Abstract
Over the past two decades, a convergence of basic and clinical evidence has established the neuropeptide calcitonin-gene-related peptide (CGRP) as a key player in migraine. Although CGRP is a recognised neuromodulator of nociception, its mechanism of action in migraine remains elusive. In this review, we present evidence that led us to propose that CGRP is well poised to enhance neurotransmission in migraine by both peripheral and central mechanisms. In the periphery, it is thought that local release of CGRP from the nerve endings of meningeal nociceptors following their initial activation by cortical spreading depression is critical for the induction of vasodilation, plasma protein extravasation, neurogenic inflammation and the consequential sensitisation of meningeal nociceptors. Mechanistically, we propose that CGRP release can give rise to a positive-feedback loop involved in localised increased synthesis and release of CGRP from neurons and a CGRP-like peptide called procalcitonin from trigeminal ganglion glia. Within the brain, the wide distribution of CGRP and CGRP receptors provides numerous possible targets for CGRP to act as a neuromodulator.
Migraine is a debilitating neurological condition experienced by approximately 6–8% of men and 15–25% of women in western countries (Ref. 1). This high prevalence has led the World Health Organization to rank migraine in the top 20 conditions leading to years lived with disability. This disability results not only from the painful headaches, but also from the host of associated symptoms that co-occur with migraine. The diagnostic criteria for migraine include episodic headache lasting from 4 to 72 h, with two of the following, throbbing, unilateral pain, aggravation on movement, or pain of at least moderate severity, and at least one of the following, nausea or vomiting, or photophobia and phonophobia (Ref. 2). For patients suffering from typical migraine, pain and accompanying symptoms have no obvious genetic, structural or molecular cause. This manuscript reviews the current understanding of migraine, focusing on the role of calcitonin-gene-related peptide (CGRP) in the context of neurogenic inflammation and photophobia.
CGRP is a multifunctional neuropeptide found in every organ system in the body (Refs 3, 4, 5, 6). CGRP immunoreactivity is especially prevalent in the trigeminal nerve, where it is found in nearly 50% of the neurons (Refs 7, 8). Its expression in the trigeminal nerve is of particular interest given the role of the trigeminovascular system in migraine (Ref. 9). The peripheral trigeminovascular system consists of sensory fibres of the trigeminal ganglion that project from meningeal blood vessels (both dural and pial) to brainstem trigeminal nuclei (Refs 10, 11). The central trigeminovascular system refers to regions of the central nervous system (CNS) that further process this input: the spinal trigeminal nucleus and posterior thalamus. At the peripheral nerve endings, CGRP is recognised as the most potent vasodilatory peptide (Ref. 12). CGRP receptors are located on cerebral vascular smooth muscle, where they cause vasodilation (Refs 13, 14, 15). In addition to vasodilation, peripheral release of CGRP also triggers mast cell degranulation, which contributes to neurogenic inflammation together with substance P (Refs 12, 16, 17). CGRP is often co-released with substance P (Refs 18, 19, 20). CGRP receptors have been identified on dural mast cells (Ref. 21). At the central terminals of the trigeminal nerve, CGRP is a neuromodulator at second-order nociceptive neurons in the spinal trigeminal nucleus caudalis (TNc) (Refs 9, 22). CGRP has a similar role in the dorsal horn of the spinal cord, where it can induce central sensitisation to tactile stimuli (Ref. 23). CGRP receptors have been identified in the TNc, a subset of trigeminal ganglion neurons and satellite glia of the trigeminal ganglion (Refs 8, 21, 24, 25, 26). Hence, there are several sites of CGRP receptor action that might be relevant to migraine.
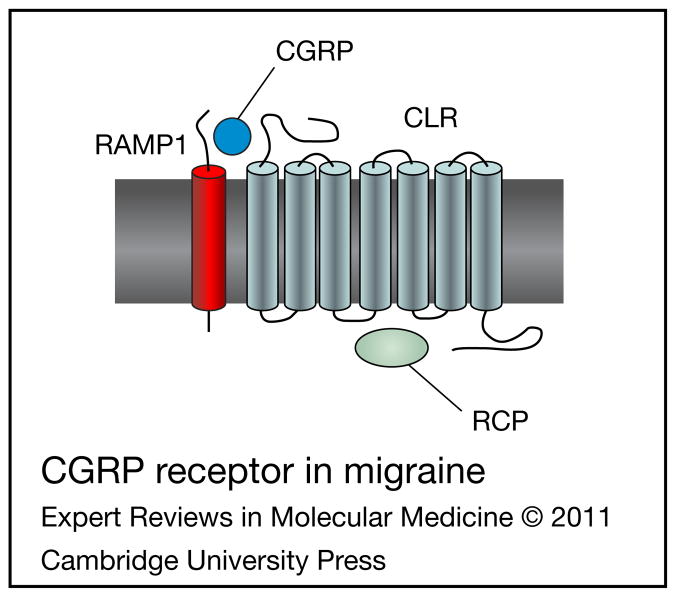
The CGRP receptor is afairly unique multimer of a G-protein-coupled receptor called calcitonin-like receptor (CLR) and a small transmembrane protein called receptor activity-modifying protein 1 (RAMP1) (Fig. 1) (Refs 27, 28). A cytoplasmic protein, receptor component protein (RCP), enhances receptor coupling to the G-protein signalling machinery (Ref. 29). CLR requires RAMP1 for both its trafficking to the cell surface and binding of CGRP (Ref. 30). Our data indicate that RAMP1 is the functional rate-limiting subunit of the receptor in the nervous system and vascular smooth muscle (Refs 31, 32, 33). The crystal structure of the N-terminal ectodomain of the CGRP receptor has recently confirmed that a heterodimer of CLR and RAMP1 forms a CGRP binding pocket and that the clinically effective CGRP receptor antagonists block this peptide-binding cleft (Ref. 34). The observed 1:1 heterodimer is consistent with a crosslinking study of full-length receptors (Ref. 35). By contrast, bimolecular fluorescence complementation indicated that the CGRP receptor contains two CLRs with only one RAMP1 (Ref. 36). The possibility that the CGRP receptor can also exist as a tetramer of two CLRs and two RAMP1 proteins with two ligand-binding sites is consistent with our data demonstrating that elevation of RAMP1 levels shifts the Hill coefficient of receptor activation from 0.9 to 2.6, which indicates RAMP1-induced positive cooperativity (Ref. 33).
Figure 1. CGRP receptor in migraine.
Schematic of the CGRP receptor complex composed of CLR, RAMP1 and RCP. Redrawn from Ref. 186 with permission. Abbreviations: CGRP; calcitonin gene-related peptide; CLR, calcitonin-like receptor; RAMP1, receptor activity-modifying protein 1; RCP, receptor component protein.
In this review, we will first discuss the evidence supporting a role for CGRP in migraine, and then discuss two anatomically distinct mechanisms of CGRP action at peripheral and central sites that might contribute to migraine.
CGRP has a key role in migraine
Although a full understanding of the neural mechanism of migraine remains elusive, there has been a convergence of basic and clinical evidence demonstrating that CGRP is a key molecular player (Ref. 37). Several clinical studies have identified a role for CGRP in migraine. Over 20 years ago, it was reported that plasma CGRP levels are increased during migraine (Refs 38, 39, 40, 41), although more recent studies have called this into question (Refs 42, 43). Elevated CGRP has also been reported in the saliva of migraineurs (Refs 44, 45). Remarkably, injection of CGRP induced a delayed, migraine-like headache in 57–75% of migraineurs with and without aura (Refs 46, 47, 48). Because CGRP did not have this effect on healthy controls, it suggests that migraineurs have increased sensitivity to CGRP. CGRP infusion also causes aura in a portion of patients who suffer from migraine with aura (Ref. 46). However, as noted by the authors, the aura episodes might be due to stress from the CGRP infusion procedure and further investigation is warranted. In contrast to CGRP actions on common migraine patients, administration of CGRP elicited migraine-like headaches in only 9–22% of patients with familial hemiplegic migraine (FHM), which was statistically not different from controls (0–10%) (Refs 49, 50). Mutations that could lead to changes in brain excitability have been identified for several forms of FHM (Refs 51, 52, 53) and will not be reviewed here. Whether the differences in CGRP susceptibility between common migraine and FHM patients indicate qualitative or quantitative differences in underlying pathways is open to debate and will probably require studies with larger populations. Certainly, for typical migraines, blocking CGRP release and receptor activity are useful therapeutic strategies. This was first shown by triptan drugs that restored CGRP levels to baseline coincident with pain relief (Ref. 41, 54). The CGRP receptor antagonists olcegepant and telcagepant are clearly effective antimigraine drugs (Refs 55, 56, 57). Unfortunately, in spite of its promising efficacy in several Phase III trials for acute migraine treatment, clinical development of telcagepant has recently been discontinued, presumably because of signs of liver toxicity from a prophylaxis clinical trial (Refs 58, 59).
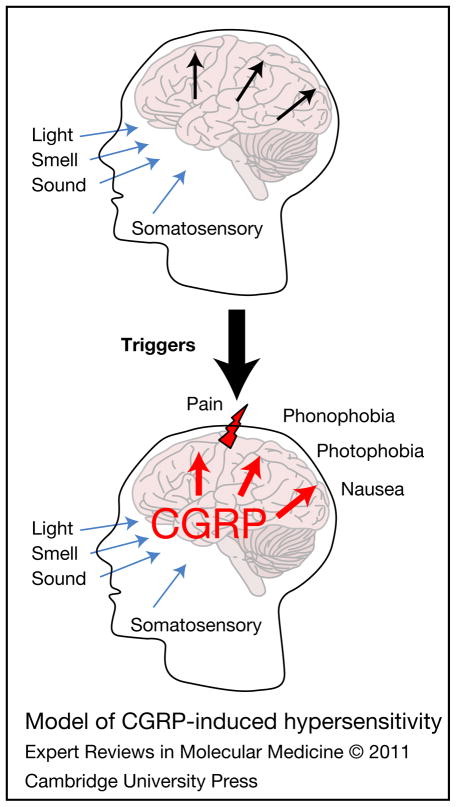
As a neuromodulator, CGRP could potentially increase synaptic transmission (for reviews, see Refs 60, 61). In the spinal cord dorsal horn, CGRP receptors colocalise with AMPA-type glutamate receptors on postsynaptic neurons. Pretreatment with CGRP increased the firing frequency of these neurons in response to AMPA, an effect that can be blocked by the peptide antagonist CGRP 8–37 (Refs 62, 63). Consequently, when CGRP levels are elevated in a susceptible individual, we hypothesise that there could be an amplification of otherwise ordinary sensory input to beyond a pain threshold (Fig. 2).
Figure 2. Model of calcitonin gene-related peptide (CGRP)-induced hypersensitivity.
