Abstract
Objective
To determine seniors’ beliefs about falls and design a fall-risk self-assessment and educational materials to promote early identification of evidence-based fall risks and encourage prevention behaviors.
Methods
Focus groups with community-dwelling seniors, conducted in two phases to identify perceptions about fall risks and risk reduction and to assess face validity of the fall-risk self-assessment and acceptability of educational materials.
Results
Lay perception of fall risks was in general concordance with evidence-based research. Maintaining independence and positive tone were perceived as key motivators for fall prevention. Seniors intended to use information in the educational tool to stimulate discussions about falls with health care providers.
Implications
An evidence-based, educational fall-risk self-assessment acceptable to older adults can build on existing lay knowledge about fall risks and perception that falls are a relevant problem and can educate seniors about their specific risks and how to minimize them.
Keywords: falls, qualitative research methods, preventive medicine, preventive care, preventive services
Despite over 30 years (Gillespie et al., 2003) of productive research, falls still have devastating consequences for older adults. More than one third of adults age 65 and older fall each year in the United States (Hausdorff, Rios, & Edelberg, 2001), and injurious falls are the leading cause of injury deaths among older adults (Centers for Disease Control and Prevention, 2006). Fall-related hip fractures account for approximately 25% of injury deaths among those over age 65, increasing to 34% among those age 85 or older (Peek-Asa & Zwerling, 2003). Direct annual medical costs associated with falls exceeded $19 billion in 2000 (Stevens, Corso, Finkelstein, & Miller, 2006).
Evidence-based clinical-practice guidelines (American Geriatrics Society, 2001; Wenger et al., 2007) recommend annual medical screening of older adults for falls and a thorough diagnostic assessment to identify modifiable risks (Tromp et al., 2001), including (in general order of relative risk) muscle weakness, recent fall history, gait and balance deficits, use of assistive devices, sensory deficits, impaired vision, medication, depression, and fear of falling (Rubenstein & Josephson, 2002). However, community physicians frequently do not follow these recommendations (Rubenstein et al., 2004; Wenger et al., 2009), and older adults may also fail to recognize their own risks (Braun, 1998).
Multifactorial health and human service interventions, including exercise programs that target balance and strength training, effectively mitigate fall risks (Chang et al., 2004; RAND Corporation, 2003), but successful implementation continues to be a challenge. Fall prevention heavily depends on individual behavior change, but older adults are often reluctant to adhere to fall-prevention regimens (Braun, 1998; Bunn, Dickinson, Barnett-Page, McInnes, & Horton, 2008; Yardley, Donovan-Hall, Francis, & Todd, 2006). In rare instances, a person’s risk of falling can be ameliorated solely by the actions of the physician (i.e., discontinuation of a medication causing dizziness or instability). Usually, older adults have multiple risk factors that can require both medical intervention (e.g., physical therapy, occupational therapy) and adoption of new behaviors (e.g., exercise).
Risk Perception and Behavior Change
Little is known about older adults’ perception of fall risk and what factors may motivate prevention activities. Yardley et al. (2006) found that the tone of fall-prevention messages was crucial to endorsement, but fall-prevention education typically was dismissed by seniors who perceived recommendations as condescending or overly directive. Awareness of individual risk is also an important facilitator of fall prevention, but many older adults may not acknowledge their own fall-risk levels. Previous research shows that although community-dwelling seniors may understand the importance of falls as a preventable health problem in general, they underestimate their own susceptibility to falls, confident that, even if they fell, they would be able to return to their current living situations (Braun, 1998). This general lack of awareness of fall risk has not been acknowledged as a self-risk that might motivate change in behavior.
