Abstract
Rates of HIV/AIDS and depression in women are significant public health concerns. The current meta-analysis tested the hypothesis that depression levels moderate change in sexual risk behavior in women participating in HIV prevention interventions. Features of the interventions were also explored as possible factors in decreasing levels of depression and sexual risk behavior. Included were HIV primary prevention interventions that measured sexual risk behavior and depression at baseline and follow-up and reported separate results for women. Ten studies (fourteen intervention groups) met the inclusion criteria. The majority of participants (N = 4,195 women) were African American; mean age was 28-years old. Both depression and sexual risk behavior decreased significantly in treatment and control groups from baseline to follow-up. Sexual risk decreased more to the extent that interventions sampled (a) participants with higher baseline levels of depression, (b) older women, (c) Hispanics/Latinas, and (d) members of risk groups (e.g., drug users, homeless). Interventions that included (e) condom provision, (f) information about condoms, and (g) HIV counseling and testing were also more successful in decreasing sexual risk. Finally (h), interventions were more likely to reduce sexual risk behavior when they decreased depression to a large extent relative to baseline levels. Interventions were more likely to decrease depression when they (a) had samples of only women; (b) targeted risk groups; and (c) provided self-management and coping skills. Reducing depression appears to play a role in decreasing sexual risk behavior, suggesting that interventions should actively address depression.
Keywords: HIV primary prevention interventions, behavioral interventions, sexual risk behavior, depression, depression severity, mental health, women, meta-analysis
AIDS is among the leading causes of death in the United States (Heron, 2011) and the number one killer worldwide of women aged 15–44 (World Health Organization, 2009). In the United States, as of 2008, the CDC (2011b) estimated nearly 1,200,000 people living with HIV/AIDS, with approximately 48,100 new cases diagnosed in 2009, 23% of whom were women (Prejean et al., 2011). Women comprise over one-third of all people living with HIV/AIDS (CDC, 2011b) and African American and Hispanic/Latina women are disproportionately affected by HIV/AIDS, with rates about 15 and 5 times higher than white women, respectively (CDC, 2011a). Depression is also a major public health concern for women as significantly higher rates of depression are seen in women compared to men (Pratt & Brody, 2008). Risk factors for depression include financial problems, low socioeconomic status, unemployment, and lower levels of education, with ethnic/racial minority women being more likely to possess these risk factors (American Psychological Association, 2010; Lorant et al., 2003; Mossakowski, 2009). Furthermore, women who experience depression/psychological distress are more likely to report unprotected sex, a higher number of sexual partners, having a sexually transmitted infection, alcohol and drug use, sex under the influence of alcohol or drugs, and unstable housing, among other HIV risk factors (Beadnell et al., 2003; Seth et al., 2009; Williams & Latkin, 2005). Therefore, depression and its risk factors also place women at increased risk for contracting HIV.
From a theoretical perspective, it is logical to expect that depression plays a role in HIV prevention intervention outcomes for women. According to the theory of gender and power (Connell, 1987), there are three structures that illustrate gender interactions between men and women: (a) the sexual division of labor, (b) the sexual division of power, and (c) cathexis, or social norms and emotional attachment, all of which function at the societal and institutional levels. Wingood and DiClemente (2000) adapted the theory of gender and power to apply to HIV risk factors for women. In the sexual division of labor, for example, paying women less than men for similar work perpetuates a cycle whereby women are financially dependent upon men. The sexual division of power reflects women’s disempowerment through the media portrayal of women as sexual objects. Cathexis dictates what sexual behavior is appropriate for women and portrays motherhood as a valued role. These three phenomena lead to less ability to negotiate safe sex practices, condom use, education, power in relationships, and access to healthcare and increased homelessness in women (Wingood & DiClemente, 2000). These outcomes not only put women at risk for HIV but also for depression.
The sexual division of labor, sexual division of power, and cathexis highlight the lack of resources that some women experience in comparison to men. The network-individual-resource model (Johnson et al., 2010a) elucidates how the individual functions within one or more networks to fulfill his or her needs. The individual’s networks continually or intermittently interact with him or her to affect levels of resources that both the individual and network possess: (a) mental resources, including efficacy, control, intentions, skills, and attitudes and (b) tangible resources, including money, condoms, and physical health. The goal of the individual is to use the network to fulfill the deficit in resources. Therefore, network, resource, and power factors converge to put women at risk for HIV and depression. In the case of HIV, for example, if a woman has insufficient money, she may use her network to obtain this resource through commercial sex work. Deficits in mental (e.g., coping skills) and tangible (e.g., housing) resources can lead to depression, as discussed above.
Individuals who are depressed (DiFranceisco et al., 1998; Kim et al., 2006) and those most at risk for HIV (e.g., those who engage in high levels of sexual risk behavior; Noguchi et al., 2007) are less likely to complete interventions. If depressed women are not being retained in interventions, then they cannot reap the benefits of reducing sexual risk behavior (e.g., increased condom use, decreased rates of unprotected sex, decreased number of partners; Crepaz et al., 2009; Mize et al., 2002). Past meta-analyses of prevention interventions with women have shown significant decreases in sexual risk behavior (e.g., Crepaz et al., 2009; Mize et al., 2002). While these meta-analyses have taken into account some psychosocial variables (e.g., empowerment, self-efficacy), to date they have not examined how psychological functioning (e.g., depressive symptoms) plays a role in the efficacy of these interventions. Meta-analyses examining other populations (e.g., men who have sex with men, Herbst et al., 2005; adolescents, Mullen et al., 2002) also have not specifically addressed depression within the context of HIV prevention interventions.
Drawing on these theoretical perspectives, empirical studies, and past meta-analyses, the main foci of this meta-analysis were to examine (a) how sexual risk behavior and depression levels change in women as a result of completing an HIV prevention intervention, (b) whether baseline severity of depression moderates the change in sexual risk behavior from baseline to follow-up, and (c) whether components of HIV interventions are related to decreased depression and sexual risk.
Method
The current meta-analysis adheres to PRISMA guidelines (Moher et al., 2009).
Literature Search
Relevant studies were located through several search strategies. First, electronic databases were searched through September 1, 2010 using a Boolean search (PsycINFO, PubMED, Academic Search Premier, CINAHL, Psychology & Behavioral Sciences Collection, Women’s Studies International, ProQuest Dissertations and Theses, Scopus). Keyword searches included: HIV prevention AND depression AND women; HIV prevention AND depressive AND women; HIV- women AND depress* AND HIV intervention; depression OR depressive AND HIV prevention AND women; depression OR depressive AND HIV prevention AND women AND condom. A full-text search was conducted using the University of Connecticut’s Synthesis of HIV/AIDS Research Project’s (SHARP) Sexual Risk Reduction database which consists of digitized reports of HIV interventions and related research. Sexual risk behavior intervention articles housed by the CDC’s Prevention Research Synthesis group were full-text searched as well. The keyword depression was truncated as depress* in order to increase sensitivity in the full-text searchs. Reference lists of articles were also searched to identify other relevant published or unpublished studies. Additionally, five journals (Journal of Acquired Immune Deficiency Syndromes, AIDS & Behavior, AIDS Care, AIDS Education & Prevention and American Journal of Public Health) were searched online (January 2009–November 2010). Finally, a request for reports was also sent to several electronic listservs (Society of Behavioral Medicine; American Public Health Association; American Psychological Association, Division 12; European Association of Social Psychology; European Health Psychology Society), but no additional qualifying studies were obtained.
In order to be included in the sample, a study must (a) report on a face-to-face HIV/AIDS prevention intervention, (b) have a control condition, and (c) report separate analyses for women for depression and sexual risk behavior at baseline and at least one post-intervention assessment. Studies could be from any country or reported in any language, although only English reports were found. Studies were excluded if (a) the intervention included only men, people living with HIV/AIDS, or transgendered individuals, (b) the study was qualitative in nature, or (c) we could not obtain enough statistical information to calculate effect sizes. From the selection criteria and literature search, 10 studies (14 different intervention groups) were included in the analyses.
