Abstract
Background
Prescribing warfarin for atrial fibrillation depends in large part on the expected reduction in ischemic stroke risk versus the expected increased risk of intracranial hemorrhage (ICH). However, the anticoagulation decision also depends on the relative severity of such events. We assessed the impact of anticoagulation on 30-day mortality from ischemic stroke vs. ICH in a large community-based cohort of patients with atrial fibrillation.
Methods
We followed 13,559 patients with atrial fibrillation enrolled in an integrated healthcare delivery system for a median 6 years. Incident ischemic strokes and ICHs were identified from computerized databases and validated through medical record review. The association of warfarin and international normalized ratio (INR) at presentation with 30-day mortality was modeled using multivariable logistic regression, adjusting for clinical factors.
Results
We identified 1025 incident ischemic strokes and 299 ICHs during follow-up. Compared with no antithrombotic therapy, warfarin was associated with reduced Rankin score and lower 30-day mortality from ischemic stroke (adjusted odds ratio and 95% confidence interval [OR] = 0.64 [0.45, 0.91]), but a higher mortality from ICH (OR = 1.62 [0.88, 2.98]). Therapeutic INRs (2-3) were associated with an especially low ischemic stroke mortality (OR = 0.38 [0.20, 0.70]) while INRs > 3 increased the odds of dying of ICH by 2.66 fold (95% confidence interval: 1.21, 5.86).
Conclusions
Warfarin reduces 30-day mortality from ischemic stroke, but increases ICH-related mortality. Both effects on event severity as well as on event rates need to be incorporated into rational decision-making about anticoagulants for atrial fibrillation.
Keywords: Acute stroke, Intracranial hemorrhage, Anticoagulants, Warfarin, Atrial fibrillation
Introduction
Atrial fibrillation is a potent risk factor for ischemic stroke. Oral anticoagulants, such as warfarin, can largely reverse this stroke risk1. However, warfarin therapy can lead to significant bleeding complications, the most important type of which is intracranial hemorrhage. The anticoagulation decision in a patient with atrial fibrillation depends in large part on the expected reduction in ischemic stroke risk due to warfarin versus its expected increase in risk of intracranial hemorrhage2. However, the anticoagulation decision should also depend on the impact of anticoagulant therapy on the severity of incident ischemic and hemorrhagic events 3.
Prior studies have quantified the decreased incidence of ischemic stroke in atrial fibrillation patients taking anticoagulants and the increased incidence of intracranial hemorrhages1. However, much less is known about the comparative severity of ischemic stroke and intracranial hemorrhage events, and how outcomes vary according to warfarin exposure and anticoagulation intensity. Direct comparison of the outcomes of such events is important when determining the net clinical benefit of anticoagulant therapy2. The objective of this study was to compare the short-term mortality and disability after ischemic stroke and intracranial hemorrhage in patients with atrial fibrillation, both on and off warfarin therapy.
Methods
The AnTicoagulation and Risk factors In Atrial fibrillation (ATRIA) study includes a cohort of 13,559 adults aged ≥ 18 years with diagnosed atrial fibrillation enrolled in Kaiser Permanente of Northern California. As described previously, cohort members were identified between July 1, 1996 and December 31, 1997 by searching automated inpatient, outpatient, and electrocardiographic databases for International Classification of Diseases, Ninth Revisions, Clinical Modification (ICD-9) diagnoses of atrial fibrillation (427.31). Subjects were followed until death, cohort disenrollment, or the study end-date of September 30, 20034, 5. Patients with diagnosed mitral stenosis, heart valve repair or replacement, transient post-operative atrial fibrillation, or concurrent hyperthyroidism were excluded so as to focus on nonvalvular, nontransient atrial fibrillation.
Identification of Ischemic Strokes and Intracranial Hemorrhages
To identify stroke and intracranial hemorrhage events, computerized hospitalization and billing databases were searched for primary discharge diagnoses of ischemic stroke and primary and secondary discharge diagnoses of intracranial hemorrhage (codes available upon request). Only the first occurrence of each event type was identified. Hospitalizations of patients at facilities outside of the network were also recorded in Kaiser Permanente databases. The medical records of potential events were abstracted and events adjudicated by an outcomes committee using a formal study protocol, with at least 2 physicians reviewing the medical records for each potential event and a third physician reviewing cases in which the initial reviewers disagreed.
