Abstract
Objective
To assess evidence of the impact of Picture Archiving and Communication Systems (PACS) on clinicians' work practices in the intensive care unit (ICU).
Methods
We searched Medline, Pre-Medline, CINAHL, Embase, and the SPIE Digital Library databases for English-language publications between 1980 and September 2010 using Medical Subject Headings terms and keywords.
Results
Eleven studies from the USA and UK were included. All studies measured aspects of time associated with the introduction of PACS, namely the availability of images, the time a physician took to review an image, and changes in viewing patterns. Seven studies examined the impact on clinical decision-making, with the majority measuring the time to image-based clinical action. The effect of PACS on communication modes was reported in five studies.
Discussion
PACS can impact on clinician work practices in three main areas. Most of the evidence suggests an improvement in the efficiency of work practices. Quick image availability can impact on work associated with clinical decision-making, although the results were inconsistent. PACS can change communication practices, particularly between the ICU and radiology; however, the evidence base is insufficient to draw firm conclusions in this area.
Conclusion
The potential for PACS to impact positively on clinician work practices in the ICU and improve patient care is great. However, the evidence base is limited and does not reflect aspects of contemporary PACS technology. Performance measures developed in previous studies remain relevant, with much left to investigate to understand how PACS can support new and improved ways of delivering care in the intensive care setting.
Keywords: Intensive care, radiology information systems, PACS, evaluation studies, work innovation, health informatics, evaluation, qualitative research, health services research, decision support, qualitative/ethnographic field study, statistical analysis of large datasets, measuring/improving outcomes in specific conditions and patient subgroups, measuring/improving patient safety and reducing medical errors, improving healthcare workflow and process efficiency
Introduction
Printing CT and MRI exams for interpretation is like printing your email in order to read it (Hirschorn, p 31)
Picture Archiving and Communication Systems (PACS) are a unique technology which provide a ‘centralised repository for all imaging data’ (Faggioni, p 2542) and deliver diagnostic images (eg, x-rays, CT scans, MRI scans) and radiology reports electronically to clinicians at the point-of-care, negating the requirement for a film-based system. PACS was expected to revolutionize and streamline the delivery of healthcare, assisting communication between radiologists and clinicians, improving clinical decision-making, and facilitating more efficient patient care processes.3–6 The last 30 years has seen PACS evolve from in-house radiology systems to fully fledged hospital-wide commercial systems integrated with electronic medical records and incorporating technologies such as voice recognition and computer-aided diagnosis as hospitals establish paperless systems.2 5 7 8 In the USA 76% of hospitals reported using PACS in 2008,9 and in England and Scotland a national roll-out of PACS has been completed with the remainder of UK hospitals implementing it by 2012.10 Despite its widespread use and the great technological advances, the question remains, has PACS simply automated the process of imaging in healthcare, as the introduction of email initially did to written communication, or has it revolutionized clinical practice and led to new ways of working?11 Although PACS has been in existence for 30 years, this question has received little research attention.
A number of studies have been conducted to determine if PACS achieves its goals of improving efficiency and effectiveness within health systems. These studies focus on its impacts on workflow, roles, patient outcomes, and costs, with variable conclusions.12–22 Much research attention has focused on gains in workflow efficiencies associated with PACS, particularly in radiology departments.12–15 22 With the integration of PACS into a number of medical units outside radiology, the intensive care unit (ICU) is one clinical area where PACS has the potential to significantly change work practices.23 The ICU is a ‘complex’ and ‘data-rich environment’24 25 where clinicians continuously multi-task and utilize multiple information sources in order to provide optimum care for critically ill patients. Images are integral to patient care,26–29 with high volumes of imaging studies conducted in ICUs daily.30–32 Rapid access to these to support decision-making can be of crucial importance. With the potential for imaging results to impact dramatically on a patient's care, the ICU provides a good setting to assess how PACS can impact on and lead to innovation in clinical work practices. To date no synthesis of the evidence to investigate the effects of PACS in the complex and demanding environment of the ICU has been performed.
We aimed to conduct a systematic review to assess evidence of the impact of the introduction of PACS on clinicians' work practices in the ICU, published between 1980 and 2010. This 30-year period provides an opportunity to examine changes in the nature and outcomes of studies over time within a context of evolving technology. A further objective of our review was to synthesize the employed core indicators, assess their validity, draw conclusions about their value for contemporary studies of PACS and clinicians' work in the ICU, and identify areas for future research.
Methods
Search strategy
We searched Medline, Pre-Medline, CINAHL, EMBASE, and the SPIE Digital Library (http://spiedigitallibrary.org) between 1980 and September 2010 using Medical Subject Headings and keywords. The full search strategy is shown in table 1. We used multiple terms to identify clinician work practices. We restricted the search to English articles and hand searched the reference lists of included articles.
Table 1.
Search strategy
| Database | Search terms |
| Medline, Pre-Medline |
|
| CINAHL |
|
| EMBASE |
|
| SPIE Digital Library‡ |
|
| |
| ‘Picture archiving and communication system’ OR PACS (searched within the results for ‘intensive care’) |
For each search we also included ‘NOT pulmonary artery catheter OR peripheral artery catheter’ as these terms are also commonly abbreviated to PACS.