Under normal conditions (top), CGRP levels are relatively low, leading to normal neurotransmission and proper filtering of sensory input. Migraine triggers initiate a transition to increased CGRP levels (bottom). The elevated CGRP levels increase synaptic transmission in the hypersensitive migraine brain. As a result, increased perception of sensory inputs is registered in the cortex as painful stimuli. Adapted from Ref. 60.
Although it is evident that CGRP has a role in nociceptive transmission, migraine is clearly a multifactorial disorder with a host of genes contributing to migraine susceptibility. For example, not all patients respond to CGRP receptor antagonists. This suggests the involvement of other contributing factors. Of course, this does not rule out CGRP involvement in the nonresponder population, just as one cannot conclude from triptan nonresponders that 5-HT1 receptors are not involved in migraine. Likewise, genetic mapping studies have failed to associate migraine with variations in the CGRP gene (Ref. 64). Similarly, a genome-wide association study has not implicated CGRP or CGRP receptor genes (Ref. 65). Furthermore, infusion of other chemicals (glyceryl trinitrate, histamine, pituitary adenylate cyclase-activating peptide) can trigger delayed migraine-like headache in migraineurs, in a manner similar to CGRP (Refs 66, 67, 68, 69). Accordingly, CGRP should be considered as one factor (among possibly many) that contributes to migraine.
Within the context of migraine, it is a reasonable speculation that CGRP acts at several steps in a cascade from the trigeminal nerve to the CNS. CGRP is released from trigeminal ganglion neurons both peripherally at the dura and centrally in the spinal trigeminal nucleus (Ref. 70). Within the CNS, both CGRP and CGRP receptors are present in many areas implicated in the pathogenesis of migraine. In this review, we will discuss evidence that CGRP could contribute to migraine by both peripheral and central mechanisms.
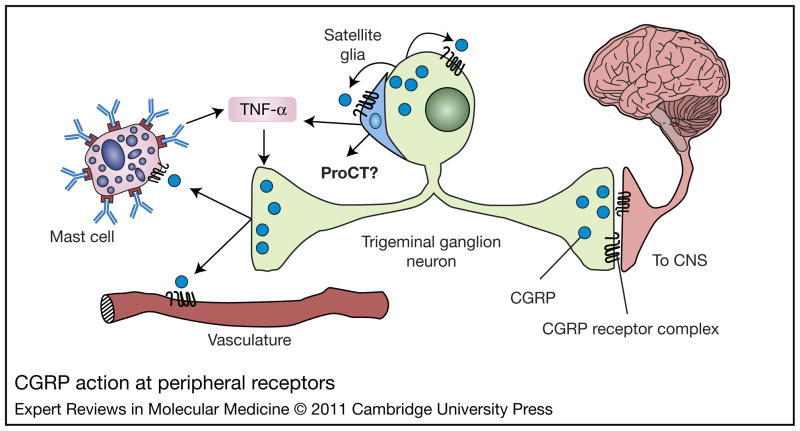
Peripheral actions of CGRP: neurogenic inflammation
Perivascular release of CGRP from the trigeminal nerve induces vasodilation and dural mast cell degranulation, which both contribute to neurogenic inflammation. Neurogenic inflammation describes a sterile, inflammatory event that occurs as a result of sensory nerve activation and is characterised by vasodilation, plasma protein extravasation, and release of proinflammatory and inflammatory molecules from resident mast cells (Ref. 71). Vasodilation is due to CGRP action on vascular smooth muscle (Ref. 72). Extravasation is caused by substance P, which is often co-released with CGRP. The inflammatory cascade can be triggered by CGRP actions on dura-resident mast cells and satellite glial cells of the trigeminal ganglion. CGRP actions at these peripheral sites are highlighted in Figure 3.
Figure 3. CGRP action at peripheral receptors.
CGRP triggers an inflammatory cascade at the periphery. Inflammatory mediators released from mast cells sensitise sensory neurons and promote vascular permeability. Satellite glia influence the local microenvironment within the ganglia by releasing proinflammatory mediators such as tumour necrosis factor α (TNF-α), which can act on trigeminal neurons to increase CGRP synthesis and secretion, setting up a positive-feedback loop, which along with direct actions mediated by CGRP on a subset of trigeminal neurons might contribute to the extended duration of migraine. Satellite glia might also release proCT, which could also activate CGRP receptors.
Despite the fact that peripheral contributions to migraine have fallen from favour in recent years (for a review see Ref. 60), the story is far from complete. Indeed, the role of cerebrovascular dilation remains controversial (Refs 48, 73, 74). The overall role of neurogenic inflammation has been discounted in large part owing to the failure of substance P receptor antagonists in migraine clinical trials (Refs 60, 75). Furthermore, animal studies strongly supported a central, not peripheral, action of CGRP (Ref. 26) and CGRP receptor antagonists (Ref. 76). Although open to interpretation, these results could be confounded by mast cell degranulation during the experimental procedure. In addition, the studies do not rule out peripheral contributions. Finally, the relatively high level of CGRP receptor antagonists required for clinical efficacy compared with in vitro predictions has been used as an argument for a central site of action beyond the blood–brain barrier (Ref. 77). However, this comparison has recently been called into question (Ref. 78) and the fact that peripheral administration of CGRP described above is able to induce migraine-like headaches has helped keep the debate open. In this context, a judicious re-evaluation of peripheral CGRP actions in neurogenic inflammation at mast cells and glia is warranted.
Mast cell degranulation
Mast cells are bone-marrow-derived cells (Refs 79, 80) that are involved in normal immune responses and allergic reactions (Ref. 81). Mast cells can be activated by direct injury (chemical or physical), crosslinking with immunoglobulin E, or activated complement proteins (Ref. 82). Several diseases that involve mast cells are associated with increased incidence of migraines, including allergies, asthma, eczema, interstitial cystitis and irritable bowel syndrome (Refs 83, 84, 85).
The involvement of mast cells in migraine has been speculated on for many years (Ref. 86), and there are several lines of evidence that support their involvement. Sinus headache, which is not an officially recognised condition, co-occurs with sinusitis symptoms. Indeed, 90% of these headaches meet the diagnostic guidelines for migraine but are misdiagnosed (Ref. 87). Sinusitis is commonly a result of an allergic response, which is mediated by mast cells (Ref. 88). The population of mast cells most likely to contribute to the pathogenesis of migraine are dura-resident mast cells. A distinguishing feature of these cells is the ability of CGRP to degranulate them, which differs from other mast cells that require substance P (Refs 9, 16). CGRP receptors are clearly present on mast cells in the dura mater (Ref. 21). These mast cells lie adjacent to both sensory neurons and the vasculature (Ref. 89). Mast cell activation and degranulation lead to the release of several neuroactive and vasoactive substances. These include bradykinin, histamine, prostaglandins, tumour necrosis factor α (TNF-α), vascular endothelial growth factor and serotonin (Ref. 17). The release of these inflammatory and proinflammatory agents can potentially generate a positive-feedback loop onto sensory neurons because they trigger CGRP release. An inflammatory soup (low pH, bradykinin, 5-HT, prostaglandin E2, histamine) (Ref. 90) induces CGRP secretion from cultured trigeminal sensory neurons (Ref. 91). This elevated secretion is predicted to be long lasting because cytokines also activate CGRP gene transcription (Ref. 92). Importantly, an inflammatory response triggered by chemical induction of mast cell degranulation sensitises primary sensory neurons that innervate the dura of the meninges (Ref 93). Mechanosensitive neurons innervating the dura show increased activity shortly after degranulation and remain hyperactive for hours. It is believed that these excitable neurons have a key role in promoting intracranial migraine pain (Refs 1, 94, 95). Increased activation of these primary afferent neurons also resulted in increased activity of neurons in the TNc, as measured by c-Fos immunoreactivity (Ref. 93). Further evidence for mast cell actions being mediated by peripheral nociceptors is that sumatriptan, an antimigraine medication that inhibits CGRP release from these nociceptors, can block the effect of mast cell degranulation on the TNc (Ref. 93).
At least one agent, histamine, released from mast cells has been directly implicated in migraine. Plasma histamine levels have been reported to be elevated in migraineurs, with a further increase during a migraine attack (Refs 96, 97, 98). Inhalation or injection of histamine causes migraine-like headaches in migraineurs, but only mild headaches in nonmigraineurs (Refs 99, 100). In a revealing experiment, Messlinger and colleagues identified a subpopulation of meningeal afferent fibres that were activated by low doses of histamine that were comparable with those predicted to occur on mast cell degranulation (Ref. 101). However, although an H1 antagonist was able to block histamine-induced migraine, it was unable to block nitric-oxide-induced migraine (Ref. 102). Antihistamines are effective in a subset of migraine patients (Refs 103, 104, 105). Consequently, although the story is incomplete, cumulative contributions from histamine and other agents released on mast cell degranulation might contribute to the migraine state.
Rather than focusing on single agents, stabilising mast cells and blocking the effects of their proinflammatory contents might be beneficial. For example, nonsteroidal anti-inflammatory drugs are one of the most commonly used treatments for migraine (Refs 106, 107). In a clinical experiment using migraineurs with known food triggers, a mast-cell-stabilising drug was effective in preventing migraine symptoms after exposure to trigger foods (Ref. 108). Montelukast is a leukotriene receptor antagonist with demonstrated efficacy in two small, open label trials for migraine prophylaxis (Refs 109, 110). This drug was not successful in a larger, double-blind study (Ref. 111); however, it could be that only a subset of migraines involves an allergic process. Recent evidence shows that amitriptyline and prochlorperazine, which are successful for migraine prophylaxis, inhibit proinflammatory mediator release from mast cells in vitro (Ref. 112).
Satellite glial activation
In the trigeminal ganglion, satellite glia are intimately associated with neuronal cell bodies and are able to influence the local microenvironment similarly to glial functions in the CNS (Refs 113, 114). Recently, satellite glia have unexpectedly been shown to behave much like mast cells in response to CGRP. Neuronal cell bodies contain the necessary machinery for releasing neuropeptides, so a mechanism for release of CGRP within the ganglion exists. Trigeminal ganglion preparations have also been shown to release CGRP in response to a combination of nitric oxide donors and inflammatory stimuli (Ref. 115). CGRP treatment of satellite glia increases proinflammatory cytokine release and actions that can sensitise sensory neurons (Refs 116, 117, 118, 119). This is a direct response because satellite glia contain functional CGRP receptors (Refs 8, 21). In addition to cytokine release, CGRP triggers additional inflammatory gene expression changes in glia in vitro (Ref. 116). These observations are consistent with evidence for neuron–glia interactions in inflammatory and pain conditions (Refs 120, 121). As with the actions of CGRP on mast cells, it has been proposed that CGRP could have a role in activation or sensitisation of the sensory neurons by satellite glia (Refs 117, 118). The further synthesis and release of CGRP from the neurons would then generate a positive-feedback loop that would enhance and sustain the inflammatory state and neuronal sensitisation (Fig. 3). Indeed, we observed elevated CGRP levels in the cerebrospinal fluid of transgenic mice sensitised to CGRP actions in the nervous system (Ref. 122). A similar elevation of CGRP mRNA levels was observed in some brain regions (Ref. 123). These observations are consistent with a CGRP-mediated positive-feedback loop in cell cultures that stimulates further CGRP synthesis (Ref. 33).
