Abstract
Background
No standard oral assessment tools are available for determining frequency of oral care in critical care patients, and the method of providing oral care is controversial.
Objectives
To examine the effects of a systematic program of oral care on oral assessment scores in critically ill intubated and nonintubated, patients.
Methods
Clinical data were collected 3 times during critical care admissions before and after institution of a systematic program of oral care in 3 different medical centers. The oral care education program consisted of instruction from a dentist or dental hygienist and a clear procedure outlining systematic oral care. The Beck Oral Assessment Scale and the mucosal-plaque score were used to assess the oral cavity. Data were analyzed by using linear mixed modeling with controls for severity of illness.
Results
Scores on the Beck Scale differed significantly (F = 4.79, P = .01) in the pattern of scores across the 3 days and between the control group (before oral education) and the systematic oral care group. Unlike the control group, the treatment group had decreasing scores on the Beck Scale from day 1 to day 5. The mucosal-plaque score and the Beck Scale scores had strong correlations throughout the study; the highest correlation was on day 5 (r = 0.798, P < .001, n = 43).
Conclusions
Oral assessment scores improved after nurses implemented a protocol for systematic oral care. Use of the Beck Scale and the mucosal-plaque score could standardize oral assessment and guide nurses in providing oral interventions.
Oral care is a basic nursing care activity that provides relief and comfort to patients who are seriously ill and cannot perform this simple activity themselves. In a critical care unit, providing oral care to patients who are uncooperative, have a high risk for aspiration, or are intubated can be a challenge and, at times, an impossible task. However, if the benefit of oral care outweighs the risk, clear, precise oral care procedures and adequate evidence to support these processes are needed. If providing systematic oral care can decrease the incidence of pneumonia and other outcome measures, the care should be considered an important and critical component of critical care nursing. Except for investigations1–3 in cardiac surgery patients, few studies4,5 have demonstrated these benefits from oral care. Studies of specific oral care practices, such as oral decontamination and toothbrushing, including use of powered toothbrushes, have not resulted in improvements in duration of mechanical ventilation, length of hospital stay, or mortality.6,7 A recent randomized clinical trial8 in critical care patients receiving mechanical ventilation indicated that powered toothbrushes reduced plaque burden, but other outcome measures, such as ventilator-associated pneumonia (VAP), were not included in the trial.
In addition to the lack of outcome data to support oral care, no standard oral assessment tools for determining the frequency and procedure for oral care are available. Treloar and Stechmiller9 developed an oral assessment tool and tested it on 16 intubated patients. However, no information on psychometric testing was provided, and the oral assessment lacked quantitative metrics or scales. Fitch et al10 used a 100-mm visual analog scale to assess the different structures in the oral cavity. In this 3-phase, longitudinal study,10 30 patients were treated according to a specific oral care protocol that included brushing with a child's toothbrush. Although the oral care was performed by the nursing staff in less than 5 minutes, no specific information was provided on the time required to perform the oral assessment. The results indicated a significant difference in the mean inflammation score between the oral care group and the comparison group, but no other variable differed between the 2 groups. Finally, Fourrier et al11 used a plaque index score12 and a dental assessment by an odontologist to assess 228 intubated patients in a double-blind, placebo-controlled trial of chlorhexidine gel for prevention of respiratory infections. Although the number of plaque cultures positive for pathogens was decreased in the intervention group by day 10, the rate of VAP, days of mechanical ventilation, and other outcome measures did not differ between the 2 groups. In a recent single-center study, Munro et al13 examined the effect of toothbrushing alone, chlorhexidine alone, and toothbrushing plus chlorhexidine in reducing the rate of VAP. The decayed, missing, and filled teeth index was used as a baseline assessment of general oral health. In a subgroup analysis of patients who did not have elevated pneumonia scores at baseline and received chlorhexidine, pneumonia rates on day 3 were reduced.
No standard oral assessment tools to determine oral care frequency and procedure are available.
Another area of research is health care practitioners' oral care practices, in particular the practices of nurses and respiratory therapists. Although nurses think oral care is important, many use inadequate instruments such as foam sponges to perform oral care.14 In addition, nurses acknowledge that oral care procedures are not evidence based.15–17
Many performance improvement studies of VAP and oral care have been published. Some of the investigators18,19 found significant decreases in VAP rates after instituting numerous interventions including oral care. However, in these studies, oral care frequency and type were not clearly defined or consisted solely of chlorhexidine rinses.18,20 None of the studies included any oral assessment measure to determine the effects of oral care.
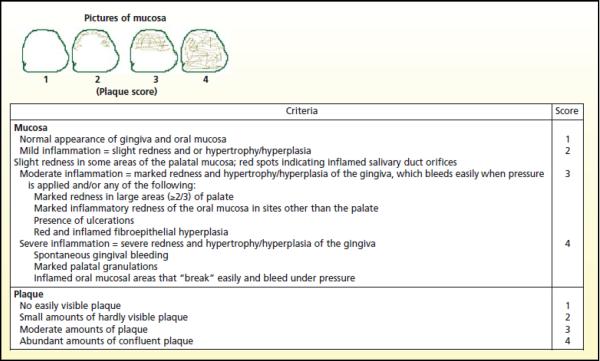
Recently, having critical care nurses provide oral care has received increased emphasis. National organizations21,22 have listed oral care in a number of prevention interventions. Providing evidence-based oral care requires data to support the intervention. Reliable and valid measures for oral assessment are essential to measure progress and guide intervention. In our study, we used a modified Beck Oral Assessment Scale (BOAS)23 and the mucosal-plaque score (MPS)24,25 to assess the oral cavity (Table 1 and Figure 1).
Table 1.