Ischemic stroke events were considered valid if they were sudden onset neurological deficits that persisted for at least 24 hours that were not explained by other etiologies (such as trauma, infection, or vasculitis). Intracranial hemorrhages were reviewed and categorized as intracerebral, subdural, or other (e.g., subarachnoid) based on radiology reports obtained from the medical records. Events that began as ischemic strokes and subsequently converted to hemorrhagic events were considered ischemic strokes. Events that occurred as complications of inpatient hospitalization, diagnostic or interventional procedures, or as a result of severe head trauma (such from a motor vehicle accident) were excluded.
Functional disability at the time of hospital discharge was determined through review of available physician, nursing, physical/occupational therapy, and social work notes in the medical record. Disability was categorized using a modified Rankin scale into: fatal inpatient event, major/severe disability (deficits that prevented independent living, corresponding to Rankin scores of 3-5), minor disability (residual deficit that did not interfere with independent living, equivalent to Rankin scores of 1-2), and no disability (Rankin score 0)6. For all cohort members sustaining an outcome event during the follow-up period, death and date of death were ascertained for a period of at least 30 days following hospital presentation with the event. Such information was obtained from medical chart review, healthplan databases, and the comprehensive California State death certificate registry.
Determination of Comorbid Conditions and Warfarin Use
We searched clinical inpatient and outpatient databases for specific medical conditions using relevant ICD-9 codes from five years before each subject’s cohort enrollment date and throughout the follow-up period, a search strategy that has demonstrated high agreement with chart documentation in previous validation studies4. Warfarin use within 5 days of the index hospitalization was determined from a previously validated warfarin algorithm based on dispensed warfarin prescriptions and international normalized ratio (INR) testing4, as well as from review of emergency department and hospitalization records. For patients on warfarin, we obtained the INR value at presentation to the hospital and prior to any administration of reversal agents (e.g., vitamin K or fresh frozen plasma). We also reviewed emergency department and hospitalization records for documentation of aspirin use on presentation. If aspirin use was not documented, then patients were presumed to not be taking aspirin.
Statistical Analysis
The primary outcome of the study was the proportion of patients whose date of death occurred within 30 days of the date of presentation to the hospital with the index event. Complete data on mortality within 30 days of presentation was available for all participants. Bivariate comparisons of clinical characteristics at the time of presentation between those on and off warfarin were assessed with t-tests for continuous variables and Chi-squared tests for categorical variables. The association of warfarin therapy with functional status at the time of discharge (modified Rankin categories of no, minor, major/severe disability, or died in hospital) was assessed by the Cochran-Armitage trend test and by ordinal logistic regression. A Chi-square test was also used to compare the proportion discharged with no or minor deficits between on and off warfarin groups. Twenty-three patients with ischemic stroke and 20 intracranial hemorrhage patients were excluded from the analysis of functional status because of missing functional status assessment at discharge. Thirty-day mortality from ischemic stroke vs. intracranial hemorrhage was assessed using Chi-squared tests. In the analysis of hospital discharge functional status and 30-day mortality from ischemic stroke, 58 patients had hospital lengths of stay > 30 days and 10 of these patients (0.96% of all ischemic strokes) had minor or no deficits at discharge. For these 10 patients, we assumed their functional status was also minor/no deficits before 30 days. Standard dichotomous logistic regression models were developed to assess the association of antithrombotic treatment (categorized into warfarin, no warfarin but on aspirin, and no documented antithrombotic therapy) with the odds of 30-day mortality. Models were adjusted for age (<65, 65-74, 75-84, and ≥85 years), sex, prior stroke, hypertension, heart failure, diabetes mellitus, and coronary artery disease. Models of intracranial hemorrhage were also adjusted for whether the event was intracerebral or not, due to the high mortality associated with intracerebral events. Additional models assessed the adjusted association of anticoagulation intensity, divided into INR categories at presentation, with 30-day mortality among patients on warfarin.