Glial production of procalcitonin
The positive-feedback loop might include not only CGRP, but also an alternative splice product from CALCA, the gene from which CGRP is transcribed (Fig. 3). CALCA also encodes the hormone calcitonin (CT) (Ref. 124). CT expression is normally restricted to parafollicular C-cells of the thyroid and regulates blood Ca2+ levels primarily by acting at its receptor on osteoclasts. CT is a cleavage product from a larger precursor peptide known as proCT (Ref. 125). Normally, neither CGRP nor CT is expressed in satellite glia because of repressive epigenetic marks (Ref. 126). However, whole organ culture of the trigeminal ganglion results in ectopic CGRP expression in satellite glia, presumably as a result of inflammatory signals (Refs 127, 128). Organ culture also increases immunoreactive proCT in satellite glia. ProCT levels are increased in many inflammatory conditions, as discussed below.
Circulating levels of proCT are generally quite low in healthy individuals. Serum proCT levels have been reported to increase several thousand times during sepsis, a severe inflammatory response that generally occurs in response to bacterial infection. Elevation of proCT in autoimmune diseases that have an inflammatory component, such as lupus and rheumatoid arthritis, has also been reported (Ref. 129). Although the exact mechanism of action of proCT under these conditions is not well understood, proCT might serve as a valuable biomarker for inflammation. Under some conditions, proCT might have a wider role. In animal models of sepsis, exogenous administration of proCT reduced survival whereas blocking endogenous proCT using a neutralising antibody increased survival (Ref. 130).
A recent study reported increased serum proCT in migraineurs during attacks when compared with baseline levels (Ref. 131). Although the levels during migraine are much lower than those seen in sepsis, the idea that proCT and inflammation are linked under other conditions suggests that the meningeal sterile inflammation believed to occur in migraine could lead to local release of proCT. As mentioned previously, whole-organ tissue culture, which is associated with inflammation, allows proCT expression in satellite glia (Ref. 128). Expression of proCT will probably require epigenetic changes because promoter methylation normally represses the CALCA gene and DNA demethylation is sufficient to allow proCT expression in cultured trigeminal ganglia glia (Ref. 126). Increased proCT might have a functional consequence in migraine because it has been shown to act as a partial agonist at CGRP receptors (Ref. 132). Further study of the significance of proCT in migraine is merited.
Cortical spreading depression as a trigger of peripheral CGRP release
Cortical spreading depression (CSD) occurs when a focal stimulation of the cerebral cortex results in a slowly propagating wave (2–6 mm/min) of neuron and glial hyperactivity followed by a prolonged suppression in neuronal activity. Previous work has associated changes in cerebral blood flow with aura, a transient, mostly visual disturbance that precedes the headache in a subset of migraine patients (Refs 133, 134, 135). Although other evidence argues against the connection between CSD and migraine (Refs 136, 137, 138), it seems reasonable that CSD might be at least one type of migraine trigger.
CSD appears to involve CGRP actions at two points. First, there is evidence that CGRP has a role in the initial hyperaemia during CSD because CGRP receptor antagonism blocks transient pial artery dilation in animal models of CSD (Refs 139, 140). This suggests that there must be local release of CGRP in the meninges, which could then serve to sensitise local sensory neurons. CGRP release in the meninges would then lead to mast cell degranulation and release of inflammatory mediators (Ref. 16). A recent report has shown that CGRP also has modest proinflammatory actions on cultured cortical astrocytes, analogous to actions on satellite glia (Ref. 119). Although experimental CSD in cats does not increase CGRP outflow in jugular blood (Ref. 141), this does not rule out local increases in CGRP in the cortex.
Studies by Moskowitz and colleagues demonstrated that experimental CSD could activate trigeminal afferents in cortical meninges (Ref. 142). This activation is predicted to be mediated by excitatory agents released from neurons and glia. In a detailed study of meningeal nociceptor activity after experimentally induced CSD in rats, Burstein and colleagues recently demonstrated remarkably long-lasting activation of these neurons (Refs 143, 144). Interestingly, there was a marked delay before the activation. Identification of the reason for this delay should be informative. Other animal models have demonstrated CSD-dependent increases in c-Fos expression in the TNc (Refs 145, 146) and meningeal plasma extravasation (Refs 142, 147). Additional recent data show that experimental CSD in rats leads to delayed activation of peripheral meningeal nociceptors and second-order neurons of the trigeminovascular system (Refs 143, 144). These results are consistent with observations following systemic mast cell degranulation (Ref. 93) and dural application of inflammatory soup or TNF-α (Refs 148, 149). An independent corticotrigeminal pathway has recently been shown to modulate activity initiated by the meningeal nociceptors in spinal trigeminal nucleus neurons (Ref. 150). In this regard, a recent study by Porreca’s group has shown that dural inflammation can trigger CGRP-dependent allodynia that is modulated by descending facilitation from the rostral ventromedial medulla (Ref. 151). Whether there is a convergent regulation by these multiple pathways remains to be determined. In addition, if the reported induction of aura by peripheral injection of CGRP is confirmed (Ref. 46), this raises the possibility that CGRP may also have a role upstream of CSD.
Possible central actions of CGRP: modulation of light sensitivity
CGRP and its receptor are widely distributed across the CNS (Refs 4, 152, 153, 154). As such, CGRP has been suggested in a number of centrally mediated activities that might be relevant to migraine, including anxiogenesis, stress responses, nociception and light aversion (Refs 3, 4, 5, 6). We will focus on light aversion because recent studies have laid out an anatomical pathway for photophobia that is well positioned to be modulated by CGRP (Ref. 155).
Before discussing potential contributions from CGRP to photophobia, it is necessary to first define different forms of photophobia. Recently, three types of photophobia have been defined: ocular discomfort caused by exposure to light, exacerbation of headache by light and heightened perception of light (Ref. 156). The first involves the trigeminal nerve. Light-induced ocular pain has been studied by exposing rats to very bright light, which resulted in activation of secondary neurons in the spinal trigeminal nucleus, presumably in response to vasodilation in the eye (Ref. 157). A connection to migraine is intriguing, but remains to be established. Most pertinent to this review is the exacerbation of headache by light that is experienced by up to 80% of migraineurs (Refs 158, 159).
Convergence of trigeminal and retinal signals in the thalamus
Photophobia in migraineurs who lack image-forming vision but retain the ability to detect light suggests that a nonvisual pathway is involved in the potentiation of migraine pain by light (Ref. 155). This observation implicates the intrinsically photosensitive retinal ganglion cells (ipRGCs), which contain the photopigment melanopsin and are involved in nonvisual responses to light, such as circadian entrainment (Ref. 160). These cells are intact in legally blind individuals that maintain the ability to detect light in the absence of functional rods and cones. Some ipRGCs terminate in posterior thalamic nuclei (Po) that also respond to dura stimulation (Ref. 155). These dura-sensitive neurons in the Po are modulated by light-driven activation of ipRGCs. This convergence of light and dural signals suggests an integrative role for the posterior thalamus in light-induced migraine pain. It is also consistent with neuroimaging studies in patients that have shown thalamic activation during migraine (Ref. 161). An intriguing observation was the variability in the stimulus-response time for light-induced activation in the Po. Whereas some units responded rapidly (within several milliseconds) to light stimulation, a significant delay lasting several hundred seconds was detected in other units (Ref. 155). This delay suggests that the thalamic pathway is part of a modulated network. We speculate that CGRP might be involved in this modulation.
Both CGRP and its receptor have been identified in the nociceptive pathway from the trigeminal nerve to the thalamus (Ref. 3). As described previously, CGRP is in about 35–50% of the first-order trigeminal ganglia neurons, and the receptor is in a subset of these CGRP-containing neurons. In culture, most if not all trigeminal ganglia neurons express both CGRP and receptor proteins, suggesting that there is dynamic plasticity in their regulation, possibly because of upregulation on nerve injury (Ref. 33). CGRP receptors, but not CGRP, have also been identified in the satellite glia of the ganglia and possibly nonmyelinating Schwann cells (Ref. 8). Second-order nociceptive neurons in the TNc contain CGRP receptors (Ref. 162). These neurons do not synthesise CGRP. Trigeminovascular input is then relayed to third-order neurons in the posterior thalamus (Ref. 163). The predominant CGRP-immunoreactive cell bodies in the thalamus are found in the subparafascicular nucleus, posterior thalamic nuclear group, peripeduncular nucleus and areas ventromedial to the posterior thalamic group (Ref. 164). Although most light-sensitive neurons in the dura were found near the dorsal edge of the posterior thalamic nuclear group (Ref. 155), others were scattered in nearby posterior nuclei, including the ventroposteromedial thalamic nucleus that contains CGRP receptors.
CGRP actions in the ventroposteromedial thalamus have recently been brought to the forefront by identification of CGRP receptors on neurons responsive to nociceptive trigeminovascular input (Ref. 165). CGRP receptor antagonists can block this nociceptive stimulation (Ref. 165). Also within the thalamus, the presence of CGRP in neurons of the subparafascicular thalamus and other posterior intralaminar thalamic nuclei is especially intriguing. These CGRP-containing neurons, as well as neurons at the caudal extent of the thalamic posterior group (Ref. 166), relay and integrate somatosensory and nociceptive stimuli from ascending pathways (Ref. 167). CGRP fibres from this region that project to the amygdala have been suggested to have a role in autonomic and behavioural responses to acoustic and somatosensory stimuli (Ref. 168). Other studies have shown that neurons in these regions can activate the hypothalamic–pituitary–adrenal axis in response to auditory stress (Ref. 169). Further studies suggest that convergence of auditory and nociception inputs to the CGRP-positive lateral parvocellular subparafascicular thalamic nucleus is important for conditioned auditory and visual fear responses (Refs 170, 171). These anatomical data show that CGRP and its receptor are in the appropriate neighbourhood to modulate trigeminovascular and photic activation of thalamic neurons.