Behavior-change theoretical models are an important consideration for fall-prevention campaigns. The extended parallel process model posits behavior change as the result of a two-step fear appraisal: perception of threat (seriousness and self-relevancy) and assessment of self-efficacy (Witte, 1992). The greater the perceived threat, the more motivated individuals will be to assess self-efficacy to complete the recommended action. However, if the recommended action is perceived as too difficult or burdensome, behavior change may not occur. The transtheoretical model, or stages of change model, suggests that interventions should also account for variations in one’s own readiness to change behavior (Prochaska & Velicer, 1997). The model outlines five stages of individual readiness to change: precontemplation (unaware of problem, not considering behavioral change), contemplation (considering behavioral change), preparation for action (taking steps to make behavior changes), action (actively changing behavior), and maintenance (sustaining behavior change). Interventions should be tailored to the specific stage of the audience. For example, individuals in the precontemplation stage would require an awareness campaign, those in the contemplation stage would require a motivational campaign, and those in the action phase would require concrete tools and resources.
Study Objectives
The purpose of this study was to develop a fall-risk self-assessment to address this important public health issue by educating people about their own fall risks. Although there are fall-risk-screening instruments, none have been successfully tested and validated in community settings. To fill this gap and enhance the likelihood of the instrument’s acceptability and usability, we sought input from older adults throughout the development process. Our objectives were to (a) determine older adults’ beliefs and attitudes about falls, including identifying the natural language used by older adults when talking about falls and the appropriate level of threat perception to motivate behavior change; (b) identify which significant fall-risk behaviors are the most, and which are the least, amenable to behavior modification; and (c) determine the acceptability of health-promotion/risk-reduction educational material in terms of amount and type of information provided, language, and imagery.
Methods
Participants
The sampling frame was constructed to represent the ethnically and economically diverse neighborhood populations in Los Angeles County (Zonta & Ong, n.d.). Senior and community centers were contacted via telephone and asked to participate as research sites. Three centers agreed to participate in Phase I and four centers agreed to participate in Phase II. Community-dwelling older adults were recruited from these centers in two separate study phases through posted fliers and newsletter announcements. In total, 45 older adults in Phase I and an additional 49 older adults in Phase II responded to recruitment efforts and were screened for eligibility; there was no overlap in participation between study phases. Participants were eligible if they were age 65 or older, were community dwelling, could understand and summarize the study purpose (to establish ability to self-consent for participation), were fluent in English, were able to hear well enough to participate in a group discussion, and were able to see well enough to read 14-point font. Reasons for nonparticipation included failure to meet eligibility criteria, scheduling conflicts, inability to be reached by study staff, and refusal to sign the consent document. The participants and the centers received a nominal honorarium for participation. The Institutional Review Board and Human Subjects Research and Development Committee of the VA Greater Los Angeles Healthcare System approved the project.
Design and Procedures
This prospective qualitative study was conducted with an iterative stepwise approach (Willis, 2005). We conducted seven focus-group interviews (one per research site) in two separate study phases with community-dwelling seniors to determine perceptions of fall risks, the perceived level of threat associated with falling, and acceptability of risk reduction. As we will describe, Phase I interviews focused on identifying community seniors’ existing knowledge and beliefs about falls. We subsequently incorporated these results into an evidenced-based fall-risk self-assessment with targeted educational material that was synthesized into a brochure format. Phase II interviews focused on community seniors’ perceptions of acceptability and perceived usability of the self-assessment brochure.
Each 60-min focus-group discussion was led by a trained moderator using discussion guides that were informed by the extended parallel process model framework to assess threat and motivation and by the transtheoretical model framework to gauge readiness to accept recommendations for behavior change. Constant comparative analysis was performed, and grounded theories generated from interviews were tested in subsequent focus groups. This application of grounded theory produced conceptually rich data to predict how a process, such as our educational intervention, would relate to theories of behavior change in this particular population (Miles & Huberman, 1994; Strauss & Corbin, 1994). Data collection in each phase terminated when data saturation or redundancy was established (Krueger & Casey, 2008).
Phase I: Knowledge and Beliefs
The semistructured, open-ended discussion guide was organized around four main study questions: How is fall risk recognized by older adults? How can falls be prevented and what preventive actions are most likely to be undertaken? What is the appropriate level of threat perception to motivate seniors to action? and, How should fall-prevention messages be communicated to older adults? These questions were derived by the study investigators with input from researchers at the Centers for Disease Control and Prevention.