Beck Oral Assessment Score (BOAS), modifieda
| Score |
||||
|---|---|---|---|---|
| Area | 1 | 2 | 3 | 4 |
| Lips | Smooth, pink, moist, and intact | Slightly dry, red | Dry, swollen isolated blisters | Edematous, inflamed blisters |
|
| ||||
| Gingiva and oral mucosa | Smooth, pink, moist, and intact | Pale, dry, isolated lesions | Swollen red | Very dry and edematous, inflamed |
|
| ||||
| Tongue | Smooth, pink, moist, and intact | Dry, prominent papillae | Dry, swollen, tip and papillae are red with lesions | Very dry, edematous, engorged coating |
|
| ||||
| Teeth | Clean no debris | Minimal debris | Moderate debris | Covered with debris |
|
| ||||
| Saliva | Thin, watery plentiful | Increase in amount | Scanty and somewhat thicker | Thick and ropy, viscid or mucid |
|
| ||||
| Total Scoreb | 5 No dysfunction |
6–10 Mild dysfunction |
11–15 Moderate dysfunction |
16–20 Severe dysfunction |
| Note: Provide moisture more often than oral care | Minimum care every 12 h | Minimum care every 8–12 | Minimum care every 8 h | Minimum care every 4 h |
Modified from Beck.23
- BOAS 0–5 Perform an oral assessment once a day. Follow oral care as outlined in the systematic oral care procedure twice per day.
- BOAS 6–10 Perform oral assessments twice a day. Moisten mouth/lips every 4 hours. Follow oral care as outlined in the systemetic oral care procedure twice per day.
- BOAS 11–15 Perform an oral assessment every shift (every 8–12 h). Follow oral care as outlined in the systematic oral care every shift. Use an ultrasoft toothbrush. Moisten lips and mouth every 2h.
- BOAS 16–20 Perform an oral assessment every 4 hours. Follow oral care as outlined. If brushing not possible use soft gauze-wrapped finger. Moisten lips and mouth every 1 – 2 hours.
Figure 1.
Mucosal-Plaque Score (MPS).a
The purpose of our study was to examine the effects of a systematic oral care program in improving oral assessment scores in critically ill patients in 3 intensive care units.
Methods
This multicenter study was conducted between November 2004 and January 2007. The study was initially approved through the intramural institutional review board of the National Institute of Dental and Craniofacial Research, and then approval was obtained from the institutional review boards of the other participating institutions. Patients were recruited from 4 different critical care units in Virginia, the District of Columbia, and Maryland. Informed consent was obtained from each patient or the patient's legally authorized representative before collection of data or specimens. All eligible patients were asked to provide consent.
A convenience sample and a pre-post study design with an educational intervention were used. Each critical care unit served as its own control when patients received standard unit-based oral care before the educational intervention. After the intervention, each critical care unit instituted systematic oral care. From November 2004 until October 2005, patients received standard care, and then the educational intervention was implemented. The systematic oral care period began in December 2005 and continued until the end of the study in January 2007.
All patients were assessed, and specimens of plaque and saliva were collected. Microbiological analysis is not reported here. Data were collected within 48 hours of admission to a critical care unit (day 1), 48 hours from initial specimen (day 3), and 96 hours after initial specimen (day 5).
Patients were excluded if their expected length of critical care stay was less than 48 hours; they were less than 18 years old; they had significant oral, facial trauma; or they were edentulous. Patients were also excluded if they could provide their own oral care. In addition, patients were excluded if they had a clinical diagnosis of pneumonia at the time of admission and/or a modified Clinical Pulmonary Infection Score (CPIS)26 of 6 or greater. Patients were excluded if their length of stay was less than 48 hours because these patients' oral environments would not be affected by the systematic oral care. Children were excluded because of a lack of this population in the critical care units that were recruited for the study. Patients with oral or facial trauma and patients who were edentulous were excluded because of the risk of oral care in the former and the significantly different oral environment in the latter. If patients could provide their own oral care, the type of oral care they would receive was different. Patients with pneumonia or a CPIS of 6 or greater were excluded because of the lack of benefit and possible risk of the systematic oral care provided. If a patient was transferred from the critical care unit, no further data were collected, and study participation ended on transfer out of the unit.
Demographic data, diagnosis, medications, and results of oral assessment measures, including the MPS value and the BOAS score, were recorded. The BOAS used for this study was simplified from the original developed by Susan Beck.23 Table 1 includes the interpretation of the timing of oral care based on the score. This interpretation was not part of the original assessment score and was developed for this study.
The Acute Physiology and Chronic Health Evaluation (APACHE) II was used to compare severity of illness between hospitals and patients. The APACHE II was developed by Knaus et al27 as a modified version of the APACHE scoring system. For the APACHE II, physiological parameters are measured at the time of admission to a critical care unit. APACHE II scores have also been used to prognostically stratify acutely ill patients by predicted risk of hospital mortality.28 Results of other studies29,30 support the use of the APACHE II score in defined groups of patients as a measure of disease severity and as a predictor of mortality, but findings suggest that measuring these outcomes in individual patients is neither possible nor justified.
A modified CPIS (Table 2), which did not include microbiological results, was obtained each day of data collection.26 The CPIS was also used to exclude patients who had pneumonia at the time of admission to the critical care unit.
Table 2.