Potential nonthalamic contributions
While we have focused on CGRP actions in the thalamus, a more comprehensive and cautious analysis must include the possibility that CGRP could also modulate photophobia by actions in other brain regions. CGRP-immunoreactive cell bodies and fibres are prevalent in nuclei of the hypothalamus, ventral tegmental area, selected brainstem nuclei (Ref. 164), periaqueductal grey (PAG) (Ref. 172) and cerebellum (Refs 152, 173). Likewise, CGRP-binding sites have been mapped to many regions of the CNS, including the cortex, limbic system (amygdala, nucleus accumbens, hypothalamus) and brainstem (PAG, medulla, pons) (Refs 4, 153, 154). Some of these regions also receive projections from the ipRGC. The function of most of the major ipRGC projections, such as the suprachiasmatic nucleus in circadian rhythms, has been well established. However, there are other relatively low abundance projections that have been less studied (Ref. 174). These include ipRGC fibres to the medial nucleus of the amygdala, bed nucleus stria terminalis (BSTN) and PAG, which are regions that contain CGRP and its receptor.
The ipRGC inputs to the extended amygdala (medial nucleus and BSTN) are of particular interest (Ref. 174). The amygdala is known to relay nociceptive information (Ref. 175), and the medial amygdala is a convergence and integration site of photic and olfactory stimuli that modulate reproductive behaviour (Refs 176, 177, 178). There are CGRP receptors in the centromedial nuclear area of the amygdala and extended regions, such as the BSTN. Injection of CGRP into the central nucleus and BSTN causes fear behaviour in rats (Ref. 179), which demonstrates that CGRP can have an anxiogenic role in the extended amygdala. The CGRP in the amygdala is primarily from fibres projecting from the thalamus (Ref. 180). There is dense CGRP innervation from the posterior thalamus and parabrachial nuclei to the central and, to a lesser extent, the medial nucleus of the amygdala (Ref. 180). Specifically, CGRP-labelled neurons were traced from the subparafascicular, lateral subparafascicular and posterior intralaminar nuclei of the thalamus to the amygdala (Ref. 168). Of particular note, the subparafascicular and lateral subparafascicular nuclei primarily projected to the medial amygdala and the amygdalostriatal transition area, which are areas found to contain ipRGC projections. Interestingly, the authors concluded that these CGRP-containing fibres mediate conditioned autonomic and behavioural responses to acoustic stimuli or somatosensory stimuli (Ref. 168). Whether these fibres project from any of the dural-activated thalamic neurons identified by Burstein and colleagues remains to be tested.
Similarly, the presence of CGRP-containing fibres and receptors in the PAG, which contains ipRGC fibres, should also be considered as potential sites of CGRP action in photophobia behaviour. CGRP-immunoreactive cell bodies are found in the PAG (Ref. 172), which is part of the descending pain inhibitory system (Ref. 181) and cooperates with the amygdala in processing fear and anxiety (Ref. 182).
Light-aversive behaviour of a CGRP-sensitised mouse model
Support for a role for central actions of CGRP in photophobia has been provided by light-aversion studies in genetically engineered mice. Although relatively unexplored, light aversion has been a useful parameter for objective light sensitivity in animal models. Differential light sensitivity between different strains of inbred mice has been shown, indicating a possible inherent sensitivity to light (Ref. 183). Light aversion was correlated to photophobia in nestin/hRAMP1 transgenic mice, a model of CGRP sensitivity (Ref. 184). The nestin/hRAMP1 mice are genetically sensitised to CGRP by nervous system overexpression of human RAMP1, a component of the CGRP receptor (described above) (Ref. 33). Compared with control littermates, nestin/hRAMP1 mice spend less time in the light after intracerebroventricular injection of CGRP, suggesting that light causes discomfort in these animals under these conditions (Refs 122, 185). However, the central administration results do not conclusively rule out a peripheral effect and the results must be interpreted with caution because it is very likely that some injected CGRP could leak at the site of injection through the meninges. Nonetheless, the ability to genetically restrict hRAMP1 expression to discrete neuronal regions in this mouse model provides a valuable tool for identifying sites of CGRP action (Ref. 186). Whether CGRP actions in the thalamus amygdala, or other sites contribute to photophobia will be an interesting area of future study.
Research in progress
Basic and clinical researchers continue to offer complementary approaches that are improving our understanding of the role of CGRP in the complex pathogenesis of migraine. Even though the story is far from complete, we propose that activation of a peripheral inflammatory response by CGRP acting in concert with central modulation by CGRP contributes to migraine pain.
Several new CGRP-based therapies are currently under development for the treatment of migraine. New small-molecule CGRP receptor antagonists have completed Phase II clinical trials, both with positive results (Refs 187, 188). Monoclonal antibodies intended to prevent CGRP from engaging its receptor are being pursued as a path towards long-term prophylactic therapy (Refs 189, 190). In preclinical studies, these antibodies were able to inhibit neurogenic inflammation without affecting cardiovascular parameters (Ref. 190). If effective in migraine therapy, systemic delivery of antibodies will highlight the importance of peripheral CGRP actions. Additional antimigraine therapies are also being developed targeting glutamate receptors, which as mentioned above could potentially be modulated by CGRP (Refs 191, 192).
Future research will probably explore other molecules that might contribute to the pathogenesis of migraine, such as histamine and proCT. It seems likely that experiments will continue to examine the relationship between the nervous and immune systems, especially the interplay of CGRP with the immune system. The identification of sites of CGRP action in the CNS should lead to more insights and improved therapeutics for migraine. In this way, increased understanding of the impact of CGRP on the trigeminovascular system will continue to propel us closer to successful therapeutics for migraine.
Acknowledgments
We gratefully acknowledge Rami Burstein for very helpful guidance and suggestions, and our peer reviewers for insightful advice on the article. This work was supported by the National Institutes of Health (DE016511 and NS075599) and a Ruth L. Kirschstein NRSA fellowship (NS074728) (to A.C.R.).
References
- 1.Pietrobon D, Striessnig J. Neurobiology of migraine. Nature Reviews Neuroscience. 2003;4:386–398. doi: 10.1038/nrn1102. [DOI] [PubMed] [Google Scholar]
- 2.Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 3.Wimalawansa SJ. Calcitonin gene-related peptide and its receptors: molecular genetics, physiology, pathophysiology, and therapeutic potentials. Endocrine Reviews. 1996;17:533–585. doi: 10.1210/edrv-17-5-533. [DOI] [PubMed] [Google Scholar]
- 4.van Rossum D, Hanisch UK, Quirion R. Neuroanatomical localization, pharmacological characterization and functions of CGRP, related peptides and their receptors. Neuroscience & Biobehavioral Reviews. 1997;21:649–678. doi: 10.1016/s0149-7634(96)00023-1. [DOI] [PubMed] [Google Scholar]
- 5.Russo AF, Dickerson IM. CGRP: A multifunctional neuropeptide. In: Lajtha A, editor. Handboook Neurochem Molec Neurobiol. 3. Springer; New York, NY: 2006. pp. 391–426. [Google Scholar]
- 6.Recober A, Russo AF. Calcitonin gene-related peptide: an update on the biology. Current Opinion in Neurology. 2009;22:241–246. doi: 10.1097/wco.0b013e32832b2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tajti J, et al. Messenger molecules and receptor mRNA in the human trigeminal ganglion. Journal of the Autonomic Nervous System. 1999;76:176–183. doi: 10.1016/s0165-1838(99)00024-7. [DOI] [PubMed] [Google Scholar]
- 8.Eftekhari S, et al. Differential distribution of calcitonin gene-related peptide and its receptor components in the human trigeminal ganglion. Neuroscience. 2010;169:683–696. doi: 10.1016/j.neuroscience.2010.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Messlinger K. Migraine: where and how does the pain originate? Experimental Brain Research. 2009;196:179–193. doi: 10.1007/s00221-009-1756-y. [DOI] [PubMed] [Google Scholar]
- 10.Messlinger K, et al. Innervation of the dura mater encephali of cat and rat: ultrastructure and calcitonin gene-related peptide-like and substance P-like immunoreactivity. Anatomy and Embryology (Berlin) 1993;188:219–237. doi: 10.1007/BF00188214. [DOI] [PubMed] [Google Scholar]
- 11.Liu Y, Broman J, Edvinsson L. Central projections of the sensory innervation of the rat middle meningeal artery. Brain Research. 2008;1208:103–110. doi: 10.1016/j.brainres.2008.02.078. [DOI] [PubMed] [Google Scholar]
- 12.Brain SD, Grant AD. Vascular actions of calcitonin gene-related peptide and adrenomedullin. Physiological Reviews. 2004;84:903–934. doi: 10.1152/physrev.00037.2003. [DOI] [PubMed] [Google Scholar]
- 13.Edvinsson L, et al. Effect of the CGRP receptor antagonist BIBN4096BS in human cerebral, coronary and omental arteries and in SK-N-MC cells. European Journal of Pharmacology. 2002;434:49–53. doi: 10.1016/s0014-2999(01)01532-1. [DOI] [PubMed] [Google Scholar]
- 14.Moreno MJ, et al. Efficacy of the non-peptide CGRP receptor antagonist BIBN4096BS in blocking CGRP-induced dilations in human and bovine cerebral arteries: potential implications in acute migraine treatment. Neuropharmacology. 2002;42:568–576. doi: 10.1016/s0028-3908(02)00008-4. [DOI] [PubMed] [Google Scholar]
- 15.Oliver KR, et al. Immunohistochemical localization of calcitonin receptor-like receptor and receptor activity-modifying proteins in the human cerebral vasculature. Journal of Cerebral Blood Flow Metabolism. 2002;22:620–629. doi: 10.1097/00004647-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Ottosson A, Edvinsson L. Release of histamine from dural mast cells by substance P and calcitonin gene-related peptide. Cephalalgia. 1997;17:166–174. doi: 10.1046/j.1468-2982.1997.1703166.x. [DOI] [PubMed] [Google Scholar]