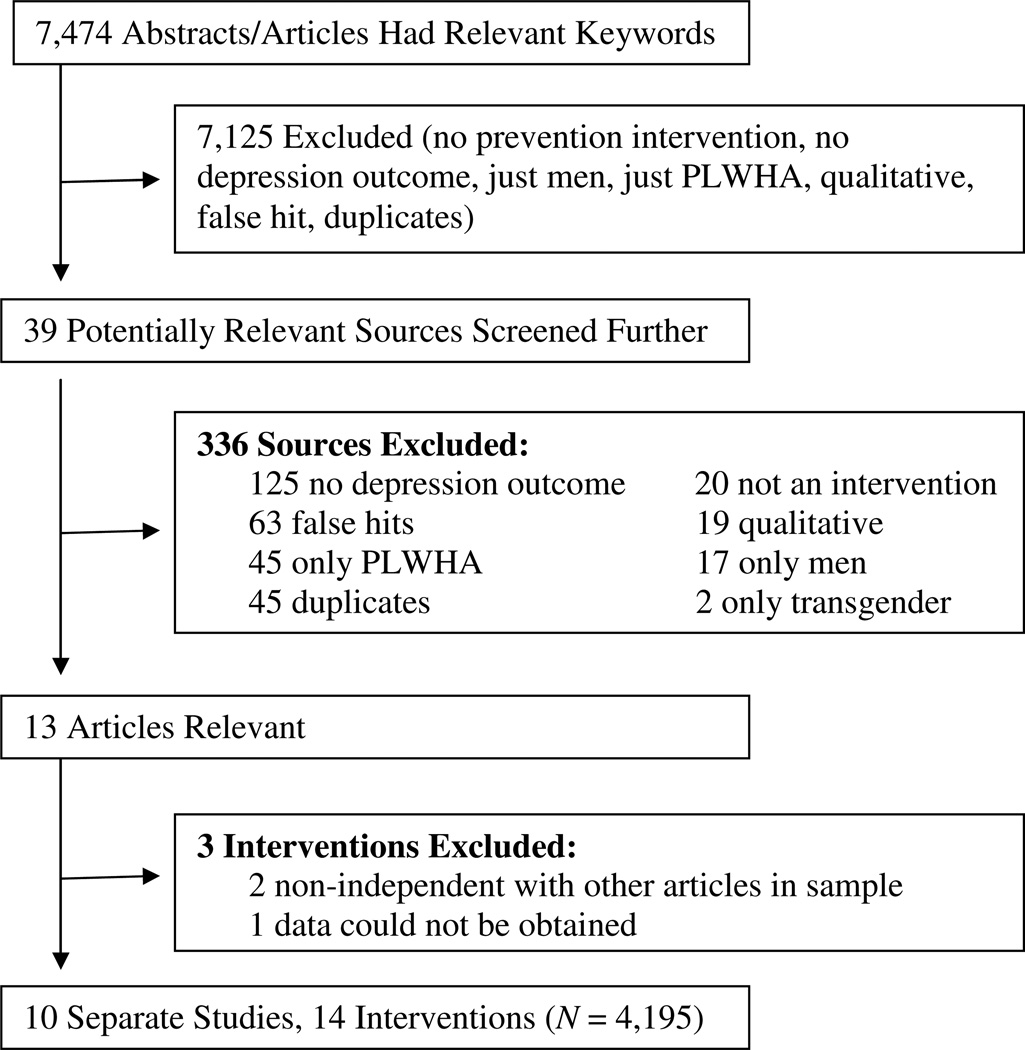
Coding
Each article, treatment group, and control group were coded. Article characteristics included such dimensions as (a) sex of first author; (b) year of data collection; (c) location of study, and (d) whether a theoretical framework guided the intervention design. Participant characteristics included (a) age; (b) race/ethnicity; (c) sample type (community, drug users, etc.); and (d) proportion of females in the sample. Design characteristics included (a) type of design (e.g., randomized controlled trial); (b) type of control group (e.g., HIV/AIDS education only); and (c) depression measure (e.g., Center for Epidemiological Studies Depression Scale [CES-D]). Intervention characteristics included (a) type of HIV/AIDS education, (b) type of motivational skills, (c) type of behavioral skills, (d) if condom information was provided, (e) if counseling and testing was provided, (f) if condoms were provided, (g) the number and length of sessions (length estimated when necessary), and (h) study quality (measure adapted from Jadad et al., 1996). Specific examples of intervention characteristics appear in Table 1. Thirteen reports met the inclusion criteria of the current meta-analysis. One report was excluded because it lacked statistical information necessary to calculate effect sizes (Tripiboon, 2001) and this information could not be obtained from the author; two other reports were excluded because their samples were non-independent from other studies included in the final sample (Nyamathi & Stein, 1997; Sales et al., 2010). Ten reports with a total of 14 intervention groups and a sample size of N = 4,195 were included in the final sample (Figure 1).
Table 1.
Coded intervention features by study.
| Intervention Feature |
Carey et al. (2010) | DiClemente et al. (2004) | DiClemente et al. (2009) | DiClemente et al. (2010) | Harris et al. (1998) |
|---|---|---|---|---|---|
| Sample | N = 555 (nc = 83; nB-INFO/I-INFO = 94, nB-INFO/I-IMB = 107, nBMI = 85, nBMI/I-INFO = 93, nBMI/I-IMB = 93); 64%AA, 23%W, 13%O, 9%:H; M age = 28.2 | N = 460 (nc = 241; nt = 219); 100%B, M age = 15.98 | N = 605 (nc = 316; nt = 289); 100%B; M age = 17.80 | N = 86 (nc = 39; nt = 47); 100%B; M age = 17.85 | N = 130 (nc = 57; nt = 73); 100%B; M age = 36.10 |
| Year of Data Collection | 2004 | 1996 | 2002 | 1999 | 1991 |
| Location | Rochester, NY | USA | Atlanta, GA | Atlanta, GA | Eastern U.S. city |
| Design | RCT | RCT | RCT | RCT | Random assignment |
| Type of Control Group | HIV/AIDS education only | Irrelevant content: nutrition & exercise | Other: Enhanced usual care comparison condition | Irrelevant content: good nutrition during pregnancy | No contact |
| Framework Used | Information-Motivation Behavioral Skills Model; Transtheoretical Model | Social Cognitive Theory; Theory of Gender & Power | Social Cognitive Theory; Theory of Gender & Power | Social Cognitive Theory; Theory of Gender & Power | Leininger's Culturally Congruent Care |
| Recruitment Site | Public walk-in STD clinic | Community health agencies | Community health clinics | Prenatal clinic at public hospital | Methadone maintenance clinic |
| Attrition Rate Baseline to FUP | 19.33% | 11.90% | 8.65% | 19.50% | 36% |
| Depression Measure | CES-D (9-item) | CES-D (brief 8-item version) | CES-D | CES-D (short version) | Rosenberg (1979) Depressive Affect Scale |
| Intervention Facilitators | Professional, paraprofessional; female | Peer, paraprofessional; female; ethnicity matched | Paraprofessional; female; ethnicity matched | Professional; both sexes represented; ethnicity matched | Professional |
| Study Quality (out of 21) | 15 | 17 | 18 | 14 | 16 |
| Intervention Feature | Ickovics et al. (1998) | Jewkes et al. (2008) | Nobles et al. (2009) | Nyamathi et al. (1993) | Nyamathi et al. (1998) |
| Sample | N = 136 (nc = 51; nt = 85); 54%W, 31%B, 11%H, 3%O; M age = 31.40 | N = 1086 (nc = 547; ne = 539); 100%AA; Age R = 15–26 | N = 149 (nc = 44; ne = 105); 100%B; M age = 30.26 | N = 858 (nc = 410; ne = 448); 81%AA, 19%H; M age = 32.8 | N = 130 (nc = 65; ne = 65); 91%AA, 8%H, 1%O; M age = 34.8 |
| Year of Data Collection | Not reported | 2003 | Not reported | Not reported | 1991 |
| Location | Connecticut | South Africa, Eastern Cape Province | USA | Los Angeles, CA | Los Angeles, CA |
| Design | Matched | RCT | Quasi-experimental | Random assignment | Quasi-experimental |
| Type of Control Group | No contact | Brief form of treatment (Stepping Stones) | No contact | HIV/AIDS education only | HIV/AIDS education only |
| Framework Used | None reported | None reported | Culturecology, African-Centered Behavioral Change | Comprehensive Health Seeking & Coping Paradigm | None reported |
| Recruitment Site | Community-based health clinics | School | Agencies providing services to African American Women | Women in homeless shelters or drug recovery programs | Women in homeless shelters or drug recovery programs |
| Attrition Rate Baseline to FUP | 25.40% | 24.45% | Not reported | 6.33% | 29.88% |
| Depression Measure | Hopkins Symptom Checklist (15 items) | CES-D | BDI | CES-D | CES-D |
| Intervention Facilitators | Paraprofessional | Paraprofessional; female | Professional, paraprofessional; female | Professional, paraprofessional; female | Professional, paraprofessional; ethnicity matched |
| Study Quality (out of 21) | 12 | 12 | 6 | 14 | 11 |
Note. N = number of participants, nc = number of participants in control condition, nt = number of participants in treatment condition; B-INFO/I-INFO = brief informational session followed by an intensive informational session; B-INFO/I-IMB = brief informational session followed by intensive information, motivation and behavioral skills training; BMI = brief motivational training; BMI/I-INFO = brief motivational training followed by an intensive informational session; BMI/I-IMB = brief motivational training followed by intensive information, motivation, and behavioral skills training; AA = African American, W = White, H = Hispanic/Latina, O = Other, STD = sexually transmitted disease, RCT = randomized controlled trial, CES-D = Center for Epidemiological Studies-Depression Scale, BDI = Beck Depression Inventory, FUP = Follow-up.