Medical Subject Headings terms or subject headings, exploded where possible.
A number of similar searches were carried out in this database to capture all possible articles.
Study selection and exclusion criteria
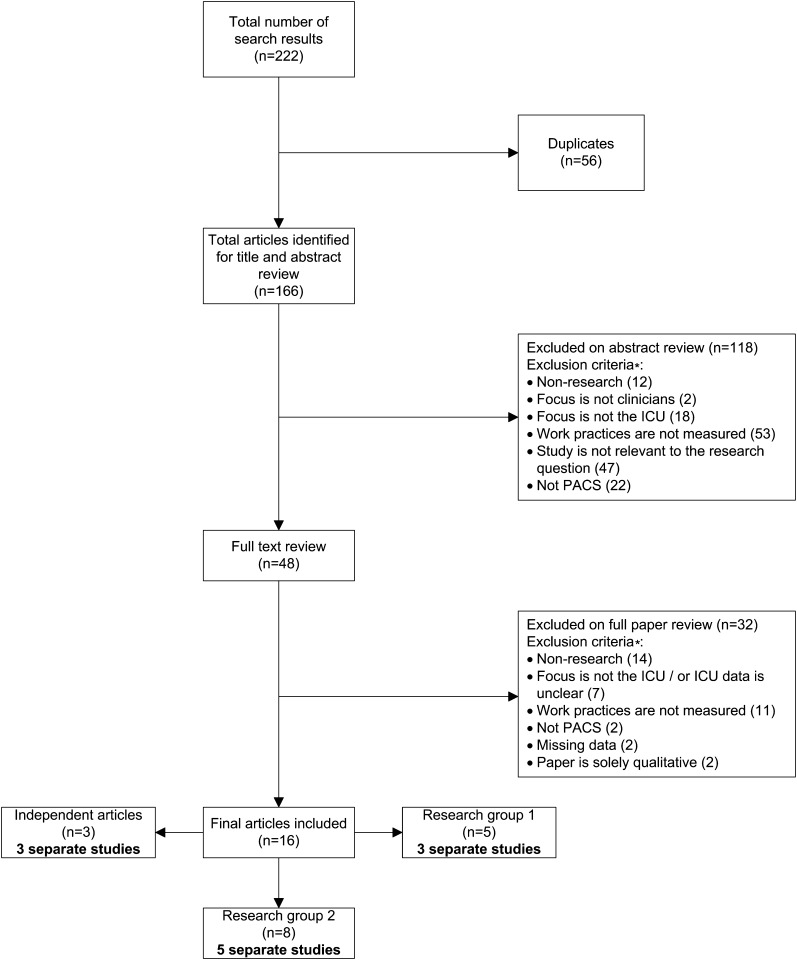
Our initial search yielded 222 articles (figure 1). Two reviewers independently undertook a title and abstract review of 166 articles after the removal of duplicates (n=56) to determine if papers met the inclusion criteria. If no abstract was available, the full text was reviewed. At this stage, 118/166 articles were excluded for the reasons shown in figure 1. The full texts of the remaining 48 papers were reviewed and consensus reached as to their inclusion. Study authors were contacted for further information if necessary. Only 16 articles met the inclusion criteria (figure 1).
Figure 1.
Process by which studies were included in the review. *Some papers were excluded under more than one exclusion criterion. PACS, Picture Archiving and Communication Systems.
Data extraction and synthesis
The following details for each paper were abstracted (if available): study design and methods, setting, country, participants, sample size, aims, outcomes, and results. Additionally, we also noted if the authors discussed integration of PACS with other systems, clinicians' attitudes toward PACS, and any limitations of the studies. Where the same data were reported across multiple manuscripts, these were combined and reported as one study. We assessed a number of potential factors that are often associated with bias, for example, the study origin and setting, when the study was conducted, and any comments made by the authors discussing why the study context may have affected particular results.
Due to the heterogeneous nature of the data, it was not possible to combine the results in a meta-analysis and so the results are reported according to the individual outcome measures described by the authors.
Results
Sixteen papers met the review criteria (figure 1), representing 11 studies, for the reasons shown in table 2.
Table 2.
Outcome measure summary
| Outcome measure | Definition(s) | Studies (n=11) | Papers |
| Availability of images | The time period from when an image is taken to the availability of the image | 5 | |
| Time to imaging information review by ICU physician | The time period from when an image is taken until the imaging information (image and/or report) is accessed by an ICU physician | 6 | |
| Viewing patterns | The time(s) of day clinicians access images | 3 | |
| Time associated with clinical decision-making |
|
7 | |
| Communication modes | Frequency and types of communication between ICU clinicians and the radiology department | 5 |
These authors each published preliminary or the same data across a number of articles.
Different aspects of the same study were reported on by these authors.
Both papers report on the same study data and so are counted as one study.
ICU, intensive care unit; PACS, Picture Archiving and Communication Systems.
Study characteristics
Three articles were published after 2000,33 40 45 but all were conducted prior to 2000. The majority were undertaken in the USA,34–39 41–48 primarily by two research groups at the University of Pennsylvania Medical Center36–39 45–48 and Duke University Medical Center,34 35 42–44 with the remainder in the UK.33 40 Study designs included three before-and-after studies,40 41 44 two surveys,33–35 two observational studies,42 43 46 and one cohort design.45 Additionally, three studies collected alternating film-only and PACS data.36–39 47 48 Full study characteristics and results are shown in supplementary online appendix 1. Table 2 summarizes the outcome measures reported by each study.