- 17.Theoharides TC, et al. The role of mast cells in migraine pathophysiology. Brain Research and Brain Research Reviews. 2005;49:65–76. doi: 10.1016/j.brainresrev.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 18.Skofitsch G, Jacobowitz DM. Calcitonin gene-related peptide coexists with substance P in capsaicin sensitive neurons and sensory ganglia of the rat. Peptides. 1985;6:747–754. doi: 10.1016/0196-9781(85)90179-2. [DOI] [PubMed] [Google Scholar]
- 19.Lundberg JM, et al. Co-existence of substance P and calcitonin gene-related peptide-like immunoreactivities in sensory nerves in relation to cardiovascular and bronchoconstrictor effects of capsaicin. European Journal of Pharmacology. 1985;108:315–319. doi: 10.1016/0014-2999(85)90456-x. [DOI] [PubMed] [Google Scholar]
- 20.Lee Y, et al. Distribution of calcitonin gene-related peptide in the rat peripheral nervous system with reference to its coexistence with substance P. Neuroscience. 1985;15:1227–1237. doi: 10.1016/0306-4522(85)90265-9. [DOI] [PubMed] [Google Scholar]
- 21.Lennerz JK, et al. Calcitonin receptor-like receptor (CLR), receptor activity-modifying protein 1 (RAMP1), and calcitonin gene-related peptide (CGRP) immunoreactivity in the rat trigeminovascular system: differences between peripheral and central CGRP receptor distribution. Journal of Comparative Neurology. 2008;507:1277–1299. doi: 10.1002/cne.21607. [DOI] [PubMed] [Google Scholar]
- 22.Fischer MJ. Calcitonin gene-related peptide receptor antagonists for migraine. Expert Opinion on Investigational Drugs. 2010;19:815–823. doi: 10.1517/13543784.2010.490829. [DOI] [PubMed] [Google Scholar]
- 23.Marquez de Prado B, Hammond DL, Russo AF. Genetic enhancement of calcitonin gene-related peptide-induced central sensitization to mechanical stimuli in mice. Journal of Pain. 2009;10:992–1000. doi: 10.1016/j.jpain.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Storer RJ, Akerman S, Goadsby PJ. Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. British Journal of Pharmacology. 2004;142:1171–1181. doi: 10.1038/sj.bjp.0705807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fischer MJ, Koulchitsky S, Messlinger K. The nonpeptide calcitonin gene-related peptide receptor antagonist BIBN4096BS lowers the activity of neurons with meningeal input in the rat spinal trigeminal nucleus. Journal of Neuroscience. 2005;25:5877–5883. doi: 10.1523/JNEUROSCI.0869-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Levy D, Burstein R, Strassman AM. Calcitonin gene-related peptide does not excite or sensitize meningeal nociceptors: implications for the pathophysiology of migraine. Annals of Neurology. 2005;58:698–705. doi: 10.1002/ana.20619. [DOI] [PubMed] [Google Scholar]
- 27.Archbold JK, et al. Structural insights into RAMP modification of secretin family G protein-coupled receptors: implications for drug development. Trends in Pharmacological Sciences. 2011;32:591–600. doi: 10.1016/j.tips.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 28.Barwell J, et al. Calcitonin and calcitonin receptor-like receptors: common themes with family B GPCRs? British Journal of Pharmacology. 2011 Jun 7; doi: 10.1111/j.1476–5381.2011.01525.x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Evans BN, et al. CGRP-RCP, a novel protein required for signal transduction at calcitonin gene-related peptide and adrenomedullin receptors. Journal of Biological Chemistry. 2000;275:31438–31443. doi: 10.1074/jbc.M005604200. [DOI] [PubMed] [Google Scholar]
- 30.McLatchie LM, et al. RAMPs regulate the transport and ligand specificity of the calcitonin-receptor-like receptor. Nature. 1998;393:333–339. doi: 10.1038/30666. [DOI] [PubMed] [Google Scholar]
- 31.Zhang Z, Dickerson IM, Russo AF. Calcitonin gene-related peptide receptor activation by receptor activity-modifying protein-1 gene transfer to vascular smooth muscle cells. Endocrinology. 2006;147:1932–1940. doi: 10.1210/en.2005-0918. [DOI] [PubMed] [Google Scholar]
- 32.Russo AF. Ramping it up: RAMP1 and the implications for migraine. Pharmacogenomics. 2007;8:687–690. doi: 10.2217/14622416.8.7.687. [DOI] [PubMed] [Google Scholar]
- 33.Zhang Z, et al. Sensitization of calcitonin gene-related peptide receptors by receptor activity-modifying protein-1 in the trigeminal ganglion. Journal of Neuroscience. 2007;27:2693–2703. doi: 10.1523/JNEUROSCI.4542-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.ter Haar E, et al. Crystal structure of the ectodomain complex of the CGRP receptor, a class-B GPCR, reveals the site of drug antagonism. Structure. 2010;18:1083–1093. doi: 10.1016/j.str.2010.05.014. [DOI] [PubMed] [Google Scholar]
- 35.Hilairet S, et al. Agonist-promoted internalization of a ternary complex between calcitonin receptor-like receptor, receptor activity-modifying protein 1 (RAMP1), and beta-arrestin. Journal of Biological Chemistry. 2001;276:42182–42190. doi: 10.1074/jbc.M107323200. [DOI] [PubMed] [Google Scholar]
- 36.Heroux M, et al. Functional calcitonin gene-related peptide receptors are formed by the asymmetric assembly of a calcitonin receptor-like receptor homo-oligomer and a monomer of receptor activity-modifying protein-1. Journal of Biological Chemistry. 2007;282:31610–31620. doi: 10.1074/jbc.M701790200. [DOI] [PubMed] [Google Scholar]
- 37.Villalon CM, Olesen J. The role of CGRP in the pathophysiology of migraine and efficacy of CGRP receptor antagonists as acute antimigraine drugs. Pharmacology & Therapeutics. 2009;124:309–323. doi: 10.1016/j.pharmthera.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 38.Goadsby PJ, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Annals of Neurology. 1990;28:183–187. doi: 10.1002/ana.410280213. [DOI] [PubMed] [Google Scholar]
- 39.Juhasz G, et al. NO-induced migraine attack: strong increase in plasma calcitonin gene-related peptide (CGRP) concentration and negative correlation with platelet serotonin release. Pain. 2003;106:461–470. doi: 10.1016/j.pain.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 40.Gallai V, et al. Vasoactive peptide levels in the plasma of young migraine patients with and without aura assessed both interictally and ictally. Cephalalgia. 1995;15:384–390. doi: 10.1046/j.1468-2982.1995.1505384.x. [DOI] [PubMed] [Google Scholar]
- 41.Goadsby PJ, Lipton RB, Ferrari MD. Migraine—current understanding and treatment. New England Journal of Medicine. 2002;346:257–270. doi: 10.1056/NEJMra010917. [DOI] [PubMed] [Google Scholar]
- 42.Tvedskov JF, et al. No increase of calcitonin gene-related peptide in jugular blood during migraine. Annals of Neurology. 2005;58:561–568. doi: 10.1002/ana.20605. [DOI] [PubMed] [Google Scholar]
- 43.Tfelt-Hansen P, Le H. Calcitonin gene-related peptide in blood: is it increased in the external jugular vein during migraine and cluster headache? A review. Journal of Headache and Pain. 2009;10:137–143. doi: 10.1007/s10194-009-0112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bellamy JL, Cady RK, Durham PL. Salivary levels of CGRP and VIP in rhinosinusitis and migraine patients. Headache. 2006;46:24–33. doi: 10.1111/j.1526-4610.2006.00294.x. [DOI] [PubMed] [Google Scholar]
- 45.Cady RK, et al. Elevated saliva calcitonin gene-related peptide levels during acute migraine predict therapeutic response to rizatriptan. Headache. 2009;49:1258–1266. doi: 10.1111/j.1526-4610.2009.01523.x. [DOI] [PubMed] [Google Scholar]
- 46.Hansen JM, et al. Calcitonin gene-related peptide triggers migraine-like attacks in patients with migraine with aura. Cephalalgia. 2010;30:1179–1186. doi: 10.1177/0333102410368444. [DOI] [PubMed] [Google Scholar]
- 47.Lassen LH, et al. CGRP may play a causative role in migraine. Cephalalgia. 2002;22:54–61. doi: 10.1046/j.1468-2982.2002.00310.x. [DOI] [PubMed] [Google Scholar]
- 48.Asghar MS, et al. Evidence for a vascular factor in migraine. Annals of Neurology. 2011;69:635–645. doi: 10.1002/ana.22292. [DOI] [PubMed] [Google Scholar]
- 49.Hansen JM, et al. Familial hemiplegic migraine type 2 does not share hypersensitivity to nitric oxide with common types of migraine. Cephalalgia. 2008;28:367–375. doi: 10.1111/j.1468-2982.2008.01542.x. [DOI] [PubMed] [Google Scholar]
- 50.Hansen JM, et al. Calcitonin gene-related peptide does not cause migraine attacks in patients with familial hemiplegic migraine. Headache. 2011;51:544–553. doi: 10.1111/j.1526-4610.2011.01861.x. [DOI] [PubMed] [Google Scholar]
- 51.Ophoff RA, et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell. 1996;87:543–552. doi: 10.1016/s0092-8674(00)81373-2. [DOI] [PubMed] [Google Scholar]
- 52.De Fusco M, et al. Haploinsufficiency of ATP1A2 encoding the Na+/K+ pump alpha2 subunit associated with familial hemiplegic migraine type 2. Nature Genetics. 2003;33:192–196. doi: 10.1038/ng1081. [DOI] [PubMed] [Google Scholar]
- 53.Dichgans M, et al. Mutation in the neuronal voltage-gated sodium channel SCN1A in familial hemiplegic migraine. Lancet. 2005;366:371–377. doi: 10.1016/S0140-6736(05)66786-4. [DOI] [PubMed] [Google Scholar]
- 54.Juhasz G, et al. Sumatriptan causes parallel decrease in plasma calcitonin gene-related peptide (CGRP) concentration and migraine headache during nitroglycerin induced migraine attack. Cephalalgia. 2005;25:179–183. doi: 10.1111/j.1468-2982.2006.01133_1.x. [DOI] [PubMed] [Google Scholar]
- 55.Olesen J, et al. Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. New England Journal of Medicine. 2004;350:1104–1110. doi: 10.1056/NEJMoa030505. [DOI] [PubMed] [Google Scholar]
- 56.Connor KM, et al. Randomized, controlled trial of telcagepant for the acute treatment of migraine. Neurology. 2009;73:970–977. doi: 10.1212/WNL.0b013e3181b87942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ho TW, et al. Randomized controlled trial of anoral CGRP receptor antagonist, MK-0974, in acute treatment of migraine. Neurology. 2008;70:1304–1312. doi: 10.1212/01.WNL.0000286940.29755.61. [DOI] [PubMed] [Google Scholar]
- 58.MerckReport. Merck announces second quarter 2011 financial results. 2011 http://www.fiercebiotech.com/press-releases/merck-announces-second-quarter-2011-financial-results-0.
- 59.ClinicalTrials.gov. MK0974 for migraine prophylaxis in patients with episodic migraine. 2009 http://clinicaltrials.gov/ct2/show/NCT00797667?term=telcagepant&rank=11.
