Abstract
Background
Electronic health records (EHR) have the potential to improve patient care through efficient access to complete patient health information. This potential may not be reached because many of the most important determinants of health outcome are rarely included. Successful health promotion and disease prevention requires patient-reported data reflecting health behaviors and psychosocial issues. Furthermore, there is a need to harmonize this information across different EHR systems.
Methods
To fill this gap a three-phased process was used to conceptualize, identify and recommend patient-reported data elements on health behaviors and psychosocial factors for the EHR. Expert panels (n=13) identified candidate measures (phase 1) that were reviewed and rated by a wide range of health professionals (n=93) using the grid-enabled measures wiki social media platform (phase 2). Recommendations were finalized through a town hall meeting with key stakeholders including patients, providers, researchers, policy makers, and representatives from healthcare settings (phase 3).
Results
Nine key elements from three areas emerged as the initial critical patient-reported elements to incorporate systematically into EHR—health behaviors (eg, exercise), psychosocial issues (eg, distress), and patient-centered factors (eg, demographics). Recommendations were also made regarding the frequency of collection ranging from a single assessment (eg, demographic characteristics), to annual assessment (eg, health behaviors), or more frequent (eg, patient goals).
Conclusions
There was strong stakeholder support for this initiative reflecting the perceived value of incorporating patient-reported elements into EHR. The next steps will include testing the feasibility of incorporating these elements into the EHR across diverse primary care settings.
Keywords: Common data elements, electronic health record, health behavior, meaningful use, measurement, measures, patient-centered, patient report, patient reported outcomes, primary care, prevention
Unhealthy behaviors are major contributors to costly chronic health conditions including heart disease, diabetes, cancer, and obesity that play a large role in the rising, unsustainable cost of healthcare. Recognizing the scope of this problem, the US Congress passed the Patient Protection and Affordable Care Act, expanding healthcare access to 30 million Americans and increasing focus on quality and patient-centered care.1 Further supporting this concern, the Health Information Technology for Economic and Clinical Health (HITECH) Act places new emphasis on the widespread and meaningful use of electronic health records (EHR).2 3
The Office of the National Coordinator for Health Information Technology within the Department of Health and Human Services and the Centers for Medicare and Medicaid Services (CMS) are responsible for implementing HITECH and coordinating efforts to facilitate the nationwide adoption of health information technology. The focus of HITECH is on promoting the exchange and meaningful use of health information to improve population health, reduce healthcare costs, and empower individuals to improve their health through the use of health information technology. The HITECH legislation also created an incentive programme for health professionals and hospitals to begin implementing and demonstrating the ‘meaningful use’ of EHR. In short, meaningful use requires that providers demonstrate the use of certified EHR technology in ways that can be measured through the electronic exchange of health information to improve the quality of care.2
The meaningful use programme has been organized as a multistage process to build up system capabilities with each stage increasing the bar for what constitutes meaningful use. Stage 1 is ongoing and includes basic EHR functionality (e-prescribing, maintaining active problems, medication, and allergy lists, etc). To demonstrate success the provider must report clinical quality measures (CQM) to CMS. CQM are endorsed standards for defining the logic for measurement of processes, outcomes, observations or treatments that relate to the meaningful use quality aims. CMS and the Office of the National Coordinator for Health Information Technology have recently released proposed criteria for stage 2 and are working to define criteria for stage 3 meaningful use, successive stages will have an increasing focus on improvements in quality and health outcomes.2 The development of well-validated CQM for behavioral health and psychosocial factors will be critical for promoting their inclusion in meaningful use.