Availability of images
Of the five studies that reported on image availability,33–40 all but one found that access to images was quicker with PACS. The studies by Kundel et al36–38 and Redfern et al39 involved four data collection periods (analog film, first PACS, computed radiography (CR) film and second PACS). Kundel et al36–38 focused on non-routine (for specific problems that can sometimes be urgent) chest examinations and Redfern et al39 on routine images. Both reported a reduction in the median time to image availability with PACS. A survey administered by Cox et al33 to evaluate ICU staff perceptions of the impact of PACS found that 90% of users thought images were available more quickly and 72% perceived there were no longer problems due to lost images. Humphrey et al34 35 measured clinicians' perceptions of PACS utility via a questionnaire, with the majority of respondents reporting that images arrived faster in soft copy rather than with a hard copy film. A significant decrease (p<0.01) in the time to image availability for routine examinations from 30 and 45 min in the baseline periods to 15 min in the PACS period was found by Watkins et al40 in their pre- and post-PACS implementation study, but there was no difference for non-routine images.
Time to imaging information review by ICU physician
The time from when an image was taken until the imaging information was accessed by an ICU physician was considered in six studies,36–38 41–46 with four reporting a decrease in this time following the introduction of PACS.41–45 Andriole and colleagues41 carried out a before-and-after study to examine the impact of PACS on physician behavior and determined that the average time from image exposure to image review decreased from 2 h 32 min to 1 h 35 min. A decrease was similarly observed in the study by Redfern et al45 which looked at the time to review of non-routine images. This study also investigated the review times according to the workload of the physician using variables such as unit occupancy, severity of illness, and APACHE III score. There was a statistically significant association between an increased workload and the length of time it took for an image to be viewed without PACS. While this time decreased with PACS, it was not statistically significant.
In their observational study, Humphrey et al42 43 compared two ICUs in the same hospital with and without PACS (a surgical intensive care unit, SICU, and a medical intensive care unit, MICU, respectively). The mean time from image exposure to image viewing in the SICU was 39 min compared to 78 min for the MICU. The authors commented that the maximum time for which an image could be ‘useful’ to the clinicians was 1 h and determined that SICU clinicians were 9.5 times more likely to access imaging results within 1 h compared to MICU clinicians (p=0.0425). The authors followed this study by looking at the MICU following PACS implementation and found the mean time to viewing dropped to 55 min.44
Kundel et al36–38 looked at the time imaging information was first accessed via usual channels (looking at the image, asking a radiologist, or reading the radiologist's report) or the PACS workstation and stratified according to the reason for the examination (pulmonary and pleural problems, or position of tubes and catheters), although the authors did not specify which information channel was used. During the first PACS period there was a significant difference in the median time to physician access between CR film (3 h 48 min) and PACS (1 h 24 min). For position of tubes and catheter images, the time until imaging information was viewed was not significantly less when PACS was available. Similarly, in the study conducted by Shile et al,46 physicians had the choice to obtain images and reports through their usual communication channels (going to visit the radiology department or at a daily ICU conference) or through a PACS workstation. Only 44% of non-routine images were first viewed using PACS. The authors noted that 19% of films were not digitized and so could not be viewed using PACS and for those that were, they were not all available within 3 h due to the slow digitization process. Almost 50% of reports were received in the first 3 h following the examination, although for those reports that were viewed alongside the image, this occurred in hard copy rather than at the PACS workstation. For images first viewed at the workstation, 34% of reports were received at least 1 h later and thus not viewed simultaneously, due to the time required for report transcription.
Viewing patterns
Three studies reported on changes to the viewing pattern of images by ICU clinicians following PACS availability.39 42 43 47 De Simone et al47 found clinicians viewed images earlier in, and more evenly during, the day when images were available electronically. The authors commented that without PACS the majority of films were viewed at the daily radiologist conference in the ICU at 15:00 h. However with electronic images, these could be viewed by physicians on the morning ward rounds and they incorporated this into their routine. Similarly, in the study reported by Redfern et al,39 19% and 27% of images were accessed before the daily radiology conference (09:15 h) in the two PACS periods compared to 0% for the film periods (p<0.001). The observational study by Humphrey et al42 43 of the SICU and MICU found that in the SICU all images were viewed evenly over the hour following the examination, however in the MICU (no PACS), apart from urgent results, image viewing was scattered over a 2.5-h period.
Time associated with clinical decision-making
Seven studies reported on the impact of PACS on the time associated with image-based clinical decisions.33–41 47 48 Five discussed the time to clinical action, with two studies reporting an overall significant decrease in the time it took for a physician to take image-based clinical action as a result of the image being available in PACS.39 47 48 In one of these, De Simone and Arenson47 48 comment on the discovery of a pneumothorax when clinicians viewed the digital image, which allowed the patient to receive prompt treatment. Additionally, Andriole et al41 found that the time to clinical action decreased from an average of 3 h 21 min to 2 h 6 min following PACS introduction. Kundel et al36–38 also reported a significant decrease (p=0.03) in the time before a primary clinical action (related to the reason for the examination) was taken for non-routine images. When they divided the time to clinical action into (a) the time to image review by the clinician and (b) the time from image review until clinical action, they found that the decrease was a result of the reduced time to image review. The before-and-after study by Watkins et al40 found no difference between baseline and PACS periods for the time to clinical action for both routine and non-routine images, although the authors commented on the limited data available for non-routine image-based clinical actions. The majority of clinicians surveyed by Cox et al33 and Humphrey et al34 35 believed PACS led to quicker decision-making.
