Abstract
Pituitary autoimmunity encompasses a spectrum of conditions ranging from histologically proven forms of lymphocytic hypophysitis to the presence of pituitary antibodies in apparently healthy subjects. Hypophysitis is a rare but increasingly recognized disorder that typically presents as a mass in the sella turcica. It mimics clinically and radiologically other non-secreting sellar masses, such as the more common pituitary adenoma. Hypophysitis shows a striking temporal association with pregnancy, and it has been recently described during immunotherapies that block CTLA-4. Several candidate pituitary autoantigens have been described in the last decade, although none has proven useful as a diagnostic tool. This review summarizes the advances made in the field since the publication of the first review on pituitary autoimmunity, and the challenges that await clarification.
Keywords: Hypophysitis, Pituitary antigens, Pituitary antibodies
1. Historical context and scope
Modern autoimmunity was born in the early 1950s with seminal discoveries in endocrine diseases. Voisin and Barber described an experimental model of autoimmune orchitis in guinea pigs in 1951, Rose and Witebsky a model of thyroiditis in rabbits in 1956, and Colover and Glynn a model of adrenalitis in guinea pigs in 1958. The fourth endocrine gland to be recognized as a target of autoimmunity was the pituitary. In 1962 Goudie and Pinkerton described the autopsy of a young woman who died of adrenal insufficiency in the post-partum period. They noted a marked lymphocytic infiltration of the anterior pituitary, the coexistence of other autoimmune endocrinopathies (thyroiditis and adrenalitis), and a clear temporal association with pregnancy. Seven additional patients with hypophysitis were reported up to 1978, the year when Bottazzo and Doniach published first review on pituitary autoimmunity.
Pituitary autoimmunity comprises as of March 2008 a total of 573 articles (see http://pathology2.jhu.edu/hypophysitis for the complete bibliography), describing the clinical features of about 500 patients with primary autoimmune hypophysitis (AH). Our review will focus on the immunological aspects of AH, highlighting the advances made in the last 30 years and the future challenges.
2. Spectrum of pituitary autoimmunity
Pituitary autoimmunity is a complex and incompletely defined spectrum of conditions. The spectrum comprises histologically proven lymphocytic hypophysitis, clinically suspected hypophysitis, pituitary antibodies in patients with isolated pituitary hormone deficiencies, with pituitary diseases not typically considered autoimmune, with non-pituitary autoimmune diseases, with non-autoimmune non-pituitary diseases, and pituitary antibodies in healthy subjects.
Autoimmune hypophysitis (histologically proven or clinically suspected)
AH is characterized pathologically by lymphocytic infiltration of the anterior and/or posterior pituitary lobe. Pure involvement of the anterior or posterior lobes are known as adenohypophysitis or infundibuloneurohypophysitis, whereas involvement of both lobes is sometimes referred to as panhypophysitis.
Lymphocytes are the dominant infiltrating cells. They can diffuse throughout the parenchyma and at times organize in true lymphoid follicles. Plasma cells are also common; more rare are eosinophils, macrophages, and neutrophils. Overall the infiltrating hematopoietic cells disrupt the normal architecture, eventually destroying the parenchyma that becomes replaced by fibrotic tissue. Occasionally, multinucleated giant cells are found in AH. They are also of hematopoietic origin (likely representing fused macrophages), and more typical of granulomatous hypophysitis, which has distinct epidemiological and clinical features from lymphocytic hypophysitis. A small percentage of AH patients (12 of 311 where a pituitary biopsy was performed, 4%), however, have mixed lymphocytic and granulomatous lesions in the anterior pituitary, suggesting common themes for the two diseases. In 1984 McKeel suggested that the two forms represent different stages of the same disease. In a recently published mouse model of lymphocytic hypophysitis, we detected multinucleated giant cells during the initial florid phase of disease.
AH is more common in women, although the female:male ratio is decreasing in recent years as more men are reported. As of October 2004, when we reviewed the first 379 AH patients for Endocrine Reviews, the female:male ratios were 6.0, 1.0, and 1.8 for adeno-, infundibuloneuro-, and pan-hypophysitis, respectively. In the last four years, 113 additional patients have been identified and these ratios have become 4.3, 1.3, and 1.7. AH is rare in children (25 cases reported in patients ≤18 years old at the time of presentation) and in seniors (27 cases in patients ≥70 years old), and peaks in incidence in the 4th decade of life. When AH affects women of the reproductive age, it shows a striking temporal association with pregnancy. In the 211 women with adenohypophysitis and age between 15 and 45 years, AH presented during late pregnancy or early post-partum in 146 of them (69%). The reasons behind this association are unknown, but if unraveled, could teach us a great deal about the interaction of the endocrine and immune system in the induction of autoimmune disease. The association is much weaker for infundibuloneurohypophysitis (3 of 11 women, 27%) and pan-hypophysitis (8 of 45 women, 18%).