While meaningful use of EHR has promise for improving health outcomes, there is a gap in current legislation and advancements in EHR technology as it relates to addressing key patient reported behavioral and psychological outcomes as well as other patient characteristics. From an epidemiological and behavioral perspective, it is clear that the rates of tobacco use, physical inactivity, poor diet, alcohol abuse, and other poor health behaviors are key preventable causes of death.4–6 Currently, only smoking behavior is addressed in the criteria for meaningful use; however, subsequent stages of the incentive programme are likely to include additional CQM addressing behavioral and psychosocial factors. Gordon and colleagues7 reviewed the cost-effectiveness of behavioral interventions to reduce smoking, improve eating habits, and increase regular physical activity. They concluded that behavioral interventions frequently produced positive outcomes at a lower cost than alternative treatments. Perhaps the strongest evidence for the cost effectiveness of behavioral interventions comes from the diabetes prevention programme.8 In that large multicentered trial, the cost per quality-adjusted life-year was US$1100 for the physical activity and nutrition intervention compared with US$31 000 for an intervention based on medication use.9 Furthermore, the benefit was maintained over an extended period of time.10 From a psychological perspective, strong evidence also exists that treating subclinical and identifying psychosocial conditions such as depression or anxiety can reduce the high costs of these disorders and lead to cost-effective treatment through primary care.11 12
While there are clear health outcome and care delivery benefits that would be associated with systematically collecting behavioral, psychological, and other patient-reported variables in EHR, there are practical limitations. Many clinical practices are under-staffed and under-resourced and struggle with meeting all of the current competing demands they face.13–15 The past decade has given rise to new mandates for practice change. Practices are being asked to re-engineer their activities and functions and transform themselves into patient-centered medical homes.16 HITECH and meaningful use are encouraging the adoption and implementation of EHR as well as mandating further workflow changes such as the expanded electronic capture of clinical data and electronic prescribing. Healthcare reform is even encouraging practices to reconsider their identity in the context of a larger care delivery system (eg, accountable care organizations). These competing demands and policy changes have led to a rapidly shifting landscape in which details such as behavioral and psychosocial measures, no matter how valuable, are likely to be lost or ignored. To be successful with systematically collecting these measures it is imperative that measures are standardized, practical, feasible, actionable, and consistent with these broader practice redesign initiatives.
Scientists from the health policy committee of the Society of Behavioral Medicine and the National Institutes of Health recently highlighted the need for a set of standards for core behavioral, psychological, and patient characteristics and identified a set of methodological criteria to identify appropriate measurement tools that could be integrated within EHR systems (box 1).17 The specific domains were identified because they are: (1) prevalent in the population; (2) strong determinants of health; (3) regularly encountered in primary care and public health settings; (4) relevant to how a physician delivers care; and (5) actionable (Glasgow et al).17 These domains also align well with the national prevention strategy released in the USA in July 2011.18 One of the main goals of the prevention strategy is to shift the focus of the healthcare system from responding to illness and disease to promoting prevention and wellness. The initiative also emphasizes the importance of standard metrics to measure progress.
Box 1. Targeted behavioral, psychological, and patient characteristic domains.
Behavioral characteristics
Eating patterns
Medication taking
Physical activity
Risky drinking
Sleep quality
Smoking/tobacco use
Substance use
Psychosocial characteristics
Anxiety and depression
Stress
Quality of life
Patient characteristics
Demographics
Health literacy/numeracy
Patient goals
The purpose of this paper is to describe a collaborative engagement process to involve key stakeholders from healthcare practice, consumer groups, researchers, policy makers, and healthcare organizations in the identification and recommendation of core behavioral, psychological, and patient characteristic data elements for inclusion in EHR. More specifically, the goal of the paper is to describe a mixed-methods approach that was used to track a three-step process of: (1) convening subject matter experts to identify and evaluate candidate data elements; (2) gathering feedback from a broad cross-section of stakeholders using the National Cancer Institute grid-enabled measures (GEM) wiki platform; and (3) developing consensus through a town hall meeting to engage scientists, practitioners, policy makers, and patient/consumer representatives. The resulting recommended data elements, along with the recommended frequency of administration for each domain, will be presented. In addition, we will discuss recommendations for the next steps and how this relates to the broader policy context.
Methods
Phases 1, 2, and 3 of the project, respectively, targeted the development of candidate measures in each domain, the rating of candidate measures using the GEM wiki, and finalizing (when possible) recommendations for specific data elements to be included in EHR.
