For over 40 years, coronary artery disease (CAD) has been the leading cause of death in the United States. Death from CAD in the U.S. has declined by 23% since 2000 through modification of biologic cardiac risk factors (hypertension, elevated cholesterol, and smoking) and improvements in the treatment of CAD.1 Measurable risk factors, unfortunately, do not completely predict cardiac risk. Depression is a common, poorly identified, and inadequately treated independent risk factor for future cardiac events.
Depression Can Be Triggered by a Major Cardiac Event
In hospitalized patients who have experienced acute myocardial infarction (AMI), depression is 3 times more common than in the general community.2 Fifteen to twenty percent of post-AMI patients meet criteria for major depression,3–5 with estimates highest in younger women.6 Estimates of the prevalence of depression are similar in patients who are hospitalized for AMI, acute coronary syndromes, angioplasty, coronary artery bypass surgery, and valve surgery.7 Higher rates of depression have been reported in women and in patients hospitalized with congestive heart failure (CHF).7,8 In community-based studies, the prevalence of depression in the general population is reported between 4.8%9 and 6.6%.10 It is 9.3% in patients living with CAD, which is comparable to the 7.9%–17% rate seen in those living with other chronic medical conditions.9
Depression Is an Independent Risk Factor for Coronary Artery Disease
Eight longitudinal studies (including 15,613 patients followed for 153,031 patient-years) have robustly shown that depression, measured by various scales and by self-reporting, increases the risk of first cardiac event (relative risk, 1.5–4.8) in patients without a history of CAD.11 Among 8,000 healthy Finnish adults without CAD, depression increased the relative risk of cardiac death by 2.05 over 6.6 years of follow-up.12
Depression Increases All-Cause Death and Cardiac Complications in Patients with Coronary Artery Disease
Multiple studies have examined the mortality rates of CAD patients who have depression.13,14 Despite methodologic differences, including sample sizes, endpoint definition, criteria for depression, and variable lengths of follow-up, most studies report a 2-fold increase in all-cause death for patients with depression in the 1 to 2 years after AMI.2,7,8,15,16 Frasure-Smith and colleagues17 reported a 4-fold increased risk of death at 6 months for patients with depression that had been diagnosed 5 to 15 days after AMI and had persisted at 18 months. The Enhancing Recovery in Coronary Heart Disease18 (ENRICHD) trial compared a subgroup of 359 depressed patients after AMI to 408 nondepressed patients and reported a late (>12-mo) increased relative risk (2.8) of all-cause death in the depressed patients.18,19 Depression after AMI that is complicated by CHF is an independent predictor of all-cause death (at 2 yr, 29% vs 18%, P=0.004) and of cardiovascular death or hospitalization (42% vs 33%, P=0.016). In a well-designed case-control study, 2,228 clinically depressed patients after AMI were at increased risk of sudden cardiac death (odds ratio [OR], 1.43; 95% confidence interval, 1.18–1.73) when compared with 4,164 control patients.20 The sudden cardiac death risk persisted after adjustment for confounding factors (including antidepressant use) and actually rose with increasing depressive symptom severity, suggesting the presence of a “dose-response” relationship between depression severity and cardiac events (OR 1.3 for less severe depression vs an OR of 1.77 for severe depression, P <0.001 for trend).