Clinical Pulmonary Infection Scorea
| Variable | Value | Score |
|---|---|---|
| Body temperature, °C | 36.5 – 38.4 | 0 |
| 38.5 – 39.0 | 1 | |
| >39.0 | 2 | |
|
| ||
| White blood cell count, × 1000/μL | 4–11 | 0 |
| 11 – 17 | 1 | |
| >17 | 2 | |
|
| ||
| Secretions | − | 0 |
| + | 1 | |
| ++ | 2 | |
|
| ||
| PaO2/fraction of inspired oxygen | >200 | 0 |
| <200 | 2 | |
|
| ||
| Infiltrates on chest radiograph | Clear | 0 |
| Patchy | 1 | |
| Localized | 2 | |
|
| ||
| Score ≥6 = pneumonia | ||
Data from Fartoukh et al.26
An evidence-based oral care procedure for critically ill patients must include reliable and valid measures to assess oral health. No single oral assessment scale has been identified that is appropriate in all clinical settings. The original BOAS,23 developed to assess the oral cavity of oncology patients with stomatitis, has 7 subscales that include voice quality and ability to swallow. The modified BOAS consists of 5 subscales: assessment of lips, mucosa and gingiva, tongue, teeth, and saliva. A higher score reflects dysfunction or tissue injury. BOAS scores range from 5 (no oral dysfunction) to 20 (severe dysfunction). A score greater than 5 is abnormal. The MPS includes only 2 scores that reflect an assessment of mucosal surfaces and plaque.25 MPS values range from 2 to 8; any score greater than 5 reflects marked lack of oral integrity. This MPS has been used in studies of elderly persons in nursing homes to assess oral hygiene but has not been used in critical care patients.24 Neither oral assessment scale has published reliability studies.
Nurses gently brushed the endotracheal tube with the toothbrush or used gauze to remove debris.
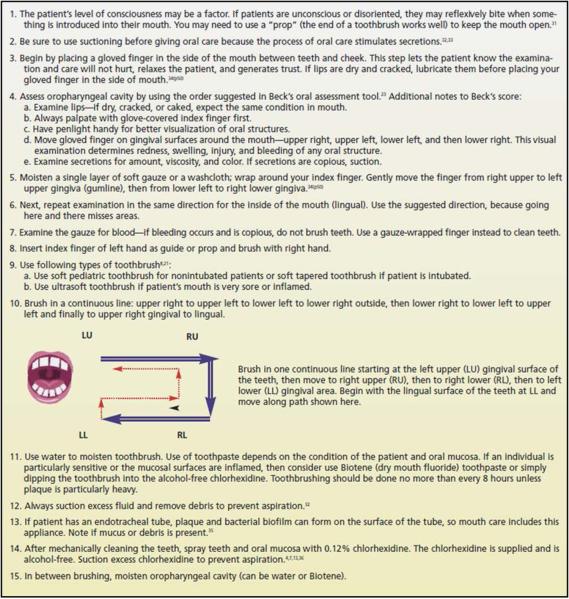
The study was designed with a baseline or control period in which each nurse in the critical care units provided standard, unit-based oral care. No common or standard oral care across the 3 units was used. Rather, standard oral care was the oral care that each unit delivered before the educational intervention. No attempts were made to vary the oral care provided in each critical care unit during the control period. After the educational intervention, a systematic oral care procedure (Figure 2) was introduced in all critical care units. Briefly, patients were assessed at the time of admission to the critical care unit and whenever a change in caregiver occurred. The frequency of oral care was determined by the BOAS score but was at least every 12 hours. Nurses were instructed to assess the level of consciousness and use suctioning before providing oral care. An oral examination was performed, and the data required in the BOAS and MPS were obtained. After assessment for bleeding, toothbrushing was performed in a systematic way to prevent missing any areas. If an endotracheal tube was present, the tube was included in the oral care. Nurses were instructed to brush it gently with the toothbrush or use gauze to remove any debris. After oral care, alcohol-free 0.12% chlorhexidine (supplied by Clinical Center Pharmacy Department, National Institutes of Health), delivered as a spray, was applied to teeth and mucosa. Excess chlorhexidine and secretions were suctioned. Between toothbrushings, the oral cavity was moistened with mouthwash (Biotene; GlaxoSmithKline Inc, Research Triangle Park, North Carolina) or water.
Figure 2.
Protocol for systematic oral care in the intensive care unit.
The study had no restriction on using tap water either to moisten and rinse the toothbrushes or to moisten the toothettes. In 2 reviews37,38 and a recent study,39 it has been noted that potentially pathogenic bacteria are present in the water supply of health care facilities. Berry et al40 recognized that tap water can be a source of nosocomial infections and stated that tap water should not be used as a mouth rinse for critically ill patients but left unresolved the use of sterile water as a substitute. Tap water is used in many critical care units when providing oral care.
Frequency of oral care was based on the results of the oral assessment. An index card was provided in the oral care kit delivered during the treatment phase for each patient. Nurses providing oral care were instructed to record the frequency of oral care and their initials on the card. The card was collected by the research nurse.
The structured educational program was multifaceted. After initial introduction by the researcher, a dentist or dental hygienist provided each patient care unit with instructions on the oral care procedure. The educational program was repeated several times according to each unit′s needs and the current staff. After the initial instruction, the oral care procedure was available as a recorded educational program on a DVD player provided to each critical care unit for the nursing staff. A colored pocket flip chart–booklet developed by the principal investigator (J.Y.) contained information and pictures describing the oral cavity and the BOAS. A copy of the booklet was placed in each patient's oral care kit. The oral care kit contained the chlorhexidine spray, a child′s toothbrush, an instruction booklet, and an oral care documentation card.
Sample Size and Statistical Analysis
The sample size for the study was based on a pilot study41 of 22 patients conducted at the Clinical Center of the National Institutes of Health in 2001. The change in the BOAS score was the main clinical outcome for both the pilot study and the study reported here. It was estimated that to detect a change in the BOAS score between the control group and the treatment group (mean score change of 2.05; SD, 2.26), a sample size of approximately 340 patients would be required based on 80% power and a 0.05 level of significance. Descriptive statistics were used to characterize the BOAS scores and the MPS values. A χ2 test and 1-way analysis of variance were used to determine differences among sites and between the treatment and control groups. Both a general linear model and linear mixed modeling were used to determine the effects of the program of systematic oral care on the BOAS scores and the MPS values.
Results
A total of 4 critical care units in 4 hospitals in the Washington, DC, area participated in the study. All 4 hospitals were trauma centers with more than 200 beds. A total of 152 patients provided informed consented for the protocol; 116 patients were included in the data analysis (Table 3). Of the 36 patients excluded from the analysis, 12 at hospital 1 received only toothbrushing without the chlorhexidine treatment; 15 were from hospital 2, which withdrew from the study with no treatment group obtained; and 12 at hospital 3 could not be reached to provide consent again after a delay in protocol renewal for that site.