In open-ended questions, participants were asked how they recognize that someone was at risk for falling. From this spontaneously generated list, they were asked how each of these risks might be prevented. Participants were then asked to identify the preventive strategies that were most difficult and easiest to adopt. Next, the moderator asked them to respond to a list of facts about fall-related outcomes that included cost, nursing home placement, injury, impaired function, and mortality. Finally, opinions on how and where to deliver information about fall-risk reduction were solicited.
The interviews were transcribed verbatim and coded for analysis using qualitative research software (QSR International Pty. Ltd., Melbourne, Australia). The study questions established the initial categories for the coding structure. The coding structure allowed a highly differentiated, fine-grain description of existing knowledge. New themes were allowed to emerge in our analysis, and the coding structure was amended to be conceptually inclusive. Coding was performed by one study author (R.V.) and independently reviewed by another (J.K.); discrepancies were discussed and resolved to achieve consensus.
Phase II: Fall-Risk Self-Assessment and Educational Intervention
The fall-risk self-assessment was designed to assess 10 validated fall-risk factors (Rubenstein & Josephson, 2002) and any additional lay recommendations identified in Phase I. These items were designed as a questionnaire with a binary response format. The relative risk of more serious factors such as leg weakness and balance deficiency (Peek-Asa & Zwerling, 2003; Tromp et al., 2001) was roughly weighted by including multiple items for that risk factor. Each focus-group participant independently completed the fall-risk self-assessment before a group discussion about each item. We tested two versions of the assessment: the self-assessment as a stand-alone screening instrument and a version that explained the specific risk posed by each item on the fall-risk self-assessment. The study team collated responses after each focus group and tested participants’ recommendations for improving the wording or language in subsequent groups, until no further problems were identified in focus groups and all elements received positive feedback.
The open-ended discussion guide was designed to examine four factors that would affect acceptance of the fall-risk brochure: Were the screening items clear, comprehensible, and acceptable? Were the fall-prevention recommendations perceived as feasible? Were the graphics and the brochure format appealing? and, How would this brochure be used in the community? At the beginning of each discussion, participants were asked to define the elements of a “good” health-education brochure and to later compare our brochure with these criteria. The appeal of graphic images was determined using card free-sorting to identify the top three images among participants in each group.
Results: Phase I. Knowledge and Beliefs
Forty-five older adults were screened for participation in Phase I, and of these, 26 (57.7%) were eligible. Seven eligible participants refused to participate or could not be reached. In total, 19 older adults representing three senior centers participated in three Phase I focus groups (Table 1). These centers were fairly reflective of Los Angeles’s diverse demography. Participants had a mean age of 73.7 years, and most were women (n = 16). We present Phase I results according to study question.
Table 1.
Characteristics of Study Participants for Phase I and Phase II
| Phase I | Phase II | |
|---|---|---|
| Screened | 45 | 49 |
| Eligible | 26 | 32 |
| Refused/Could not be reached | 7 | 13 |
| N | 19 | 19 |
| Number of focus groups | 3 | 4 |
| Mean (SD) age, years | 73.7 (8.6) | 74.1 (6.6) |
| % (n) male | 16% (3) | 5% (1) |
| Ethnicity—% (n) | ||
| Non-Hispanic White | 53% (10) | 26% (5) |
| African American | 32% (6) | 47% (9) |
| Asian | 0% (0) | 0% (0) |
| Hispanic | 5% (1) | 26% (5) |
| American Indian/Alaska native | 5% (1) | 0% (0) |
| other | 5% (1) | 0% (0) |
How Is Fall Risk Recognized by Older Adults?
Participants spontaneously identified several fall-risk factors (Table 2). They immediately described seniors at risk for falling as appearing “unsteady” or “wobbly” while walking. One focus group described individuals with balance deficiencies, stating, “They stumble … They can’t walk straight …. They’re swaying … not quite on balance.” Seniors also opined that individuals with balance impairment should use an assistive device, and all groups perceived that nonadherence to a prescribed assistive device could increase one’s chances of falling.
Table 2.