Communication modes
Communication with the radiology department was reported in five studies.36–39 41 46–48 Three found that PACS use led to a decrease in communication between physicians and radiologists.36–39 47 48 Kundel et al36–38 observed a significant reduction in the input physicians received from radiologists (p<0.05) in the first PACS period, with only 26% of images receiving radiologist input via the telephone, direct radiologist contact, or the radiologist's report. Similarly, the Redfern study39 also found a significant decrease in the level of radiologist–physician communication. However, there was little change in ‘film and report’ encounters, with the authors commenting that while some images were viewed before the radiology conference, the reports for these were discussed alongside the images at the daily conference. While De Simone and Arenson47 48 did not measure the significance of the changes, they did find there was less consultation with the radiologist. Physicians did, however, review the radiologists' reports, transmitted through PACS, for 50% of images, whereas the preliminary report was read for only 16% of images without PACS. These authors commented that the presence of PACS enhanced communication between physicians on the ward round through facilitating discussions regarding patient care. In contrast, Andriole et al41 found no difference in the level of consultation pre- and post-PACS. Shile et al46 reported that in the first 4 h after an image had been taken, physicians primarily visited the radiology department to verbally receive the radiologist's report. Only 25% of radiologist reports were first read on PACS and this occurred at least 2 h after the examination.
Discussion
Studies to date identify a number of areas in which PACS impacts on clinicians' work practices in the ICU, however the current evidence base to determine if PACS delivers on its promises is weak, inconsistent in some areas, and leaves many questions unanswered. Despite searching databases for papers published in the last 30 years, we identified only 16 papers which reported 11 studies, with two US research groups responsible for eight. All studies were conducted at a single site and these factors are likely to play a role in the generalizability of the results. No randomized controlled trials were conducted, although three out of the 11 studies utilized a before-and-after methodology40 41 44 and two alternated control periods with PACS periods.36–39 The lack of control groups in other studies invites concern. Further, four studies did not report or test the statistical significance of their findings. Although PACS is now considered ubiquitous in many ICUs worldwide, no empirical studies have been conducted in over 10 years, limiting the ability to draw firm conclusions about its impact on contemporary practice. Many of the ICUs in this review were early adopters of PACS, utilizing basic systems, and some operated PACS in parallel with a film-based system during studies, which is less likely to occur today, particularly as the aim of PACS is to provide filmless imaging.36–39 45–48 Much discussion has taken place surrounding the importance of PACS integration with electronic medical records and computerized provider order entry,2 5 12 which are also becoming commonplace in the ICU.49 The level at which PACS is used and how it is incorporated into clinical practice will be influenced by the extent to which it is integrated. None of the reviewed studies provided details of system integration for us to take this into account in our analysis.
Despite the limited number of studies, the evidence suggests a broad framework of relevance for future studies seeking to evaluate the influence of PACS on clinician work practices focusing on three core indicator areas: efficiency of work practices, work associated with clinical decision-making, and communication practices.
Efficiency of work practices
One of the many purported benefits of PACS is improved efficiencies in the delivery of healthcare.4 50 All studies measured various aspects of efficiency. One study commented on the eradication of issues associated with lost images,33 which is commonly cited as a benefit of PACS, negating the need for clinicians to spend time searching for images.12 51 52 Four studies demonstrated a reduction in the time to access an image with PACS, improving the efficiency of a clinician's work. Other studies did not show this level of efficiency. The authors of one study36–38 commented that the time to image availability included transport of the CR plates to an area away from the ICU, which then had to be scanned before being transmitted to the ICU PACS workstation. With the development of portable digital radiography, substantial improvements in efficiencies are likely to have been achieved.53 A few studies demonstrated clinicians accessing and viewing images earlier, due to the ability to now view images when required on the ward round. This is consistent with recent literature.51 54 A recent qualitative study conducted across three ICUs in Australia also reported positive, although varied, changes to the structure of ward rounds following the implementation of PACS.55
Work associated with clinical decision-making
Informed clinical decision-making is vital in an ICU where a critically ill patient's condition can rapidly change and quick information access is essential. Ready availability of images through PACS can have positive effects on clinical decision-making16 52 54 56 and this was perceived to be the case in two studies.33–35 When times to clinical action were measured in other studies, the results were inconsistent.36–41 47 48 Many organizational factors in the ICU57 can affect decision-making. Kundel and Watkins both discuss potential factors that may have influenced their ‘negative’ results,36 40 such as the lack of a ‘flag’ to signify that the image was available. This could result in delayed clinical action, as also suggested by Peer et al.54 The presence of PACS alone will not allow the ICU to reap the benefits of more timely decision-making if the work processes, such as a ‘flag’ to signal image availability, are not in place to allow clinicians to take advantage of results upon which clinical actions, such as changing medications or adjusting a tube position, are dependent.