Figure 1.
Flow chart of selected studies. Note. False hits were characterized if the words depression, depressive, or depressed were mentioned only in the reference section or in the introduction of the article (e.g., stating that there is a relationship between depression and HIV risk behaviors). PLWHA = people living with HIV/AIDS.
Effect Size Calculation and Analysis
Effect sizes (ESs) were calculated from information provided in the article or from information received directly from the authors. For both sexual risk and depressive symptoms (termed depression throughout the current paper), ESs were calculated as the mean difference between pretest and posttest divided by the standard deviation of the pretest (Becker, 1988) for each group separately, correcting for sample size bias (Hedges, 1981). Multiple ESs were calculated if the study reported more than one intervention or multiple time measures, averaging ESs when there was more than one follow-up before or after eight months. Only data for women are included in the analyses. Sexual risk behavior was defined as unprotected intercourse, condom use, or number of partners. The sign of ESs was set so that negative values signify a decrease of either depression or sexual risk behavior, even when the absolute pattern might have been an increase of the behavior (e.g., an increase in condom use). Due to the small sample size of included studies, we examined sexual risk reduction broadly (i.e., averaged over types of risk behavior) rather than one specific sexual risk behavior (e.g., increased condom use).
The ESs were examined using fixed- and random-effects models (Lipsey & Wilson, 2001; Wilson, 2002); because there were no differences in results between these models only random-effects model estimations are reported, which can be more robustly generalized. The homogeneity statistic, Q, and the I2 index and its corresponding 95% confidence intervals (Huedo-Medina, et al., 2006) were calculated to determine whether each set of mean standardized mean differences (ES+s) plausibly shared a common parametric mean ES. Possible asymmetries in the distribution of the ESs, which may indicate reporting bias, were analyzed using Begg’s strategy (Begg & Mazundar, 1994) and Egger’s test (Egger et al., 1997).
To examine depression as a moderator, it was necessary to transform the scales into a common metric because a variety of measures appeared in the literature with a range of possible scores (e.g., 0–60 for the CES-D, 0–63 for the Beck Depression Inventory; Beck et al., 1979). Scales were placed on a uniform 0–100 scale based on the percent of maximum possible (POMP) score formula detailed below (Cohen et al., 1999):
Once all measures of depression were on the same metric, the scores on each scale could now plausibly be compared and depression could be examined as a potential moderator of the sexual risk ESs. To test the moderation effect of the baseline levels of depression and coded content on our targeted outcomes, sexual risk behavior and depression ESs were entered as the dependent variable into weighted least-squares regressions incorporating random-effects assumptions (Lipsey & Wilson, 2001). Confidence bands in figures and confidence intervals in tables for moderation patterns were created using the moving constant technique (Johnson & Huedo-Medina, in press).
Results
Description of Studies
Of the 10 included articles, 9 (90%) were conducted in the United States and 1 (10%) in South Africa. Seven (70%) used a theoretical framework to guide the intervention. The most common type of sample was a community sample (k = 6; 60%). The average age across samples was 28.04 years (range = 15.98–36.10; k = 9); 5 studies included 100% African Americans and 4 other studies had at least 30% African Americans, 4 studies included at least 8% Hispanic/Latina participants, 2 included at least 23% white participants, and 1 was an African sample. The mean number of intended session was 5.93 (range = 1–17) for treatment groups and 1.9 (range = 0–10) for control groups. On average, treatment group participants received 12.76 hours (range = 0.30–50.42) of contact and control group participants received 3.38 hours (range = 0–16). The median number of post-intervention follow-ups was 2.25 (range = 1–4). The first post-intervention assessment occurred, on average, at 16.50 weeks (SD = 9.01, range = 0–28 weeks) after the intervention and the last follow-up occurred, on average, at 52.55 weeks (SD = 8.62; range = 48–96 weeks). The most commonly used depression measure was the CES-D (70%; Radloff, 1977). Mean baseline levels of depression in participants were variable (range = 2.82–58.27). Sexual risk was assessed as unprotected sex in 5 studies (50%), condom use in 4 studies (40%), and by multiple sexual partners in 1 study (10%). Tables 1 and 2 provide qualitative summaries of intervention features.
Table 2.
Coded intervention components by study.
| Intervention Component |
Carey et al. (2010) B-INFO/I-INFO |
Carey et al. (2010) B-INFO/I-IMB |
Carey et al. (2010) BMI |
Carey et al. (2010) BMI/I-INFO |
Carey et al. (2010) BMI/I-IMB |
|---|---|---|---|---|---|
| Educational Components (C) | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention |
| Educational Components (T) | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention |
| Motivational Components (T) | None | For HIV prevention | For HIV prevention | For HIV prevention | For HIV prevention |
| Condom Components (C) | Condom provision | Condom provision | Condom provision | Condom provision | Condom provision |
| Condom Components (T) | Condom provision | Condom information, demonstration and skills, condom provision | Condom information and provision | Condom information and provision | Condom information, demonstration and skills, condom provision |
| HIV C & T (C) | Yes | Yes | Yes | Yes | Yes |
| HIV C & T (T) | Yes | Yes | Yes | Yes | Yes |
| Other Skills (T) | None | Communication, other (problem solving, identifying triggers, role playing) | None | None | Communication, other (problem solving, identifying triggers, role playing) |
| Risky Sexual Behavior Measure | Number of unprotected sexual episodes | Number of unprotected sexual episodes | Number of unprotected sexual episodes | Number of unprotected sexual episodes | Number of unprotected sexual episodes |
| Total Contact Time (HIV-Related content; C) | 20 (15) | 20 (15) | 20 (15) | 20 (15) | 20 (15) |
| Total Contact Time (HIV-Related Contact Time; T) | 260 (255) | 260 (255) | 20 (20) | 260 (260) | 260 (260) |
| Intervention Component | DiClemente et al. (2004) | DiClemente et al. (2009) | DiClemente et al. (2010) | Harris et al. (1998) | Ickovics et al. (1998) |
| Educational Components (C) | None | General HIV education, HIV prevention | None | None | None |
| Educational Components (T) | HIV prevention | HIV prevention, other (peer norms of condom use, negatives of douching) | HIV prevention, other (adverse consequences of STDs/HIV to unborn child & themselves) | General HIV education, HIV prevention, other (sex & sexuality as related to AIDS) | General HIV education, HIV prevention |
| Motivational Components (T) | For HIV prevention, bolster group identity | For HIV prevention, build self-esteem | Build self-esteem | For HIV prevention, build self-esteem, bolster group identity, other (e.g., empowerment) | None |
| Condom Components (C) | None | None | None | None | None |
| Condom Components (T) | Condom information, demonstration, and skills | Condom information, demonstration, and skills | Condom information and demonstration, and skills | None | None |
| HIV C & T (C) | No | No | No | No | No |
| HIV C & T (T) | No | No | No | No | Yes |
| Other Skills (T) | Communication, safe sex negotiation, other (role play, cognitive rehearsal) | Communication, other (facilitate male partner testing, role playing) | Communication, safe sex negotiation | None | None |
| Risky Sexual Behavior Measure | Unprotected sex (past 6 months) | Consistent condom use (past 60 days) | Consistent condom use (past 30 days) | Safer sex (condom use) | Level of sexual Risk (unprotected sex) |
| Total Contact Time (HIV-Related Contact Time; C)a | 960 (0) | 60 (60) | 120 (0) | 0 (0) | 0 (0) |
| Total Contact Time (HIV-Related Contact Time; T)a | 960 (600) | 540 (540) | 480 (480) | 1440 (864) | 40 (40) |
| Intervention Component | Jewkes et al. (2008) | Nobles et al. (2009) | Nyamathi et al. (1993) | Nyamathi et al. (1998) | |
| Educational Components (C) | General HIV education, HIV prevention | None | General HIV education, HIV prevention | General HIV education, HIV prevention | |
| Educational Components (T) | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention | General HIV education, HIV prevention | |
| Motivational Components (T) | None | Build self-esteem, bolster group identity | Build self-esteem, other (self-control) | Build self-esteem | |
| Condom Components (C) | Condom information | None | Condom information and provision | Condom information and provision | |
| Condom Components (T) | Condom information | None | Condom information, demonstration and practice on correctly using a condom, condom provision | Condom information, demonstration and practice on correctly using a condom, condom provision | |
| HIV C&T (C) | Yes | No | Yes | Yes | |
| HIV C & T (T) | Yes | No | Yes | Yes | |
| Other Skills (T) | Communication, other (role play) | Other (meditation, journaling) | Needle/syringe disinfection, other (coping responses, enhancing self-esteem and feelings of control) | Needle/syringe disinfection, other (how to cope/reduce stress, enhancing self-esteem & feelings of control | |
| Risky Sexual Behavior Measure | Correct condom use (at last sex) | Risky sexual behavior (unprotected sex) | Multiple sexual partners | Unprotected sex | |
| Total Contact Time (HIV-Related Contact Time; C)a | 205 (205) | 0 (0) | 130 (130) | 535 (535) | |
| Total Contact Time (HIV-Related Contact Time; T)a | 3,025 (1,523) | 1,920 (960) | 190 (150) | 1,060 (500) | |
Note. C = control group, T = treatment group, B-INFO/I-INFO = brief informational session followed by an intensive informational session; B-INFO/I-IMB = brief informational session followed by intensive information, motivation and behavioral skills training; BMI = brief motivational training; BMI/I-INFO = brief motivational training followed by an intensive informational session; BMI/I-IMB = brief motivational training followed by intensive information, motivation, and behavioral skills training, C & T = counseling and testing.