AH typically presents as a sella turcica mass with four variable categories of symptoms: headache and/or visual disturbances (287 of 492 patients, 58%); symptoms of hypopituitarism [218 of 492 patients, 44%, most commonly symptoms from low ACTH (158 patients), low TSH (76 patients), low gonadotropins (70 patients), or low prolactin (37 patients)]; polyuria and polydipsia (151 of 492 patients, 31%); and, least commonly, symptoms of hyperprolactinemia (90 of 492 patients, 18%). Overall, symptoms are not specific for AH but rather shared with other masses occupying the sella turcica, such as the more common pituitary adenoma. Even MRI does not allow distinction of AH from sellar masses, so that about half of AH patients are misdiagnosed as having a non-secreting pituitary adenoma and undergo unnecessary surgery [1]. Currently, a diagnosis of certainty of AH can only be achieved by pathological examination of a pituitary biopsy, which requires an invasive surgical intervention. It should be possible to distinguish before surgery AH from the other non-secreting sellar masses because only AH has an autoimmune pathogenesis. This distinction would be very beneficial for the affected patients because the treatment of AH differs significantly from that of the other sellar masses. Unfortunately, the key autoantigen(s) targeted by the patient’s own immune system in AH await identification or clinical confirmation, so that valid antigen-specific antibody assays have yet to be developed. Current immunological tests for AH (such as those based on immunofluorescence, IF) lack adequate sensitivity and specificity, and therefore have little role in the diagnosis and management of AH patients.
Clinically suspected AH forms are those where the diagnosis is made on clinical, endocrinological, and MRI grounds without the aid of pituitary biopsy and pathological exam. About a third of the patients are diagnosed in this fashion. Notable in this group are the cases described following cancer immunotherapies that block CTLA-4, used as a booster of immune responsiveness. For example, 5% of patients with advanced melanoma who are vaccinated with the gp100 melanoma associated antigen and receive a CTLA-4 blocking antibody also develop AH.
The natural history of AH is variable. Most patients improve after a mass reducing treatment (pituitary surgery or high-dose glucocorticoids) and either require some form of long-term hormone replacement (72%) or need no medications (17%); other patients die because of an irreversible adrenal insufficiency (7%); and the remaining few (4%) improve spontaneously without treatment. Morphologically, the pituitary mass demonstrated at diagnosis shrinks in most patients. A radiological follow-up was available in 204 AH patients and showed reduction or disappearance of the initial pituitary mass in 181 cases (88%), and no significant change in 23 cases (12%). An empty sella developed in 21 of the 204 (10%) patients.
Pituitary antibodies in isolated pituitary hormone deficiencies
Isolated pituitary hormone deficiencies are those conditions where only one of the pituitary hormones is lacking or inactive. Most common are the isolated defects of adrenocorticotropin (ACTH) and growth hormone (GH), whereas only a few cases have been reported with isolated gonadotropin, thyrotropin, or prolactin deficiencies. Isolated pituitary defects recognize four main causes: genetic (such as mutations of the T-box transcription factor Tpit for ACTH), iatrogenic, brain trauma or irradiation, and autoimmune. At times, however, their cause remains unknown (idiopathic forms).
Isolated ACTH deficiency, first described in 1954 by Steinberg, is a potentially lethal condition diagnosed by demonstrating low cortisol and inappropriately low ACTH, absent adrenal response to pituitary stimuli, and intact adrenal response to synthetic ACTH injection. Its most common cause remains iatrogenic (the one induced by glucocorticoid administration), but autoimmune forms are increasingly recognized. An autoimmune basis for isolated ACTH deficiency has been established using the following criteria: the pathological demonstration in rare cases of the typical lymphocytic infiltration in the anterior pituitary [2;3]; the association with other, better characterized autoimmune diseases, such as Hashimoto thyroiditis, vitiligo, and premature ovarian failure [4]; and the presence of pituitary antibodies. These antibodies have been measured by IF, immunoblotting (IB), and ELISA and found positive in about 40% of the patients (Table 1). The largest ongoing cohort of patients with isolated ACTH deficiency, curated by Kasperlik-Zaluska, now comprises almost 300 cases. These patients have a striking female preponderance (F:M ratio of about 11:1), as seen in many autoimmune diseases, and a pituitary antibody prevalence of 34%.
Table 1.
Prevalence of pituitary antibodies in autoimmune hypophysitis, various diseases, and healthy controls.