Communication practices
Effective communication is of crucial importance in the delivery of healthcare generally57 58 and also in the ICU.59 60 However, as PACS has developed, concerns have arisen that it changes communication between clinicians and radiologists,61 62 potentially causing clinicians to view and interpret images independently and without the aid of expert radiology advice.56 Three studies in our review reported a decrease in clinician–radiologist communication after the introduction of PACS.36–39 47 48 The changes to image viewing patterns, as highlighted above, are likely to have altered the clinician's requirement to regularly visit the radiology department for film and/or report review, a common practice before the introduction of PACS. While communication processes have become more electronic in nature, some continue to encourage face-to-face conferences,15 55 as highlighted by one ICU in our review.39 Two studies displayed no changes in communication,41 46 corresponding with the inconsistencies reported in the literature regarding PACS and communication processes.15 52 54 63
PACS also creates opportunities for enhanced shared decision-making and has been found to improve communication processes within clinician groups12 51 64 and between clinicians and radiologists,12 22 54 65 enhancing clinical discussions and decision-making. However, only one of our included studies commented on this.47 48
Implications for future research
Despite the ubiquitous presence of PACS in many ICUs, the findings from this review and others66 suggest that more research is required. PACS are being integrated with electronic clinical information systems with increasingly sophisticated features including decision support functionalities, voice recognition, and image manipulation technologies, yet this review has starkly highlighted the absence of research on how practice changes, or fails to change, as a result of these technological advances.
Regardless of the marked improvements in PACS technology since the included studies were published, the three core indicator areas synthesized from the existing research evidence remain relevant and they should continue to be a focus for future studies. While the studies do not necessarily show profound innovative changes in the way clinicians undertake their daily work, the potential of PACS to increase efficiencies and influence clinical decision-making may only be realized, as Siegel et al suggest,67 if an effort is made by clinicians to redesign their work flow, access images earlier than they previously would have, and integrate PACS into their work practice. A recent study conducted in three ICUs where PACS is integrated with clinical ordering and results systems (one ICU had access to PACS at the bedside), found that expected behaviors, such as integrating viewing of images during ward rounds at the bedside, did not occur at the site with point-of-care terminals.55 This was despite clinicians reporting that bedside availability of PACS was a great advantage in their ICU. However, doctors from the site with only centralized PACS access consistently navigated between the bedside and the work station in order to view images during ward rounds. With the increasing use worldwide of mobile technologies such as tablets and iPads, great potential also exists for such technologies to be used within clinical areas such as the ICU to allow clinicians instant access to imaging information, particularly on ward rounds for example, where point-of-care terminals are not always available.68 This would be an area worthy of future investigation.
Future research should prioritize the refinement of outcome measures utilized in the current studies and the design of new objective indicator measures to understand how PACS does indeed impact on efficiency, decision-making, and communication practices in the ICU, as well as the implications for patient care. The context and organizational nature of the ICU will influence how PACS and their associated technologies impact and transform work practices. A literature review carried out by Maslove et al on the use of computerized provider order entry in the ICU environment concluded that a ‘lack of compelling evidence demonstrating its value’ was apparent and highlighted the importance of taking a socio-technical approach for future evaluations.69 Such conclusions are no less true for PACS and further research should take the context of the ICU into account when developing and refining these indicators. However, it will likely be difficult to conduct any before-and-after studies with PACS now commonplace in many ICUs. Thus the early studies presented in this review provide some useful indicators of baseline experiences of ICUs pre-PACs which can assist in the interpretation of future findings.
The challenge for future researchers is to examine how the definitions of some of the specific outcome measures (table 2) require refinement to take account of the changes in PACS technology. While the majority of the measures continue to be relevant, there is no doubt that contemporary PACS allows for quicker availability of images and image review than that in the included studies and so a measurement such as ‘availability of images’, as quantified by Kundel et al36 for example, is not likely to be as important today. However, the inclusion of technologies such as voice recognition software, ought to impact on the availability of imaging reports alongside images and thus refinement of the ‘availability’ measure would be a worthy adaptation.
Limitations
Despite using a broad search strategy, we found only 16 papers, which reported on a total of 11 studies. It is possible we may have missed papers that were indexed under other terms, used different key words, or were published in the gray literature or in languages other than English, resulting in a publication bias. Due to the heterogeneous nature of the studies, we were unable to conduct a full quality assessment and so synthesized the results according to the outcomes presented by the authors, rather than a meta-analysis. We only included quantitative studies, however these can often be one-dimensional and, as suggested above, there is a need to look beyond quantitative studies in future work.
Conclusion
Our review highlights that within the ICU setting limited evidence exists to suggest that ‘the perceived benefits of PACS match well the proclaimed benefits’.51 Certainly, it is difficult to draw firm conclusions on how PACS may have significantly changed clinical practice on a large scale. Evidence of change exists in some specific areas of work and PACS has great potential to improve clinical work practices in the ICU, thus improving patient care.12 16 The framework of three core indicator areas synthesized from the key outcome measures and results provides the basis for much needed further investigations of the impact of PACS in supporting new and improved ways of delivering quality, safe, and efficient care.