Phase 1: identifying candidate measures
A multidisciplinary panel of subject matter experts was convened to complete phase 1 (see supplementary appendix 1, available online only, for a complete list of panel members). For each of the behavioral, psychological, and patient characteristic domains small working groups from the multidisciplinary panel examined available measurement tools. The working groups were instructed to consider a set of scientific and practical criteria in making their recommendations (table 1). Scientific criteria included reliability over time, several types of validity, breadth of applicability (cross-cultural studies; validation in Spanish and English), and sensitivity to change. Practical considerations for widespread implementation in the context of primary care weighed heavily in decision-making and included feasibility (brevity and burden to patients and staff), importance to primary care clinicians, being actionable, user friendly and transparent, cost/being in the public domain, and the extent to which an item or measure potentially enhanced patient engagement. All criteria were emphasized repeatedly throughout the three-phase process to help guide discussion and decisions. Based on the criteria, each working group recommended up to four practical measures as candidates for inclusion in EHR. In the case when a pre-existing candidate measure was not identified, the working groups were instructed to propose measures that aligned with existing measures.
Table 1.
Targeted behavioral, psychological, and patient characteristic domains
| Characteristic | Recommended criteria |
| Reliable | Especially test–retest (less on internal consistency) |
| Valid | Construct validity, criterion validity, established norms |
| Sensitive to change* | Longitudinal use, goal attainment tracking, repeated administration |
| Feasible* | Brief (generally three items or less); easy to score/interpret |
| Important to clinicians | Indices for health conditions that are prevalent, costly, challenging |
| Public health relevance | Can be related to HP 2020 goals |
| Actionable* | Realistic actions, reliable referral, immediate discussion, on-line resources, how easy or difficult would it be to develop a clinical response ‘toolkit’ |
| User friendly | Patient interpretability; face validity; meaningful to clinicians, public health officials, and policy makers |
| Broadly applicable | Available in English and Spanish, validated in different cultures and contexts |
| Cost | Publicly available or very low cost |
| Enhancing patient engagement | Having this information is likely to further patient involvement in their care and decision-making |
These criteria were given special emphasis.
Phase 2: wiki-facilitated ratings of candidate measures
Each of the expert panel working groups posted candidate measures and a summary of their recommendations on the GEM wiki (http://www.gem-beta.org), and key stakeholders were invited to submit ratings and comments. Stakeholder groups included those that represented primary care, consumer/patient groups, professional societies, scientists, regulators, and federal entities. Agencies and organizations invited to participate in the GEM wiki process can be found in table 2. Outreach activities occurred in February to April 2011 to engage stakeholder organizations and individuals and included outreach through newsletters and listservs, and communication with key stakeholders from different organizations to engage their members to participate.
Table 2.
Stakeholder agencies and organizations invited to participate in the process and those that attended phase 3 stakeholder meetings
| Organization | Attended key stakeholder meeting |
| Agency for Healthcare Research and Quality | Yes |
| American Academy of Family Physicians | Yes |
| American College of Preventive Medicine | Yes |
| American College of Sports Medicine | Yes |
| American Geriatrics Society | No |
| American Heart Association | Yes |
| American Medical Informatics Association | No |
| American Psychological Association | No |
| Center for the Advancement of Health | Yes |
| Centers for Medicare and Medicaid Services | No |
| Coalition for the Advancement of Health through Behavioral and Social Sciences Research | No |
| Consortium of Social Science Associations | No |
| Consumers Union | Yes |
| Epic Marketing (EHR vendor) | No |
| Federation of Associations in Behavioral and Brain Sciences | No |
| Geisinger Health System | Yes |
| Graham Center for Family Medicine | No |
| Group Health Cooperative | Yes |
| Health Research Services Administration/Bureau of Primary Care | Yes |
| Health Partners | Yes |
| HMO Research Network | No |
| Legacy Foundation | No |
| Microsoft Health Vault (Personal Health Record Vendor) | No |
| North American Primary Care Research Group | Yes |
| National Alliance on Mental Illness | No |
| National Cancer Institute, NIH | Yes |
| National Committee for Quality Assurance | Yes |
| National Heart, Lung, and Blood Institute, NIH | Yes |
| National Institute on Drug Abuse, NIH | Yes |
| National Institute of Diabetes and Digestive and Kidney Diseases | No |
| National Institute of Mental Health, NIH | Yes |
| National Institute of Nursing Research, NIH | Yes |
| National Quality Forum | Yes |
| NIDA Community Treatment Network | Yes |
