Abstract
BACKGROUND:
Reconstruction of acquired auricular defects is a challenging procedure. Since its emergence, the helical advancement technique has proved to be an excellent method of repairing many auricle defects. This technique may occasionally result in an alteration in the dimensions of the neoauricle, with subsequent deformity. However, the advantages of this technique are well known, while the pitfalls are scarce.
OBJECTIVE:
To critically review the selection criteria of patients with acquired auricular defects to determine which are eligible for helical advancement technique without subsequent deformity.
METHODS:
From March 2004 to January 2006, 18 patients with three types of upper one-third auricle defects underwent the helical advancement procedure. All patients were male, with mean age of 33.5 years. The defects ranged from 1.2 cm to 4.3 cm in length. Two helical flaps (one on either side of the injury) were advanced along the helical margin to ensure closure. The vertical and horizontal auricular axes were measured before and after surgery, and the actual reduction in millimetres was calculated. Patients were followed up for three months postoperatively. Assessment of the surgical outcome was performed by surgeon (with patient feedback) in the final patient visit.
RESULTS:
The principle pitfall in the form of small neoauricle with or without cupping was reported in five patients (27.77%). The defects in these cases were >2.8 cm and the mean resultant reduction in vertical axes was >5 mm. Statistical analysis resulted in χ2=4.24 and P=0.04
CONCLUSION:
The three varieties of upper one-third auricle defects can best be corrected by the helical advancement technique when the defect is <2.8 cm. Furthermore, perioperative reduction in the vertical axis of the neoauricle >5 mm was an important predictive factor in the development of subsequent deformity.
Keywords: Acquired ear deformity, Antia and Buch, Chondrocutaneous flap, Helical advancement
Abstract
HISTORIQUE :
Les anomalies acquises de l’oreille ont toujours posé un défi de reconstruction. Depuis son émergence, la technique d’avancement de l’hélix s’est révélée une excellente méthode pour réparer de nombreuses anomalies de l’oreille. Cette technique peut parfois provoquer une altération de la dimension du nouveau pavillon et une malformation subséquente. Cependant, ses avantages sont bien connus et ses écueils sont rares.
OBJECTIF :
Procéder à l’analyse critique des critères de sélection des patients ayant des anomalies acquises de l’oreille pour déterminer ceux qui sont admissibles à la technique d’avancement de l’hélix, sans risque de malformation subséquente.
MÉTHODOLOGIE :
De mars 2004 à janvier 2006, 18 patients présentant trois types d’anomalies du tiers supérieur de l’oreille ont subi une intervention d’avancement de l’hélix. Les patients, tous de sexe masculin, avaient un âge moyen de 33,5 ans. Les anomalies mesuraient de 1,2 cm à 4,3 cm. Les médecins ont fait avancer deux lambeaux de l’hélix (de chaque côté de la blessure) sur le bord de l’hélix, pour en garantir la fermeture. Ils ont mesuré les axes vertical et horizontal de l’oreille avant et après l’opération et calculé la réduction obtenue, en millimètres. Ils ont suivi les patients jusqu’à trois mois après l’opération. Le chirurgien a procédé à l’évaluation des résultats de l’opération (compte tenu des commentaires du patient) lors de la dernière visite du patient.
RÉSULTATS :
Le principal écueil, la formation d’un nouveau petit pavillon avec ou sans cupule, a été signalé chez cinq patients (27,77 %). Dans ces situations, les malformations mesuraient plus de 2,8 cm et la réduction moyenne des axes verticaux, plus de 5 mm. L’analyse statistique a résulté en un χ2=4,24 et en un P=0,04.
CONCLUSION :
Les trois variétés d’anomalies du tiers supérieur de l’oreille sont mieux corrigées par la technique d’avancement de l’hélix lorsqu’elles mesurent moins de 2,8 cm. De plus, une réduction périopératoire de l’axe vertical du nouveau pavillon supérieure à 5 mm constitue un important facteur prédictif de malformation subséquente.
Reconstruction of acquired auricular defects is one of the most challenging procedures confronting plastic surgeons. These defects are commonly caused by trauma, motor vehicle accidents, sports injury, human fights, and human and animal bites (1). Less commonly, auricular defects are acquired as the result of thermal injury, with subsequent dry gangrene and autoamputation (2). The treatment of auricular tumours by Mohs chemosurgery also results in the need for auricular repair (3). An exceptional rare cause of auricular defect is the method of political punishment that was practiced in Iraq circa 1994, as reported in our case series study.
Since the emergence of the helical advancement technique more than four decades ago, it has proved to be an excellent method of repairing many defects confined to the helical margin with or without scaphal cartilage involvement (3–6). The benefits of this technique include patient convenience, superior cosmesis, hidden scar, technical simplicity, preserved normal auricular anatomical landmarks and low risk of flap necrosis. Furthermore, its one-stage procedure requires a short learning curve and is easily reproducible (4–7). The reported pitfalls are scarce.