| Diagnosis | Patients | IF | IB | ELISA | in vitro transcription and translation | References | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| GH | PGSF1 | PGSF2 | α-enolase | TRDR6 | PC1 | 7B2 | ||||||
| Hypophysitis | 159 | 16/28 (57 %) | 50/100 (50 %) | 2/17 (12 %) | 1/17 (6 %) | 2/17 (12 %) | 7/17 (41 %) | 0/11 (0 %) | 2/14 (14 %) | 2/14 (14 %) | [5–12] | |
| Isolated ACTH def. | 151 | 11/33 (33 %) | 35/88 (40 %) | 5/14 (36 %) | 1/10 (10 %) | 2/10 (20 %) | 1/10 (10 %) | 2/10 (20 %) | 0/10 (0 %) | 0/10 (0 %) | [13–16;6–10;17;18] | |
| Isolated GH def. | 275 | 26/177 (15 %) | 10/55 (18 %) | 10/65 (15 %) | [19–21;16;22–24] | |||||||
| Isolated gonadotropin def. | 21 | 8/21 (38%) | [25] | |||||||||
| Isolated TSH def. | 12 | 1/4 (25 %) | 0/4 (0 %) | 2/4 (50 %) | 0/4 (0 %) | 0/4 (0 %) | 0/4 (0 %) | [8–10] | ||||
| Multiple pituitary hormone def. | 78 | 5/26 (19%) | 10/41 (24%) | 2/18 (11%) | [20;26;16;7;22;25] | |||||||
| Empty sella | 106 | 24/32 (75 %) | 8/36 (22 %) | 16/38 (42 %) | [27;28;22;29] | |||||||
| Addison disease | 71 | 4/40 (10 %) | 6/14 (43 %) | 0/17 (0 %) | [27;5;23;11] | |||||||
| Graves disease | 783 | 51/378 (13 %) | 64/259 (25 %) | 65/312 (21 %) | 0/10 (0 %) | 0/10 (0 %) | 0/10 (0 %) | 1/10 (10 %) | [5;7–9;30;12] | |||
| Hashimoto thyroid. | 1147 | 150/898 (17%) | 26/156 (17 %) | 35/172 (20 %) | 1/10 (10 %) | 0/10 (0 %) | 1/10 (10 %) | 2/10 (20 %) | [5;7–9;30;12] | |||
| Polyglandular auto. | 608 | 31/455 (7 %) | 39/67 (58 %) | 42/86 (49 %) | [31;32;11;33] and Scherbaum, Lancet, 1983 | |||||||
| Type 1 diabetes | 372 | 47/243 (19 %) | 41/90 (46 %) | 25/64 (39 %) | 0/20 (0 %) | [32;13;14;34;21;6;23;11] | ||||||
| Celiac disease | 130 | 7/130 (5 %) | Iughetti L, Eur J Pediatr, 2006 | |||||||||
| Lupus | 45 | 0/13 (0 %) | 0/7 (0 %) | 1/7 (14 %) | 1/7 (14 %) | 0/25 (0 %) | [27;8;11], and Hansen BL, J Neuroimmunol, 1983 | |||||
| Multiple sclerosis | 33 | 11/33 (33 %) | Hansen BL, J Neuroimmunol, 1983 | |||||||||
| Rheumatoid arthr. | 25 | 2/15 (13 %) | 3/10 (30 %) | [5;9] | ||||||||
| Sjögren syndrome | 20 | 0/20 (0 %) | [11] | |||||||||
| Diabetes insipidus | 197 | 39/197 (20 %) | [35;27;23] and Scherbaum, Lancet, 1983 | |||||||||
| Idiopathic ↑ PRL | 163 | 34/132 (26 %) | 13/31 (42 %) | [22;36;37] | ||||||||
| Pituitary adenoma | 287 | 23/142 (16 %) | 16/68 (24 %) | 12/85 (14 %) | 0/11 (0 %) | 0/11 (0 %) | 0/11 (0 %) | 6/13 (46 %) | 5/11 (45 %) | 4/11 (36 %) | [27;28;5;21;16;22;8;23;9;10;36;12] and Scherbaum, Lancet, 1987 | |
| Sheehan syndrome | 54 | 8/23 (35 %) | 14/25 (56 %) | 0/6 (0 %) | 2/3 (67 %) | 0/3 (0 %) | 0/3 (0 %) | [15;16;38;9;10;39] | ||||
| Eating disorders | 57 | 42/57 (74 %) | Fetissov SO, PNAS, 2002 | |||||||||
| Cryptorchidism | 52 | 25/52 48 % | Pouplard A., Lancet, 1984 | |||||||||
| Type 2 diabetes | 279 | 23/93 (25 %) | 39/188 (21 %) | [34;21] and Kobayashi T, Endocr J, 1998 | ||||||||
| Goiter (non-autoimmune) | 339 | 3/339 (1 %) | [30] and Kobayashi I, Endocrinol Jpn, 1998 | |||||||||
| Healthy controls | 2438 | 28/940 (3 %) | 62/917 (7 %) | 44/736 (6 %) | 0/36 (0 %) | 0/36 (0 %) | 0/36 (0 %) | 2/46 (4 %) | 0/90 (0 %) | 0/36 (0 %) | 0/36 (0 %) | |
| 7902 | 593/4389 | 386/2024 | 266/1729 | 5/105 | 4/105 | 7/105 | 25/123 | 42/269 | 7/78 | 6/78 | ||
IF: Immuno Fluorescence, IB: Immuno Blotting, ELISA: Enzyme-Linked Immuno Sorbent Assay, GH: Growth Hormone 1, PGSF1, 2: Pituitary Gland Specific Factor 1, 2, TDRD6: Tudor Domain Containing Protein 6, PC1: Prohormone Convertase 1, 7B2: neuroendocrine secretory protein 7B2 (secretogalanin V),
↑ PRL: hyperprolactinemia, “Number of positive patients” divided by “Total number of tested patients” and the percentage of positive patients are indicated.
Isolated GH deficiency causes short stature in children, whereas it is usually asymptomatic in adults. In the majority of children no cause can be identified (idiopathic forms); in the remaining minority, isolated GH deficiency results from defects in the genes coding for GH1 or GH releasing hormone receptor. In adults, isolated GH deficiency is most commonly caused by traumatic brain injury or external irradiation treatments, although several cases remain idiopathic. Autoimmunity has been proposed to explain some forms of idiopathic isolated GH deficiency based on the presence of pituitary antibodies. Seven papers have tested pituitary antibodies in patients (mainly children) with isolated GH deficiency, showing a prevalence of about 15%. This prevalence, although higher than that of healthy controls, is overall low. The role of autoimmunity remains unclear.