Results
We identified 1025 ischemic strokes during 64,891 person-years (49.7% on warfarin) and 299 intracranial hemorrhages during 66,409 person-years of follow up (50.3% on warfarin) in patients with atrial fibrillation. The clinical characteristics of patients at the time of stroke or intracranial hemorrhage presentation, on or off warfarin, are presented in Table 1. The vast majority of the patients taking warfarin had been on warfarin for over 6 months; 83% of patients sustaining an ischemic stroke on warfarin had been taking warfarin for >6 months and 89% of those sustaining an intracranial hemorrhage on warfarin had been taking warfarin for >6 months. Warfarin-users who presented with ischemic stroke were slightly younger, more likely to be male, and have diagnosed hypertension, diabetes mellitus, or prior stroke compared to non-warfarin users. Tissue plasminogen activator was used very infrequently in the patients sustaining an ischemic stroke: in 4.4% of patients not on warfarin and in 1.3% of patients taking warfarin. Patients who were taking warfarin at the time of their intracranial hemorrhage were also younger than those off warfarin. Aspirin use was more common among patients who were not taking warfarin; few patients took warfarin and aspirin concomitantly (Table 1).
Table 1.
Bivariate Comparison of Characteristics of Patients with Ischemic Stroke and Intracranial Hemorrhage On and Off Warfarin
| Ischemic Stroke N=1025 |
Intracranial Hemorrhage N=299 |
|||||
|---|---|---|---|---|---|---|
| On Warfarin N=382 |
Off Warfarin N=643 |
P-value | On Warfarin N=193 |
Off Warfarin N=106 |
P-value | |
|
|
||||||
| Age (mean ± SD) | 77 ± 8 | 80 ± 9 | <0.001 | 77 ± 8 | 81 ± 10 | 0.003 |
|
| ||||||
| Female (%) | 46.1 | 57.1 | <0.001 | 37.3 | 45.3 | 0.18 |
|
| ||||||
| Diagnosed hypertension (%) |
74.9 | 67.7 | 0.01 | 69.9 | 60.4 | 0.09 |
|
| ||||||
| Congestive heart failure (%) |
44.0 | 41.4 | 0.41 | 42.5 | 36.8 | 0.34 |
|
| ||||||
| Diabetes mellitus (%) | 31.7 | 23.8 | 0.006 | 19.2 | 18.9 | 0.95 |
|
| ||||||
| Prior stroke (%) | 23.6 | 16.0 | 0.003 | 24.4 | 16.0 | 0.09 |
|
| ||||||
| Coronary artery disease (%) |
39.8 | 37.5 | 0.46 | 34.7 | 29.2 | 0.34 |
|
| ||||||
| Documented aspirin use at time of event (%) |
4.7 | 44.5 | <0.001 | 5.7 | 30.2 | <0.001 |
|
| ||||||
Association of Warfarin with Outcomes
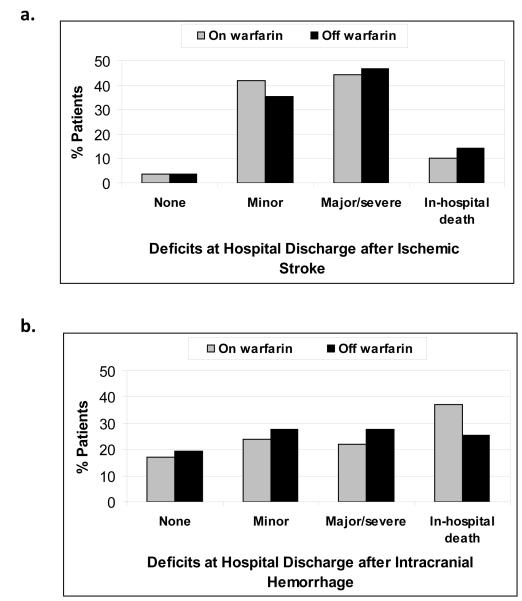
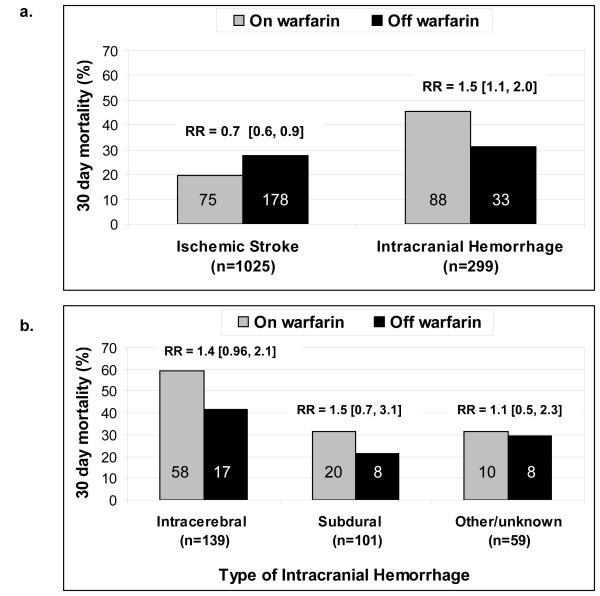
Warfarin use compared to use of aspirin or no antithrombotic therapy was associated with milder ischemic strokes: 3.8%% of patients presenting with ischemic stroke on warfarin were discharged with no deficits, 41.9% with minor, 44.3% with major/severe deficits, and 10% inpatient death, compared to 3.6% with no deficits, 35.4% with minor, 46.7% with major/severe, and 14.2% inpatient death off warfarin (p for trend =0.025, Figure 1a). Combining categories, 45.7% of patients presenting with ischemic stroke on warfarin were discharged with no or minor deficits, compared to 39.1% presenting off warfarin (p=0.046). This association persisted after controlling for age, sex, prior stroke, hypertension, heart failure, diabetes