Contact time estimated where necessary.
All 14 treatment groups received an educational component; 11 (79%; percentage rounded to nearest whole number) received general HIV education (e.g., definition of HIV, symptoms) and all groups received HIV prevention education (e.g., condoms prevent transmission). Ten (71 %) treatment groups were given information about condoms (e.g., condoms are effective in decreasing HIV risk), half (k = 7) were given condoms and received a condom use demonstration from the facilitator, and 6 (43%) of the groups were given an opportunity to practice how to properly use a condom. Other skills that the treatment groups were taught included coping/self-management (k = 10, 71%), communication (k = 6, 43%), safe sex negotiation (k = 2, 14 %), role playing, (k = 3, 21%) and proper needle cleaning (k = 2; 14%). Eleven of the treatment groups (79%) received motivational components: Seven (50%) included motivation for prevention of HIV/AIDS (e.g., risk awareness), 6 (43%) included motivation to boost esteem, and 3 (21%) included motivation to bolster group identity (e.g., connect with other women and/or people of the same race/ethnicity). Five (50%) of the control groups received HIV prevention education and the same 5 (50%) were given general HIV education. Three (30%) of the control groups were given information about condoms, 2 (20%) were given condoms, and 5 (50%) received no content related to HIV risk. Control groups received no motivational or behavioral skill components.
Quantitative Analyses
Initial analyses revealed no significant differences between treatment and control groups on sexual risk or depression levels at either interval (first vs. last follow-up; see Table 3). Nonetheless, we found that control groups that received “active” HIV-related intervention components (e.g., HIV/AIDS education, condoms) saw larger decreases in sexual risk reduction compared to “true” control groups (i.e., no or irrelevant content, see Table 4). The lack of difference between groups, coupled with the fact that half of control groups included relevant preventive content, justified further analyses focused on temporal change for sexual risk and depression outcomes, treating results from both treatment and control groups as one group (see Table 3). Finally, there were no asymmetries in the distributions of the ESs, suggesting the absence of publication bias (Begg’s test [z = −0.15, p = 0.88; z = −1.22, p = 0.22]; Egger’s test [t = 0.97, p = 0.34; t = 0.29, p = 0.77] for sexual risk behavior and depression, respectively).
Table 3.
Weighted Mean Effect Sizes of Depression and Sexual Risk Behavior.
| Depression | Sexual Risk Behavior | |||||
|---|---|---|---|---|---|---|
| Condition | k | M weeks | ES+ (95% CI) | I2 (95% CI)a | ES+ (95% CI) | I2 (95% CI)a |
| Treatment | 13 | |||||
| First FUP | 17 | −0.22 (−0.33, −0.10) | 80.72 (68.59, 88.16) | −0.33 (−0.56, −0.11) | 93.69 (91.02, 95.57) | |
| Last FUP | 50 | −0.21 (−0.33, −0.09) | 83.21 (73.14, 89.50) | −0.29 (−0.39, −0.31) | 94.65 (92.51, 96.18) | |
| Control | 10 | |||||
| First FUP | 16 | −0.27 (−0.41, −0.13) | 88.32 (80.59, 92.97) | −0.30 (−0.57, −0.028) | 98.07 (97.42, 98.56) | |
| Last FUP | 51 | −0.28 (−0.42, −0.13) | 87.70 (79.41, 92.65) | −0.30 (−0.58, −0.025) | 98.15 (97.53, 98.61) | |
| Combined | 24 | |||||
| First FUP | 21 | −0.24 (−0.33, −0.15) | 84.11 (77.45, 88.80) | −0.32 (−0.49, −0.16) | 96.62 (95.79, 97.29) | |
| Last FUP | 39 | −0.24 (−0.33, −0.15) | 84.79 (78.52, 89.24) | −0.30 (−0.48, −0.12) | 96.88 (96.13, 97.48) | |
Note. A negative effect size indicates a decrease in depression or sexual risk behavior. M = mean, k = number of comparisons, ES+ = Weighted standardized mean difference effect size under random-effects assumptions. CI = Confidence interval. FUP = follow-up.
Significance implies rejection of the hypothesis of homogeneity
Table 4.
Sexual Risk Behavior as a Function of Control and Intervention Features at Last Follow-Up Assessment.
| Features of studiesa | ES+ib | 95% CI for ES+ | βc |
|---|---|---|---|
| Sample Characteristics | |||
| Baseline depression (k = 24) | −0.54** | ||
| Low (2.82) | 0.19 | −0.15, 0.53 | |
| High (58.27) | −0.72 | −1.03, −0.41 | |
| M age (k = 27) | −0.56** | ||
| 16 years | 0.034 | −0.31, 0.38 | |
| 36 years | −0.55 | −0.84, −0.26 | |
| Percent Hispanic/Latina (k = 24) | −0.36** | ||
| None | −0.087 | −0.29, 0.12 | |
| 19% | −0.81 | −1.17, −0.45 | |
| Type of population | 0.58*** | ||
| Risk group (k = 8) | −0.70 | −0.94, −0.46 | |
| General population (k = 16) | −0.094 | −0.27, 0.076 | |
| Intervention Components | |||
| Control content | −0.54** | ||
| Wait-list or irrelevant (k = 5) | −0.26 | −0.36, −0.16 | |
| Relevant (k = 5) | −0.44 | −0.50, −0.39 | |
| Condom provision | −0.52** | ||
| Absent (k = 14) | −0.13 | −0.34, 0.078 | |
| Present (k = 10) | −0.53 | −0.78, −0.28 | |
| Condom information | −0.47* | ||
| Absent (k = 11) | −0.079 | −0.32, 0.16 | |
| Present (k = 13) | −0.48 | −0.70, −0.26 | |
| Counseling and testing | −0.45* | ||
| Absent (k = 11) | −0.10 | −0.35, 0.14 | |
| Present (k = 13) | −0.46 | −0.68, −0.23 | |
| Intervention Impact on Depression | |||
| Effect size (d) for change in depression (k = 24) | 0.63*** | ||
| Large (d = −0.72) | −0.82 | −1.17, −0.48 | |
| None (d = 0.087) | 0.053 | −0.20, 0.31 |
Note. Abbreviations: CI, confidence interval; ES+ = Weighted standardized mean difference effect size.
When the feature is continuous, extremes of the observed feature are estimated.
Values under random-effects assumptions; negative ESs imply lower sexual risk behavior at the final available measures; estimates appear for observed extremes of continuous features
Standardized regression coefficient.
p < .05,
p < .01,
p < .001.