Isolated gonadotropin deficiency of autoimmune origin was first reported in 1985 by Barkan in two men with autoimmune polyglandular autoimmune type 2, and more recently by De Bellis and colleagues in a cohort of 21 cases. These authors found by IF pituitary antibodies in 38% of the cases, as compared to 6% (3 of 50) of healthy controls [25].
Isolated thyrotropin deficiency of autoimmune origin was first reported by Wong in 2004 in a biopsy proven case of lymphocytic hypophysitis, and then by Hashimoto in a case series of 6 patients (one of whom was histologically proven) [40]. Pituitary antibodies against candidate pituitary antigens have been measured by Amino’s group in four additional patients, and found to be absent or low (Table 1).
Pituitary antibodies in non-autoimmune pituitary diseases
Pituitary antibodies have been described in pituitary diseases not typically considered autoimmune in nature, but for which an autoimmune component has been proposed: the empty sella syndrome and Sheehan syndrome.
Empty sella is the herniation of the subarachnoid space into the sella turcica. This herniation can occur because of anatomical variations of the diaphragma sellae (usually an incidental finding known as primary empty sella), or from a loss of intrasellar volume (secondary empty sella). The latter develops for example in pituitary adenomas that are surgically removed, treated with radiotherapy, or undergo hemorrhagic infarction, or in Sheehan syndrome. AH is a potential cause of secondary empty sella considering that the pituitary gland, following the initial increase in size, gradually becomes atrophic and fibrotic. Empty sella has been, in fact, demonstrated in 10% of AH patients who had at presentation a pituitary mass and later developed pituitary atrophy.
An autoimmune basis for secondary empty sella was first proposed in 1986 by Okada, who reported a case of partial hypopituitarism with empty sella and pituitary antibodies after pregnancy. Six subsequent papers have discussed pituitary autoimmunity in the context of an empty sella: [28;22;29] and Nishiyama S 1993, Beressi N 1999 and Klein J 2005. In particular, Beressi and colleagues concluded their excellent review by writing “empty sella may in fact be the final term of initially undiagnosed lymphocytic hypophysitis”. Pituitary antibodies have been found in patients with empty sella (Table 1) with contrasting results. From one hand, Komatsu detected by IF antibodies recognizing mouse corticotroph cells (AtT-20) in 24 of 32 patients with empty sella (75%) [27]; Mau found by IB antibodies against human GH and ACTH in 2 of 6 patients (33%) [28]; and Keda by ELISA found them in 16 of 38 patients (42%) [22]. On the other hand, Bensing and colleagues found no evidence of autoimmunity in patients with empty sella: antibodies to 49 kDa alpha-enolase were present in 6 of 30 patients (20%), similar to what found in healthy controls (11 of 50, 22%) [29]. Timing of pituitary antibodies measurement is important. Antibodies decrease over time when the antigenic load decreases, such as when a gland is destroyed by the autoimmune attack and becomes atrophic. In 2003, Chiovato et al published that antibodies to thyroperoxidase, thyroglobulin, and thyrotropin receptor progressively disappear after complete ablation of the thyroid (either by surgery or radioiodine), indicating that continued antibody production requires autoantigen persistence. Thus, if empty sella is caused by AH, the pituitary gland at that stage is by definition atrophic and predicted to have low antigenic load and, consequently, low or absent pituitary antibodies. In summary, AH is a possible cause of secondary empty sella, although the issue remains to be clarified.
Sheehan syndrome, first described in 1937, is an ischemic necrosis of the anterior pituitary caused by a severe peri-partum hemorrage. Autoimmunity has been proposed as a mechanism for Sheehan syndrome, but the data are scanty. After the original report in 1965 by Engelberth & Jezkova, which described high titer of pituitary antibodies by complement consumption test in a woman with clinical signs of Sheehan syndrome 5 years after delivery, two case-control studies found pituitary antibodies in Sheehan patients at significantly higher prevalence than in healthy controls. Goswami and colleagues detected by IB antibodies to 49 kDa alpha enolase in 12 of 19 cases and in only 9 of 56 controls (p= 0.007) [38]. De Bellis and colleagues recently found by IF pituitary antibodies in 7 of 20 Sheehan cases and in none of 50 healthy controls (p= 0.001) [39].
Pituitary antibodies in other diseases
Pituitary antibodies have been detected in a variety of other conditions, ranging in prevalence from a minimum of 5% in celiac disease to a maximum of 74% in eating disorders (Table 1). Autoimmune thyroiditis (represented by Graves disease and Hashimoto thyroiditis) is the most common condition where pituitary antibodies have been measured (with 13 publications). Manetti and colleagues recently published the largest cohort [30] and tabulated results of six previous studies. One subsequent study was published in Polish by Gut et al; the remaining articles are listed in Table 1. The functional significance and clinical value of pituitary antibodies in these conditions remain to be established.
3. Candidate pituitary autoantigens
Identification of “pathogenic” autoantigen(s) is critical to advance the field in any autoimmune disease. A pathogenic autoantigen causes disease when attacked by the patient’s own immune system (either during the initiation or the effector phase), and recreates the human disease when injected into experimental animals in an immunogenic context. Such identification has at least two clear benefits. First, it allows the development of specific autoantibody assays that can be used to diagnose, monitor, or predict an autoimmune disease. Second, it enables reproduction in experimental animals of the human disease with a single protein (or even a single epitope), greatly facilitating understanding of the autoimmune response. Such understanding is necessary for developing novel antigen-specific immunotherapies. For AH pathogenic autoantigens are yet to be discovered, although several candidates have been proposed during the last eight years.