Pathophysiologic Links between Depression and Coronary Artery Disease Risk Can Be Direct or Indirect
Depression contributes both to direct and indirect mechanisms that increase the risk of adverse events in patients with CAD. Biomarkers that have been shown to predict cardiac events and promote atherosclerosis (C-reactive protein, interleukin-6, tumor necrosis factor, fibrinogen, adrenaline, urinary catecholamines, intracellular adhesion molecule-1, and platelet factor 4) are elevated in depressed patients with CAD and provide a direct biological link to inflammatory cardiac events. Indirectly, depression augments the risk of CAD development and progression by increasing or continuing unhealthful lifestyle choices: continued smoking, inactivity, poor diet, and social isolation.19,21–24 Depression is associated with poor adherence to prescribed medications25 and with a 3-fold rise in noncompliance with medical treatment regimens.26
Screening for Depression Is Recommended in All Cardiac Patients
A nationwide survey of cardiologists revealed that 49% were unaware that depression was an independent risk factor for CAD and that 71% failed to inquire about depression in over half of their patients.27 Because cardiologists are often the point-of-care physician after acute cardiac events, they doubtless have a responsibility to screen for depression. A simple 2-question assessment, the Patient Health Questionnaire-2 (PHQ-2) (Fig. 1), has been validated to identify currently depressed patients. The PHQ-2 has been endorsed as a screening tool in cardiac patients by the American Heart Association, the American Psychiatric Association, and others.11,28 A response score of 3 or more to the PHQ-2 indicates the need for a follow-up, 5-minute, 9-question screening test (Fig. 2) that provides a provisional depression diagnosis and a severity score with reasonable sensitivity and specificity. A score greater than 10 suggests a high probability of depression, and scores greater than 20 are associated with severe functional impairment. Patients with scores over 10 should be referred for more comprehensive evaluation and treatment.
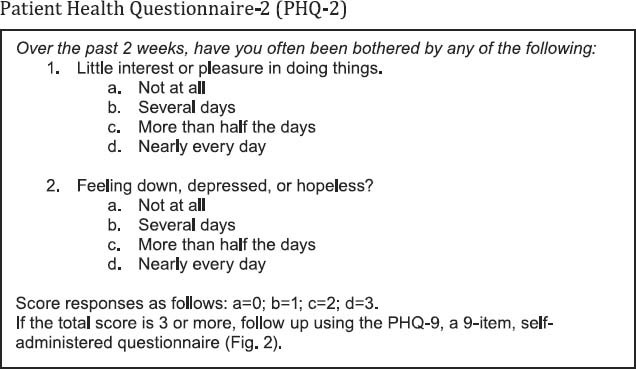
Fig. 1 The Patient Health Questionnaire-2 (PHQ-2) is a simple 2-question assessment that has been validated to identify currently depressed patients. Developed by Drs. Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke, and colleagues, with an educational grant from Pfizer Inc. No permission required to reproduce, translate, display, or distribute.
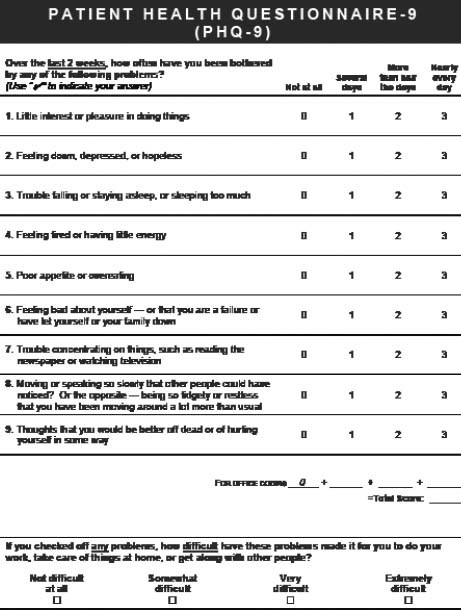
Fig. 2 The Patient Health Questionnaire-9 (PHQ-9) is a 5-minute, 9-question screening test that is administered in response to a PHQ-2 response score of 3 or higher. The PHQ-9 provides a provisional diagnosis of depression and a severity score that imparts reasonable sensitivity and specificity. A score greater than 10 suggests a high probability of depression, and scores greater than 20 are associated with severe functional impairment. Patients with scores over 10 should be referred for a more comprehensive evaluation and treatment plan. Developed by Drs. Robert L. Spitzer, Janet B.W. Williams, Kurt Kroenke, and colleagues, with an educational grant from Pfizer Inc. No permission required to reproduce, translate, display, or distribute.