In the present article, the reconstructive outcome of the helical advancement technique to repair a variety of auricular defects is reviewed. In particular, the selection criteria were examined with a view to avoiding subsequent deformity.
METHODS
A prospective study was conducted from March 2004 to January 2006. The study sample was selected from patients with acquired auricular defects who were referred to the plastic surgery unit at Alkindy Teaching Hospital, Baghdad, Iraq, for reconstruction. In total, 18 patients with three types of upper one-third auricle defects (helical rim, wedge and upper one-third [Figure 1]) were selected to undergo reconstruction with the helical advancement flap technique (Table 1). The size of the defects along the helical margins ranged from 1.2 cm to 4.3 cm, the Y-shape antihelical ridges were preserved in all three types, and the triangular fossae were mostly intact. All patients were male, and 30 to 37 years of age (mean age 33.5 years). The mechanism of injury dated back to circa 1994, a result of punishment practiced on opponents of the political regime. In all cases, the elapsed date from the injury was 10 to 12 years. Initial physical and psychological assessments were undertaken, and all injuries were photographed preoperatively.
Figure 1).
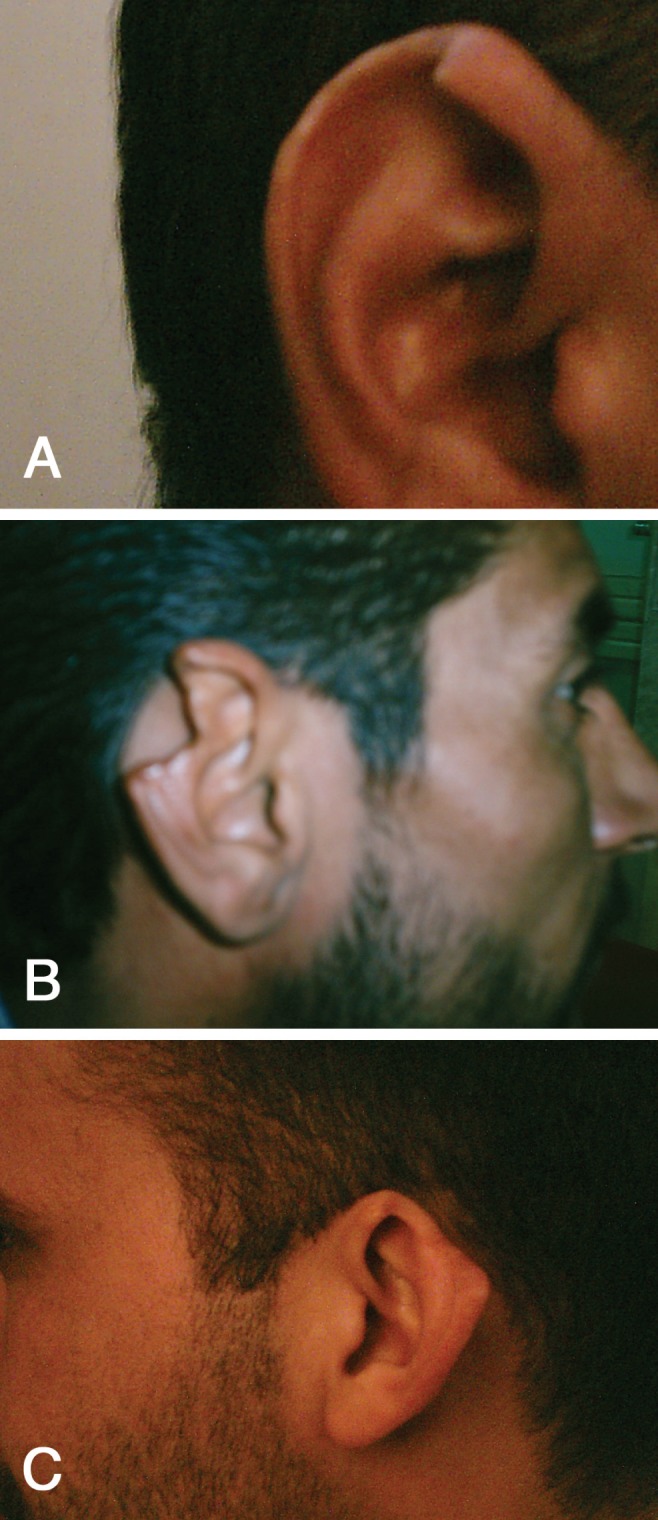
A Helical rim injury; B Wedge injury; C Upper one-third injury of the auricle
TABLE 1.