Growth hormone. In 2001, Takao and colleagues reported that a pituitary cytosolic band of 22 kDa was recognized by the serum of 11 of 15 (73%) patients with clinically suspected hypophysitis and 7 of 9 (78%) patients with isolated ACTH deficiency, but not by healthy controls, Hashimoto thyroiditis, or Graves disease patients [7]. Sequencing of this band yielded a nonapeptide fragment that corresponds to either the pituitary GH1 or the placental GH2. When Tanaka and colleagues expressed in vitro the full-length GH1, however, they reported a low recognition in hypophysitis (2 of 17, 12%), isolated ACTH deficiency (1 of 10, 10%), and other autoimmune diseases (2 of 31, 6%) [8].
Alpha-enolase. Crock’s laboratory reported that a 49 kDa pituitary cytosolic band was recognized more frequently by hypophysitis sera (19 of 32) than by sera of healthy controls (5 of 52, p< 0.0001), patients with other autoimmune diseases (13 of 62, p= 0.011), or pituitary adenoma (4 of 20, p= 0.059) [5]. In 2002, the same laboratory identified the 49 kDa band as alpha-enolase, an ubiquitous glycolytic enzyme. Tanaka et al. expressed in vitro the full-length alpha-enolase to assess its clinical utility, and showed that it was recognized not only by hypophysitis patients (7 of 17, 41%), but also by pituitary adenomas (6 of 13, 46%), other autoimmune diseases (6 of 30, 20%), and healthy controls (2 of 46, 4%) [9]. Antibodies against alpha-enolase are now known to be present in a large variety of infectious and autoimmune diseases, and are therefore not specific for AH.
Pituitary gland specific factors 1a and 2 transcripts were found in 2002 by Amino’s laboratory during a gene expression profile of the human pituitary, but experimental support for the proteins is lacking. Factor 1a, now classified as chromosome 19 open reading frame 30, was expressed in vitro and reported to be recognized only minimally by hypophysitis sera (1 of 17, 6%), isolated ACTH deficiency (2 of 10, 20%), and other autoimmune diseases (1 of 31, 3%) [8]. Factor 2 showed a similar low recognition in that study population [8].
Secretogranin II. In 2007, Bensing and colleagues described a 70-yr-old man with clinically suspected hypophysitis whose serum identified five clones in a human pituitary cDNA expression library all corresponding to secretogranin II. The protein is highly expressed in the pituitary but also in organs and tissues containing neuroendocrine cells. Secretogranin II is an interesting candidate that needs to be tested in a larger number of cases and non-affected controls.
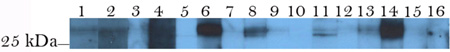
In 2008 we described two new candidate autoantigens in the 27 kDa pituitary cytosolic region that were recognized by hypophysitis but not by healthy control sera: chromosome 14 open reading frame 166 and chorionic somatomammotropin [12]. The first one, also known as CGI99, is an RNA binding protein of incomplete characterization. We have tested his-tagged human CGI99 for its recognition by AH (Figure 1, lanes 1, 4, 9, and 13), Hashimoto thyroiditis (lanes 2 and 7), and healthy control sera (remaining lanes), and found no specificity. Chorionic somatomammotropin is an interesting candidate (see discussion in [12]) but awaits confirmation.
4. Pituitary antibodies
Pituitary antibodies have been measured both by non-antigen specific and antigen-specific methods. The first methods include mainly IF, IB, and ELISA, and have been excellently reviewed in 2006 by Crock. The second ones include currently in vitro transcription/translation assays based on candidate pituitary autoantigens, and are summarized in Table 1.
IF does not require knowledge of the precise autoantigens. It is therefore a useful tool when a new autoimmune disease is being characterized, although IF is poorly sensitive and subjective in the interpretation. IF using pituitary substrates has additional challenges. In 1975 Bottazzo and colleagues described the recognition of prolactin-secreting cells (not prolactin itself) in patients with autoimmune endocrine diseases [31]. The authors noted that only freshly obtained human pituitary glands provided a suitable substrate, whereas post-mortem human pituitaries, rat, or bovine pituitary yielded low sensitivity or high background fluorescence. The following year, the same group showed that adult human ACTH-producing cells express Fc receptors: therefore such pituitary sections can bind aspecifically all antibodies, not only those directed against the pituitary. Fetal ACTH cells do not express Fc receptors but are almost impossible to obtain nowadays. The importance of the species as the substrate for pituitary IF was emphasized by Gluck and Scherbaum in 1990. They tested a set of well-characterized sera (46 positive and 37 negative on human fetal pituitary) on pituitary glands from six other species (fetal Macaca fascicularis, adult baboon, pig, beef, sheep, and rat) and reported very low sensitivity and specificity. They concluded their paper by writing that “the use of animal tissue, including non-human primate, yields results that bear no clinical significance”. Nevertheless, commercially available IF kits now use pituitaries from baboon or Macaca mulatta. Different substrates are likely an explanation for the variability observed in IF-based pituitary antibody tests (Table 1).