Supplementary Material
Acknowledgments
The authors thank Ms Anne Marks for assistance in study selection and initial data extraction.
Footnotes
Funding: This review was supported by an Australian Research Council linkage grant in partnership with Sydney South West Area Health Service (LP0989144). The funding source had no role in the design, conduct, or reporting of this review.
Competing interests: None.
Contributors: All authors contributed to the conception and design and interpretation of data. IH analyzed the data and drafted the article and AG and JW critically reviewed and revised it accordingly. All authors approved the final version.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hirschorn DS. Introduction. In: Dreyer KJ, Hirschorn DS, Thrall JH, et al., eds. PACS: A Guide to the Digital Revolution. New York: Springer, 2006:3–7 [Google Scholar]
- 2.Faggioni L, Neri E, Castellana C, et al. The future of PACS in healthcare enterprises. Eur J Radiol 2011;78:253–8 [DOI] [PubMed] [Google Scholar]
- 3.Caramella D. Is PACS research and development still necessary? Int Congr Ser 2005;1281:11–14 [Google Scholar]
- 4.Huang HK. Enterprise PACS and image distribution. Comput Med Imaging Graph 2003;27:241–53 [DOI] [PubMed] [Google Scholar]
- 5.van de Wetering R, Batenburg R. A PACS maturity model: a systematic meta-analytic review on maturation and evolvability of PACS in the hospital enterprise. Int J Med Inform 2009;78:127–40 [DOI] [PubMed] [Google Scholar]
- 6.Warburton RN. Evaluation of PACS-induced organizational change. Int J Biomed Comput 1992;30:243–8 [DOI] [PubMed] [Google Scholar]
- 7.Wiley G. The prophet motive: how PACS was developed and sold. Imaging Economics 2005. http://www.imagingeconomics.com/issues/articles/2005-05_01.asp (accessed 12 Jan 2012). [Google Scholar]
- 8.Lemke HU. Short history of PACS (Part II: Europe). Eur J Radiol 2011;78:177–83 [DOI] [PubMed] [Google Scholar]
- 9.HIMSS Foundation Picture Archiving and Communication Systems: A 2000-2008 Study. 2010. http://www.himss.org/foundation/docs/PACS_ResearchWhitePaperFinal.pdf?src=pr (accessed 1 Nov 2010). [Google Scholar]
- 10.Sutton LN. PACS and diagnostic imaging service delivery–a UK perspective. Eur J Radiol 2011;78:243–9 [DOI] [PubMed] [Google Scholar]
- 11.Westbrook JI, Braithwaite J. Will information and communication technology disrupt the health system and deliver on its promise? Med J Aust 2010;193:399–400 [DOI] [PubMed] [Google Scholar]
- 12.van de Wetering R, Batenburg R, Versendaal J, et al. A balanced evaluation perspective: picture archiving and communication system impacts on hospital workflow. J Digit Imaging 2006;19(Suppl 1):10–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mackinnon AD, Billington RA, Adam EJ, et al. Picture archiving and communication systems lead to sustained improvements in reporting times and productivity: results of a 5-year audit. Clin Radiol 2008;63:796–804 [DOI] [PubMed] [Google Scholar]
- 14.Nitrosi A, Borasi G, Nicoli F, et al. A filmless radiology department in a full digital regional hospital: quantitative evaluation of the increased quality and efficiency. J Digit Imaging 2007;20:140–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siegel EL, Reiner BI. Filmless radiology at the Baltimore VA Medical Center: a 9 year retrospective. Comput Med Imaging Graph 2003;27:101–9 [DOI] [PubMed] [Google Scholar]
- 16.Crowe B, Sim L. An assessment of the effect of the introduction of a PACS and RIS on clinical decision making and patient management at Princess Alexandra Hospital Brisbane, Australia: Final report-December 2004. Int Congr Ser 2005;1281:964–7 [Google Scholar]
- 17.Bryan S, Weatherburn GC, Watkins JR, et al. The benefits of hospital-wide picture archiving and communication systems: a survey of clinical users of radiology services. Br J Radiol 1999;72:469–78 [DOI] [PubMed] [Google Scholar]
- 18.Hurlen P, Østbye T, Borthne A, et al. Introducing PACS to the late majority. A longitudinal study. J Digit Imaging 2010;23:87–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Findlay G. The filmless ICU: introduction of computed radiology and PACS. Care of the Critically Ill 2000;16:180–3 [Google Scholar]
- 20.Hayt DB, Alexander S, Drakakis J, et al. Filmless in 60 days: the impact of picture archiving and communications systems within a large urban hospital. J Digit Imaging 2001;14:62–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watkins JR, Bryan S, Muris NM, et al. Examining the influence of picture archiving communication systems and other factors upon the length of stay for patients with total hip and total knee replacements. Int J Technol Assess Health Care 1999;15:497–505 [PubMed] [Google Scholar]
- 22.Fridell K, Edgren L, Lindsköld L, et al. The impact of PACS on radiologists' work practice. J Digit Imaging 2007;20:411–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steckel RJ. The current applications of PACS to radiology practice. Radiology 1994;190:50A–2A [DOI] [PubMed] [Google Scholar]