mellitus, and coronary artery disease (odds ratio for more severe outcome 0.77, 95% confidence interval 0.60 to 0.99). Warfarin use was also associated with lower unadjusted 30-day mortality after ischemic stroke (19.6% vs. 27.7%, p=0.004, Figure 2a). Degree of deficit at discharge was strongly related to subsequent 30-day mortality. Deaths that occurred by 30-days were primarily among patients who had major or severe deficits (24.0% mortality rate at 30-days compared to 2.6% among those who had minor or no deficits, p<0.001). In a multiple logistic regression model including terms for aspirin monotherapy as well as age, sex, prior stroke, hypertension, heart failure, diabetes mellitus, and coronary artery disease, warfarin use at the time of ischemic stroke event was associated with decreased 30-day mortality, with an adjusted odds ratio (OR) versus no antithrombotic therapy of 0.64 [0.45, 0.91]. Aspirin monotherapy was not significantly associated with lower 30-day mortality (adjusted OR 0.75 [0.52, 1.1).
Figure 1.
Unadjusted functional deficits at the time of hospital discharge after ischemic stroke (Figure 1a) and intracranial hemorrhage (Figure 1b), stratified by warfarin status at the time of presentation. The comparator group includes patients on aspirin monotherapy or on no antithrombotic agent. Figure 1a percentages are based on 358 patients on warfarin and 621 patients off warfarin with known disability status. Figure 1b percentages are based on 169 patients on warfarin and 90 patients off warfarin with known disability status.
Figure 2.
a. Unadjusted relative risk of 30-day mortality associated with warfarin exposure, stratified by ischemic stroke and intracranial hemorrhage. The comparator group includes patients on aspirin monotherapy or on no antithrombotic agent. Numbers on bars indicate the number of events in each category. RR = relative risk [95% confidence interval].
b. Unadjusted relative risk of 30-day mortality associated with warfarin exposure, stratified by type of intracranial hemorrhage. Numbers on bars indicate the number of events in each category. RR = relative risk [95% confidence interval]
In patients with intracranial hemorrhage, warfarin use at presentation was associated with increased 30-day mortality (45.6% on warfarin vs. 31.1% off warfarin, p=0.02) but not with a significant difference in discharge deficits (p for trend =0.19, Figures 2a and 1b). When intracranial hemorrhages were subdivided by type, intracerebral hemorrhages were the most common type of intracranial hemorrhages that occurred on warfarin (50.8% intracerebral, 32.6% subdural, and 16.6% other hemorrhages), whereas the proportions of intracerebral and subdural hemorrhages were roughly equal in patients not taking warfarin (38.7% intracerebral and 35.9% subdural). This difference in composition of types of intracranial hemorrhage, on versus off warfarin, did not quite achieve statistical significance (p=0.08). Intracerebral hemorrhages were associated with particularly high 30-day mortality especially among patients taking warfarin, 59.2% on warfarin and 41.5% off warfarin (Figure 2b).