Table 3.
Characteristics by sample site (n=116)
| Variablesa | Site | Statisticsb | ||
|---|---|---|---|---|
| Hospital 1 | Hospital 3 | Hospital 4 | ||
|
|
||||
| Group | χ2 = 19.5, p<.001 | |||
| Treatment | 7 (24) | 35 (76) | 23 (56) | |
| Control | 22 (76) | 11 (24) | 18 (44) | |
|
| ||||
| Ethnicity | χ2 = 45.0, P<.001 | |||
| White | 19 (66) | 13 (28) | 34 (83) | |
| African American | 5 (17) | 28 (61) | 1 (2) | |
| Other | 5 (17) | 5 (11) | 6 (15) | |
|
| ||||
| Sex | χ2 = 2.4, P>.30 | |||
| Male | 13 (45) | 26 (57) | 26 (63) | |
| Female | 16 (55) | 20 (43) | 15 (37) | |
|
| ||||
| Antibiotic usec | χ2 = 5.1, P<.O8 | |||
| No | 4 (14) | 10 (22) | 15(37) | |
| Yes | 25 (86) | 36 (78) | 26 (63) | |
|
| ||||
| Mechanical ventilationd | χ2 = 21.4, P<.001 | |||
| No | 6 (21) | 8 (17) | 25 (61) | |
| Yes | 23 (79) | 38 (83) | 16 (39) | |
|
| ||||
| Age, mean (SD),y | 62.5 (15.03) | 62.7 (20.79) | 72.6 (17.56) | F2,113 = 3.86, P<.02 |
|
| ||||
| APACHE II score, mean (SD) | 15.6 (7.13) | 19.5 (7.24) | 16.0 (4.96) | F2,113 = 4.30, P<.016 |
|
| ||||
| CPIS on day 1, mean (SD) | 2.8 (1.48) | 2.9 (1.66) | 2.4 (1.80) | F2,113 = 1.29, P<.28 |
|
| ||||
| BOAS score on day 1, mean (SD) | 10.9 (3.24) | 9.6 (2.37) | 10.3 (2.99) | F2,113 = 1.90, P<.15 |
|
| ||||
| MPS value on day 1, mean (SD) | 4.1 (1.27) | 3.8 (1.4) | 4.1 (1.29) | F2,113 = 0.70, P<.50 |
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; BOAS, Beck Oral Assessment Scale; CPIS, Clinical Pulmonary Infection Score; MPS, mucosal-plaque score.
Values for the 3 hospitals are number (%) of patients unless otherwise indicated. Because of rounding, not all percentages total 100.
F statistics are from a 1-way analysis of variance.
Patient received some antibiotics during hospital stay.
Patient was intubated and required mechanical ventilation at time of initial data collection.
Patients enrolled at the 3 sites differed significantly by hospital setting in age, ethnicity, treatment with mechanical ventilation, and APACHE II scores (Table 3). We found no difference by hospital setting when sex or administration of antibiotics was considered. In addition, the percentage of treatment and control group patients differed by site. Scores on day 1 (BOAS, MPS, and CPIS) did not differ significantly among hospitals, as indicated by analysis of variance.
When patients were compared by treatment group (Table 4), differences were not significant for sex (χ2 = 1.7; P = .20), use of antibiotics (χ2 = 0.6; P = .45), requiring mechanical ventilation (χ2 = 0.1; P = .73), or age (t = 1.08; P = .28). Treatment and control groups, however, did differ significantly for APACHE II scores (t = 2.19; P = .03), and the BOAS score on day 1 (t=2.53; P=.01). The treatment group had a higher mean APACHE II score than the control group (18.5 vs 15.8) and a lower mean BOAS score on day 1 (9.6 vs 10.9). On day 1, the mean BOAS score for all patients was 10.2 (SD, 2.99), and the MPS value for all patients was 3.9 (SD, 1.37); the differences between the groups were not significant. The MPS values and the BOAS scores had strong correlations; the highest correlation was on day 5 (r = 0.798; P < .001; n = 43). Correlations on day 1 (r = 0.727; P < .001; n = 116) and day 3 (r = 0.663; P < .001; n = 101) were also significant.
Table 4.
Characteristics of sample by group
| Characteristica | Control Group (n = 51) | Treatment Group (n = 65) | Overall (n = 116) |
|---|---|---|---|
|
| |||
| Ethnicity | |||
| White | 29 (57) | 37 (57) | 66 (56.9) |
| African American | 13 (25) | 21 (32) | 34 (29.3%) |
| Other | 9 (18) | 7 (11) | 16 (13.8%) |
|
| |||
| sex | |||
| Male | 32 (63) | 33 (51) | 65 (56.0) |
| Female | 19 (37) | 32 (49) | 51 (44.0) |
|
| |||
| Antibiotic useb | |||
| No | 11 (22) | 18 (28) | 29 (25.0) |
| Yes | 40 (78) | 47 (72) | 87 (75.0) |
|
| |||
| Mechanical ventilationc | |||
| No | 18 (35) | 21 (32) | 39 (33.6) |
| Yes | 33 (65) | 44 (68) | 77 (66.4) |
|
| |||
| Age, mean (SD), y | 64.0 (15.84) | 67.8 (20.8) | 66.2 (18.82) |
|
| |||
| APACHE II score, mean (SD) | 15.8 (5.83) | 18.5 (7.09) | 17.3 (6.68) |
|
| |||
| BOAS score on day 1, mean (SD) | 10.9 (2.77) | 9.6 (2.79) | 10.2 (2.99) |
|
| |||
| MPS value on day 1 mean (SD) | 4.2 (1.25) | 3.8 (1.38) | 4.0 (1.33) |
Abbreviations: APACHE, Acute Physiology and Chronic Health Evaluation; BOAS, Beck Oral Assessment Scale; MPS, mucosal-plaque score.