- 60.Ho TW, Edvinsson L, Goadsby PJ. CGRP and its receptors provide new insights into migraine pathophysiology. Nature Reviews Neurology. 2010;6:573–582. doi: 10.1038/nrneurol.2010.127. [DOI] [PubMed] [Google Scholar]
- 61.Seybold VS. The role of peptides in central sensitization. In: Canning BJ, Spina D, editors. Handbook of Experimental Pharmacology. Vol. 194. Springer-Vertag; Berlin & Heidelberg: 2009. pp. 451–491. [DOI] [PubMed] [Google Scholar]
- 62.Ebersberger A, et al. Differential effects of calcitonin gene-related peptide and calcitonin gene-related peptide 8–37 upon responses to N-methyl-D-aspartate or (R, S)-alpha-amino-3-hydroxy-5-methylisoxazole-4-propionate in spinal nociceptive neurons with knee joint input in the rat. Neuroscience. 2000;99:171–178. doi: 10.1016/s0306-4522(00)00176-7. [DOI] [PubMed] [Google Scholar]
- 63.Gu XL, Yu LC. The colocalization of CGRP receptor and AMPA receptor in the spinal dorsal horn neuron of rat: a morphological and electrophysiological study. Neuroscience Letters. 2007;414:237–241. doi: 10.1016/j.neulet.2006.12.056. [DOI] [PubMed] [Google Scholar]
- 64.Menon S, et al. Association study of calcitonin gene-related polypeptide-alpha (CALCA) gene polymorphism with migraine. Brain Research. 2011;1378:119–124. doi: 10.1016/j.brainres.2010.12.072. [DOI] [PubMed] [Google Scholar]
- 65.Anttila V, et al. Genome-wide association study of migraine implicates a common susceptibility variant on 8q22.1. Nature Genetics. 2010;42:869–873. doi: 10.1038/ng.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Iversen HK, Olesen J, Tfelt-Hansen P. Intravenous nitroglycerin as an experimental model of vascular headache. Basic characteristics. Pain. 1989;38:17–24. doi: 10.1016/0304-3959(89)90067-5. [DOI] [PubMed] [Google Scholar]
- 67.Christiansen I, et al. Glyceryl trinitrate induces attacks of migraine without aura in sufferers of migraine with aura. Cephalalgia. 1999;19:660–667. doi: 10.1046/j.1468-2982.1999.019007660.x. discussion 626. [DOI] [PubMed] [Google Scholar]
- 68.Lassen LH, Thomsen LL, Olesen J. Histamine induces migraine via the H1-receptor. Support for the NO hypothesis of migraine. Neuroreport. 1995;6:1475–1479. doi: 10.1097/00001756-199507310-00003. [DOI] [PubMed] [Google Scholar]
- 69.Schytz HW, et al. PACAP38 induces migraine-like attacks in patients with migraine without aura. Brain. 2009;132:16–25. doi: 10.1093/brain/awn307. [DOI] [PubMed] [Google Scholar]
- 70.O’Connor T, van der Kooy D. Enrichment of a vasoactive neuropeptide (calcitonin gene related peptide) in the trigeminal sensory projection to the intracranial arteries. Journal of Neuroscience. 1988;8:2468–2476. doi: 10.1523/JNEUROSCI.08-07-02468.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Markowitz S, Saito K, Moskowitz MA. Neurogenically mediated leakage of plasma protein occurs from blood vessels in dura mater but not brain. Journal of Neuroscience. 1987;7:4129–4136. doi: 10.1523/JNEUROSCI.07-12-04129.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McCulloch J, et al. Calcitonin gene-related peptide: functional role in cerebrovascular regulation. Proceedings of the National Academy of Sciences USA. 1986;83:5731–5735. doi: 10.1073/pnas.83.15.5731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Olesen J, et al. Origin of pain in migraine: evidence for peripheral sensitisation. Lancet Neurology. 2009;8:679–690. doi: 10.1016/S1474-4422(09)70090-0. [DOI] [PubMed] [Google Scholar]
- 74.Chan KY, et al. Potential mechanisms of prospective antimigraine drugs: a focus on vascular (side) effects. Pharmacology & Therapeutics. 2011;129:332–351. doi: 10.1016/j.pharmthera.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 75.Diener HC. RPR100893, a substance-P antagonist, is not effective in the treatment of migraine attacks. Cephalalgia. 2003;23:183–185. doi: 10.1046/j.1468-2982.2003.00496.x. [DOI] [PubMed] [Google Scholar]
- 76.Sixt ML, Messlinger K, Fischer MJ. Calcitonin gene-related peptide receptor antagonist olcegepant acts in the spinal trigeminal nucleus. Brain. 2009;132:3134–3141. doi: 10.1093/brain/awp168. [DOI] [PubMed] [Google Scholar]
- 77.Edvinsson L. CGRP blockers in migraine therapy: where do they act? British Journal of Pharmacology. 2008;155:967–969. doi: 10.1038/bjp.2008.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tfelt-Hansen P, Olesen J. Possible site of action of CGRP antagonists in migraine. Cephalalgia. 2011;31:748–750. doi: 10.1177/0333102411398403. [DOI] [PubMed] [Google Scholar]
- 79.Lambracht-Hall M, Dimitriadou V, Theoharides TC. Migration of mast cells in the developing rat brain. Brain Research Developmental Brain Research. 1990;56:151–159. doi: 10.1016/0165-3806(90)90077-c. [DOI] [PubMed] [Google Scholar]
- 80.Wedemeyer J, Tsai M, Galli SJ. Roles of mast cells and basophils in innate and acquired immunity. Current Opinion of Immunology. 2000;12:624–631. doi: 10.1016/s0952-7915(00)00154-0. [DOI] [PubMed] [Google Scholar]
- 81.Hakim-Rad K, Metz M, Maurer M. Mast cells: makers and breakers of allergic inflammation. Current Opinion in Allergy and Clinical Immunology. 2009;9:427–430. doi: 10.1097/ACI.0b013e32832e9af1. [DOI] [PubMed] [Google Scholar]
- 82.Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. Journal of Allergy and Clinical Immunology. 2003;111:S486–S494. doi: 10.1067/mai.2003.120. [DOI] [PubMed] [Google Scholar]
- 83.Low NC, Merikangas KR. The comorbidity of migraine. CNS Spectrums. 2003;8:433–434. 437–444. doi: 10.1017/s1092852900018745. [DOI] [PubMed] [Google Scholar]
- 84.Koziol JA, et al. The natural history of interstitial cystitis: a survey of 374 patients. Journal of Urology. 1993;149:465–469. doi: 10.1016/s0022-5347(17)36120-7. [DOI] [PubMed] [Google Scholar]
- 85.Warnock JK, Clayton AH. Chronic episodic disorders in women. Psychiatric Clinics of North America. 2003;26:725–740. doi: 10.1016/s0193-953x(03)00042-x. [DOI] [PubMed] [Google Scholar]
- 86.Theoharides TC. Mast cells and migraines. Perspectives in Biology and Medicine. 1983;26:672–675. doi: 10.1353/pbm.1983.0028. [DOI] [PubMed] [Google Scholar]
- 87.Tepper SJ. New thoughts on sinus headache. Allergy and Asthma Proceedings. 2004;25:95–96. [PubMed] [Google Scholar]
- 88.Theoharides TC, Kalogeromitros D. The critical role of mast cells in allergy and inflammation. Annals of the New York Academy of Science. 2006;1088:78–99. doi: 10.1196/annals.1366.025. [DOI] [PubMed] [Google Scholar]
- 89.Rozniecki JJ, et al. Morphological and functional demonstration of rat dura mater mast cell-neuron interactions in vitro and in vivo. Brain Research. 1999;849:1–15. doi: 10.1016/s0006-8993(99)01855-7. [DOI] [PubMed] [Google Scholar]
- 90.Burstein R, Collins B, Jakubowski M. Defeating migraine pain with triptans: a race against the development of cutaneous allodynia. Annals of Neurology. 2004;55:19–26. doi: 10.1002/ana.10786. [DOI] [PubMed] [Google Scholar]
- 91.Durham PL, Russo AF. Regulation of calcitonin gene-related peptide secretion by a serotonergic antimigraine drug. Journal of Neuroscience. 1999;19:3423–3429. doi: 10.1523/JNEUROSCI.19-09-03423.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bowen EJ, et al. Tumor necrosis factor-alpha stimulation of calcitonin gene-related peptide expression and secretion from rat trigeminal ganglion neurons. Journal of Neurochemistry. 2006;96:65–77. doi: 10.1111/j.1471-4159.2005.03524.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Levy D, et al. Mast cell degranulation activates a pain pathway underlying migraine headache. Pain. 2007;130:166–176. doi: 10.1016/j.pain.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Strassman AM, Levy D. Response properties of dural nociceptors in relation to headache. Journal of Neurophysiology. 2006;95:1298–1306. doi: 10.1152/jn.01293.2005. [DOI] [PubMed] [Google Scholar]
- 95.Waeber C, Moskowitz MA. Migraine as an inflammatory disorder. Neurology. 2005;64:S9–15. doi: 10.1212/wnl.64.10_suppl_2.s9. [DOI] [PubMed] [Google Scholar]
- 96.Launay JM, et al. Histamine-release and migraine. Revue de Médecine Interne. 1987;8:273–275. doi: 10.1016/s0248-8663(87)80230-8. [DOI] [PubMed] [Google Scholar]
- 97.Heatley RV, et al. Increased plasma histamine levels in migraine patients. Clinical Allergy. 1982;12:145–149. doi: 10.1111/j.1365-2222.1982.tb01633.x. [DOI] [PubMed] [Google Scholar]
- 98.Sjaastad O, Sjaastad OV. Histamine metabolism in cluster headache and migraine. Catabolism of 14C histamine. Journal of Neurology. 1977;216:105–117. doi: 10.1007/BF00312944. [DOI] [PubMed] [Google Scholar]
- 99.Krabbe AA, Olesen J. Headache provocation by continuous intravenous infusion of histamine. Clinical results and receptor mechanisms. Pain. 1980;8:253–259. doi: 10.1016/0304-3959(88)90012-7. [DOI] [PubMed] [Google Scholar]
- 100.Lassen LH, et al. Histamine inhalation is a specific but insensitive laboratory test for migraine. Cephalalgia. 1996;16:550–553. doi: 10.1046/j.1468-2982.1996.1608550.x. [DOI] [PubMed] [Google Scholar]
- 101.Schwenger N, et al. Interaction of calcitonin gene-related peptide, nitric oxide and histamine release in neurogenic blood flow and afferent activation in the rat cranial dura mater. Cephalalgia. 2007;27:481–491. doi: 10.1111/j.1468-2982.2007.01321.x. [DOI] [PubMed] [Google Scholar]
- 102.Lassen LH, et al. Histamine-1 receptor blockade does not prevent nitroglycerin induced migraine. Support for the NO-hypothesis of migraine. European Journal of Clinical Pharmacology. 1996;49:335–339. doi: 10.1007/BF00203773. [DOI] [PubMed] [Google Scholar]
- 103.Rossi P, Fiermonte G, Pierelli F. Cinnarizine in migraine prophylaxis: efficacy, tolerability and predictive factors for therapeutic responsiveness. An open-label pilot trial. Functional Neurology. 2003;18:155–159. [PubMed] [Google Scholar]
- 104.Lewis DW, et al. Prophylactic treatment of pediatric migraine. Headache. 2004;44:230–237. doi: 10.1111/j.1526-4610.2004.04052.x. [DOI] [PubMed] [Google Scholar]