Types of upper one-third auricle defects
| Defect | n (%) |
|---|---|
| Auricle rim | 3 (16.66) |
| Auricle wedge | 3 (16.66) |
| Auricle upper one-third | 12 (66.66) |
| Total | 18 (100) |
The surgical procedure was explained and all patients provided written informed consent. After the patient was anesthetized, the contralateral (uninjured) auricle was measured vertically (V1) and horizontally (H1), and the measurements recorded. The length of the defect along helical rim was also recorded (Figure 2). Two helical chondrocutaneous flaps, one on either side of the defect were created by performing an anterior incision along the remnant helical groove (Figure 3). The incision included skin and the cartilage, with the posterior auricle skin left intact. Subsequent undermining of the scaphal cartilage medially provided further mobilization of the flaps. When necessary, an additional incison to circumvent the helical root gave extra length by V-Y advancement. Flaps were advanced along the helical margin to ensure closure. Following closure, if a tented or cupped scapha occurred, a Burow’s triangle from the scaphal cartilage was excised to relieve the tented part of the cartilage. After auricle closure, vertical (V2) and horizontal (H2) axes of the neoauricle were measured, corresponding to the preoperative measurements of the contralateral ear. The actual reduction in vertical axis (V1–V2) and in horizontal axis (H1–H2) (in millimetres) was calculated. Patients were followed up for a period of three months. At the patient’s final visit, postoperative outcome was classified as either satisfactory or unsatisfactory, based on surgeon assessment and patient feedback regarding symmetry and shape of the neoauricle.
Figure 2).

Length of auricle defect mesurement
Figure 3).

Two helical flaps (one on either side of the injury) were created
RESULTS
Five patients were left with unsatisfactory results (27.77%). Three patients presented with a small neoauricle and two patients presented with a small and cupped auricle (Table 2) (Figure 4). The original defect size in these five patients was >2.8 cm, and there was significant postoperative reduction in the vertical axis, ranging from 6 mm to 8 mm, as shown in Table 3 (patients 7, 8, 10, 13 and 14). Additional cupping was present in patients 8 and 13. The reduction in vertical axis in the entire patient population ranged from 1 mm to 8 mm, with a mean of 3.55 mm. Reduction in the horizontal axis ranged from 0 mm to 2 mm, with a mean of 0.94 mm.
TABLE 2.
Complications with the reconstructive outcome in five patients
| Complication | Patients, n (%) |
|---|---|
| Size | 3 (16.66) |
| Size and shape | 2 (11.11) |
| Total | 5 (27.77) |
Figure 4).

Small neoauricle with cupping
TABLE 3.
Postoperative results according to original defect size, using a cut-off point of 2.8 cm
| Defect size |
Result*, n
|
H1–H2, mm | V1–V2, mm | |
|---|---|---|---|---|
| Satisfactory | Unsatisfactory | |||
| <2.8 mm† | 13 | 0 | 2 to 5 | 0 to 2 |
| >2.8 mm‡ | 5 | 5 | 6 to 7 | 1 to 2 |
Surgeon assessment and patient feedback;
Patients 1, 2, 3, 4, 5, 6, 9, 11, 12, 15, 16, 17 and 18;
Patients 7, 8, 10, 13 and 14. H1–H2 Difference in horizontal axis (preoperative horizontal measurement of contralateral ear – postoperative horizontal measurement of reconstructed ear); V1–V2 Difference in vertical axis (preoperative vertical measurement of contralateral ear – postoperative vertical measurement of reconstructed ear)
DISCUSSION
Although the helical advancement flap was originally designed to repair auricle defects confined to the helical rim, it is also useful in the repair of wedge defects, as well as defects in the upper and middle one-third of the auricle. These defects are confined to skin and cartilage, which can be replaced by the helical advancement flap (6,7).
There are two variations of this flap. In the first, the flap is detached from both the anterior and posterior surfaces of the helix. This design allows maximal mobility but can jeopardize flap viability (8). In the second variation, the posterior skin is left intact, resulting in a broader flap base with little or no risk to flap viability but limited mobility, as Antia and Buch originally described (4). Depending on the type of defect, the helical flap must be mobilized either unilaterally or bilaterally along the helical margin, and an extra length gained by V-Y advancement of the helical root in the upper flap (9). Following the repair of an auricular defect using the helical advancement technique, the resulting neoauricle is smaller than it was at baseline. This technique may be less effective in larger defects, but the true cut-off value has yet to be determined. A review of the literature revealed that helical advancement flaps can repair defects up to 4 cm in length (8). However, in the present study, an analysis of the results showed less favourable results when the original defect was >2.8 cm (χ2=4.24, P=0.04) (Table 4). Satisfactory surgical outcome of the neoauricle is judged on symmetry and shape preservation. In the present study, five patients were left with auricle asymmetry based on subjective observation by the surgeon and patient feedback. The defect size in these five cases was >2.8 cm and the final reduction in the vertical axis ranged from 6 mm to 8 mm. All patients in the present study showed a reduction in the horizontal axis of 0 mm to 2 mm (Table 3). Two studies support these results: Orticochea (10) has successfully performed the helical advancement technique in auricle defects up to 2.5 cm without resulting asymmetry. Another study by Calhoun et al (11) examined the procedure by creating 2 cm defects in cadavers and in reviewing 10 consecutive patients without subsequent asymmetry (11).