Change in sexual risk behavior and depression from baseline to follow-up
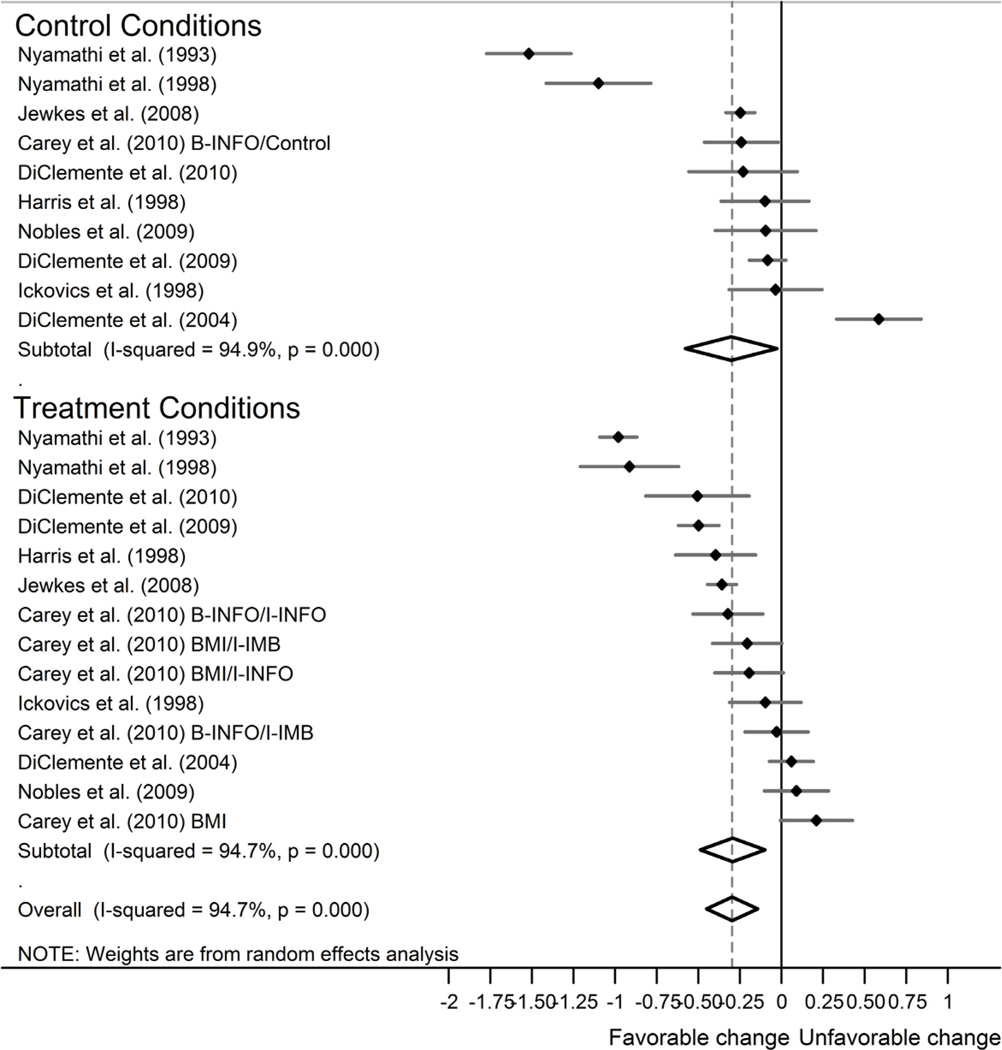
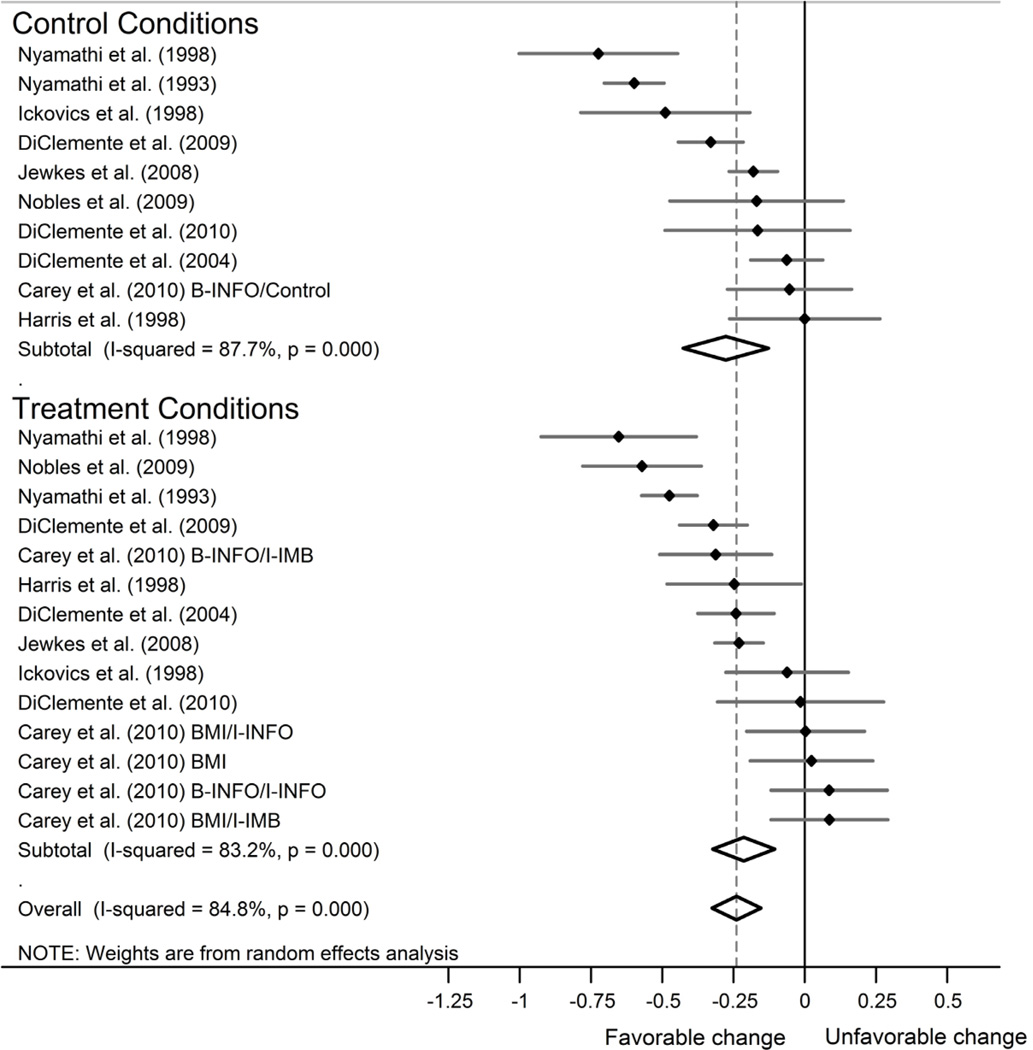
Figure 2 provides a forest plot of the distribution of sexual risk behavior ESs for both groups at the last follow-up. Overall, there was a small significant decrease in sexual risk behavior from baseline to first and last follow-up for the treatment, control, and combined groups (see Table 3). The significant I2 value implies that the ES results vary more from study to study than expected by sampling error alone and that more complex models (i.e., moderation models) are necessary. A forest plot of the distribution of depression ESs for both groups at the last follow-up appears in Figure 3. Overall, there was a small significant decrease in depression from baseline to first and last follow-up for the treatment, control, and combined groups (see Table 3), but effects were again marked by heterogeneity, as evidenced by a large I2 and significant Q statistic.
Figure 2.
Forest plot of effect sizes gauging sexual risk from baseline to the last available follow-up, grouped by condition and ordered by magnitude. Negative (positive) effect sizes correspond to a decrease (increase) in sexual risk. Confidence intervals (lines) for each effect size are significant when they do not include zero. Weighted mean effect sizes (diamonds) show a significant decrease in sexual risk behavior for each combination of conditions.
Figure 3.
Forest plot of effect sizes gauging depression from baseline to the last available follow-up, grouped by condition and ordered by magnitude. Negative (positive) effect sizes correspond to a decrease (increase) in depression. Confidence intervals (lines) for each effect size are significant when they do not include zero. Weighted mean effect sizes (diamonds) show a significant decrease in depression for each combination of conditions.
Baseline depression as a moderator of change in sexual risk behavior
Samples with higher baseline mean levels of depression exhibited more risk behavior change at the last assessment (r = −.46, p < .05), but when the amount of change in depression was standardized, this pattern was non-significant. Depression levels at baseline, follow-up length, and amount of change did not significantly relate to attrition (|rs|<.22).