- 24.Mador RL, Shaw NT. The impact of a Critical Care Information System (CCIS) on time spent charting and in direct patient care by staff in the ICU: a review of the literature. Int J Med Inform 2009;78:435–45 [DOI] [PubMed] [Google Scholar]
- 25.Martich GD, Waldmann CS, Imhoff M. Clinical informatics in critical care. J Intensive Care Med 2004;19:154–63 [DOI] [PubMed] [Google Scholar]
- 26.Strange C. Infection in the intensive care unit: a clinician's view of the role of imaging. Semin Roentgenol 2007;42:7–10 [DOI] [PubMed] [Google Scholar]
- 27.Trotman-Dickenson B. Radiology in the intensive care unit (Part I). J Intensive Care Med 2003;18:198–210 [DOI] [PubMed] [Google Scholar]
- 28.Revell MA, Pugh M, Smith TL, et al. Radiographic studies in the critical care environment. Crit Care Nurs Clin North Am 2010;22:41–50 [DOI] [PubMed] [Google Scholar]
- 29.Horii SC, Mun SK, Elliott LP, et al. PACS clinical experience at Georgetown University. Int J Biomed Comput 1992;30:275–80 [DOI] [PubMed] [Google Scholar]
- 30.Carey B, kundel ML, Shile PE, et al. In situ evaluation of physician encounters with a PACS workstation in an MICU. Appl Radiol 1993;22:31–4 [Google Scholar]
- 31.Cho PS, Huang HK, Tillisch J, et al. Clinical evaluation of a radiologic picture archiving and communication system for a coronary care unit. Am J Roentgenol 1988;151:823–7 [DOI] [PubMed] [Google Scholar]
- 32.Hillis DJ, Crowe BL, McDonald IG, et al. Initial qualitative evaluation of computed radiography in an intensive care unit. Australas Radiol 1996;40:291–7 [DOI] [PubMed] [Google Scholar]
- 33.Cox B, Dawe N. Evaluation of the impact of a PACS system on an intensive care unit. J Manag Med 2002;16:199–205 [DOI] [PubMed] [Google Scholar]
- 34.Humphrey LM, Fitzpatrick K, Paine S, et al. Extended experience with digital radiography and viewing in an ICU environment. In: Jost RG, ed. Medical Imaging VI: PACS Design and Evaluation. Newport Beach, CA, USA: SPIE, 1992:408–14 [Google Scholar]
- 35.Humphrey LM, Fitzpatrick K, Paine SS, et al. Physician experience with viewing digital radiographs in an intensive care unit environment. J Digit Imaging 1993;6:30–6 [DOI] [PubMed] [Google Scholar]
- 36.Kundel HL, Seshadri SB, Langlotz CP, et al. Prospective study of a PACS: information flow and clinical action in a medical intensive care unit. Radiology 1996;199:143–9 [DOI] [PubMed] [Google Scholar]
- 37.Kundel HL, Seshadri SB, Langlotz CP, et al. Prospective comparison of the usage of conventional film and PACS based computed radiography for portable chest x-ray imaging in a medical intensive care unit. In: Jost RG, Dwyer III SJ, eds. Medical Imaging 1995: PACS Design and Evaluation: Engineering and Clinical Issues. San Diego, CA, USA: SPIE, 1995:302–9 [Google Scholar]
- 38.Kundel HL, Seshadri SB, Shile PE, et al. Evaluation of PACS in a medical intensive care unit: the effect of computed radiography. In: Jost RG, ed. Medical Imaging 1994: PACS: Design and Evaluation. Newport Beach, CA, USA: SPIE, 1994:481–7 [Google Scholar]
- 39.Redfern RO, Kundel HL, Polansky M, et al. Image workstation in a medical intensive care unit changes viewing patterns and timing of image-based clinical actions in routine portable chest radiographs. In: Jost RG, Dwyer III SJ, eds. Medical Imaging 1996: PACS Design and Evaluation: Engineering and Clinical Issues. Newport Beach, CA, USA: SPIE, 1996:298–306 [Google Scholar]
- 40.Watkins J, Weatherburn G, Bryan S. The impact of a picture archiving and communication system (PACS) upon an intensive care unit. Eur J Radiol 2000;34:3–8 [DOI] [PubMed] [Google Scholar]
- 41.Andriole KP, Storto ML, Gamsu G, et al. Impact and utilization studies of a PACS display station in an ICU setting. In: Jost RG, Dwyer III SJ, eds. Medical Imaging 1996: PACS Design and Evaluation: Engineering and Clinical Issues. Newport Beach, CA, USA: SPIE, 1996:286–9 [Google Scholar]
- 42.Humphrey LM, Fitzpatrick K, Atallah N, et al. Time comparison of ICUs with and without digital viewing systems. In: Jost RG, ed. Medical Imaging VI: PACS Design and Evaluation. Newport Beach, CA, USA: SPIE, 1992:402–7 [Google Scholar]
- 43.Humphrey LM, Fitzpatrick K, Atallah N, et al. Time comparison of intensive care units with and without digital viewing systems. J Digit Imaging 1993;6:37–41 [DOI] [PubMed] [Google Scholar]
- 44.Humphrey LM, Do Van M, Paine S, et al. Time comparison of a medical intensive care unit before and after installation of a digital viewing station. In: Jost RG, ed. Medical Imaging 1994: PACS: Design and Evaluation. Newport Beach, CA, USA: SPIE, 1994:452–5 [Google Scholar]
- 45.Redfern RO, Kundel HL, Polansky M, et al. A picture archival and communication system shortens delays in obtaining radiographic information in a medical intensive care unit. Crit Care Med 2000;28:1006–13 [DOI] [PubMed] [Google Scholar]
