonable option for use in patients with contraindications to iodine-based media because of severe allergy; it provides acceptable imaging quality, with some risk for ventricular arrhythmias when administered in recommended doses. The combination of gadolinium use with a power injector appears to improve image quality and reduce the amount of gadolinium administered.
Figure 2).
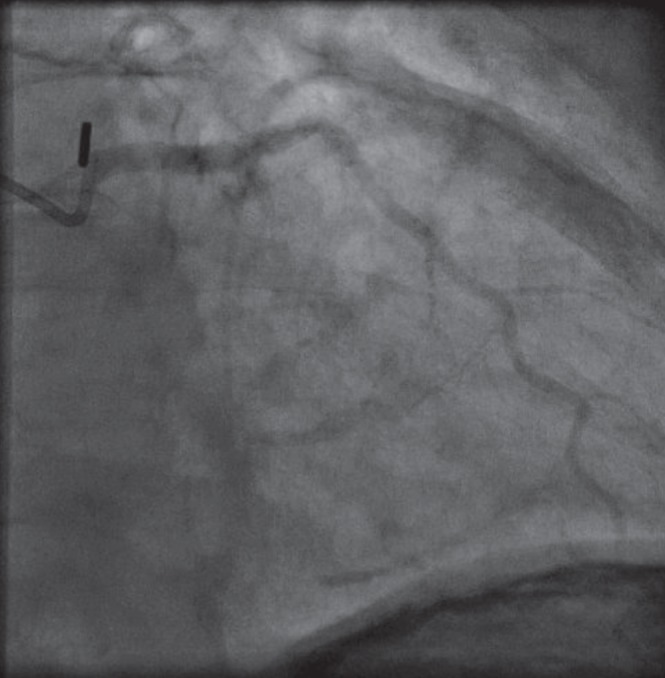
Cranial anterior oblique view showing 100% occluded circumflex artery without any significant left anterior descending artery disease
REFERENCES
- 1.Katayama H, Yamaguchi K, Kozuka T, Takashima T, Seez P, Matsuura K. Adverse reactions to ionic and nonionic contrast media. A report from the Japanese Committee on the Safety of Contrast Media. Radiology. 1990;175:621–8. doi: 10.1148/radiology.175.3.2343107. [DOI] [PubMed] [Google Scholar]
- 2.Spinosa DJ, Angle JF, Hartwell GD, Hagspiel KD, Leung DA, Matsumoto AH. 2002. Gadolinium-based contrast agents in angiography and interventional radiology. Radiol Clin North Am. 2002;40:693–710. doi: 10.1016/s0033-8389(02)00022-2. [DOI] [PubMed] [Google Scholar]
- 3.Parodi JC, Ferreira LM. Gadolinium-based contrast: An alternative contrast agent for endovascular interventions. Ann Vasc Surg. 2000;14:480–3. doi: 10.1007/s100169910085. [DOI] [PubMed] [Google Scholar]
- 4.Hammer FD, Malaise J, Goffette PP, Mathurin P. Gadolinium dimeglumine: An alternative contrast agent for digital subtraction angiography in patients with renal failure. Transplant Proc. 2000;32:432–3. doi: 10.1016/s0041-1345(00)00840-x. [DOI] [PubMed] [Google Scholar]
- 5.Spinosa DJ, Matsumoto AH, Angle JF, Hagspiel KD, Leung DA, Hartwell GD. Gadolinium contrast agents: Their role in vascular and nonvascular diagnostic angiography and interventions. Tech Vasc Interv Radiol. 2001;4:45–52. doi: 10.1053/tvir.2001.22008. [DOI] [PubMed] [Google Scholar]
- 6.Hatrick AG, Jarosz JM, Irvine AT. Gadopentate dimeglumine as an alternative contrast agent for use in interventional procedures. Clin Radiol. 1997;52:948–52. doi: 10.1016/s0009-9260(97)80230-9. [DOI] [PubMed] [Google Scholar]
- 7.Ose K, Doue T, Zen K, et al. ‘Gadolinium’ as an alternative to iodinated contrast media for X-ray angiography in patients with severe allergy. Circ J. 2005;69:507–9. doi: 10.1253/circj.69.507. [DOI] [PubMed] [Google Scholar]
- 8.Kälsch H, Kälsch T, Eggebrecht H, Konorza T, Kahlert P, Erbel R. Gadolinium-based coronary angiography in patients with contraindication for iodinated x-ray contrast medium: A word of caution. J Interv Cardiol. 2008;21:167–74. doi: 10.1111/j.1540-8183.2007.00340.x. [DOI] [PubMed] [Google Scholar]
- 9.Sayin T, Turhan S, Akyürek O, Kilickap M. Gadolinium:nonionic contrast media (1:1) coronary angiography in patients with impaired renal function. Angiology. 2007;58:56–4. doi: 10.1177/0003319707303640. [DOI] [PubMed] [Google Scholar]
- 10.Briguori C, Colombo A, Airoldi F, et al. Gadolinium-based contrast agents and nephrotoxicity in patients undergoing coronary artery procedures. Catheter Cardiovasc Interv. 2006;67:175–80. doi: 10.1002/ccd.20592. [DOI] [PubMed] [Google Scholar]
- 11.Giozzet M, Cavagna E, De Dea M, et al. [Gadolinium for DSA in two patients with azotemia: Images of suitable quality and risk of acute renal failure] G Ital Nefrol. 2003;20:298–301. [PubMed] [Google Scholar]
- 12.Sam AD, Morasch MD, Collins J, Song G, Chen R, Pereles FS. Safety of gadolinium contrast angiography in patients with chronic renal insufficiency. J Vasc Surg. 2003;38:313–8. doi: 10.1016/s0741-5214(03)00315-x. [DOI] [PubMed] [Google Scholar]
- 13.Tishler S, Hoffman JC. Anaphylactoid reactions to i.v. gadopentetate dimeglumine. AJNR Am J Neuroradiol. 1990;11:1167. discussion 1168–9. [PMC free article] [PubMed] [Google Scholar]