Treatment of Depression Includes Pharmacologic Treatment and Behavioral Therapy
Although behavioral therapy might be effective in the long run, it has not been shown to be beneficial for treating depression in acute cardiac patients because of the need for immediate results. Selective serotonin reuptake inhibitors (SSRIs) are the preferred treatment for depression in patients with CAD, whereas tricyclic antidepressants and monoamine oxidase inhibitors are contraindicated due to their adverse cardiotoxic effects. Two SSRIs, sertraline and citalopram, have been shown in randomized clinical trials to be safe and efficacious in CAD patients with moderate or severe depression.29,30 Treatment (nonrandomized) of depression with an SSRI in patients with AMI enrolled in the Enhancing Recovery in Coronary Heart Disease Patients study yielded a 42% reduction in death or recurrent myocardial infarction when compared with depressed patients not treated with an antidepressant.31 Although there are as yet no randomized antidepressant trials proving that treatment of depression improves cardiac outcome in patients with CAD, treatment has been shown to be safe and might improve depressive symptoms, adherence to treatment, and medication compliance.
Summary
Why do we stay in prison when the door is wide open?
— Jalal ad-Din Rumi
Depression is an independent risk factor for the development of CAD. Patients with CAD have a high rate of depression, which worsens their prognosis. Screening CAD patients with the 2-question PHQ-2 to identify those at greatest risk of depression is strongly recommended, as is referring patients for further evaluation and possible treatment when depression has been identified by the PHQ-9. Treating depression is likely to improve cardiovascular outcomes.
The PHQs are in the public domain and free to use. To download and for more information, visit www.phqscreeners.com.
Footnotes
Address for reprints: Stephanie A. Coulter, MD, Cardiology Department, Texas Heart Institute at St. Luke's Episcopal Hospital, 6770 Bertner St. (C550B), Houston, TX 77030
E-mail: scoulter@texasheart.org
Presented at the 2nd Annual Symposium on Risk, Diagnosis and Treatment of Cardiovascular Disease in Women; Texas Heart Institute, Houston; 1 October 2011.
⋆ CME Credit
References
- 1.Brown JR, O'Connor GT. Coronary heart disease and prevention in the United States. N Engl J Med 2010;362(23):2150–3. [DOI] [PubMed]
- 2.Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, et al. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med 2006;21(1):30–8. [DOI] [PMC free article] [PubMed]
- 3.Lesperance F, Frasure-Smith N. Depression in patients with cardiac disease: a practical review. J Psychosom Res 2000;48 (4–5):379–91. [DOI] [PubMed]
- 4.Carney RM, Freedland KE. Depression, mortality, and medical morbidity in patients with coronary heart disease. Biol Psychiatry 2003;54(3):241–7. [DOI] [PubMed]
- 5.Bush DE, Ziegelstein RC, Patel UV, Thombs BD, Ford DE, Fauerbach JA, et al. Post-myocardial infarction depression. Evid Rep Technol Assess (Summ) 2005;(123):1–8. [PMC free article] [PubMed]
- 6.Mallik S, Spertus JA, Reid KJ, Krumholz HM, Rumsfeld JS, Weintraub WS, et al. Depressive symptoms after acute myocardial infarction: evidence for highest rates in younger women. Arch Intern Med 2006;166(8):876–83. [DOI] [PubMed]
- 7.Frasure-Smith N, Lesperance F. Recent evidence linking coronary heart disease and depression. Can J Psychiatry 2006;51 (12):730–7. [DOI] [PubMed]
- 8.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure: a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol 2006;48(8):1527–37. [DOI] [PubMed]
- 9.Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry 2007;29(5):409–16. [DOI] [PubMed]
- 10.Kessler RC. Epidemiology of women and depression. J Affect Disord 2003;74(1):5–13. [DOI] [PubMed]