Values are number (%) of patients unless otherwise indicated.
Patient received some antibiotics during their stay.
Patient was intubated and required mechanical ventilation at time of initial data collection.
Analysis with a general linear model was performed with the BOAS score as the primary outcome. Sample size was reduced to 45 (26 control and 19 treatment) because of the requirement that all patients have data for all 3 days of data collection. Results indicated a significant difference among the 3 times (F = 4.80; P = .01) with no difference in the pattern of scores between treatment and control groups and time (interaction F = 1.57; P = .21). Means for the treatment group on days 1, 3, and 5 were 9.7 (SD, 3.68), 9.8 (SD, 2.48), and 8.1 (SD, 2.80), respectively. Means for the control group were 11.5 (SD, 2.44), 12.6 (SD, 3.50), and 11.5 (SD, 31.4). In addition, the 2 groups differed overall (F = 12.75; P = .001); the control group had a higher mean than the treatment group did.
Mixed linear modeling was used to analyze the BOAS scores and MPS values across time. In mixed linear modeling, patterns are used to predict or model missing data.42 In this method, in contrast to general linear modeling, no assumption is made that all time points must have data present. The pattern of BOAS scores differed significantly across the 5 days depending on the group (interaction F = 4.19; P = .02). The difference in BOAS scores was also significant over time, day 1, 3, or 5 (F = 5.1; P = .009), and between groups, treatment or control, (F=29.05; P < .001). In the control group, the estimated marginal means of the BOAS scores increased slightly from day 1 to day 3 (10.9 to 11.9) and then decreased slightly from day 3 to day 5 (11.9 to 11.0). In contrast, the treatment group had a slight decrease from day 1 to day 3 (9.5 to 9.2) and then a more pronounced decrease from day 3 to day 5 (9.2 to 7.7). BOAS scores differed overall between the 2 groups; the control group had a higher mean score (Table 5). The MPS values followed a similar pattern with a significant difference in the patterns of scores across the 5 days depending on the group (interaction F = 4.56; P=.01). The MPS values were also significantly different across time, day 1, 3, or 5, (F=7.33; P<.001) and by group, treatment or control (F = 16.83; P < .001).
Table 5.
Estimated marginal means (standard error) for scores on Beck Oral Assessment Scale and scores on mucosal-plaque score for groups across time (n = 116)
| Group | Day 1 | Day 3 | Day 5 | Overall |
|---|---|---|---|---|
| Beck Oral Assessment Scale |
||||
| Control | 10.9 (0.39) | 11.9 (0.38) | 11.0 (0.51) | 11.3 (0.33) |
| Treatment | 9.5 (0.35) | 9.1 (0.36) | 7.7 (0.58) | 8.8 (0.32) |
| Overall | 10.2 (0.26) | 10.5 (0.26) | 9.4 (0.38) | |
| Mucosal-Plaque Score |
||||
| Control | 4.1 (0.19) | 4.3 (0.16) | 4.0 (0.25) | 4.2 (0.16) |
| Treatment | 3.8 (0.16) | 3.3 (0.16) | 2.6 (0.28) | 3.3 (0.15) |
| Overall | 4.0 (0.12) | 3.8 (0.11) | 3.2 (0.19) | |
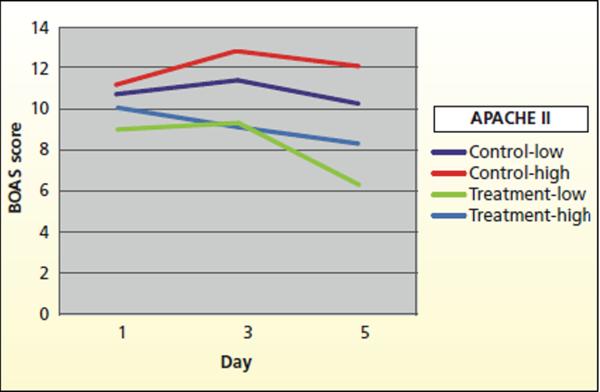
Because APACHE II scores differed between the treatment and control groups (Table 4), APACHE II groups were formed by using a median split. This step resulted in 32 control patients and 28 treatment patients in the low APACHE II group (APACHE II scores 2–17) and 19 and 37 patients, respectively, in the high APACHE II group (APACHE II scores ≥ 18). When the APACHE group was included in the mixed modeling as a control factor, results indicated that although scores changed across time, the pattern of scores differed between the treatment and the control groups (interaction F = 4.79; P = .01; Table 6). BOAS scores differed significantly between the control group and the treatment groups (F = 34.10; P < .001) and by day (F = 6.47; P = .003). Examination of the estimated marginal means indicated that BOAS scores in the control group increased on day 5 (11.2) and did not return to day 1 (10.9) levels, whereas scores in the treatment group decreased from day 1 (9.5) to day 5 (7.4). This finding was also true for patients in the high APACHE group or patients who had an increased severity of illness score. Among patients who had APACHE II scores greater than 17, indicating the patients were more acutely ill on admission to the critical care unit than the patients with lower scores, the mean BOAS scores were higher in the control group than in the treatment group. In the control group with high APACHE II scores, the BOAS scores were higher across time when day 1 scores were compared with day 5 scores. In the treatment group, the BOAS scores decreased across time (Figure 3). The control patients with both high and low APACHE II scores had overall higher mean BOAS scores for the day than did the treatment patients with both high and low APACHE II scores.
Table 6.