| NIH Behavioral and Social Sciences Research Coordinating Committee | Yes |
| Office of Behavioral and Social Sciences Research, NIH | Yes |
| Office of the National Coordinator for Health Information Technology, HHS | Yes |
| Partnership for Prevention | No |
| Patients Like Me (personal health record vendor) | No |
| Preventive Cardiovascular Nurses Association | Yes |
| PROMIS Network—Patient Reported Outcomes Measurement Information System | Yes |
| Robert Wood Johnson Foundation | Yes |
| Society for Research on Nicotine and Tobacco | Yes |
| Society of Behavioral Medicine | Yes |
| Society of General Internal Medicine | Yes |
| Society of Teachers of Family Medicine | No |
| Substance Abuse and Mental Health Services Administration | No |
| US Department of Veterans Affairs | Yes |
The GEM tool originated several years ago from strategic efforts to bring population science into the collective domain of network and information technologies, more commonly described as grid and cloud computing; in other words, using an internet-based research workspace. GEM serves as a portal for health scientists who wish to take advantage of the benefits of collaboration using socially mediated technology—referred to by some as Science 2.019—to accelerate scientific discovery. The GEM database has two overarching goals: (1) to promote use of standardized measures, which are tied to theoretically based constructs; and (2) to facilitate sharing of harmonized data resulting from the use of standardized measures. GEM runs on a wiki platform and allows users to comment on existing constructs and comment and rate existing measures (see Moser et al20 for details).
Phase 2 took advantage of GEM's functionality to obtain reactions to the recommendations for patient-reported measures for EHR. Adaptations to GEM specific for phase 2 included adding an EHR campaign link to the GEM homepage that directed participants to a distinct EHR common data elements-specific homepage. On the project homepage, users found background information; instructions for participation; the list of each domain's candidate measures, evaluation criteria, and a summary of recommendations developed by the phase 1 working groups. Users were provided the practical, broad perspective review of each measure based on the domains in box 1 (ie, meta-data, definition, theoretical foundation, synonyms). Users were instructed to use specific evaluation forms that contained the respective recommendations from the working groups and a list of the candidate measures along with a 1 to 5 rating scale (ranging from weak to strong) for each of the measures. Users were also able to provide text comments and to suggest alternative measures. All wiki ratings, comments, and suggestions for alternative measures were collated and provided the basis for the domain-specific workgroup discussions that occurred in phase 3.
Phase 3: town hall and key stakeholder meetings
The final phase of the project included a 2-day meeting with a specific objective for each day. The purpose of the first day was to get broad feedback from key stakeholders, using a town hall format. The second day was focused on working towards consensus on candidate data elements with a smaller subset of key stakeholders and decision-makers (table 2).
The town hall meeting included an introductory session that focused on the need for common patient-reported data elements. Brief presentations from representatives of patient groups, healthcare organizations, community health centers, and the Office of the National Coordinator for Health Information Technology were used to provide context from a variety of stakeholder perspectives. These presentations were followed by talks demonstrating two successful implementations of health information technology systems using similar behavioral and psychosocial data elements in practice-based research networks. The remainder of the town hall activities included breakout sessions describing the results of the GEM wiki process and soliciting feedback from town hall participants.
Members of the expert panels from phase 1 moderated each of the breakout sessions and tracked the degree to which there was agreement about the importance of the domain, recommendations on candidate measures, the readiness for inclusion in EHR, and dissenting views. Recommendations for possible adaptations or new directions for a given domain were also discussed. The structure of each breakout session included an overview of the workgroup's rationale for the recommendations, presentation of the key criteria for consideration (ie, table 1), a description of each of the candidate measures, and ratings and comments that were generated during phase 2. At the completion of the town hall, the organizing committee discussed the feedback and prioritized the findings for discussion in day 2 activities.
Day 2 was a smaller meeting of key stakeholders (see table 2 for participating organizations) and also included breakout sessions for each of the domains. The breakout groups were instructed to work towards consensus on final recommendations, when possible, for a single measure for each domain. The breakout groups also discussed recommendations for frequency of assessment for each tool (ie, each visit/regularly; annually; only once).