- 105.Togha M, Ashrafian H, Tajik P. Open-label trial of cinnarizine in migraine prophylaxis. Headache. 2006;46:498–502. doi: 10.1111/j.1526-4610.2006.00381.x. [DOI] [PubMed] [Google Scholar]
- 106.Diener HC, et al. Aspirin in the treatment of acute migraine attacks. Expert Review of Neurotherapeutics. 2006;6:563–573. doi: 10.1586/14737175.6.4.563. [DOI] [PubMed] [Google Scholar]
- 107.Silberstein SD, Goadsby PJ. Migraine: preventive treatment. Cephalalgia. 2002;22:491–512. doi: 10.1046/j.1468-2982.2002.00386.x. [DOI] [PubMed] [Google Scholar]
- 108.Monro J, Carini C, Brostoff J. Migraine is a food-allergic disease. Lancet. 1984;2:719–721. doi: 10.1016/s0140-6736(84)92626-6. [DOI] [PubMed] [Google Scholar]
- 109.Sheftell F, et al. Montelukast in the prophylaxis of migraine: a potential role for leukotriene modifiers. Headache. 2000;40:158–163. doi: 10.1046/j.1526-4610.2000.00022.x. [DOI] [PubMed] [Google Scholar]
- 110.de Souza Carvalho D, et al. Asthma plus migraine in childhood and adolescence: prophylactic benefits with leukotriene receptor antagonist. Headache. 2002;42:1044–1047. doi: 10.1046/j.1526-4610.2002.02236.x. [DOI] [PubMed] [Google Scholar]
- 111.Brandes JL, et al. Montelukast for migraine prophylaxis: a randomized, double-blind, placebo-controlled study. Headache. 2004;44:581–586. doi: 10.1111/j.1526-4610.2004.446006.x. [DOI] [PubMed] [Google Scholar]
- 112.Clemons A, et al. Amitriptyline and prochlorperazine inhibit proinflammatory mediator release from human mast cells: possible relevance to chronic fatigue syndrome. Journal of Clinical Psychopharmacology. 2011;31:385–387. doi: 10.1097/JCP.0b013e3182196e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Pannese E, et al. Satellite cell reactions to axon injury of sensory ganglion neurons: increase in number of gap junctions and formation of bridges connecting previously separate perineuronal sheaths. Anatomy and Embryology (Berlin) 2003;206:337–347. doi: 10.1007/s00429-002-0301-6. [DOI] [PubMed] [Google Scholar]
- 114.Hansson E, Ronnback L. Glial neuronal signaling in the central nervous system. FASEB Journal. 2003;17:341–348. doi: 10.1096/fj.02-0429rev. [DOI] [PubMed] [Google Scholar]
- 115.Eberhardt M, et al. Glyceroltrinitrate facilitates stimulated CGRP release but not gene expression of CGRP or its receptor components in rat trigeminal ganglia. Neuropeptides. 2009;43:483–489. doi: 10.1016/j.npep.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 116.Vause CV, Durham PL. Calcitonin gene-related peptide differentially regulates gene and protein expression in trigeminal glia cells: findings from array analysis. Neuroscience Letters. 2010;473:163–167. doi: 10.1016/j.neulet.2010.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Thalakoti S, et al. Neuronglia signaling in trigeminal ganglion: implications for migraine pathology. Headache. 2007;47:1008–1023. doi: 10.1111/j.1526-4610.2007.00854.x. discussion 1024–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Capuano A, et al. Proinflammatory-activated trigeminal satellite cells promote neuronal sensitization: relevance for migraine pathology. Molecular Pain. 2009;5:43. doi: 10.1186/1744-8069-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.De Corato A, et al. Trigeminal satellite cells express functional calcitonin gene-related peptide receptors, whose activation enhances interleukin-1beta pro-inflammatory effects. Journal of Neuroimmunology J Neuroimmunol. 2011 Aug 15;237(1–2):39–46. doi: 10.1016/j.jneuroim.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 120.Watkins LR, Milligan ED, Maier SF. Spinal cord glia: new players in pain. Pain. 2001;93:201–205. doi: 10.1016/S0304-3959(01)00359-1. [DOI] [PubMed] [Google Scholar]
- 121.Cao H, Zhang YQ. Spinal glial activation contributes to pathological pain states. Neuroscience and Biobehavioral Review. 2008;32:972–983. doi: 10.1016/j.neubiorev.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 122.Recober A, et al. Role of calcitonin gene-related peptide in light-aversive behavior: implications for migraine. Journal of Neuroscience. 2009;29:8798–8804. doi: 10.1523/JNEUROSCI.1727-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Russo AF, et al. Positive-feedback regulation of CGRP synthesis in a preclinical migraine model. Cephalalgia. 2009;29:86. [Google Scholar]
- 124.Amara SG, et al. Alternative RNA processing in calcitonin gene expression generates mRNAs encoding different polypeptide products. Nature. 1982;298:240–244. doi: 10.1038/298240a0. [DOI] [PubMed] [Google Scholar]
- 125.Moya F, Nieto A, JLRC Calcitonin biosynthesis: evidence for a precursor. European Journal of Biochemistry/FEBS. 1975;55:407–413. doi: 10.1111/j.1432-1033.1975.tb02176.x. [DOI] [PubMed] [Google Scholar]
- 126.Park KY, et al. Epigenetic regulation of the calcitonin gene-related peptide gene in trigeminal glia. Cephalalgia. 2011;31:614–624. doi: 10.1177/0333102410391487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kristiansen KA, Edvinsson L. Neurogenic inflammation: a study of rat trigeminal ganglion. Journal of Headache and Pain. 2010;11:485–495. doi: 10.1007/s10194-010-0260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tajti J, et al. Organ culture of the trigeminal ganglion induces enhanced expression of calcitonin gene-related peptide via activation of extracellular signal-regulated protein kinase 1/2. Cephalalgia. 2011;31:95–105. doi: 10.1177/0333102410382796. [DOI] [PubMed] [Google Scholar]
- 129.Buhaescu I, Yood RA, Izzedine H. Serum procalcitonin in systemic autoimmune diseases – where are we now? Seminars in Arthritis and Rheumatism. 2010;40:176–183. doi: 10.1016/j.semarthrit.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 130.Martinez JM, et al. Late immunoneutralization of procalcitonin arrests the progression of lethal porcine sepsis. Surgical Infection (Larchmt) 2001;2:193–202. doi: 10.1089/109629601317202678. discussion 202–193. [DOI] [PubMed] [Google Scholar]
- 131.Turan H, et al. Procalcitonin levels in migraine patients. Canadian Journal of Neurological Sciences. 2011;38:124–128. doi: 10.1017/s0317167100011161. [DOI] [PubMed] [Google Scholar]
- 132.Sexton PM, et al. Procalcitonin has bioactivity at calcitonin receptor family complexes: potential mediator implications in sepsis. Critical Care Medicine. 2008;36:1637–1640. doi: 10.1097/CCM.0b013e318170a554. [DOI] [PubMed] [Google Scholar]
- 133.Olesen J, Larsen B, Lauritzen M. Focal hyperemia followed by spreading oligemia and impaired activation of rCBF in classic migraine. Annals of Neurology. 1981;9:344–352. doi: 10.1002/ana.410090406. [DOI] [PubMed] [Google Scholar]
- 134.Lauritzen M. Pathophysiology of the migraine aura. The spreading depression theory. Brain. 1994;117(Pt 1):199–210. doi: 10.1093/brain/117.1.199. [DOI] [PubMed] [Google Scholar]
- 135.Hadjikhani N, et al. Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proceedings of the National of Academy Science USA. 2001;98:4687–4692. doi: 10.1073/pnas.071582498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ayata C, et al. Suppression of cortical spreading depression in migraine prophylaxis. Annals of Neurology. 2006;59:652–661. doi: 10.1002/ana.20778. [DOI] [PubMed] [Google Scholar]
- 137.Wolthausen J, et al. Are cortical spreading depression and headache in migraine causally linked? Cephalalgia. 2009;29:244–249. doi: 10.1111/j.1468-2982.2008.01713.x. [DOI] [PubMed] [Google Scholar]
- 138.Hauge AW, et al. Effects of tonabersat on migraine with aura: a randomised, double-blind, placebo-controlled crossover study. Lancet Neurology. 2009;8:718–723. doi: 10.1016/S1474-4422(09)70135-8. [DOI] [PubMed] [Google Scholar]
- 139.Colonna DM, et al. Calcitonin gene-related peptide promotes cerebrovascular dilation during cortical spreading depression in rabbits. American Journal of Physiology. 1994;266:H1095–H1102. doi: 10.1152/ajpheart.1994.266.3.H1095. [DOI] [PubMed] [Google Scholar]
- 140.Wahl M, et al. Involvement of calcitonin gene-related peptide (CGRP) and nitric oxide (NO) in the pial artery dilatation elicited by cortical spreading depression. Brain Research. 1994;637:204–210. doi: 10.1016/0006-8993(94)91234-3. [DOI] [PubMed] [Google Scholar]
- 141.Piper RD, et al. Cortical spreading depression does not result in the release of calcitonin gene-related peptide into the external jugular vein of the cat: relevance to human migraine. Cephalalgia. 1993;13:180–183. doi: 10.1046/j.1468-2982.1993.1303180.x. discussion 149. [DOI] [PubMed] [Google Scholar]
- 142.Bolay H, et al. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nature Medicine. 2002;8:136–142. doi: 10.1038/nm0202-136. [DOI] [PubMed] [Google Scholar]
- 143.Zhang X, et al. Activation of meningeal nociceptors by cortical spreading depression: implications for migraine with aura. Journal of Neuroscience. 2010;30:8807–8814. doi: 10.1523/JNEUROSCI.0511-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zhang X, et al. Activation of central trigeminovascular neurons by cortical spreading depression. Annals of Neurology. 2011;69:855–865. doi: 10.1002/ana.22329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Moskowitz MA. Neurogenic inflammation in the pathophysiology and treatment of migraine. Neurology. 1993;43:S16–S20. [PubMed] [Google Scholar]
- 146.Kunkler PE, Kraig RP. Hippocampal spreading depression bilaterally activates the caudal trigeminal nucleus in rodents. Hippocampus. 2003;13:835–844. doi: 10.1002/hipo.10139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Buzzi MG, Bonamini M, Moskowitz MA. Neurogenic model of migraine. Cephalalgia. 1995;15:277–280. doi: 10.1046/j.1468-2982.1995.1504277.x. [DOI] [PubMed] [Google Scholar]