Analysis of scores on Beck Oral Assessment Scale across time with APACHE II scores (low/high) controlled for by using linear mixed modelinga
| Degrees of freedom |
||||
|---|---|---|---|---|
| Source | Numerator | Denominator | F | P |
| APACHE II score | 1 | 105.44 | 5.44 | .02 |
| Low (2– 17) | ||||
| High (>18) | ||||
|
| ||||
| Group: treatment or control | 1 | 105.44 | 34.10 | <.001 |
|
| ||||
| Day: day 1, 3, 5 | 2 | 61.79 | 6.47 | .003 |
|
| ||||
| APACHE II × Day | 2 | 61.79 | 1.24 | .28 |
|
| ||||
| APACHE II × Group | 1 | 105.44 | 0.10 | .75 |
|
| ||||
| Day × Group | 2 | 61.79 | 4.79 | .01 |
|
| ||||
| APACHE II × Group × Day | 2 | 61.79 | 1.65 | .20 |
Abbreviation: APACHE, Acute Physiology and Chronic Health Evaluations.
Analysis assumed unstructured covariance matrix.
Figure 3.
Estimated marginal mean score on Beck Oral Assessment Scale (BOAS) vs scores on the Acute Physiology and Chronic Health Evaluation (APACHE) II by day. Control patients with high and low APACHE II scores have overall higher mean BOAS scores than do treatment patients with high and low APACHE II scores.
The index cards on which nurses recorded the times of providing oral care were used to assess the integrity of the intervention. A total of 52% of the treatment group (n = 65) had study cards completed. However, some of the cards had only a few notations.
Discussion
In this multicenter study of 116 critically ill patients, the BOAS scores were higher before the educational intervention, reflecting poor oral health for patients who received standard unit-based oral care rather than systematic oral care. Compared with patients who had standard unit-based oral care, patients who had systematic oral care had significantly lower BOAS scores overall. When critically ill patients with APACHE II scores of 18 or greater were compared, this effect of systematic oral care remained. Overall in the study, the APACHE II scores reflected a moderate level of severity of illness; the highest score was 35, in a patient in the treatment group. The majority (66.4%) of the patients in this study were intubated and receiving mechanical ventilation, but many of the patients were not intubated. The presence of nonintubated patients in the critical care unit reflects some other organ dysfunction and places this group at high risk for aspiration.
The modified BOAS provides a realistic and clinically useful assessment of oral integrity in critically ill patients. The 5 subscales, saliva, teeth, tongue, lips, and oral mucosa, encompass the uniqueness of the oral cavity. As reflected in the BOAS scores, the overall results show that systematic oral care can improve oral health in critically ill patients. With the MPS, a much more widely used measure, only the mucosa and the plaque on the teeth are assessed. However, even though BOAS scores are a broader representation of the oral cavity, both the BOAS and the MPS positively correlated across all times. Use of these 2 oral assessment scores can help standardize oral care by providing a mechanism to measure the effects of this important nursing intervention.
In the study by Munro et al,13 the oral care interventions, toothbrushing and chlorhexidine treatment, were performed by study personnel. This method is the optimum one to use to ensure the integrity of the intervention. In our study, the critical care nurses who cared for the patients delivered the oral care. Although it could be assumed that oral care was provided more often than was recorded on the intervention cards, we have no way to know how often. The study by Munro et al13 included only patients treated with mechanical ventilation, whereas our study included critically ill patients who were not intubated. Because of the lack of a secure airway, patients who are not intubated might be at greater risk for aspiration than are intubated patients. Another interesting finding of Munro et al is that the toothbrushing group had higher CPIS values than did the other groups in their study because the toothbrushing group received additional days of brushing. Munro et al stated that these high CPIS values could have been related to dislodgement of plaque biofilm organisms by toothbrushing and subsequent entry of the organisms into the lungs. Munro et al question the safety of toothbrushing in critically ill patients and note that the “optimal oral care practices … have not been tested.”13(p436)
In the study by Fitch et al,10 a complex assessment of oral care was used that included evaluation of 9 factors in the mouth: inflammation, bleeding, salivary flow, candidiasis, dental plaque, purulent material, calculus, stains, and caries. These factors were assessed by using a 100-point scale. Clearly, a limitation of this scale would be the time required to administer it. This characteristic alone would render this oral assessment measure less than useful in the clinical environment.
The major limitations of our study were the pre-post test design and the differences between the treatment and control groups, including diagnosis, severity of illness, and other factors. Despite these differences between the 2 groups, acuity, sex, and antibiotic use did not differ significantly. The length of time between the 2 parts of the study was also a limitation. A smaller than anticipated sample size, loss of study patients who were transferred from the critical care unit and had to provide informed consent again to be in the study, and loss of patients because 1 site did not wish to continue, were also limitations. Measuring the fidelity of the intervention in terms of the consistency of the nursing staff performing the systematic oral care was difficult. Despite the training and educational reminders, variations occurred in the oral care delivered. If the oral intervention cards were a true reflection of protocol compliance, then only 52% of the oral care procedures were performed. However, the BOAS scores still differed significantly between the systematic oral care group and the control group. In future studies, a more reliable method for recording systematic oral care should be implemented. For example, the care could be recorded in the patient's medical record.
Tap water is used in many critical care units for providing oral care. Researchers37–39 have noted that potentially pathogenic bacteria are present in the water supplies of health care facilities. Berry et al40 recognized that tap water can be a source of nosocomial infections and stated that tap water should not be used as a mouth rinse for critically ill patients, but they left unresolved the use of sterile water as a substitute. This issue requires further study.
Patients who had systematic oral care had significantly lower overall scores on the Beck Oral Assessment Scale.
The strength of our study is that we tested, in a clinical setting, 2 oral assessment measures, the BOAS and the MPS. These measures are easy to use and teach to critical care nurses. BOAS scores and MPS values reflect the condition of the oral cavity and can be used to guide oral care in criti cally ill patients. The BOAS scores and the MPS values improved after nurses implemented an intervention for systematic oral care. This improvement took place despite inconsistent adherence to this oral intervention. Future research should focus on testing the reliability and validity of these oral assessment measures. Oral care interventions must be tested for safety in high-risk critically ill patients before any recommendation can be made to follow the interventions in routine care.