Moderators of change in sexual risk behavior and depression
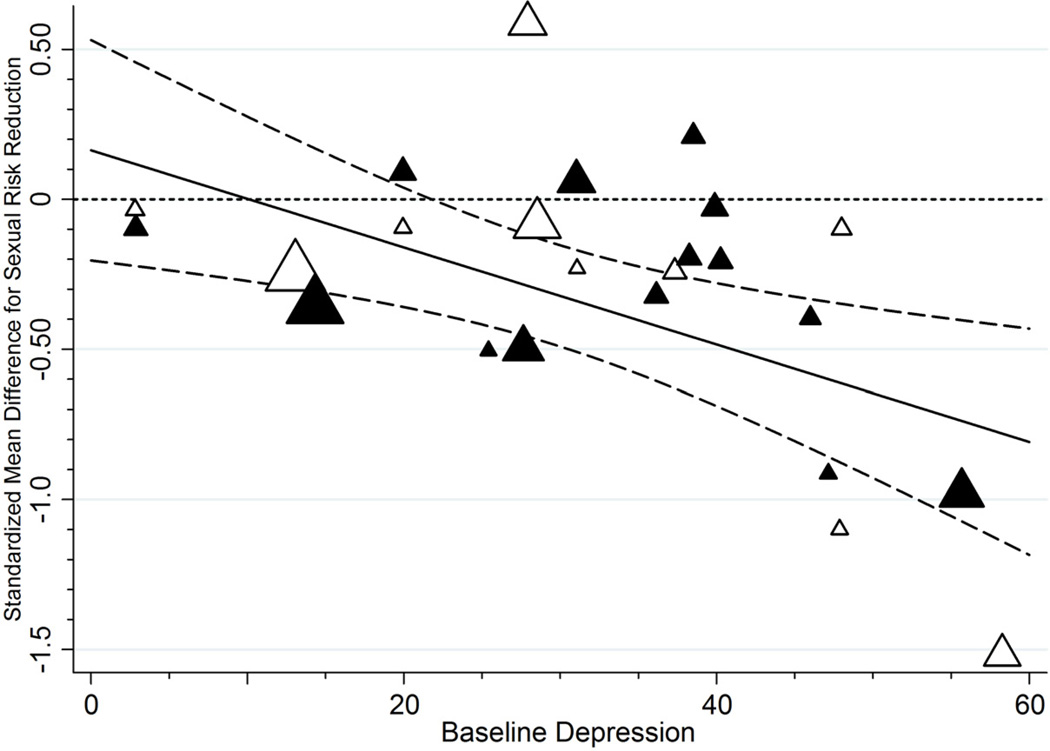
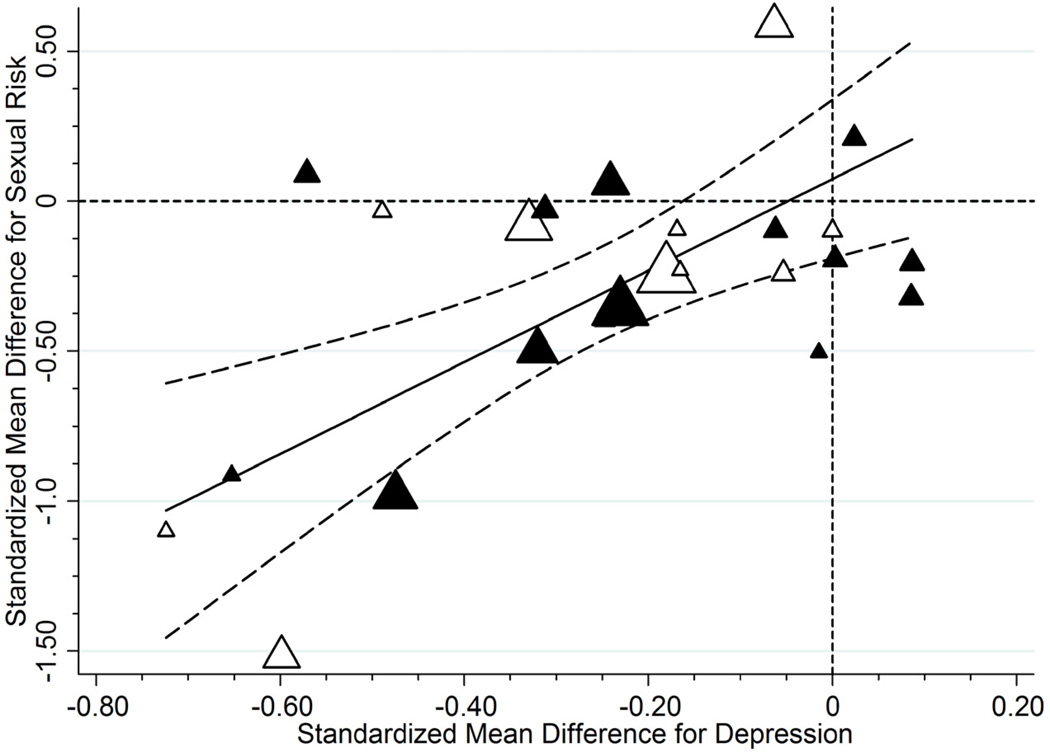
As Table 4 details, interventions were more successful in decreasing sexual risk behavior to the extent that they sampled (a) participants with higher baseline levels of depression (Figure 4), (b) older women, (c) larger percentages of Hispanics/Latinas, and (d) risk groups (e.g., drug users, homeless). Interventions also were more successful when they provided (e) condoms, (f) information about condoms, (g) HIV counseling and testing, and (h) active treatment components to the control group; finally, (i) interventions were more likely to reduce sexual risk behavior when they decreased depression to a large extent relative to baseline levels (Figure 5). As Table 5 details, interventions were more likely to decrease depression when they (a) had samples of only women (vs. also sampling men); (b) targeted risk groups (i.e., drug users, homeless); and (c) provided self-management and coping skills.
Figure 4.
Sexual risk reduction as a function of baseline depression. Sexual risk behavior declined following the intevention at the last available follow-up to the extent that samples had higher levels of baseline depression (treatment [control] group effects appear as black [white] triangles; the size of each plotted value reflects its weight in the analysis). The solid regression line indicates trends across initial levels of depression; dashed lines provide 95% confidence bands for these trends.
Figure 5.
Depression as a moderator of reductions in sexual risk behavior. Sexual risk behavior reductions at last available follow-up as a function of reductions of depression from baseline (treatment [control] group effects appear as black [white] triangles; the size of each plotted value reflects its weight in the analysis). The solid regression line indicates trends across levels of standardized change in depression levels; dashed lines provide 95% confidence bands for these trends.
Table 5.
Change in Depression as a Function of Control and Intervention Features at the Last Follow-Up Assessment.
| Features of studies | ES+ia | 95% CI for ES+ | βb |
|---|---|---|---|
| Sample Characteristics | |||
| Percentage of women sample | 0.52** | ||
| 52.5% | −0.082 | −0.21, 0.051 | |
| All women | −0.33 | −0.42, −0.22 | |
| Type of population | 0.34* | ||
| Risk group (k = 8) | −0.38 | −0.52, −0.24 | |
| General population (k = 16) | −0.16 | −0.26, −0.063 | |
| Intervention Components | |||
| Coping/self-management skills | −0.45** | ||
| Absent (k = 8) | −0.081 | −0.22, 0.063 | |
| Present (k = 16) | −0.31 | −0.40, −0.21 |
Note. Abbreviations: CI, confidence interval; ES+ = Weighted standardized mean difference effect size.
Values under random effects assumptions; negative ESs imply lower levels of depression at the last evaluation.
Standardized regression coefficient.
p < .05,
p < .01,
p < .001.
Discussion
To our knowledge, this meta-analytic review is the first to document that primary HIV prevention interventions can successfully address not only HIV risk but also depression levels in at-risk women. Overall, women participating in behavioral interventions targeting sexual risk reduction against HIV infection exhibited significant decreases in both depressive symptoms and sexual risk behavior at follow-up regardless of follow-up length and intervention condition. Overall, interventions that ameliorated depression the most also had the largest sexual risk reduction; indeed, the confidence bands in Figure 5 reveal that on average, interventions had non-significant risk reduction unless they also reduced depression levels at least somewhat. Importantly, decreases in sexual risk behavior from baseline to follow-up paralleled decreases in levels of depression from baseline over the same period.
In the current sample of trials that also included depression outcomes, patterns of sexual risk reduction (Table 4) generally mirrored results from past meta-analyses that did not require included studies to measure depression. Speaking to the generalizability of our results, many of our findings are akin to past domestic (e.g., Crepaz et al., 2009; Mize et al., 2002) and international (e.g., Huedo-Medina et al., 2010) meta-analyses showing that prevention interventions are successful in decreasing sexual risk behavior when they target women. Our results also support past findings that greater risk reduction appears in samples of young adults compared to adolescents (Johnson et al., 2010b, Noar, 2008), samples with larger percentages of Hispanics/Latinos (Albarracín et al., 2008), samples provided with condoms (Johnson et al., 2003), and a broad sample of interventions with sexual frequency outcomes (Smoak et al., 2006). More generally, providing condoms and condom information, as well as HIV counseling and testing, appears to afford participants the mental and tangible resources necessary to reduce sexual risk behavior (Johnson et al., 2010a). It may be beneficial, however, to evaluate outcomes for interventions that measure depression as compared to those that do not measure depression. Our results suggest that depressive symptoms may be acting as an often unmeasured—or unreported—mechanism of change in sexual risk behavior.