IB to detect pituitary antibodies was first reported in 1993 by Crock and colleagues [19]. We have recently compared IF and IB and found that IB was more sensitive (64% vs. 57%) and specific (86% vs. 76%) than IF in predicting histologically-proven AH. These two non-antigen specific methods, however, lack sufficient accuracy to be clinically useful. Similar concerns pertain to ELISA assays, which have used a variety of antigenic substrates and smaller patient subsets (Table 1).
Antigen-specific methods, such as in vitro transcription/translation or more common immunoassays, are the way of the future and will certainly further our understanding of AH once the pathogenic autoantigen(s) become identified.
Take-home messages.
Autoimmune hypophysitis (AH) is an increasingly recognized disorder of the pituitary gland that poses diagnostic challenges with the other, more common, non-secreting masses of the sella turcica.
AH is associated with pregnancy and with immunotherapies that block CTLA-4.
The pathogenic pituitary autoantigen(s) remain to be elucidated, although several candidates have been proposed.
Current methods to detect pituitary antibodies have limited clinical value.
Acknowledgements
The work was supported in part by NIH grant DK55670 to PC.
Abbreviations
- AH
autoimmune hypophysitis
- IF
immunofluorescence
- IB
immunoblotting
- ACTH
corticotropin
- GH
growth hormone
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Leung GK, Lopes MB, Thorner MO, Vance ML, Laws ER. Primary hypophysitis: a single-center experience in 16 cases. J Neurosurg. 2004;101:262–271. doi: 10.3171/jns.2004.101.2.0262. [DOI] [PubMed] [Google Scholar]
- 2.Richtsmeier AJ, Henry RA, Bloodworth JM, Ehrlich EN. Lymphoid hypophysitis with selective adrenocorticotropic hormone deficiency. Archives of Internal Medicine. 1980;140:1243–1245. [PubMed] [Google Scholar]
- 3.Jensen MD, Handwerger BS, Scheithauer BW, Carpenter PC, Mirakian R, Banks PM. Lymphocytic hypophysitis with isolated corticotropin deficiency. Annals of Internal Medicine. 1986;105:200–203. doi: 10.7326/0003-4819-105-2-200. [DOI] [PubMed] [Google Scholar]
- 4.Kasperlik-Zaluska AA, Czarnocka B, Czech W. Autoimmunity as the most frequent cause of idiopathic secondary adrenal insufficiency: report of 111 cases. Autoimmunity. 2003;36:155–159. doi: 10.1080/0891693031000095871. [DOI] [PubMed] [Google Scholar]
- 5.Crock PA. Cytosolic autoantigens in lymphocytic hypophysitis. J Clin Endocrinol Metab. 1998;83:609–618. doi: 10.1210/jcem.83.2.4563. [DOI] [PubMed] [Google Scholar]
- 6.Nishiki M, Murakami Y, Ozawa Y, Kato Y. Serum antibodies to human pituitary membrane antigens in patients with autoimmune lymphocytic hypophysitis and infundibuloneurohypophysitis. Clin Endocrinol (Oxf) 2001;54:327–333. doi: 10.1046/j.1365-2265.2001.01210.x. [DOI] [PubMed] [Google Scholar]
- 7.Takao T, Nanamiya W, Matsumoto R, Asaba K, Okabayashi T, Hashimoto K. Antipituitary antibodies in patients with lymphocytic hypophysitis. Horm Res. 2001;55:288–292. doi: 10.1159/000050015. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka S, Tatsumi KI, Kimura M, Takano T, Murakami Y, Takao T, Hashimoto K, Kato Y, Amino N. Detection of autoantibodies against the pituitary-specific proteins in patients with lymphocytic hypophysitis. Eur J Endocrinol. 2002;147:767–775. doi: 10.1530/eje.0.1470767. [DOI] [PubMed] [Google Scholar]
- 9.Tanaka S, Tatsumi KI, Takano T, Murakami Y, Takao T, Yamakita N, Tahara S, Teramoto A, Hashimoto K, Kato Y, Amino N. Anti-alpha-enolase antibodies in pituitary disease. Endocr J. 2003;50:697–702. doi: 10.1507/endocrj.50.697. [DOI] [PubMed] [Google Scholar]
- 10.Tatsumi KI, Tanaka S, Takano T, Tahara S, Murakami Y, Takao T, Hashimoto K, Kato Y, Teramoto A, Amino N. Frequent appearance of autoantibodies against prohormone convertase 1/3 and neuroendocrine protein 7B2 in patients with nonfunctioning pituitary macroadenoma. Endocrine. 2003;22:335–340. doi: 10.1385/ENDO:22:3:335. [DOI] [PubMed] [Google Scholar]