Fall Risk Factors and Risk-Reduction Strategies Identified by Phase I Focus Groups
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| Fall risk factors | |||
| muscle weakness | X | X | X |
| gait or balance deficiency | X | X | X |
| environmental hazards (home, community) | X | X | X |
| poor vision | X | X | X |
| medications | X | X | X |
| dizziness | X | X | X |
| nonadherence to prescribed assistive device | X | X | X |
| inattention | X | X | |
| reaching or climbing for high objects | X | X | |
| inappropriate footwear | X | X | |
| loss of sensation in feet | X | ||
| Fall-risk-reduction strategies | |||
| exercise | X | X | X |
| adherence to prescribed assistive device | X | X | X |
| home modifications/safety | X | X | X |
| concentration/paying attention | X | X | |
| supportive footwear | X | X | |
| talking to doctor about medications | X | X | |
| pay service (e.g., Lifeline) | X | ||
| routine eye examinations | X | ||
| proper gait (e.g., “Don’t shuffle”) | X | ||
| falls education in the community | X | ||
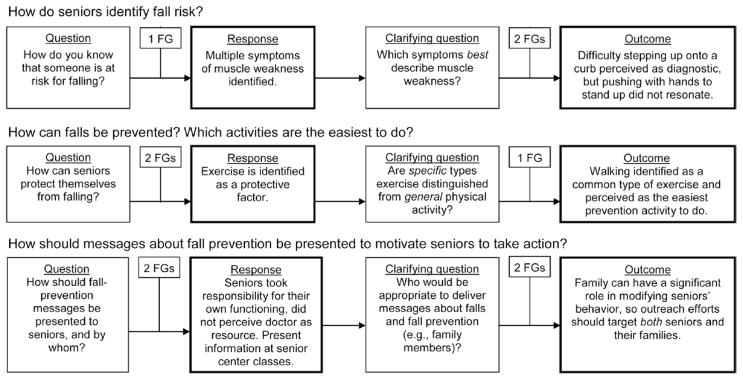
Difficulty stepping up onto a curb, climbing stairs, and getting up from a seated position on the floor were consistent descriptors for muscle weakness (Figure 1). Participants identified stepping up onto a street curb as a unique indicator of fall risk because curbs lack a handrail for leverage or support. This assertion resonated as a major risk in every focus group and was added to the evidence-based risk factors for Phase II. One participant described this differentiation, stating, “Well, the stairs usually will have a banister or a wall or railing or something, and the curb, you really have nothing. The curb is very difficult because you have nothing to hold on to.”
Figure 1.
Example of an iterative process of data collection in Phase I focus groups (FGs), indicating number of FGs contributing to each stage of outcome.
How Can Falls Be Prevented?
Participants spontaneously offered fall-prevention recommendations (Table 2) that ranged in relative difficulty to adopt. Seniors perceived exercise as the most readily acceptable fall-prevention strategy, often offering personal examples of successful participation in exercise programs and independent physical activity. Formal exercise programs were accessible at senior and community centers, and walking was perceived as the easiest physical activity (Figure 1). One participant discussed the importance of exercise that targets balance training, saying, “The movement is important, but [also] trying to exercise exactly what you need … to find the exercise that you need to get the balance that you want.” In addition to exercise, seniors in each focus group shared their own positive experiences with home modifications such as installation of grab bars in the shower and removal of hazardous throw rugs in their homes. Some seniors accessed specific agencies to help them with home safety. For example, a participant said,
I live in an apartment and I got an okay from them [to have] a handheld shower. [The agency will] give you a stool to sit in the shower if you want to. They give you the strips for the bottom of the tub and two bars—one bar to get in and one bar to get out.
Despite recognizing its importance for fall prevention, participants perceived using an assistive device as the most difficult fall-prevention activity for seniors to adopt. Participants attributed this difficulty to a social stigma associated with canes and walkers, particularly among older men. One participant shared a personal example:
There are a lot of people that, to them, [a cane] is a projection of age, but a cane is just to keep your balance. My dad never used a cane and he fell in the yard. There’s just something about using the cane or a walker that just turns them off.