Results
Phase 1
Each group of subject matter experts identified two to four candidate measures for their respective domains. For 10 of the 13 content areas, the recommendations consisted of existing measures, or selected subsets of existing instruments, for consideration. For the areas of health numeracy/literacy, physical activity, and patient goals, the working groups also included a recommendation for a new face valid set of items that were similar to, or based closely on, existing validated measures that, for a variety of reasons, were not practical for self-administration or were not directly actionable. A written summary of each of the subject matter expert working groups' recommendations can be located through: https://www.gem-beta.org/Public/EHRInitiative.aspx?cat=4.
Phase 2
Recommendations from each of the working groups were posted on the GEM website and the availability of this information was widely promoted among approximately 43 agencies and organizations (table 2) as well as informal networks involved in primary care and public health. There was a total of 296 comments and 603 ratings from 98 unique users over the 6-week period. Table 3 includes the number of comments and ratings for each candidate measure across the domains. As can be seen, there was moderate variability in ratings across potential data elements within most content areas.
Table 3.
Ratings of candidate measures by domain
| Domain (n comments) | Candidate measure | Number ratings | Mean/median rating |
| Eating patterns (24) | Start the conversation | 20 | 4.0/4.0 |
| NCI fruit and vegetable screener | 20 | 3.0/3.0 | |
| NCI energy from fat screener | 20 | 2.8/3.0 | |
| Medication taking (44) | Morisky 4-item | 28 | 3.5/4.0 |
| Morisky 8-item | 28 | 3.1/3.0 | |
| Physical activity (30) | Exercise vital sign | 23 | 4.2/4.0 |
| Physical activity vital sign | 23 | 3.5/4.0 | |
| Risky drinking | AUDIT-C (alcohol consumption questions) | 0 | –/– |
| Sleep quality (16) | Neuro-QOL item bank v1.0–sleep disturbance | 11 | 3.3/3.0 |
| Sleep deprivation scale | 11 | 3.3/ 4.0 | |
| Sleep disturbance–PROMIS short form | 11 | 3.3/4.0 | |
| Smoking/tobacco use (7) | Tobacco use screener | 0 | –/– |
| Substance use (3) | NIDA modified assist | 0 | –/– |
| Anxiety and depression (35) | Patient health questionnaire for depression and anxiety (PHQ-4) | 28 | 4.9/5.0 |
| PROMIS anxiety and depression | 28 | 3.6/4.0 | |
| Stress (22) | Distress thermometer | 20 | 3.8/4.5 |
| Domain-specific distress follow-up | 20 | 3.2/3.0 | |
| Domain-specific distress Thermometers | 20 | 3.2/3.0 | |
| Demographics (35) | BRFSS demographics survey | 21 | 3.2/3.0 |
| PHENX demographics | 21 | 3.2/3.0 | |
| Health information national trends survey demographics | 21 | 3.9/4.0 | |
| Health literacy/numeracy (26) | Health literacy screening questions | 21 | 3.3/3.0 |
| Patient literacy preferences | 21 | 3.5/4.0 | |
| Subjective health literacy and numeracy | 16 | 3.1/3.0 | |
| Patient goals (17) | Control preferences scale | 15 | 3.7/4/0 |
| Goal evaluation scale | 15 | 2.9/3.0 | |
| Open-ended goal setting tool | 15 | 2.9/3.0 | |
| Patient's preferred method for communication | 15 | 3.7/4.0 | |
| Quality of life (32) | BRFSS–quality of life | 24 | 2.9/3.0 |
| PROMIS global physical health short survey | 24 | 3.8/4.0 | |
| SF-8 general health survey (short form) | 24 | 3.5/3.0 | |
| EQ-5D | 19 | 2.6/3.0 |
Phase 3
There were 123 participants in day 1 activities and 41 participants on day 2. Both the open town hall meeting and the key stakeholder meeting on the following day generated strong interest and active discussions. The dominant theme that emerged at both meetings was that the data elements needed to be actionable and not overly burdensome. We observed a modest ‘commons dilemma’21 in that each of the breakout groups felt that their specific topic was exceedingly complex and required somewhat lengthier assessment, whereas assessment in the other content areas needed to be very brief, possibly as little as a single item, to prevent patient and practitioner burden. Still, the stakeholder group came to consensus that there were measures sufficiently valid, feasible and actionable to move forward to testing in the real world settings in nine of the 13 topic areas (table 4).
Table 4.