It is important to note that decreasing levels of depression was not a stated goal of these interventions, with only two exceptions (Harris et al., 1998; Jewkes et al., 2008). Because depression was a secondary outcome in nearly all of the included studies, it is remarkable to see a significant decrease in depression in both groups. Given that drug trials commonly document robust placebo effects even for samples and patients with very severe depression (Fournier et al., 2010; Kirsch et al., 2008), it is conceivable that HIV interventions act as a sort of placebo agent, thereby reducing depression levels in participants. More plausibly, interventions may act as a form of social support for participants, which have been found to decrease risk of depression in women (Kendler et al., 2005). Social support may also explain why interventions with only female participants were more effective in decreasing levels of depression compared to interventions that also included male participants. In addition, when participants were taught coping and self-management skills (Table 5), there was a larger decrease in depression. Arming participants with skills that are necessary to manage factors that may contribute to depression (e.g., stress) seems to aid in managing depression and may be the reason why our review found no association between depression and the rates of completing trials. This finding is extremely pertinent as reductions in depression and sexual risk behavior seem to go hand-in-hand.
The qualitative analysis of the literature highlights the lack of uniformity in intervention design (e.g., type of intervention components). Overall, control groups received a high number of the intervention components which could account for the lack of differences between control and treatment groups. Control groups received a high level of care with 5 (50%) receiving HIV/AIDS education and 4 (40%) receiving HIV counseling and testing (Table 1). Because control arms resembled treatment arms, we combined the groups in order to detect the main components that were affecting study results. Our findings parallel results of some other health promotion meta-analyses that have shown that the content of the control arm affects comparisons between treatment and control (e.g., de Bruin et al., 2010; Johnson et al., 2003).
Several limitations apply to the current meta-analysis. First, despite an extensive search (Figure 1), the small number of studies available (k = 10, 24 groups) limits power and the ability to find conclusive results, test certain moderators (e.g., intervention components), and generalize to other countries and cultures. Second, all of the qualifying studies were published in peerreviewed journals and no unpublished studies were obtained (e.g., dissertations), even though they could have qualified if found. Third, this study highlights the need to capture “fugitive” literature through more extensive access to full-text searching options. Most available databases (e.g., PubMED, PsycINFO) only permit keyword searches of the title and abstract and cannot identify those reports in which a particular variable (e.g., depression) was not a main focus. To that end, we cannot be certain that all relevant studies were included in this meta-analysis. Fourth, the current results do not speak to the temporal ordering of change: It is possible that reducing sexual risk is empowering and therefore ameliorates depression rather than the reverse, although one longitudinal study suggests that higher rates of depressive symptoms leads to riskier sexual behavior (Williams & Latkin, 2005). Finally, the current results cannot address whether the link between depression and sexual risk behavior change observed is due to regression to the mean, floor effects, or unmeasured third variables.
The current meta-analysis highlights the importance of examining depression within the context of HIV prevention interventions, especially since AIDS is a leading cause of death in the United States (Heron, 2011) and worldwide (World Health Organization, 2009), women are more likely to be diagnosed with depression than men (Pratt & Brody, 2008), and HIV and depression share common risk factors. The theory of gender and power (Connell, 1987; Wingood & DiClemente, 2000) and the network-individual-resource model (Johnson et al., 2010a) highlight the theoretical threats that place women at risk for HIV (e.g., lack of resources, power, and healthy networks/social support) and these theories can be applied to depression as well. Interventions conducted with people living with HIV/AIDS are also effective in decreasing depression (Sherr et al., 2011), indicating that depression may have implications for both primary and secondary HIV prevention. Because a significant decrease in depression was found without interventions explicitly addressing depression, it is conceivable that an even larger decrease in depression and sexual risk behavior could be obtained if depression is directly addressed. Although we cannot determine causality, future trials could address the sequential timing of the depression-sexual risk behavior link. Future research should also explore whether the patterns obtained in this review match those for other samples such as men and transgendered individuals who participate in HIV prevention intervention trials. Finally, future research should elucidate the causal relationship between depression and sexual risk behavior.
Acknowledgments
We extend our gratitude to Michael P. Carey, Ralph J. DiClemente, Jeanette R. Ickovics, Rachel Jewkes, Wade Nobles, and Jessica M. Sales for providing us information about their HIV prevention trials. We also thank Michelle R. Warren and four anonymous reviewers for comments on earlier drafts of this manuscript.
This research was supported by an NIH traineeship to Carter A. Lennon under U. S. Public Health Service Institutional National Research Service Award T32-MH074387 (PI: Seth C. Kalichman) and grants R01-MH58563 and K18-AI094581 (PI: Blair T. Johnson).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
* indicates reference was included in the meta-analysis.
- Albarracín J, Albarracín D, Durantini M. Effect of HIV-prevention interventions for samples with higher and lower percents of Latinos and Latin Americans: A meta-analysis of change in condom use and knowledge. AIDS & Behavior. 2008;12:521–543. doi: 10.1007/s10461-007-9209-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychological Association. Women and depression. [Retrieved April 2, 2010];2010 from http://www.apa.org/about/gr/issues/women/depression.aspx. [Google Scholar]
- Beadnell B, Baker S, Knox K, Stielstra S, Morrison DM, Degooyer E, Oxford M. The influence of psychosocial difficulties on women’s attrition in an HIV/STD prevention programme. AIDS Care. 2003;15(6):807–820. doi: 10.1080/09540120310001618658. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford; 1979. [Google Scholar]
- Becker BJ. Synthesizing standardized mean-change measures. British Journal of Mathematical and Statistical Psychology. 1988;41(2):257–278. [Google Scholar]
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;4(50):1088–1101. [PubMed] [Google Scholar]
- *.Carey MP, Senn TE, Vanable PA, Coury-Doniger P, Urban MA. Brief and intensive behavioral interventions to promote sexual risk reduction among STD clinic patients: Results from a randomized controlled trial. AIDS & Behavior. 2010;14:504–517. doi: 10.1007/s10461-009-9587-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. HIV among women. [Retrieved October 26, 2011];2011a from http://www.cdc.gov/hiv/topics/women/index.htm.
- CDC. HIV surveillance—United States, 1981–2008. [Retrieved October 26, 2011];Morbidity and Mortality Weekly Report. 2011b 60(21):689–693. from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6021a2.htm?s_cid=mm6021a2_w. [PubMed] [Google Scholar]
- Cohen P, Cohen J, Aiken LS, West SG. The problem of units and the circumstances for POMP. Multivariate Behavioral Research. 1999;34(3):315–346. [Google Scholar]
- Connell RW. Gender and power. Stanford, CA: Stanford University Press; 1987. [Google Scholar]
- Crepaz N, Marshall KJ, Aupont LW, Jacobs ED, Mizuno Y, Kay LS, O’Leary A. The efficacy of HIV/STI behavioral interventions for African American females in the United States: A meta-analysis. American Journal of Public Health. 2009;99(11):2069–2078. doi: 10.2105/AJPH.2008.139519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin M, Viechtbauer W, Schaalma HP, Kok G, Abraham C, Hospers HJ. Standard care impact on effects of highly active antiretroviral therapy adherence interventions: A meta-analysis of randomized controlled trials. Archives of Internal Medicine. 2010;170(3):240–250. doi: 10.1001/archinternmed.2009.536. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lopman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist. In: Pichot P, editor. Psychological measurement in psychopharmacology: Modern problems in pharmacopsychiatry. Vol. 7. Basel, Switzerland: Karger; 1974. pp. 79–110. [DOI] [PubMed] [Google Scholar]
- *.DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Robillard A. Efficacy of an HIV prevention intervention for African American adolescent girls: A randomized controlled trial. Journal of the American Medication Association. 2004;292:171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- *.DiClemente RJ, Wingood GM, Rose ES, Sales JM, Lang DL, Caliendo AM, Hardin JW, Crosby RA. Efficacy of a sexually transmitted disease/human immunodeficiency virus sexual risk-reduction intervention for African American adolescent females seeking sexual health services. Archives of Pediatric Adolescent Medicine. 2009;163:1112–1121. doi: 10.1001/archpediatrics.2009.205. [DOI] [PubMed] [Google Scholar]