In general, vanity and maintaining independence were identified as key factors that influenced engagement in fall-prevention strategies. Strategies that negatively affected seniors’ perceived sense of independence had less likelihood of endorsement.
What Is the Effective Level of Threat Perception?
Many participants were not aware of the prevalence and severity of fall-related outcomes among older adults. In reaction to fall-related death rates, a participant said, “I had no idea people died from a fall. I figure once in a blue moon someone fell and died, but [this] is a lot.” Seniors were asked whether this information would motivate them to change their behaviors and engage in fall-prevention strategies. Although these facts were admittedly surprising to participants, they were also perceived as overly negative. Information about morbidity and mortality was “too scary” because “it takes your independence away.” Reframing this information in a positive tone would be more effective in motivating behavior because “people would listen to it.”
One new major theme emerged from the discussions. The concept of independence cross-cut spontaneous responses to the study questions. Maintaining independence was perceived as the key motivational strategy to reduce fall risk. Loss of independence was a more complicated notion involving the perceived stigma associated with aging, restriction of activity, and placement in a nursing home. Other beliefs, as well as knowledge, directly addressed the study questions.
How Should Fall-Prevention Messages Be Delivered to Promote Behavior Change?
Seniors generally felt responsible for managing their own health but were dissatisfied that doctors did not routinely address fall prevention during clinical visits. When asked if a doctor is the key person to motivate fall-prevention behavior, a participant answered, “Heavens, no. You are not his responsibility; you are your own responsibility.” Participants said that information on fall prevention would be well received when presented at a senior center class or in an educational pamphlet made available at doctors’ offices and community centers. Senior centers were perceived as a focal point for disseminating information because of the high volume of older adults who attend these centers and the informal social networks that exist there. “Word of mouth” was a key strategy for exchanging information among friends, relatives, and the community.
Results: Phase II. Fall-Risk Self-Assessment and Educational Intervention
Forty-nine older adults were screened for participation in Phase I, and of these, 32 (65.3%) were eligible. Thirteen eligible participants refused to participate or could not be reached. In total, 19 older adults representing four senior centers participated in four Phase II focus groups (Table 1). A greater proportion of ethnic minorities participated in Phase II, whereas age and gender proportions were comparable to those of Phase I.
Fall-Risk Self-Assessment
Although each of the fall-risk self-assessment’s 13 items (Table 3) resonated as a general and familiar experience, the lack of frequency qualifiers (e.g., sometimes, always, never) at the beginning of a question produced false positive and false negative responses. Participants found these items difficult to answer because the forced yes/no response did not allow for such dynamic concepts as occasionally treading on slippery surfaces. Seniors distinguished necessity from habit in the assessment items by adding need to before certain actions (e.g., “I need to use hands to push up from a chair” vs. “I use my hands to push up from a chair”). Seniors also distinguished habitual fear from situational fear about falls by changing verb tense (e.g., “I am worried about falling” vs. “I worry about falling”). The item that assessed difficulty in stepping up onto a curb continued to be well received and was considered unambiguous. Participants strongly preferred that facts explaining the fall risk accompany each screening item. This additional information helped clarify each item’s intent and provided insight into the meaning of a positive response.
Table 3.