- 11.Khawaja IS, Westermeyer JJ, Gajwani P, Feinstein RE. Depression and coronary artery disease: the association, mechanisms, and therapeutic implications. Psychiatry (Edgmont) 2009;6(1):38–51. [PMC free article] [PubMed]
- 12.Aromaa A, Raitasalo R, Reunanen A, Impivaara O, Helioaara M, Knekt P, et al. Depression and cardiovascular diseases. Acta Psychiatr Scand Suppl 1994;377:77–82. [DOI] [PubMed]
- 13.Dickens C, McGowan L, Percival C, Douglas J, Tomenson B, Cotter L, et al. Association between depressive episode before first myocardial infarction and worse cardiac failure following infarction. Psychosomatics 2005;46(6):523–8. [DOI] [PubMed]
- 14.Lauzon C, Beck CA, Huynh T, Dion D, Racine N, Carignan S, et al. Depression and prognosis following hospital admission because of acute myocardial infarction. CMAJ 2003;168 (5):547–52. [PMC free article] [PubMed]
- 15.Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med 2004;66(6):802–13. [DOI] [PubMed]
- 16.van Melle JP, de Jonge P, Spijkerman TA, Tijssen JG, Ormel J, van Veldhuisen DJ, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysis. Psychosom Med 2004;66(6): 814–22. [DOI] [PubMed]
- 17.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction [published erratum appears in Circulation 1998;97(7):708]. Circulation 1995;91(4):999–1005. [DOI] [PubMed]
- 18.ENRICHD Investigators. Enhancing Recovery in Coronary Heart Disease (ENRICHD) study intervention: rationale and design. Psychosom Med 2001;63(5):747–55. [PubMed]
- 19.Carney RM, Blumenthal JA, Catellier D, Freedland KE, Berkman LF, Watkins LL, et al. Depression as a risk factor for mortality after acute myocardial infarction. Am J Cardiol 2003;92(11):1277–81. [DOI] [PubMed]
- 20.Empana JP, Jouven X, Lemaitre RN, Sotoodehnia N, Rea T, Raghunathan TE, et al. Clinical depression and risk of out-of-hospital cardiac arrest. Arch Intern Med 2006;166(2):195–200. [DOI] [PubMed]
- 21.Lett HS, Blumenthal JA, Babyak MA, Sherwood A, Strauman T, Robins C, Newman MF. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med 2004;66(3):305–15. [DOI] [PubMed]
- 22.Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res 2002;53(4):897–902. [DOI] [PubMed]
- 23.Laghrissi-Thode F, Wagner WR, Pollock BG, Johnson PC, Finkel MS. Elevated platelet factor 4 and beta-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biol Psychiatry 1997;42(4):290–5. [DOI] [PubMed]
- 24.Maes M, Smith R, Christophe A, Vandoolaeghe E, Van Gastel A, Neels H, et al. Lower serum high-density lipoprotein cholesterol (HDL-C) in major depression and in depressed men with serious suicidal attempts: relationship with immune-inflammatory markers. Acta Psychiatr Scand 1997;95 (3):212–21. [DOI] [PubMed]
- 25.Carney RM, Freedland KE, Eisen SA, Rich MW, Jaffe AS. Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychol 1995;14(1):88–90. [DOI] [PubMed]
- 26.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med 2000;160(14):2101–7. [DOI] [PubMed]
- 27.Feinstein RE, Blumenfield M, Orlowski B, Frishman WH, Ovanessian S. A national survey of cardiovascular physicians' beliefs and clinical care practices when diagnosing and treating depression in patients with cardiovascular disease. Cardiol Rev 2006;14(4):164–9. [DOI] [PubMed]
- 28.Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lesperance F, et al. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation 2008;118(17): 1768–75. [DOI] [PubMed]
- 29.Lesperance F, Frasure-Smith N, Koszycki D, Laliberte MA, van Zyl LT, Baker B, et al. Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trial [published erratum appears in JAMA 2007;298(1):40]. JAMA 2007;297(4):367–79. [DOI] [PubMed]
- 30.Glassman AH, O'Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT Jr, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA 2002;288(6):701–9. [DOI] [PubMed]
- 31.Taylor CB, Youngblood ME, Catellier D, Veith RC, Carney RM, Burg MM, et al. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry 2005;62(7):792–8. [DOI] [PubMed]