In a multivariable model adjusting for clinical factors as well as type of intracranial hemorrhage at presentation (intracerebral vs. non-intracerebral), warfarin use at the time of hemorrhage was associated with an adjusted OR for 30-day mortality of 1.62 (0.88, 2.98) compared to no antithrombotic therapy, but the association did not reach statistical significance.
Association of Anticoagulation Intensity with Mortality
Anticoagulation intensity, as measured by the INR at the time of presentation, was strongly associated with the outcomes of both ischemic stroke and intracranial hemorrhage. Compared to no antithrombotic therapy, patients who presented with ischemic stroke and had INRs in the therapeutic range of 2-3 had substantially lower 30-day mortality from ischemic stroke, with an adjusted OR of 0.38 (0.20, 0.70) (Table 2). In contrast, elevated INRs were associated with worse outcomes from intracranial hemorrhage: patients with intracranial hemorrhage presenting with INRs > 3.0 had an adjusted OR of 2.66 (1.21, 5.86) for 30-day mortality compared to patients who were on no antithrombotic therapy (Table 2). When INR was further subdivided into additional INR categories, the adjusted OR for 30-day mortality after intracranial hemorrhage was 2.51 (0.71, 8.80) for INRs 3.1-3.5 and 2.72 (1.14, 6.49) for INRs > 3.5.
Table 2.
Multivariable Analysis of Anticoagulation Intensity at Presentation and Association with 30-day Mortality after Ischemic Stroke and Intracranial Hemorrhage in Patients with Atrial Fibrillation
| Ischemic Stroke | Intracranial Hemorrhage | |
|---|---|---|
| Adjusted odds ratio [95% confidence interval] |
||
| Antithrombotic therapy at hospital presentation |
||
| Neither aspirin nor warfarin | Referent | Referent |
|
| ||
| Aspirin use only | 0.73 [0.51, 1.05] | 0.79 [0.30, 2.05] |
|
| ||
| Warfarin | ||
|
| ||
| INR < 2.0 | 0.74 [0.50, 1.12] | 1.01 [0.42, 2.43] |
|
| ||
| INR 2.0-3.0 | 0.38 [0.20, 0.70] | 1.32 [0.66, 2.64] |
|
| ||
| INR > 3.0 | 0.48 [0.19, 1.21] | 2.66 [1.21, 5.86] |
|
| ||
| Clinical features at hospital presentation | ||
| Age | ||
| < 65 | 0.86 [0.41, 1.83] | 0.54 [0.18, 1.59] |
|
| ||
| 65-74 | Referent | Referent |
|
| ||
| 75-84 | 1.48 [0.95, 2.31] | 0.92 [0.47, 1.82] |
|
| ||
| 85+ | 3.32 [2.07, 5.32] | 1.24 [0.58, 2.67] |
|
| ||
| Female | 0.88 [0.65, 1.20] | 0.96 [0.57, 1.61] |
|
| ||
| Prior stroke | 0.91 [0.62, 1.34] | 0.95 [0.51, 1.77] |
|
| ||
| Hypertension | 1.16 [0.84, 1.62] | 1.43 [0.83, 2.47] |
|
| ||
| Heart failure | 1.46 [1.08, 1.98] | 1.22 [0.73, 2.03] |
|
| ||
| Coronary artery disease | 1.06 [0.78, 1.45] | 0.92 [0.53, 1.59] |
|
| ||
| Diabetes mellitus | 1.34 [0.95, 1.88] | 0.70 [0.35, 1.37] |
|
| ||
| Intracerebral hemorrhage at presentation | n/a | 2.93 [1.77, 4.85] |
Comparative Mortality of Ischemic stroke vs. Intracranial Hemorrhage
Intracranial hemorrhages occurring on warfarin were associated with significantly higher 30-day mortality rates than ischemic strokes on warfarin (45.6% vs. 19.6%, p<0.001) while mortality occurring off warfarin did not significantly differ (31.1% after intracranial hemorrhage vs. 27.7% after ischemic stroke, p=0.46). The relative risk of 30-day mortality from intracranial hemorrhages occurring on warfarin (45.6%) compared to mortality from ischemic strokes off warfarin (27.7%), was 1.65 [1.35, 2.01].
