Abstract
Herpes zoster is relatively uncommon after surgery in immunocompetent patients. To our knowledge, there have been no reports of herpes zoster after the resection of a thoracic schwannoma. We report the case of a 48-year-old woman in whom acute shingles developed after the video-assisted thoracic surgical resection of a posterior mediastinal schwannoma adjacent to the 4th thoracic vertebral body. The patient recovered after receiving timely antiviral therapy.
Rash and pain are common in patients who have wound infections and contact dermatitis after surgery, so the possible reactivation of varicella virus might not be prominent in the surgeon's mind. This case serves as a reminder that viral infections such as shingles should be considered in the differential diagnosis of postoperative erythema and pain.
Key words: Diagnosis, differential; herpes zoster/diagnosis/epidemiology/etiology; postoperative complications; skin diseases, viral/diagnosis/drug therapy; thoracic surgery, video-assisted; virus activation
Herpes zoster (shingles) results from the reactivation of varicella-zoster virus (VZV) in the dorsal root ganglia. Shingles has been reported after mechanical trauma, the transplantation of organs, and certain surgical procedures.1–3 However, we found no report of herpes zoster after the resection of a thoracic schwannoma. Schwannoma, also known as neurilemoma, is derived from the Schwann cell, which is responsible for myelination of the peripheral nervous system. Schwannoma is second to neurofibroma among the most common peripheral nerve tumors. Thoracic schwannoma is usually benign; however, it often requires resection in order to exclude malignancy and prevent compressive symptoms.4 We report the case of a woman in whom acute shingles developed after the video-assisted thoracic surgical (VATS) resection of a right-sided thoracic schwannoma.
Case Report
A 48-year-old woman presented at our clinic with a newly discovered mass in the right posterior mediastinum at the level of the 4th thoracic vertebral body. This mass had been detected on magnetic resonance imaging (MRI), which was performed when the patient had recently visited a spine surgeon because of a sharp pain in her upper back with constant dull pain between the scapulae. The pain had failed to resolve with the use of muscle relaxants and nonsteroidal anti-inflammatory drugs (NSAIDS) several weeks after a workplace accident. The mass was 2.8 cm in diameter, sharply circumscribed and ovoid, and contiguous with the right anterolateral aspect of the T4 vertebral body. On MRI, the mass had yielded an inhomogeneous, hyperintense T2 signal and a short T1 inversion recovery signal with an intermediate T1 signal. The adjacent T4 vertebral body had a normal marrow signal. The mass did not appear to arise from the vertebral body itself (Fig. 1).
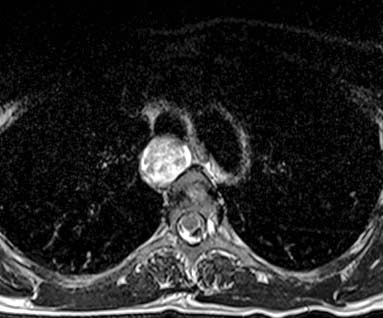
Fig. 1 T2-weighted magnetic resonance image, with an inhomogeneous, hyperintense signal of the posterior mediastinal mass anterolateral to the spine.
The patient had no dyspnea, orthopnea, hemoptysis, dysphagia, or reflux symptoms. Her medical history included migraine headaches. No surgical procedures had ever been performed on her neck, thorax, abdomen, or spine. She took no medications other than NSAIDS for relief of symptoms. She was immunocompetent and had never been treated for cancer. As a child, she had had an uncomplicated case of varicella zoster (chickenpox). She had smoked occasionally while in college but had not used tobacco in at least 20 years. On physical examination, there was reproducible point tenderness at the upper thoracic spine to the right of the T4 vertebral body, but no palpable masses. She had no deficits of movement or sensation.
Because of the unusual location of the mass, the patient was advised to undergo a tissue biopsy before surgical excision. An esophageal ultrasound-guided biopsy revealed an intact interface between the mass and the esophagus, suggesting no invasion. Anatomic pathologic results from the biopsy showed hypocellular neural tissue of benign appearance, with positive staining for S-100 protein and negative staining for desmin and smooth-muscle actin. All findings were consistent with neurofibroma or schwannoma.3
The patient underwent a right VATS resection of the mass. Two 1-cm ports were inserted, one at the 5th intercostal space below the tip of the right scapula and the other at the 6th intercostal space at the anterior axillary line. A 2-cm utility incision was made at the 4th intercostal space at the anterior axillary line. The mass was in the posterior mediastinum beneath the pleura without involvement of the trachea or esophagus (Fig. 2). The pleura was sharply divided with Endo Shears™ (Covidien; Mansfield, Mass), and the mass was enucleated by means of blunt dissection and with use of a LigaSure™ bipolar divider (Valleylab, part of Covidien Energy-Based Devices; Boulder, Colo). The mass was placed in an Endo Catch™ bag (Covidien) and removed through the anterior utility port. A 32F chest tube was placed in the lower anterior port. The patient tolerated the procedure well. The chest tube was removed on postoperative day 1, and the patient was then discharged from the hospital. Pathologic examination revealed a schwannoma with Verocay bodies and Antoni A and B components, with no malignant features.