TABLE 4.
Analysis of results showing a significant difference in outcome according to the size of the original defect, using a cut point of 2.8 cm
| Group | >2.8 cm | ≤2.8 cm | Total |
|---|---|---|---|
| Satisfactory results | 0 | 13 | 13 |
| Unsatisfactory results | 5 | 0 | 5 |
| Total | 5 | 13 | 18 |
χ2=4.24, P=0.04
The management of auricle asymmetry is a controversial issue. Addressing the asymmetry by surgical reduction of the contralateral (normal) auricle is technically feasible, but contoversial; currently, most plastic surgeons are not in favour. Gault et al (12) have used the helical advancement technique as mean of reduction otoplasty in cases of congenital asymmetry. Benedict et al (13) used the same technique in treating cases of congenital macrotia. Further studies considering the social, cultural and psychological factors should be included to justify the application of this procedure to the normal auricle.
CONCLUSION
The three varieties of upper one-third auricle defects in the present article were best corrected by the helical advancement technique when the defect was <2.8 cm. A perioperative reduction in the vertical axis of the neoauricle of >5 mm was an important predictive factor in development of the subsequent deformity.
REFERENCES
- 1.Harris PA, Ladhani K, Das-Gupta R, Gault DT. Reconstruction of acquired sub-total ear defects with autologous costal cartilage. Br J Plast Surg. 1999;52:268–75. doi: 10.1054/bjps.1998.3053. [DOI] [PubMed] [Google Scholar]
- 2.Brunelli A, Bottini DJ, Cervelli V, Cervelli G, Grimaldi M. Reconstruction of partially amputated external ear with costal cartilage graft: Case report. Acta Otorhinolaryngol Ital. 2004;24:150–6. [PubMed] [Google Scholar]
- 3.Ramsey ML, Marks VJ, Klingensmith MR. The chondrocutaneous helical rim advancement flap of Antia and Buch. Dermatol Surg. 1995;21:970–4. doi: 10.1111/j.1524-4725.1995.tb00535.x. [DOI] [PubMed] [Google Scholar]
- 4.Antia NH, Buch VI. Chondrocutaneous advancement of flap for the marginal defect of the ear. Plast Reconstr Surg. 1967;39:472–7. doi: 10.1097/00006534-196705000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Soni A, Sheoran S, Rajput A. Helical reconstruction in a post human bite defect. Indian J Plast Surg. 2006;39:79–80. [Google Scholar]
- 6.Zenn MR. Helical advancement with a posterior auricular pull-through flap: A technique for reconstruction of combined helical and scaphal defects. Aesthetic Plast Surg. 1999;23:131–3. doi: 10.1007/s002669900255. [DOI] [PubMed] [Google Scholar]
- 7.Millard DR. The chondro-cutaneous flap in partial auricular repair. Plast Recon Surg. 1966;27:523. doi: 10.1097/00006534-196606000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Bialostocki A, Tan ST. Modified Antia-Buch repair for full-thickness upper pole auricle. Plast Reconstr Surg. 1999;103:1476–9. doi: 10.1097/00006534-199904050-00019. [DOI] [PubMed] [Google Scholar]
- 9.Brent BD. The acquired auricular deformity. A systematic approach to its analysis. Plast Reconstr Surg. 1977;59:575–85. [PubMed] [Google Scholar]
- 10.Orticochea M. Reconstruction of partial loss of the auricle. Plast Reconstr Surg. 1970;46:403–5. doi: 10.1097/00006534-197010000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Calhoun KH, Slaughter D, Kassir R, Seikaly H, Hokansonj A. Biomechanics of the helical rim advancement flap. Arch Otolaryngol Head Neck Surg. 1996;122:1119–23. doi: 10.1001/archotol.1996.01890220083014. [DOI] [PubMed] [Google Scholar]
- 12.Gault DT, Grippaudo FR, Tyler M. Ear reduction. Br J Plast Surg. 1995;48:30–4. doi: 10.1016/0007-1226(95)90027-6. [DOI] [PubMed] [Google Scholar]
- 13.Benedict M, Pirwitz KU. Plastic external ear reduction in bilateral macrotia. J Laryngol Otol. 2003;1176:487–9. doi: 10.1007/s106-002-8066-6. [DOI] [PubMed] [Google Scholar]