- 11.Bensing S, Fetissov SO, Mulder J, Perheentupa J, Gustafsson J, Husebye ES, Oscarson M, Ekwall O, Crock PA, Hokfelt T, Hulting AL, Kampe O. Pituitary autoantibodies in autoimmune polyendocrine syndrome type 1. Proc Natl Acad Sci U S A. 2007;104:949–954. doi: 10.1073/pnas.0610070104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lupi I, Broman KW, Tzou SC, Gutenberg A, Martino E, Caturegli P. Novel autoantigens in autoimmune hypophysitis. Clin Endocrinol. 2008;68 doi: 10.1111/j.1365-2265.2008.03180.x. [DOI] [PubMed] [Google Scholar]
- 13.Sugiura M, Hashimoto A, Shizawa M, Tsukada M, Maruyama S, Ishido T, Kasahara T, Hirata Y. Heterogeneity of anterior pituitary cell antibodies detected in insulin-dependent diabetes mellitus and adrenocorticotropic hormone deficiency. Diabetes Res. 1986;3:111–114. [PubMed] [Google Scholar]
- 14.Sugiura M, Hashimoto A, Shizawa M, Tsukada M, Saito T, Hayami H, Murayama M, Ishido T. Detection of antibodies to anterior cell surface membrane with insulin-dependent diabetes mellitus and ACTH deficiency. Diabetes Res. 1986;4:63–66. [PubMed] [Google Scholar]
- 15.Kajita K, Yasuda K, Yamakita N, Murai T, Matsuda M, Morita H, Mori A, Murayama M, Tanahashi S, Sugiura M, Miura K. Anti-pituitary antibodies in patients with hypopituitarism and their families: longitudinal observation. Endocrinol Jpn. 1991;38:121–129. doi: 10.1507/endocrj1954.38.121. [DOI] [PubMed] [Google Scholar]
- 16.Kikuchi T, Yabe S, Kanda T, Kobayashi I. Antipituitary antibodies as pathogenetic factors in patients with pituitary disorders. Endocr J. 2000;47:407–416. doi: 10.1507/endocrj.47.407. [DOI] [PubMed] [Google Scholar]
- 17.Bensing S. Pituitary autoantibodies in endocrine disorders. Stockholm: Karolinska Institutet; 2005. [Google Scholar]
- 18.Bensing S, Kasperlik-Zaluska AA, Czarnocka B, Crock PA, Hulting A. Autoantibodies against pituitary proteins in patients with adrenocorticotropin-deficiency. Eur J Clin Invest. 2005;35:126–132. doi: 10.1111/j.1365-2362.2005.01459.x. [DOI] [PubMed] [Google Scholar]
- 19.Crock PA, Salvi M, Miller A, Wall J, Guyda H. Detection of anti-pituitary antibodies by immunoblotting. J Immunol Methods. 1993;162:31–40. doi: 10.1016/0022-1759(93)90404-u. [DOI] [PubMed] [Google Scholar]
- 20.Maghnie M, Lorini R, Severi F. Antipituitary antibodies in patients with pituitary abnormalities and hormonal deficiency. Clin Endocrinol (Oxf) 1994;40:809–810. doi: 10.1111/j.1365-2265.1994.tb02518.x. [DOI] [PubMed] [Google Scholar]
- 21.Yabe S, Kanda T, Hirokawa M, Hasumi S, Osada M, Fukumura Y, Kobayashi I. Determination of antipituitary antibody in patients with endocrine disorders by enzyme-linked immunosorbent assay and Western blot analysis. J Lab Clin Med. 1998;132:25–31. doi: 10.1016/s0022-2143(98)90021-x. [DOI] [PubMed] [Google Scholar]
- 22.Keda YM, Krjukova IV, Ilovaiskaia IA, Morozova MS, Fofanova OV, Babarina MB, Marova EI, Pankov YA, Kandror VI. Antibodies to pituitary surface antigens during various pituitary disease states. J Endocrinol. 2002;175:417–423. doi: 10.1677/joe.0.1750417. [DOI] [PubMed] [Google Scholar]
- 23.De Bellis A, Bizzarro A, Conte M, Perrino S, Coronella C, Solimeno S, Sinisi AM, Stile LA, Pisano G, Bellastella A. Antipituitary antibodies in adults with apparently idiopathic growth hormone deficiency and in adults with autoimmune endocrine diseases. J Clin Endocrinol Metab. 2003;88:650–654. doi: 10.1210/jc.2002-021054. [DOI] [PubMed] [Google Scholar]
- 24.De Bellis A, Salerno M, Conte M, Coronella C, Tirelli G, Battaglia M, Esposito V, Ruocco G, Bellastella G, Bizzarro A, Bellastella A. Antipituitary antibodies recognizing growth hormone (GH)-producing cells in children with idiopathic GH deficiency and in children with idiopathic short stature. J Clin Endocrinol Metab. 2006;91:2484–2489. doi: 10.1210/jc.2006-0040. [DOI] [PubMed] [Google Scholar]
- 25.De Bellis A, Sinisi AA, Conte M, Coronella C, Bellastella G, Esposito D, Pasquali D, Ruocco G, Bizzarro A, Bellastella A. Antipituitary antibodies against gonadotropin-secreting cells in adult male patients with apparently idiopathic hypogonadotropic hypogonadism. J Clin Endocrinol Metab. 2007;92:604–607. doi: 10.1210/jc.2006-1216. [DOI] [PubMed] [Google Scholar]
- 26.Stromberg S, Crock P, Lernmark A, Hulting AL. Pituitary autoantibodies in patients with hypopituitarism and their relatives. J Endocrinol. 1998;157:475–480. doi: 10.1677/joe.0.1570475. [DOI] [PubMed] [Google Scholar]