Recommended common data elements by domain
| Domain | Final measure | Recommended frequency | Items |
| Eating patterns | Modified from starting the conversation (STC)22 | Annual | Over the past 7 days:
|
| Physical activity | The exercise vital sign23 | Annual |
|
| Risky drinking | Alcohol use screener24 | Annual | How many times in the past year have you had X or more drinks in a day? (where X is 5 for men and 4 for women) |
| Smoking/tobacco use | Tobacco use screener25 | Annual |
|
| Substance use | Drug use screener26 | Annual | How many times in the past year have you used an illegal drug or used a prescription medication for non-medical reasons? |
| Anxiety and depression | PHQ-427 | Annual | Over the past 2 weeks have you been bothered by these problems? (Leichert scale: not at all, several days, more days than not, nearly every day)
|
| Stress | Distress thermometer28 | Annual | Please circle the number (0–10) that best describes how much distress you have been experiencing in the past week including today. |
| Demographics | Multiple sources29 | Variable | 9 items: Sex, date of birth, race, ethnicity, English fluency, occupation, household income, marital status, education, address, insurance status, veteran's status. |
| Sleep | Adapted BRFSS25; Neuro-QOL30 | Annual | Do you snore or has anyone told you that you snore?In the past 7 days, I was sleepy during the daytime… never, rarely, sometimes, often, always |
In particular, the four areas that were not considered ready for implementation into EHR were quality of life, patient goals, medication-taking behavior, and health literacy/numeracy. While there were differences in the reasons that each of the areas were not considered ready, the primary issues tended to be a lack of a reasonably short measure sensitive to different levels of the construct (eg, health literacy), the breadth of the construct (eg, medication-taking behavior), the difficulty in following up with specific action (eg, quality of life), or the degree to which the construct was specific to a given patient (eg, patient goals). The stakeholder group was unanimous that these were each important and useful content areas, but that available measures needed further development to be practical and actionable in primary care and for the EHR.
A key issue that emerged was that the common data elements should be collected with differential periodicity. For example, some of the demographic and related variables that are very stable might only need to be collected on a patient joining a healthcare group and may only need to be reviewed for accuracy thereafter. A second set of data elements consisting of most of the health behavior and psychosocial issues that are not actively being addressed by a given patient were recommended to be repeated at approximately yearly intervals. The only data elements recommended to be collected more often, such as before each primary care visit, were content topics that the patient and/or health professional is actively focusing on improving. The items recommended for the nine domains that were considered ready for implementation are shown in table 4.
Discussion
The goals for this paper were to describe the process and resulting products at each step of a three-stage process for developing consensus on common data elements for core patient-reported health behavior and psychosocial issues to be included in the primary care EHR. The combination of small group and large community efforts was successful at achieving strong consensus on a reasonably small set of items felt to be important and useful, as well as practical and actionable in primary care settings.
Participants at all stages of the process understood the need to be practical and brief, and that insistence on using typical psychometric standards would create a situation in which the perfect could become the enemy of the good. There were some areas in which the participants felt that although the content area was important, no currently available measures were ready for widespread implementation and that more research and development was needed. We encourage other researchers to place priority on the need for such items as assessing patient goals, health literacy, and medication-taking behaviors.
There was lively discussion at both the town hall meeting and especially the following day key stakeholder meeting about important next steps. Almost all agreed that ‘proof of concept feasibility testing’ was required, given that these exact items have not, to our knowledge, been used before as an integrated survey. The majority also felt that some type of transparent but automated clinical decision support and feedback including recommendations to both patients and their healthcare team would be required to make these items actionable in most primary care settings. Our plans will undoubtedly evolve as the process progresses and new partners emerge. As of this writing, our plan is to conduct separate formative evaluations with patients to assess understanding, usability and potential navigation issues; and diverse primary care teams to understand their priorities, workflow issues and preferences, and their needs for clinical decision support protocols for each domain.
Understanding perspectives, from a wide variety of patients, on the appropriateness of the items is obviously key in this process. If patients feel there are too many questions or questions that do not seem relevant there is a potential for incomplete and invalid responses. Fortunately, as collecting patient-reported outcomes becomes more commonplace in the clinical encounter, there is mounting empirical evidence that collecting valid and useful patient-reported outcomes data is feasible. For instance, several empirical studies have shown compliance with using self-report systems—electronic or otherwise—to gather information regarding symptoms, and patients reported high satisfaction with the process.31 32 There is also evidence that these data have value for the patients and those treating them. For example, Cleeland and colleagues33 showed that cancer patients who reported outcomes to their physicians showed more improvements than control patients.