Discussion
The anticoagulation decision for patients with atrial fibrillation depends in large part on balancing the expected reduction in the rate of ischemic stroke with warfarin therapy vs. the increased rate of intracranial hemorrhage2. However, this balance also needs to account for the severity of these events on and off anticoagulants. Although studies have quantified the reduction in ischemic stroke rate due to warfarin treatment1, there are relatively few data on the comparative severity of ischemic strokes and intracranial hemorrhages on and off anticoagulation. Our study found warfarin therapy was associated with milder functional deficits and reduced 30-day mortality from ischemic stroke. This effect of warfarin was particularly beneficial when the INR level was ≥ 2.0. In our ATRIA cohort, the (unadjusted) rate ratio for ischemic stroke, on versus off warfarin, was 0.60. The rate ratio for fatal ischemic stroke was 0.43, reflecting the effect of warfarin in preventing fatal ischemic events. By contrast, our results confirm the grim outcome of anticoagulation-associated intracranial hemorrhage, for which we observed a 46% mortality rate by 30 days. Intracerebral hemorrhages on warfarin were particularly severe, with a nearly 60% mortality rate by 30 days. Compared with no antithrombotic therapy, the adjusted odds of dying by 30 days after intracranial hemorrhage were increased by 62%. Warfarin was most harmful at INR levels above 3.0. In our ATRIA cohort, the (unadjusted) rate ratio for intracranial hemorrhage, on versus off warfarin, was 1.80. However, the rate ratio for fatal intracranial hemorrhage was 2.63, here reflecting the disproportionate increase in fatality of intracranial hemorrhages occurring on warfarin. Further, our analysis shows that intracranial hemorrhages on warfarin are associated with 1.65 times the 30-day mortality of ischemic strokes occurring off warfarin. These results, based on consequences of events as well as rates of events, are relevant to estimating the net clinical benefit of warfarin therapy in different subgroups of patients with atrial fibrillation2.
Our current findings add detail and precision to our previous report based on the first follow-up of the ATRIA cohort 7. In particular, we include an additional 400 ischemic strokes and an analysis of the severity of outcomes associated with intracranial hemorrhage. The general patterns of the effects of warfarin on outcomes of ischemic stroke are similar in the two reports. Other reports of warfarin-associated intracerebral hemorrhage, especially for INR values above 3.5, find similarly poor outcomes to our study, and suggest a relationship between higher INRs and increased volume of hematoma expansion8, 9. Newer anticoagulants appear to result in fewer intracranial hemorrhages compared to warfarin10, 11. Analyses addressing whether new anticoagulants result in less severe outcomes will be important.
Our study reflects the experience of a large, community-based cohort of patients with atrial fibrillation followed on average over a six-year period. We observed over a thousand ischemic strokes and nearly 300 intracranial hemorrhages allowing fairly precise comparisons of outcome by warfarin status. The events in our study were validated by review of the medical charts, which reduces the potential misclassification associated with reliance on administrative codes alone. Nevertheless, there are also several limitations to our study. The analysis was limited to patients who presented to hospitals. As a result, patients who died before reaching a hospital or who were managed solely in an outpatient setting may have been missed. Given the severity of strokes and intracranial hemorrhages, patients treated outside the hospital likely constitute a small fraction of all patients sustaining such events. Our multivariable adjustment for potential confounders may be incomplete, lacking unmeasured or unknown features linked to outcome and also associated with use of warfarin, such as “do not resuscitate” preference or pre-admission functional status. Similarly, assessment of discharge functional status was limited to information recorded in clinical notes, although the correlation of our estimates of Rankin scores and subsequent mortality makes large scale misclassification unlikely. Presence of unmeasured confounders, either prior to or during hospitalization, may result in possible over- or under-estimation of the association between warfarin use and outcomes.