Fall-Risk Self-Assessment Screener Examined in Phase II Focus Groups
| Check your risk for falling | Facts about falls |
|---|---|
| I have fallen in the last 6 months. | People who have already fallen are likely to fall again. |
| I worry about falling. | People who worry about falling are at risk for a serious fall. |
| When walking, I sometimes feel unsteady. When walking at home, I hold on to furniture to steady myself. |
Unsteadiness and needing support while walking are signs of poor balance. |
| I use or have been advised to use a cane or walker to get around safely. | Canes or walkers can reduce the chance of falling, but only when used correctly. |
| When standing up from a chair, I use my hands to help push myself up. I have some trouble stepping up onto a curb. |
These are signs of leg-muscle weakness—a major reason for falling. |
| I often have to rush to the toilet. | Rushing to the bathroom, especially at night, increases your risk of falling. |
| I have lost some feeling in my feet. | Numbness in the feet can cause stumbles and falls. |
| I take medicine that sometimes makes me feel light-headed or more tired than usual. I take medicine to help me sleep or improve my mood. |
Medication side effects can sometimes increase the risk of falls and fall-related injuries. |
| I often feel sad or depressed. | Symptoms of depression, such as not feeling well or feeling slowed down, are associated with falls. |
| Because I don’t see well, I have difficulty avoiding hazards in my path, such as tree roots or electrical cords. | Poor vision is linked to falls and injuries. |
Educational Intervention
In the educational section of the brochure, four key recommendations for fall prevention were listed: improving strength and balance through exercise, making specific home modifications, having annual eye examinations, and talking to a doctor about falls. Many participants said that this section of the brochure could serve as a guide for discussions with their health care providers about fall-prevention strategies. The brochure was perceived as a way to focus doctors on issues of concern that may not be receiving attention or that seniors may have trouble articulating.
Overall Appeal and Imagery
Each group independently specified similar criteria for health-information brochures: attractiveness, relevance to older adults, relevance to health concerns, informativeness, and inclusion of information that could be shared with members of the community. All groups agreed that, overall, the fall-risk self-assessment brochure met these criteria. The brochure was considered particularly strong in presenting new information (e.g., history of falling predicts future falls) that could be shared with others. Participants continued to point out that the dissemination route of health education in this population included informal networks of family and friends who share information with each other.
Participants continued to emphasize that information about falls and fall prevention should remain positive and hopeful. For example, the title “Stay Independent—Avoid a Fall!” was received well, whereas a quote, “We are all just one fall away from the nursing home,” was perceived as overly negative. Participants preferred images of active seniors participating in activity and exercise, grandparents interacting with grandchildren, and images presenting realistic depictions of older adults.
Discussion
Participant knowledge about fall risk and fall prevention generally matched current evidence (although not always using medical terminology). For example, seniors perceived muscle weakness (i.e., described as difficulty climbing stairs) as the most serious risk factor for falls. Muscle weakness has been shown in most studies to consistently be an important risk factor—increasing fall risk four- to fivefold (RAND, 2003). Although this is not supported by evidence-based research, participants perceived stepping up onto a curb as a unique fall-risk factor. Explicit consequences such as nursing home placement or death were unacceptably negative and would not motivate new behaviors. This is consistent with the findings of Yardley et al. (2006) indicating that overly negative messages about fall risk were not well received by seniors. Participants consistently recommended that a brochure encourage seniors to take an active role in fall prevention and provide specific prevention recommendations.
Seniors’ main concern about potential consequences of falling was the resultant loss of independence. This concern extended to the relationship of fall-prevention strategies and perceived social stigma; prevention strategies that outwardly implied a loss of independence or frailty, such as use of an assistive device, were the most difficult to accept. Despite the acknowledged difficulty in adopting these prevention strategies, seniors did recognize that nonadherence to prescribed assistive devices would likely increase the risk of falls.
Although data suggest that two thirds of seniors in California are sedentary (Wallace, Nadereh, Enriquez-Haass, & Sripipatana, 2003), seniors in the current study thought that increasing exercise was one of the easier prevention strategies to adopt. Current exercisers tended to be overrepresented in our sample, all of whom had access to senior-center-based exercise programs, underscoring the important current role of community centers in delivering exercise programs to community-dwelling older adults. The current benefits of community-based exercise programs may be further enhanced by increasing the availability of evidence-based programs that target fall prevention.
From a transtheoretical model behavior-change perspective, these community-dwelling groups were typically at a precontemplative or contemplative stage of readiness to change. Some individuals had taken steps to prevent falls, such as participating in exercise programs, suggesting that some were in the action or maintenance phases, as well. Based on the diversity of stages present in our participants, general public health educational campaigns are unlikely to be sufficient to motivate many seniors to engage in fall-prevention activities; some individuals will need individualized recommendations and relevant motivational statements (e.g., “maintain your independence”). The preference for facts about falls accompanying each self-assessment item appeared to enhance self-relevancy, a critical factor in motivating behavioral change in the extended parallel process model framework. Individual scores on the fall-risk self-assessment increased self-relevance of the risks. In addition, the inclusion of information about community resources was well-received and may increase self-efficacy for making the necessary behavioral changes.