- 46.Shile PE, Kundel HL, Seshadri SB, et al. Factors affecting the electronic communication of radiological information to an intensive-care unit. J Telemed Telecare 1996;2:199–204 [DOI] [PubMed] [Google Scholar]
- 47.De Simone DN, Kundel HL, Arenson RL, et al. Effect of a digital imaging network on physician behavior in an intensive care unit. Radiology 1988;169:41–4 [DOI] [PubMed] [Google Scholar]
- 48.Arenson RL, Seshadri SB, Kundel HL, et al. Clinical evaluation of a medical image management system for chest images. Am J Roentgenol 1988;150:55–9 [DOI] [PubMed] [Google Scholar]
- 49.Lapinsky SE, Holt D, Hallett D, et al. Survey of information technology in intensive care units in Ontario, Canada. BMC Med Inform Decis Mak 2008;8:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hood MN, Scott H. Introduction to picture archive and communication systems. J Radiol Nurs 2006;25:69–74 [Google Scholar]
- 51.Pilling JR. Picture archiving and communication systems: the users' view. Br J Radiol 2003;76:519–24 [DOI] [PubMed] [Google Scholar]
- 52.Srinivasan M, Liederman E, Baluyot N, et al. Saving time, improving satisfaction: the impact of a digital radiology system on physician workflow and system efficiency. J Healthc Inf Manag 2006;20:123–31 [PubMed] [Google Scholar]
- 53.Lehnert T, Naguib NN, Ackermann H, et al. Novel, portable, cassette-sized, and wireless flat-panel digital radiography system: initial workflow results versus computed radiography. Am J Roentgenol 2011;196:1368–71 [DOI] [PubMed] [Google Scholar]
- 54.Peer R, Peer S, Sander H, et al. Radiography for intensive care: participatory process analysis in a PACS equipped and film/screen environment. In: Siegel EL, Huang HK, eds. Medical Imaging 2002: PACS and Integrated Medical Information Systems: Design and Evaluation. San Diego, CA, USA: SPIE, 2002:182–8 [Google Scholar]
- 55.Hains IM, Creswick N, Westbrook JI. Does PACS facilitate work practice innovation in the intensive care unit? In: Moen A, Andersen SK, Aarts J, et al., eds. Stud Health Technol Inform. Amsterdam: IOS Press, 2011:397–401 [PubMed] [Google Scholar]
- 56.Weatherburn G, Bryan S, Nicholas A, et al. The effect of a picture archiving and communications system (PACS) on diagnostic performance in the accident and emergency department. J Accid Emerg Med 2000;17:180–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zimmerman JE, Shortell SM, Rousseau DM, et al. Improving intensive care: observations based on organizational case studies in nine intensive care units: a prospective, multicenter study. Crit Care Med 1993;21:1443–51 [PubMed] [Google Scholar]
- 58.World Health Organisation Global Priorities for Patient Safety Research. Switzerland, 2009. http://whqlibdoc.who.int/publications/2009/9789241598620_eng.pdf (accessed 7 Feb 2010). [Google Scholar]
- 59.Hendel SA, Flanagan BT. Communication failure in the intensive care unit–learning from a near miss. Anaesth Intensive Care 2009;37:847–50 [DOI] [PubMed] [Google Scholar]
- 60.Reader TW, Flin R, Cuthbertson BH. Communication skills and error in the intensive care unit. Curr Opin Crit Care 2007;13:732–6 [DOI] [PubMed] [Google Scholar]
- 61.Mates J, Branstetter B, Morgan M, et al. ‘Wet reads’ in the age of PACS: technical and workflow considerations for a preliminary report system. J Digit Imaging 2007;20:296–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hayt DB, Alexander S. The pros and cons of implementing PACS and speech recognition systems. J Digit Imaging 2001;14:149–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Reiner BI, Siegel EL, Hooper F, et al. Impact of filmless imaging on the frequency of clinician review of radiology images. J Digit Imaging 1998;11:149–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tan SL, Lewis RA. Picture archiving and communication systems: a multicentre survey of users experience and satisfaction. Eur J Radiol 2010;75:406–10 [DOI] [PubMed] [Google Scholar]
- 65.Watkins J. A hospital-wide picture archiving and communication system (PACS): the views of users and providers of the radiology service at Hammersmith Hospital. Eur J Radiol 1999;32:106–12 [DOI] [PubMed] [Google Scholar]
- 66.Black AD, Car J, Pagliari C, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med 2011;8:e1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Siegel EL, Reiner B. Work flow redesign: the key to success when using PACS. J Digit Imaging 2003;16:164–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Choudhri AF, Radvany MG. Initial experience with a handheld device digital imaging and communications in medicine viewer: Osirix mobile on the iPhone. J Digit Imaging 2011;24:184–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Maslove DM, Rizk N, Lowe HJ. Computerized physician order entry in the critical care environment: a review of current literature. J Intensive Care Med 2011;26:165–71 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.