Our findings demonstrate that warfarin’s benefits for patients with atrial fibrillation extend beyond simply reducing the risk of ischemic stroke. Anticoagulation, particularly in the therapeutic range of INR 2-3, reduces the severity of deficits and short-term mortality associated with ischemic strokes. Similarly, warfarin’s harms extend beyond simply increasing the risk of intracranial hemorrhages and also include increasing the severity of such events. While warfarin’s effects on the incidence of ischemic stroke and intracranial hemorrhage dominate the anticoagulation decision, effects on the severity of such events are important additional considerations and should be incorporated into clinical decision-making for individual patients and formal decision analyses.
Acknowledgments
Funding Sources This study was supported by the National Institute on Aging (R01 AG15478 and K23 AG028978), the National Heart, Lung and Blood Institute (U19 HL91179 and RC2HL101589), and the Eliot B. and Edith C. Shoolman fund of the Massachusetts General Hospital (Boston, MA). The funding sources had no role in study design, data collection, data analysis, data interpretation, or preparation of this manuscript.
Footnotes
Potential Financial Conflicts of Interest: D.E. Singer has consulted for Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Inc., Johnson & Johnson, Inc., Merck and Co., Bayer Healthcare, Pfizer, and Sanofi Aventis, Inc., and has received research support from Daiichi Sankyo, Inc. A.S. Go has received research support from Johnson & Johnson, Inc.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hart R, Pearce LA, Aguilar MI. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Annals of Internal Medicine. 2007;146:857–867. doi: 10.7326/0003-4819-146-12-200706190-00007. [DOI] [PubMed] [Google Scholar]
- 2.Singer DE, Chang Y, Fang MC, Borowsky LH, Pomernacki NK, Udaltsova N, et al. The net clinical benefit of warfarin anticoagulation in atrial fibrillation. Ann Intern Med. 2009;151:297–305. doi: 10.7326/0003-4819-151-5-200909010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point. Circulation: Cardiovascular Quality and Outcomes. 2011;4:14–21. doi: 10.1161/CIRCOUTCOMES.110.958108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Go AS, Hylek EM, Borowsky LH, Phillips KA, Selby JV, Singer DE. Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: The anticoagulation and risk factors in atrial fibrillation (atria) study. Annals of Internal Medicine. 1999;131:927–934. doi: 10.7326/0003-4819-131-12-199912210-00004. [DOI] [PubMed] [Google Scholar]
- 5.Go AS, Hylek EM, Chang Y, Phillips KA, Henault LE, Capra AM, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: How well do randomized trials translate into clinical practice? JAMA. 2003;290:2685–2692. doi: 10.1001/jama.290.20.2685. [DOI] [PubMed] [Google Scholar]
- 6.UK-TIA Study Group The united kingdom transient ischaemic attack (uk-tia) aspirin trial: Final results. Journal of Neurology, Neurosurgery, and Psychiatry. 1991;54:1044–1054. doi: 10.1136/jnnp.54.12.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. New England Journal of Medicine. 2003;349:1019–1026. doi: 10.1056/NEJMoa022913. [DOI] [PubMed] [Google Scholar]
- 8.Rosand J, Eckman MH, Knudsen KA, Singer DE, Greenberg SM. The effect of warfarin and intensity of anticoagulation on outcome of intracerebral hemorrhage. Archives of Internal Medicine. 2004;164:880–884. doi: 10.1001/archinte.164.8.880. [DOI] [PubMed] [Google Scholar]
- 9.Flibotte JJ, Hagan N, O’Donnell J, Greenberg SM, Rosand J. Warfarin, hematoma expansion, and outcome of intracerebral hemorrhage. Neurology. 2004;63:1059–1064. doi: 10.1212/01.wnl.0000138428.40673.83. [DOI] [PubMed] [Google Scholar]
- 10.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 11.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. New England Journal of Medicine. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]