- 148.Jakubowski M, et al. Sensitization of central trigeminovascular neurons: blockade by intravenous naproxen infusion. Neuroscience. 2007;148:573–583. doi: 10.1016/j.neuroscience.2007.04.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Zhang XC, et al. Tumor necrosis factor-alpha induces sensitization of meningeal nociceptors mediated via local COX and p38 MAP kinase actions. Pain. 2011;152:140–149. doi: 10.1016/j.pain.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Noseda R, et al. Changes of meningeal excitability mediated by corticotrigeminal networks: a link for the endogenous modulation of migraine pain. Journal of Neuroscience. 2010;30:14420–14429. doi: 10.1523/JNEUROSCI.3025-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Edelmayer RM, et al. Medullary pain facilitating neurons mediate allodynia in headache-related pain. Annals of Neurology. 2009;65:184–193. doi: 10.1002/ana.21537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Dobolyi A, et al. Calcitonin gene-related peptide-containing pathways in the rat forebrain. Journal of Comparative Neurology. 2005;489:92–119. doi: 10.1002/cne.20618. [DOI] [PubMed] [Google Scholar]
- 153.Skofitsch G, Jacobowitz DM. Autoradiographic distribution of 125I calcitonin gene-related peptide binding sites in the rat central nervous system. Peptides. 1985;6:975–986. doi: 10.1016/0196-9781(85)90331-6. [DOI] [PubMed] [Google Scholar]
- 154.Yashpal K, et al. Quantitative autoradiographic distribution of calcitonin gene-related peptide (hCGRP alpha) binding sites in the rat and monkey spinal cord. Journal of Comparative Neurology. 1992;322:224–232. doi: 10.1002/cne.903220208. [DOI] [PubMed] [Google Scholar]
- 155.Noseda R, et al. A neural mechanism for exacerbation of headache by light. Nature Neuroscience. 2010;13:239–245. doi: 10.1038/nn.2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Noseda R, Burstein R. Advances in understanding the mechanisms of migraine-type photophobia. Current Opinion in Neurology. 2011;24:197–202. doi: 10.1097/WCO.0b013e3283466c8e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Okamoto K, et al. Bright light activates a trigeminal nociceptive pathway. Pain. 2010;149:235–242. doi: 10.1016/j.pain.2010.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Selby G, Lance JW. Observations on 500 cases of migraine and allied vascular headache. Journal of Neurology, Neurosurgery & Psychiatry. 1960;23:23–32. doi: 10.1136/jnnp.23.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Drummond PD. A quantitative assessment of photophobia in migraine and tension headache. Headache. 1986;26:465–469. doi: 10.1111/j.1526-4610.1986.hed2609465.x. [DOI] [PubMed] [Google Scholar]
- 160.Freedman MS, et al. Regulation of mammalian circadian behavior by non-rod, non-cone, ocular photoreceptors. Science. 1999;284:502–504. doi: 10.1126/science.284.5413.502. [DOI] [PubMed] [Google Scholar]
- 161.Afridi SK, et al. A positron emission tomographic study in spontaneous migraine. Archives of Neurology. 2005;62:1270–1275. doi: 10.1001/archneur.62.8.1270. [DOI] [PubMed] [Google Scholar]
- 162.Liu H, et al. Immumohistochemical localization of the CLR/RAMP1 receptor complex in the trigeminovascular system of the cynomologus monkey. Headache. 2011;51:6. [Google Scholar]
- 163.Burstein R, et al. Chemical stimulation of the intracranial dura induces enhanced responses to facial stimulation in brain stem trigeminal neurons. Journal of Neurophysiology. 1998;79:964–982. doi: 10.1152/jn.1998.79.2.964. [DOI] [PubMed] [Google Scholar]
- 164.Kresse A, Jacobowitz DM, Skofitsch G. Detailed mapping of CGRP mRNA expression in the rat central nervous system: comparison with previous immunocytochemical findings. Brain Research Bulletin. 1995;36:261–274. doi: 10.1016/0361-9230(94)00201-b. [DOI] [PubMed] [Google Scholar]
- 165.Summ O, et al. Modulation of nocioceptive transmission with calcitonin gene-related peptide receptor antagonists in the thalamus. Brain. 2010;133:2540–2548. doi: 10.1093/brain/awq224. [DOI] [PubMed] [Google Scholar]
- 166.Gauriau C, Bernard JF. Posterior triangular thalamic neurons convey nociceptive messages to the secondary somatosensory and insular cortices in the rat. Journal of Neuroscience. 2004;24:752–761. doi: 10.1523/JNEUROSCI.3272-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.de Lacalle S, Saper CB. Calcitonin gene-related peptide-like immunoreactivity marks putative visceral sensory pathways in human brain. Neuroscience. 2000;100:115–130. doi: 10.1016/s0306-4522(00)00245-1. [DOI] [PubMed] [Google Scholar]
- 168.Yasui Y, Saper CB, Cechetto DF. Calcitonin gene-related peptide (CGRP) immunoreactive projections from the thalamus to the striatum and amygdala in the rat. Journal of Comparative Neurology. 1991;308:293–310. doi: 10.1002/cne.903080212. [DOI] [PubMed] [Google Scholar]
- 169.Campeau S, Watson SJ., Jr Connections of some auditory-responsive posterior thalamic nuclei putatively involved in activation of the hypothalamo–pituitary–adrenocortical axis in response to audiogenic stress in rats: an anterograde and retrograde tract tracing study combined with Fos expression. Journal of Comparative Neurology. 2000;423:474–491. [PubMed] [Google Scholar]
- 170.Coolen LM, et al. Parvocellular subparafascicular thalamic nucleus in the rat: anatomical and functional compartmentalization. Journal of Comparative Neurology. 2003;463:117–131. doi: 10.1002/cne.10740. [DOI] [PubMed] [Google Scholar]
- 171.Coolen LM, et al. Afferent connections of the parvocellular subparafascicular thalamic nucleus in the rat: evidence for functional subdivisions. Journal of Comparative Neurology. 2003;463:132–156. doi: 10.1002/cne.10739. [DOI] [PubMed] [Google Scholar]
- 172.Ma W, et al. Localization and modulation of calcitonin gene-related peptide-receptor component protein-immunoreactive cells in the rat central and peripheral nervous systems. Neuroscience. 2003;120:677–694. doi: 10.1016/s0306-4522(03)00159-3. [DOI] [PubMed] [Google Scholar]
- 173.Edvinsson L, et al. Cerebellar distribution of calcitonin gene-related peptide (CGRP) and its receptor components calcitonin receptor-like receptor (CLR) and receptor activity modifying protein 1 (RAMP1) in rat. Molecular and Cellular Neuroscience. 2011;46:333–339. doi: 10.1016/j.mcn.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 174.Hattar S, et al. Central projections of melanopsin-expressing retinal ganglion cells in the mouse. Journal of Comparative Neurology. 2006;497:326–349. doi: 10.1002/cne.20970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Calvino B, Grilo RM. Central pain control. Joint Bone Spine. 2006;73:10–16. doi: 10.1016/j.jbspin.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 176.Cooper HM, et al. Neuroanatomical pathways linking vision and olfaction in mammals. Psychoneuroendocrinology. 1994;19:623–639. doi: 10.1016/0306-4530(94)90046-9. [DOI] [PubMed] [Google Scholar]
- 177.Elliott AS, Weiss ML, Nunez AA. Direct retinal communication with the periamygdaloid area. Neuroreport. 1995;6:806–808. doi: 10.1097/00001756-199503270-00025. [DOI] [PubMed] [Google Scholar]
- 178.Morin LP, Blanchard JH. Forebrain connections of the hamster intergeniculate leaflet: comparison with those of ventral lateral geniculate nucleus and retina. Visual Neuroscience. 1999;16:1037–1054. doi: 10.1017/s0952523899166069. [DOI] [PubMed] [Google Scholar]
- 179.Sink KS, et al. Calcitonin gene-related peptide in the bed nucleus of the stria terminalis produces an anxiety-like pattern of behavior and increases neural activation in anxiety-related structures. Journal of Neuroscience. 2011;31:1802–1810. doi: 10.1523/JNEUROSCI.5274-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.D’Hanis W, Linke R, Yilmazer-Hanke DM. Topography of thalamic and parabrachial calcitonin gene-related peptide (CGRP) immunoreactive neurons projecting to subnuclei of the amygdala and extended amygdala. Journal of Comparative Neurology. 2007;505:268–291. doi: 10.1002/cne.21495. [DOI] [PubMed] [Google Scholar]
- 181.Gebhart GF. Descending modulation of pain. Neuroscience & Biobehavioral Review. 2004;27:729–737. doi: 10.1016/j.neubiorev.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 182.Behbehani MM. Functional characteristics of the midbrain periaqueductal gray. Progress in Neurobiology. 1995;46:575–605. doi: 10.1016/0301-0082(95)00009-k. [DOI] [PubMed] [Google Scholar]
- 183.Thiels E, Hoffman EK, Gorin MB. A reliable behavioral assay for the assessment of sustained photophobia in mice. Current Eye Research. 2008;33:483–491. doi: 10.1080/02713680802130347. [DOI] [PubMed] [Google Scholar]
- 184.Recober A, et al. CGRP-induced photophobia blocked by olcegepant and rizatriptan in a transgenic migraine model. Cephalalgia. 2009;29:1. [Google Scholar]
- 185.Recober A, et al. Induction of multiple photophobic behaviors in a transgenic mouse sensitized to CGRP. Neuropharmacology. 2010;58:156–165. doi: 10.1016/j.neuropharm.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Russo AF, et al. A potential preclinical migraine model: CGRP-sensitized mice. Molecular and Cellular Pharmacology. 2009;1:264–270. [PMC free article] [PubMed] [Google Scholar]
- 187.Diener HC, et al. BI 44370 TA, an oral CGRP antagonist for the treatment of acute migraine attacks: results from a phase II study. Cephalalgia. 2011;31:573–584. doi: 10.1177/0333102410388435. [DOI] [PubMed] [Google Scholar]
- 188.Hewitt DJ, et al. Randomized controlled trial of the CGRP receptor antagonist MK-3207 in the acute treatment of migraine. Cephalalgia. 2011;31:712–722. doi: 10.1177/0333102411398399. [DOI] [PubMed] [Google Scholar]
- 189.Shi L, et al. In vitro characterization of a group of potent and selective human monoclonal antibodies against CGRP receptor. Headache. 2011;51(Suppl 1):59. [Google Scholar]
- 190.Zeller J, et al. CGRP function-blocking antibodies inhibit neurogenic vasodilatation without affecting heart rate or arterial blood pressure in the rat. British Journal of Pharmacology. 2008;155:1093–1103. doi: 10.1038/bjp.2008.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Sang CN, et al. LY293558, a novel AMPA/GluR5 antagonist, is efficacious and well-tolerated in acute migraine. Cephalalgia. 2004;24:596–602. doi: 10.1111/j.1468-2982.2004.00723.x. [DOI] [PubMed] [Google Scholar]
- 192.ClinicalTrials.gov. Efficacy and safety of BGG492 in the treatment of migraine. 2011 http://clinicaltrials.gov/ct2/show/NCT00892203?term=BGG492&rank=7.