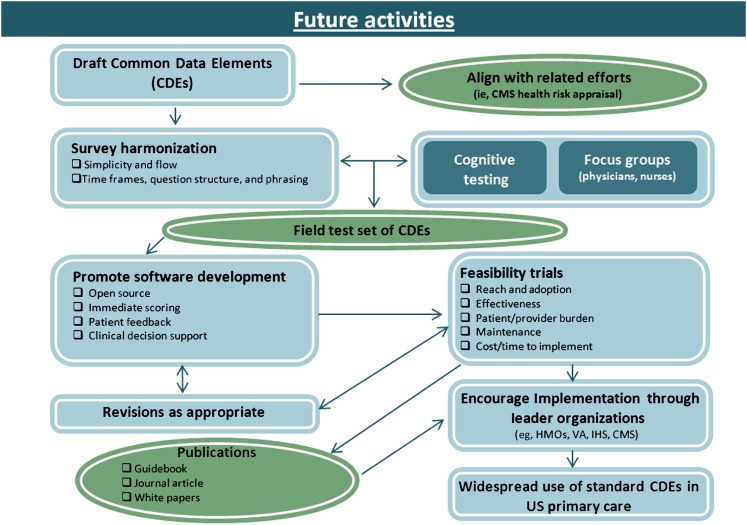
We plan to conduct rapid pilot demonstration projects to determine feasible implementation strategies for the proposed common data elements across different healthcare systems (eg, community health centers, health maintenance organization or veterans' affairs settings, and possibly rural or small fee for service settings). Based on the findings we also plan to make the resulting product available for public use and to those wishing to conduct more comprehensive evaluations or quality improvement projects (figure 1). Obtaining feedback from a wide variety of healthcare systems will also provide details on the processes by which patients and providers in each context may adapt the methods by which behavioral and psychosocial patient-reported outcomes are collected.
Figure 1.
Anticipated next steps in the development and promotion of standardized patient-reported data elements. CDE, common data element.
The remaining concern among some participants was whether the set of common data elements proposed was too much, and whether dividing the data elements into those to be collected only initially; annually; and a few to be collected on a routine basis in conjunction with primary care visits would prove feasible. This issue will be addressed in the near future through the rapid pilot demonstrations. All participants agreed that these next steps should be taken and that the item set in table 4 should not be recommended for widespread adoption until such testing and demonstrations have been completed. There is great potential for the use of such patient-reported data elements to enhance the primary care medical home, meaningful use, and achievement of the Institute of Medicine goals of providing care that is patient centered, equitable, efficient, effective, timely and safe.2 34
Many other efforts are underway to incorporate behavioral and psychosocial measures into EHR. For example, each of our candidate measures maps nicely onto existing meaningful use subdomains and proposed outcomes in future meaningful use stages. For example, meaningful use currently mandates the systematic collection of smoking status and the expectation is that subsequent stages will require the collection of additional patient-reported measures.34 Similarly, the assessment of eating and physical activity behaviors maps directly to the population and public health subdomain of healthy lifestyle behaviors, while the candidate measures of depression, anxiety, and stress map to the subdomain of effective preventive services, and the assessment of demographic characteristics is critical for the subdomain of health equity. Also, beginning in 2011, the Affordable Care Act authorized the CMS to reimburse clinicians for an annual wellness visit, one component of this visit is the collection of a health risk assessment (also a meaningful use indicator under the patient and family engagement subdomain of patient health outcomes). To realize the full value of these initiatives, and successfully to promote the nationwide systematic collection of behavioral and psychosocial measures there is a need for collaboration and agreement on what measurements to collect.
This exercise has definite limitations. First, our approach focused on developing candidate measures and did not focus on where and how these data would fit within the EHR, including the need to incorporate the values in patient assessment instruments into standard clinical terminologies.35 However, our ongoing work includes a focus on the implementation of these measures into existing EHR systems in a way that will allow for easy access for both patient and provider. Second, and perhaps the most obvious, given the large number of behavioral and psychosocial issues relevant to the primary care medical home and comprehensive primary care, and the demand for brevity, few of the resulting recommended items would be considered ‘gold standard measures’ from a psychometric perspective.