- *.DiClemente RJ, Wingood GM, Rose E, Sales JM, Crosby RA. Evaluation of an HIV/STD sexual risk-reduction intervention for pregnant African American adolescents attending a prenatal clinic in an urban public hospital: Preliminary evidence of efficacy. Journal of Pediatric and Adolescent Gynecology. 2010;23:32–38. doi: 10.1016/j.jpag.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranceisco W, Kelly JA, Sikkema KJ, Somlai AM, Murphy DA, Stevenson LY. Differences between completers and early dropouts from 2 HIV intervention trials. A health belief approach to understanding prevention program attrition. American Journal of Public Health. 1998;88(7):1068–1073. doi: 10.2105/ajph.88.7.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey G, Schneider M, Minder C. Bias in meta-analysis detected by a simple graphical test. British Medical Journal. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J. Antidepressant drug effects and depression severity. A patient-level meta-analysis. Journal of American Medical Association. 2010;303:47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Harris RM, Bausell RB, Scott DE, Hetherington SE, Kavanagh KH. An intervention for changing high risk HIV behaviors of African American drug-dependent women. Research in Nursing & Health. 1998;21(3):239–250. doi: 10.1002/(sici)1098-240x(199806)21:3<239::aid-nur7>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. Journal of Educational and Behavioral Statistics. 1981;6(2):107–128. [Google Scholar]
- Herbst JH, Sherba RT, Crepaz N, DeLuca JB, Zohrabyan L, Stall RD, Lyles CM. A meta-analytic review of HIV behavioral interventions for reducing sexual risk behavior of men who have sex with men. Journal of Acquired Immune Deficiency Syndromes. 2005;39:228–241. [PubMed] [Google Scholar]
- Heron M. Deaths: Leading causes for2007. National Vital Statistics Reports. 2011;59(8):1–06. [PubMed] [Google Scholar]
- Huedo-Medina TB, Boynton MH, Warren MR, LaCroix JM, Carey MP, Johnson BT. Efficacy of HIV prevention interventions in Latin American and Caribbean Nations, 1995–2008: A meta-analysis. AIDS & Behavior. 2010;14:1237–1251. doi: 10.1007/s10461-010-9763-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huedo-Medina TB, Sánchez-Meca J, Martín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods. 2006;11(2):193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- *.Ickovics JR, Druley JA, Grigorenko EL, Morrill AC, Beren SE, Rodin J. Long-term effects of HIV counseling and testing for women: Behavioral and psychological consequences are limited at 18 months posttest. Health Psychology. 1998;17(5):395–402. doi: 10.1037//0278-6133.17.5.395. [DOI] [PubMed] [Google Scholar]
- Jadad AR, Moore A, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clinical Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- *.Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, Duvvury N. Impact of Stepping Stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: Cluster randomised controlled trial. British Medical Journal. 2008;337(7666) doi: 10.1136/bmj.a506. Retrieved from http://www.bmj.com/cgi/reprint/337/aug07_1/a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BT, Carey MP, Marsh KL, Levin KD, Scott-Sheldon LAJ. Interventions to reduce sexual risk for the Human Immunodeficiency Virus in adolescents, 1985–2000: A research synthesis. Archives of Pediatrics & Adolescent Medicine. 2003;157:381–388. doi: 10.1001/archpedi.157.4.381. [DOI] [PubMed] [Google Scholar]
- Johnson BT, Huedo-Medina TB. Depicting estimates using the intercept in meta-regression models: The moving constant technique. Research Synthesis Methods. doi: 10.1002/jrsm.49. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BT, Redding CA, DiClemente RJ, Mustanski BS, Dodge BM, Sheeran P, Fishbein M. A network-individual-resource model for HIV prevention. AIDS & Behavior. 2010a;S14:S204–S221. doi: 10.1007/s10461-010-9803-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson BT, Scott-Sheldon LA, Carey MP. Meta-synthesis of health behavior change meta-analyses. American Journal of Public Health. 2010b;100:2193–2198. doi: 10.2105/AJPH.2008.155200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Myers J, Prescott CA. Sex differences in the relationship between social support and risk for major depression: A longitudinal study of opposite-sex twin pairs. The American Journal of Psychiatry. 2005;162(2):250–256. doi: 10.1176/appi.ajp.162.2.250. [DOI] [PubMed] [Google Scholar]
- Kim Y-J, Peragallo N, DeForge B. Predictors of participation in an HIV risk reduction intervention for socially deprived Latino women: A cross-sectional cohort study. International Journal of Nursing Studies. 2006;43:527–534. doi: 10.1016/j.ijnurstu.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Kirsch I, Deacon BJ, Huedo-Medina TB, Scoboria A, Moore TJ, Johnson BT. Initial severity and antidepressant benefits: A meta-analysis of data submitted to the Food and Drug Administration. PLoS Medicine. 2008;5:260–268. doi: 10.1371/journal.pmed.0050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey MW, Wilson DB. Practical meta-analysis: Applied social research methods. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-anlaysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Mize SJS, Robinson BE, Bockting WO, Scheltema KE. Meta-analysis of the effectiveness of HIV prevention interventions for women. AIDS Care. 2002;14(2):163–180. doi: 10.1080/09540120220104686. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine. 2009;6(6):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossakowski KN. The influence of past unemployment duration on symptoms of depression among young women and men in the United States. American Journal of Public Health. 2009;99:1826–1832. doi: 10.2105/AJPH.2008.152561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullen PD, Ramírez G, Strouse D, Hedges LV, Sogolow E. Meta-analysis of the effects of behavioral HIV prevention interventions on the sexual risk behavior of sexually experienced adolescents in controlled studies in the United States. Journal of Acquired Immune Deficiency Syndromes. 2002;30:S94–S105. [PubMed] [Google Scholar]
- Noar SM. Behavioral interventions to reduce HIV-related sexual risk behavior: Review and synthesis of meta-analytic evidence. AIDS and Behavior. 2008;12:335–353. doi: 10.1007/s10461-007-9313-9. [DOI] [PubMed] [Google Scholar]
- *.Nobles WW, Goddard LL, Gilbert DJ. Culturecology, women, and African-centered HIV prevention. Journal of Black Psychology. 2009;35:228–246. [Google Scholar]
- Noguchi K, Albarracín D, Durantini MR, Glasman LR. Who participates in which health promotion programs? A meta-analysis of motivations underlying enrollment and retention in HIV-prevention interventions. Psychological Bulletin. 2007;133(6):955–975. doi: 10.1037/0033-2909.133.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Nyamathi AM, Leake B, Flaskerud J, Lewis C, Bennett C. Outcomes of specialized and traditional AIDS counseling programs for impoverished women of color. Research in Nursing & Health. 1993;16:11–21. doi: 10.1002/nur.4770160104. [DOI] [PubMed] [Google Scholar]
- *.Nyamathi AM, Flaskerud J, Keenan C, Leake B. Effectiveness of a specialized vs. traditional AIDS education program attended by homeless and drug-addicted women alone or with supportive partners. AIDS Education and Prevention. 1998;10(5):433–446. [PubMed] [Google Scholar]
- Nyamathi AM, Stein JA. Assessing the impact of HIV risk reduction counseling in impoverished African American women: A structural equations approach. AIDS Education and Prevention. 1997;9(3):253–273. [PubMed] [Google Scholar]
- Pratt LA, Brody DJ. Depression in the United States household population, 2005–2006. NCHS Data Brief. 2008;7:1–8. [PubMed] [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker A, Hall HI for the HIV Incidence Surveillance Group. Estimated HIV incidence in the United States, 2006–2009. PLos ONE. 2011;6(8):1–13. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rosenberg M. Conceiving the self. New York: Basic Books; 1979. [Google Scholar]
- Sales JM, Lang DL, Hardin JW, DiClemente RJ, Wingood GM. Efficacy of an HIV prevention program among African American female adolescents reporting high depressive symptomatology. Journal of Women’s Health. 2010;18:219–227. doi: 10.1089/jwh.2008.1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seth P, Raiji PT, DiClemente RJ, Wingood GM, Rose E. Psychological distress as a correlate of a biologically confirmed STI, risky sexual practices, self-efficacy and communication with male sex partners in African-American female adolescents. Psychology, Health & Medicine. 2009;14:291–300. doi: 10.1080/13548500902730119. [DOI] [PubMed] [Google Scholar]
- Sherr L, Clucas C, Harding R, Sibley E, Catalan J. HIV and depression – a systematic review of interventions. Psychology, Health & Medicine, online first. 2011:1–35. doi: 10.1080/13548506.2011.579990. [DOI] [PubMed] [Google Scholar]
- Smoak ND, Scott-Sheldon LAJ, Johnson BT, Carey MP. Sexual risk reduction interventions do not inadvertently increase the overall frequency of sexual behavior: A meta-analysis of 174 studies with 116,735 participants. Journal of Acquired Immune Deficiency Syndromes. 2006;41:374–384. doi: 10.1097/01.qai.0000185575.36591.fc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tripiboon D. A HIV/AIDS prevention program for married women in rural northern Thailand. Australian Journal of Primary Health. 2001;7(3):83–90. [Google Scholar]
- Williams CT, Latkin CA. The role of depressive symptoms in predicting sex with multiple and high-risk partners. Journal of Acquired Immunodeficiency Syndromes. 2005;38:69–73. doi: 10.1097/00126334-200501010-00013. [DOI] [PubMed] [Google Scholar]
- Wilson DB. Meta-analysis macros for SAS, SPSS, and Stata [Computer Software] [Retrieved, April 5, 2010];2002 from http://mason.gmu.edu/~dwilsonb/ma.html. [Google Scholar]
- Wingood GM, DiClemente RJ. Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health Education & Behavior. 2000;27(5):539–565. doi: 10.1177/109019810002700502. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Women’s health. [Retrieved March 26, 2011];2009 from http://www.who.int/mediacentre/factsheets/fs334/en/