ACKNOWLEDGMENTS
This research received support from the intramural program of the National Institute of Dental and Craniofacial Research and the Clinical Center Nursing and Patient Care Services of the National Institutes of Health. We thank the entire nursing staffs of the 4 critical care units that participated in this study.
Footnotes
FINANCIAL DISCLOSURES None reported.
REFERENCES
- 1.Segers P, Speekenbrink RG, Ubbink DT, van Ogtrop ML, de Mol BA. Prevention of nosocomial infection in cardiac surgery by decontamination of the nasopharynx and oropharynx with chlorhexidine gluconate: a randomized controlled trial. JAMA. 2006;296(20):2460–2466. doi: 10.1001/jama.296.20.2460. [DOI] [PubMed] [Google Scholar]
- 2.Houston S, Hougland P, Anderson JJ, LaRocco M, Kennedy V, Gentry LO. Effectiveness of 0.12% chlorhexidine gluconate oral rinse in reducing prevalence of nosocomial pneumonia in patients undergoing heart surgery. Am J Crit Care. 2002;11(6):567–570. [PubMed] [Google Scholar]
- 3.DeRiso AJ, Jr, Ladowski JS, Dillon TA, Justice JW, Peterson AC. Chlorhexidine gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest. 1996;109(6):1556–1561. doi: 10.1378/chest.109.6.1556. [DOI] [PubMed] [Google Scholar]
- 4.Koeman M, van der Ven AJ, Hak E, et al. Oral decontamination with chlorhexidine reduces the incidence of ventilator associated pneumonia. Am J Respir Crit Care Med. 2006;173(12):1348–1355. doi: 10.1164/rccm.200505-820OC. [DOI] [PubMed] [Google Scholar]
- 5.Mori H, Hirasawa H, Oda S, Shiga H, Matsuda K, Nakamura M. Oral care reduces incidence of ventilator-associated pneumonia in ICU populations. Intensive Care Med. 2006;32(2):230–236. doi: 10.1007/s00134-005-0014-4. [DOI] [PubMed] [Google Scholar]
- 6.Pobo A, Lisboa T, Rodriguez A, et al. RASPALL Study Investigators A randomized trial of dental brushing for preventing ventilator-associated pneumonia. Chest. 2009;136(2):433–439. doi: 10.1378/chest.09-0706. [DOI] [PubMed] [Google Scholar]
- 7.Chan EY, Ruest A, Meade MO, Cook DJ. Oral decontamination for prevention of pneumonia in mechanically ventilated adults: systematic review and meta analysis. BMJ. 2007;334(7599):889. doi: 10.1136/bmj.39136.528160.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Needleman IG, Hirsch NP, Leemans M, et al. Randomized controlled trial of toothbrushing to reduce ventilator-associated pneumonia pathogens and dental plaque in a critical care unit. J Clin Periodontol. 2011;38(3):246–252. doi: 10.1111/j.1600-051X.2010.01688.x. [DOI] [PubMed] [Google Scholar]
- 9.Treloar DM, Stechmiller JK. Use of a clinical assessment tool for orally intubated patients. Am J Crit Care. 1995;4(5):355–360. [PubMed] [Google Scholar]
- 10.Fitch JA, Munro CL, Glass CA, Pellegrini JM. Oral care in the adult intensive care unit. Am J Crit Care. 1999;8(5):314–318. [PubMed] [Google Scholar]
- 11.Fourrier F, Dubois D, Pronnier P, et al. PIRAD Study Group Effect of gingival and dental plaque antiseptic decontamination on nosocomial infections acquired in the intensive care unit: a double-blind placebo-controlled multicenter study. Crit Care Med. 2005;33(8):1728–1735. doi: 10.1097/01.ccm.0000171537.03493.b0. [DOI] [PubMed] [Google Scholar]
- 12.Klein H, Palmer CE, Knutson JW. Studies on dental caries, I: dental status and dental needs of elementary school children. Public Health Rep. 1938;53(10):751–765. [Google Scholar]
- 13.Munro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexidine, toothbrushing, and preventing ventilator associated pneumonia in critically ill adults. Am J Crit Care. 2009;18(5):428–437. doi: 10.4037/ajcc2009792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feider LL, Mitchell P, Bridges E. Oral care practices for orally intubated critically ill adults. Am J Crit Care. 2010;19(2):175–183. doi: 10.4037/ajcc2010816. [DOI] [PubMed] [Google Scholar]
- 15.Kjonegaard R, Fields W, King ML. Current practice in airway management: a descriptive evaluation. Am J Crit Care. 2010;19(2):168–173. doi: 10.4037/ajcc2009803. [DOI] [PubMed] [Google Scholar]
- 16.Binkley C, Furr LA, Carrico R, McCurren C. Survey of oral care practices in US intensive care units. Am J Infect Control. 2004;32(3):161–169. doi: 10.1016/j.ajic.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Rello J, Koulenti D, Blot S, et al. Oral care practices in intensive care units: a survey of 59 European ICUs. Intensive Care Med. 2007;33(6):1066–1070. doi: 10.1007/s00134-007-0605-3. [DOI] [PubMed] [Google Scholar]
- 18.Bouadma L, Mourvillier B, Deiler V, et al. A multifaceted program to prevent ventilator-associated pneumonia: impact on compliance with preventive measures. Crit Care Med. 2010;38(3):789–796. doi: 10.1097/CCM.0b013e3181ce21af. [DOI] [PubMed] [Google Scholar]
- 19.Hutchins K, Karras G, Erwin J, Sullivan KL. Ventilator-associated pneumonia and oral care: a successful quality improvement project. Am J Infect Control. 2009;37(7):590–597. doi: 10.1016/j.ajic.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 20.Rello J, Lode H, Cornaglia G, Masterton R. A European care bundle for prevention of ventilator associated pneumonia. Intensive Care Med. 2010;36(5):773–780. doi: 10.1007/s00134-010-1841-5. [DOI] [PubMed] [Google Scholar]
- 21.AACN practice alerts: oral care for patients at risk for ventilator associated pneumonia. [Accessed June 13, 2011];American Association of Critical-Care Nurses Web site. http://www.aacn.org/WD/Practice/Docs/PracticeAlerts/oral%20care%2004-2010%20final.pdf.