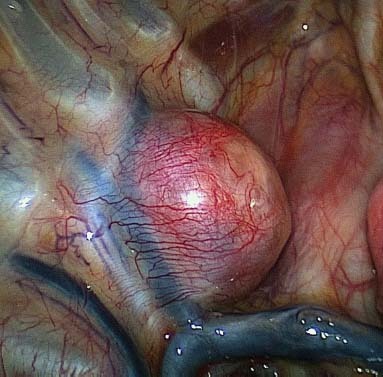
Fig. 2 Photograph shows a schwannoma in the posterior mediastinum beneath the pleura, without involvement of the trachea or esophagus.
The patient presented at our clinic 1 week after surgery with a 2-day history of pain and erythema in a band-like T6 dermatomal distribution along her right side (Fig. 3). She was afebrile, and all incisions were healing well. There was no evidence of wound infection or contact dermatitis. The erythema was confluent, and there were no lesions. On the basis of these symptoms and a physical examination, the diagnosis was acute shingles. The patient was prescribed valacyclovir for 10 days. Two days after her office visit, papules and then vesicles developed along her right side in the same band-like T6 dermatomal distribution. Three weeks after the diagnosis of herpes zoster, the patient was seen in the clinic without any erythema or scarring related to vesicle formation or post-herpetic neuralgia.

Fig. 3 Photograph shows herpes zoster underneath the right breast, evidenced by band-line erythema in T6 distribution, which did not cross the midline.
Discussion
To our knowledge, this is the first report of herpes zoster after the resection of a thoracic schwannoma. Before the availability of the VZV vaccine, VZV had afflicted 90% of adults before the age of 30 years; accordingly, most adults harbor the virus within their dorsal root ganglia.1 Herpes zoster is recognizable from the unique dermatomal distribution of the rash, which is unilateral and does not cross the midline.1 In the absence of recent trauma to the affected area and resultant changes to the skin consistent with the nature of the trauma, the diagnosis of herpes zoster can readily be made by most practitioners in the proper clinical setting. However, when erythema is seen 1 week after surgery around the area of the incisions, herpes zoster is not likely to be the first thought in the surgeon's mind. Wound infections and contact dermatitis from antiseptic preparation or adhesive bandaging are two of the more common causes of such findings. In an immunocompetent patient and an uncomplicated surgical case, and with the absence of classical features of wound infection, bacterial involvement is less likely. Especially after VATS and the insertion and removal of a chest tube, discomfort along the surgical site can easily be attributed to expected postoperative pain. Complicating the diagnosis of herpes zoster at a postoperative surgical site is the possible absence of papules early in the course of the disease.5 Clinicians often miss the brief erythematous and macular phase that precedes the rapid appearance of papules and then vesicles.5 Prompt response to antiviral therapy was confirmatory in our patient.
Surgeons are skilled at identifying postoperative wound infections, because these are so commonly encountered. Our patient's skin did not have the appearance of a wound infection, which helped guide the therapy; however, had antibiotics been administered, the rash would not have improved, and a progression to papules and crusting would have occurred. Massad and colleagues3 used lack of response to appropriate antibiotic therapy to rule out both bacterial and microbial involvement in a patient who developed shingles after thoracic sympathectomy for hyperhidrosis. If the patient is seen clinically during this erythematous and macular phase, the surgeon might recognize the characteristic lesions of herpes zoster and treat the patient accordingly. Clinical symptoms are the primary avenue for the diagnosis of shingles; however, if doubt exists, VZV can be expressed via polymerase chain reaction or be cultured in the laboratory.5
We speculate that intraoperative manipulation of the schwannoma or trauma to the intercostal nerve during insertion of the ports reactivated the VZV in our patient's dorsal root ganglia and led to acute shingles. In case-control studies, trauma has been associated with the development of herpes zoster within 1 month of an injury.2 Reactivation of the virus in our patient could have resulted from direct pressure on the intercostal nerve bundles by thoracoscopic instruments.3
Our patient's rapid recovery can be attributed to the timely administration of antiviral therapy. Although the condition is rare, we wish to draw attention to the possible development of herpes zoster after the resection of a thoracic schwannoma, and the importance of differential diagnosis when postoperative rash and pain occur.
Footnotes
Address for reprints: Min P. Kim, MD, Department of Surgery and Weill Cornell Medical College, The Methodist Hospital, SM 1661, 6550 Fannin St., Houston, TX 77030
E-mail: mpkim@tmhs.org
References
- 1.Tan HH, Goh CL. Viral infections affecting the skin in organ transplant recipients: epidemiology and current management strategies. Am J Clin Dermatol 2006;7(1):13–29. [DOI] [PubMed]
- 2.Thomas SL, Wheeler JG, Hall AJ. Case-control study of the effect of mechanical trauma on the risk of herpes zoster. BMJ 2004;328(7437):439. [DOI] [PMC free article] [PubMed]
- 3.Massad MG, Navarro RA, Rubeiz H, Kpodonu J, Karol J, Blacha M, Evans A. Acute postoperative shingles after thoracic sympathectomy for hyperhidrosis. Ann Thorac Surg 2004; 78(6):2159–61. [DOI] [PubMed]
- 4.Yamaguchi M, Yoshino I, Fukuyama S, Osoegawa A, Kameyama T, Tagawa T, Maehara Y. Surgical treatment of neurogenic tumors of the chest. Ann Thorac Cardiovasc Surg 2004;10(3):148–51. [PubMed]
- 5.Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, et al. Recommendations for the management of herpes zoster. Clin Infect Dis 2007;44 Suppl 1:S1–26. [DOI] [PubMed]