Participants’ health care experiences reflect a lack of attention to fall prevention in primary-care settings. Generally, seniors did not view doctors as a major resource for information on fall prevention. Across all focus groups, participants shared their intentions of using a fall-prevention brochure to prompt a discussion with their doctors. In addition, seniors recommended that the brochure be distributed to medical offices to increase awareness of both patients and staff.
Although our population sample was intended to reflect the U.S. Census in ethnic diversity, the demographics of our senior centers tended to be less diverse, leading to an underrepresentation of Asian American participants. Nonetheless, our sample is more diverse than is typical in many studies of older patients. In addition, participants at these senior centers who volunteered were generally high functioning and at relatively low risk of falling; however, the target audience for a fall-risk brochure would also include those who are low functioning and at moderate to high risk of falling. Men were underrepresented in our sample, which was likely because of the higher proportion of women than men that attend community and senior centers.
Findings from this study should be extended in future research. Specifically, future studies will need to establish the validity of the fall-risk self-assessment and its scoring scale to identify and quantify fall risk. Future studies should also examine the impact of the brochure on encouraging behavior change among seniors at risk for falls.
To our knowledge, this is the first systematic development of a fall-risk educational brochure including a self-assessment inventory for use by seniors in the community. We found that seniors recognize falls as a serious threat, and some prevention strategies are more acceptable than others. National dissemination of this brochure, including the fall-risk self-assessment, may be a low-cost way to improve identification of fall risks, encourage seniors to discuss falls with their health care providers, and stimulate fall-prevention activities. Distribution of the brochure may increase practitioner awareness of the need to regularly screen for fall risks in older patients. Practitioners can use the brochure as a prescreening instrument and use the “Facts About Falls” section as patient education.
Acknowledgments
This study was funded in part by the Centers for Disease Control and Prevention (05FED28430), National Institutes of Health (K23AG028452), and the Archstone Foundation (01-01-10).
We acknowledge the contributions of the Archstone Foundation–funded Fall Prevention Center of Excellence for assistance with graphic materials used in this research project. We also acknowledge Judy Stevens, PhD, and Shane Diekman, PhD, for their contributions to the focus-group discussion guides and to the development of the brochure.
Contributor Information
Rebecca L. Vivrette, Geriatric Research, Education and Clinical Center, VA Greater Los Angeles Healthcare System, North Hills, CA
Laurence Z. Rubenstein, Donald W. Reynolds Dept. of Geriatric Medicine, University of Oklahoma College of Medicine, Oklahoma City, OK 73104
Jennifer L. Martin, Geriatric Research, Education and Clinical Center, VA Greater Los Angeles Healthcare System, North Hills, CA
Karen R. Josephson, Geriatric Research, Education and Clinical Center, VA Greater Los Angeles Healthcare System, North Hills, CA
B. Josea Kramer, Division of Geriatrics, David Geffen School of Medicine at UCLA, Los Angeles, CA.
References
- American Geriatrics Society, British Geriatrics Society, American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. Journal of the American Geriatrics Society. 2001;49(5):664–672. [PubMed] [Google Scholar]
- Braun BL. Knowledge and perception of fall-related risk factors and fall-reduction techniques among community-dwelling elderly individuals. Physical Therapy. 1998;78(12):1262–1276. doi: 10.1093/ptj/78.12.1262. [DOI] [PubMed] [Google Scholar]
- Bunn F, Dickinson A, Barnett-Page E, McInnes E, Horton K. A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing and Society. 2008;28:449–472. [Google Scholar]
- Centers for Disease Control and Prevention & National Center for Injury Prevention and Control. Web-based injury statistics query and reporting system (WISQARS) 2006 Retrieved from www.cdc.gov/ncipc/wisqars.
- Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, Shekelle PG. Interventions for the prevention of falls in older adults: Systematic review and meta-analysis of randomized clinical trials. British Medical Journal. 2004;328:680–683. doi: 10.1136/bmj.328.7441.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie L, Robertson MG, Lamb S, Gates S, Cumming R, Rowe B. Interventions for preventing falls in elderly people. Cochrane Database of Systematic Reviews. 2003;4:CD000340. doi: 10.1002/14651858.CD000340. [DOI] [PubMed] [Google Scholar]
- Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: A 1-year prospective study. Archives of Physical Medicine and Rehabilitation. 2001;82:1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- Krueger R, Casey M. Focus groups: A practical guide to applied research. 4. Thousand Oaks, CA: Sage; 2008. [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Peek-Asa C, Zwerling C. Role of environmental interventions in injury control and prevention. Epidemiologic Reviews. 2003;25:77–89. doi: 10.1093/epirev/mxg006. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of change. American Journal of Health Promotion. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- RAND Corporation. Evidence report and evidence-based recommendations. Falls prevention interventions in the Medicare population. 2003 Retrieved from http://www.rand.org/pubs/reprints/2007/RAND_RP1230.pdf.
- Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clinics in Geriatric Medicine. 2002;18(2):141–158. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Solomon DH, Roth CP, Young RT, Shekelle PG, Chang JT, Wenger NS. Detection and management of falls and instability in vulnerable elders by community physicians. Journal of the American Geriatrics Society. 2004;52(9):1527–1531. doi: 10.1111/j.1532-5415.2004.52417.x. [DOI] [PubMed] [Google Scholar]
- Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and nonfatal falls among older adults. Injury Prevention. 2006;12:290–295. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Grounded theory methodology: An overview. In: Denzin N, Lincoln Y, editors. Handbook of qualitative research. Thousand Oaks, CA: Sage; 1994. pp. 273–285. [Google Scholar]
- Tromp A, Pluijm S, Smit J, Deeg D, Bouter L, Lips P. Fall-risk screening test: A prospective study on predictors for falls in community-dwelling elderly. Journal of the American Geriatrics Society. 2001;54(8):837–844. doi: 10.1016/s0895-4356(01)00349-3. [DOI] [PubMed] [Google Scholar]
- Wallace S, Nadereh P, Enriquez-Haass V, Sripipatana A. Health of older Californians: County data book (Paper 16) 2003 Oct 1; Retrieved from UCLA Center for Health Policy Research: http://repositories.cdlib.org/ucla_healthpolicy/16.
- Wenger N, Roth C, Shekelle P, Young R, Solomon D, Kamberg C, Reuben MD. A practice-based intervention to improve primary care for falls, urinary incontinence, and dementia. Journal of the American Geriatrics Society. 2009;47:547–555. doi: 10.1111/j.1532-5415.2008.02128.x. [DOI] [PubMed] [Google Scholar]
- Wenger NS, Solomon DH, Amin A, Besdine RK, Blazer DG, Cohen H, Rosenthal RA. Application of assessing care of vulnerable elders—3 quality indicators to patients with advanced dementia and poor prognosis. Journal of the American Geriatrics Society. 2007;55(Suppl 2):S457–S463. doi: 10.1111/j.1532-5415.2007.01375.x. [DOI] [PubMed] [Google Scholar]
- Willis G. Cognitive interviewing: A tool for improving questionnaire design. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- Witte K. Putting the fear back into fear appeals: The extended parallel process model. Communication Monographs. 1992;59:329–349. [Google Scholar]
- Yardley L, Donovan-Hall M, Francis K, Todd C. Older people’s views of advice about falls prevention: A qualitative study. Health Education Research. 2006;21(4):508–517. doi: 10.1093/her/cyh077. [DOI] [PubMed] [Google Scholar]
- Zonta M, Ong P. Los Angeles County: Racial/Ethnic diversity 2000. n.d Retrieved from UCLA School of Public Affairs: http://lewis.sppsr.ucla.edu/special/metroamerica/ladiversity/Newr00.jpg.