- 22.Bouza E, Burillo A. Advances in the prevention and management of ventilator-associated pneumonia. Curr Opin Infect Dis. 2009;22(4):345–351. doi: 10.1097/QCO.0b013e32832d8910. [DOI] [PubMed] [Google Scholar]
- 23.Beck S. Impact of a systematic oral care protocol on stomatitis after chemotherapy. Cancer Nurs. 1979;2(3):185–199. [PubMed] [Google Scholar]
- 24.Henriksen BM, Ambjornsen E, Axell TE. Evaluation of a mucosal-plaque index (MPS) designed to assess oral care in groups of elderly. Spec Care Dentist. 1999;19(4):154–157. doi: 10.1111/j.1754-4505.1999.tb01378.x. [DOI] [PubMed] [Google Scholar]
- 25.Silness P, Löe H. Periodontal disease in pregnancy, II: correlation between oral hygiene and periodontal condition. Acta Odentol Scand. 1964;22(1):121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 26.Fartoukh M, Maitre B, Honore S, Cerf C, Zahar JR, Brun Buisson C. Diagnosing pneumonia during mechanical ventilation: the Clinical Pulmonary Infection Score revisited. Am J Respir Crit Care Med. 2003;168(2):173–179. doi: 10.1164/rccm.200212-1449OC. [DOI] [PubMed] [Google Scholar]
- 27.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 28.Del Bufalo C, Morelli A, Bassein L, et al. Severity scores in respiratory intensive care: APACHE II predicted mortality better than SAPS II. Respir Care. 1995;40(10):1042–1047. [PubMed] [Google Scholar]
- 29.Moreno R, Apolone G, Miranda DR. Evaluation of the uniformity of fit of general outcome prediction models. Intensive Care Med. 1998;24(1):40–47. doi: 10.1007/s001340050513. [DOI] [PubMed] [Google Scholar]
- 30.Koperna T, Semmler D, Marian F. Risk stratification in emergency surgical patients: is the APACHE II score a reliable marker of physiological impairment? Arch Surg. 2001;136(1):55–59. doi: 10.1001/archsurg.136.1.55. [DOI] [PubMed] [Google Scholar]
- 31.Fields LB. Oral care intervention to reduce incidence of ventilator associated pneumonia in the neurologic intensive care unit. J Neurosci Nurs. 2008;40(5):291–298. doi: 10.1097/01376517-200810000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Chao YF, Chen YY, Wang KW, Lee RP, Tsai H. Removal of oral secretion prior to position change can reduce the incidence of ventilator-associated pneumonia for adult ICU patients: a clinical controlled trial study. J Clin Nurs. 2009;18(1):22–28. doi: 10.1111/j.1365-2702.2007.02193.x. [DOI] [PubMed] [Google Scholar]
- 33.Tsai HH, Lin FC, Chang SC. Intermittent suction of oral secretions before each positional change may reduce ventilator associated pneumonia: a pilot study. Am J Med Sci. 2008;336(5):397–401. doi: 10.1097/MAJ.0b013e31816b8761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Darby ML, Walsh M, editors. Dental Hygiene: Theory and Practice. 3rd ed. Saunders; St Louis, MO: 2010. [Google Scholar]
- 35.Perkins SD, Woeltje KF, Angenent LT. Endotracheal tube biofilm inoculation of oral flora and subsequent colonization of opportunistic pathogens. Int J Med Microbiol. 2010;300(7):503–511. doi: 10.1016/j.ijmm.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 36.Panchabhai TS, Dangayach NS, Krishnan A, Kothari VM, Karnad DR. Oropharyngeal cleansing with 0.2% chlorhexidine for prevention of nosocomial pneumonia in critically ill patients: an open label randomized trial with 0.01% potassium permanganate as control. Chest. 2009;135(5):1150–1156. doi: 10.1378/chest.08-1321. [DOI] [PubMed] [Google Scholar]
- 37.Anaissie EJ, Penzak SR, Dignani MC. The hospital water supply as a source of nosocomial infections: a plea for action. Arch Intern Med. 2002;162(13):1483–1492. doi: 10.1001/archinte.162.13.1483. [DOI] [PubMed] [Google Scholar]
- 38.Exner M, Kramer A, Lajoie L, Gebel J, Engelhart S, Hartemann P. Prevention and control of health care associated waterborne infections in health care facilities. Am J Infect Control. 2005;33(5 suppl 1):S26–S40. doi: 10.1016/j.ajic.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Wang JL, Chen ML, Lin YE, Chang SC, Chen YC. Association between contaminated faucets and colonization or infection by nonfermenting gram negative bacteria in intensive care units in Taiwan. J Clin Microbiol. 2009;47(10):3226–3230. doi: 10.1128/JCM.00034-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berry AM, Davidson PM, Masters J, Rolls K. Systematic literature review of oral hygiene practices for intensive care patients receiving mechanical ventilation. Am J Crit Care. 2007;16(6):552–562. [PubMed] [Google Scholar]
- 41.Yates J. The Role of a Meticulous Oral Hygiene Program in Reducing Oral Assessment Scores, Mucosal Plaque Scores, Colonization of Dental Plaque, and Exposition to Pathogen Colonization That May Lead to Nosocomial Infection [dissertation] George Mason University; Fairfax, VA: 2003. [Google Scholar]
- 42.SPSS Inc. Linear Mixed Effects Modeling in SPSS: An Introduction to the MIXED Procedure. SPSS Inc; Chicago, IL: 2005. [Google Scholar]