- 27.Komatsu M, Kondo T, Yamauchi K, Yokokawa N, Ichikawa K, Ishihara M, Aizawa T, Yamada T, Imai Y, Tanaka K, Taniguchi K, Watanabe T, Takahashi Y. Antipituitary antibodies in patients with the primary empty sella syndrome. J Clin Endocrinol Metab. 1988;67:633–638. doi: 10.1210/jcem-67-4-633. [DOI] [PubMed] [Google Scholar]
- 28.Mau M, Phillips TM, Ratner RE. Presence of anti-pituitary hormone antibodies in patients with empty sella syndrome and pituitary tumours. Clin Endocrinol (Oxf) 1993;38:495–500. doi: 10.1111/j.1365-2265.1993.tb00345.x. [DOI] [PubMed] [Google Scholar]
- 29.Bensing S, Rorsman F, Crock P, Sanjeevi C, Ericson K, Kampe O, Brismar K, Hulting AL. No evidence for autoimmunity as a major cause of the empty sella syndrome. Exp Clin Endocrinol Diabetes. 2004;112:231–235. doi: 10.1055/s-2004-817968. [DOI] [PubMed] [Google Scholar]
- 30.Manetti L, Lupi I, Morselli LL, Albertini S, Cosottini M, Grasso L, Genovesi M, Pinna G, Mariotti S, Bogazzi F, Bartalena L, Martino E. Prevalence and functional significance of antipituitary antibodies in patients with autoimmune and non-autoimmune thyroid diseases. J Clin Endocrinol Metab. 2007;92:2176–2181. doi: 10.1210/jc.2006-2748. [DOI] [PubMed] [Google Scholar]
- 31.Bottazzo GF, Pouplard A, Florin-Christensen A, Doniach D. Autoantibodies to prolactin-secreting cells of human pituitary. Lancet. 1975;2:97–101. doi: 10.1016/s0140-6736(75)90004-5. [DOI] [PubMed] [Google Scholar]
- 32.Mirakian R, Cudworth AG, Bottazzo GF, Richardson CA, Doniach D. Autoimmunity to anterior pituitary cells and the pathogenesis of insulin-dependent diabetes mellitus. Lancet. 1982;1:755–759. doi: 10.1016/s0140-6736(82)91809-8. [DOI] [PubMed] [Google Scholar]
- 33.O'Dwyer DT, McElduff P, Peterson P, Perheentupa J, Crock PA. Pituitary autoantibodies in autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED) Acta Biomed. 2007;78:248–254. [PubMed] [Google Scholar]
- 34.Kobayashi T, Yabe S, Kikuchi T, Kanda T, Kobayashi I. Presence of anti-pituitary antibodies and GAD antibodies in NIDDM and IDDM. Diabetes Care. 1997;20:864–866. doi: 10.2337/diacare.20.5.864. [DOI] [PubMed] [Google Scholar]
- 35.Scherbaum WA, Wass JA, Besser GM, Bottazzo GF, Doniach D. Autoimmune cranial diabetes insipidus: its association with other endocrine diseases and with histiocytosis X. Clin Endocrinol (Oxf) 1986;25:411–420. doi: 10.1111/j.1365-2265.1986.tb01707.x. [DOI] [PubMed] [Google Scholar]
- 36.De Bellis A, Colao A, Pivonello R, Savoia A, Battaglia M, Ruocco G, Tirelli G, Lombardi G, Bellastella A, Bizzarro A. Antipituitary antibodies in idiopathic hyperprolactinemic patients. Ann N Y Acad Sci. 2007;1107:129–135. doi: 10.1196/annals.1381.014. [DOI] [PubMed] [Google Scholar]
- 37.De Bellis A, Colao A, Savoia A, Coronella C, Tirelli G, Conte M, Pivonello R, Bellastella A, Sinisi AA, Bizzarro A, Lombardi G, Bellastella G. Effect of long-term cabergoline therapy on the immunological pattern and pituitary function of patients with idiopathic hyperprolactinaemia positive for antipituitary antibodies. Clin Endocrinol (Oxf) 2008 doi: 10.1111/j.1365-2265.2008.03200.x. [DOI] [PubMed] [Google Scholar]
- 38.Goswami R, Kochupillai N, Crock PA, Jaleel A, Gupta N. Pituitary autoimmunity in patients with Sheehan's syndrome. J Clin Endocrinol Metab. 2002;87:4137–4141. doi: 10.1210/jc.2001-020242. [DOI] [PubMed] [Google Scholar]
- 39.De Bellis A, Kelestimur F, Sinisi AA, Ruocco G, Tirelli G, Battaglia M, Bellastella G, Conzo G, Tanriverdi F, Unluhizarci K, Bizzarro A, Bellastella A. Anti-hypothalamus and anti-pituitary antibodies may contribute to perpetuate the hypopituitarism in patients with Sheehan's syndrome. Eur J Endocrinol. 2008;158:147–152. doi: 10.1530/EJE-07-0647. [DOI] [PubMed] [Google Scholar]
- 40.Hashimoto KI, Yamakita N, Ikeda T, Matsuhisa T, Kuwayama A, Sano T, Hashimoto K, Yasuda K. Longitudinal Study of Patients with Idiopathic Isolated TSH Deficiency: Possible Progression of Pituitary Dysfunction in Lymphocytic Adenohypophysitis. Endocr J. 2006;53:593–601. doi: 10.1507/endocrj.k06-055. [DOI] [PubMed] [Google Scholar]