Conclusion
We conclude that a set of harmonized patient report and psychosocial data items offers great potential to further multiple aims including: (1) enhancing and promoting patient-centered care; (2) creating a concrete starting point for the creation of decision aids and other tools to facilitate collaborative goal setting and action planning;36 37 and (3) providing the basis for more comprehensive population-based research that includes patient-reported measures as well as biomedical and healthcare utilization data routinely present in EHR systems.
Supplementary Material
Footnotes
Contributors: PE, REG, MB, KME and HK conceptualized the three-phased initiative described in the paper and were the core organizing committee for all three phases. BH and RPM oversaw, implemented, and interpreted data from phase 2 of the initiative. AHK and MVT participated in the organization and implementation of phase 3 of the project and assisted in qualitative analysis, led workgroups, and completed interpretation of the data. PE completed the first draft of the paper with contributions from all of the co-authors. All co-authors also provided feedback and revisions to the final manuscript.
Funding: Funding for the activities described in this paper was provided by the NIH Office of Behavioral and Social Sciences Research, the National Cancer Institute, the Society for Behavioral Medicine, the National Institute of Nursing Research, the Preventive Cardiovascular Nurses Association, and the American College of Sports Medicine. The opinions expressed are those of the authors and do not necessarily represent those of any of these organizations.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All data are available at the request of the corresponding author.
References
- 1.The Patient Protection and Affordable Care Act. Public Law. 2010. 2nd Session Ed 111–114 [Google Scholar]
- 2.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med 2010;363:501–4 [DOI] [PubMed] [Google Scholar]
- 3.US Department of Health and Human Services; The Office of the National Coordinator for Health Information Technology. Meaningful use. http://healthit.hhs.gov (accessed Jul 2011). [Google Scholar]
- 4.Fisher EB, Fitzgibbon ML, Glasgow RE, et al. Behavior matters. Am J Prev Med 2011;40:e15–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mokdad AH, Marks JS, Stroup DF, et al. Actual causes of death in the U.S., 2000. JAMA 2004;291:1238–45 [DOI] [PubMed] [Google Scholar]
- 6.Mokdad AH, Marks JS, Stroup DF, et al. Correction: actual causes of death in the U.S., 2000. JAMA 2005;293:293–4 [DOI] [PubMed] [Google Scholar]
- 7.Gordon L, Graves N, Hawkes A, et al. A review of the cost effectiveness of face-to-face behavioural interventions for smoking, physical activity, diet and alcohol. Chronic Illn 2007;3:101–29 [DOI] [PubMed] [Google Scholar]
- 8.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herman WH, Hoerger TJ, Brandle M, et al. The cost-effectiveness of lifestyle modifıcation or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann Intern Med 2005;142:323–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ratner RE; for the Diabetes Prevention Program Research Group An update on the diabetes prevention program. Endocr Pract 2006;12:20–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cameron IM, Lawton K, Reid IC. Recognition and subsequent treatment of patients with sub-threshold symptoms of depression in primary care. J Affect Disord 2011;130:99–105 [DOI] [PubMed] [Google Scholar]
- 12.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 2002;288:2836–45 [DOI] [PubMed] [Google Scholar]
- 13.Stange KC, Zyzanski SJ, Jaen CR, et al. Illuminating the ‘black box’. A description of 4454 patient visits to 138 family physicians. J Fam Pract 1998;46:377–89 [PubMed] [Google Scholar]
- 14.Yarnall KS, Pollak KI, Ostbye T, et al. Primary care: is there enough time for prevention? Am J Public Health 2003;93:635–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003;348:2635–45 [DOI] [PubMed] [Google Scholar]
- 16.Crabtree BF, Nutting PA, Miller WL, et al. Summary of the National Demonstration Project and recommendations for the patient-centered medical home. Ann Fam Med 2010;8(Suppl 1):S80–90; S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glasgow RE, Kaplan R, Okene J, et al. The need for practical patient-report measures of health behaviors and psychosocial issues in electronic health records. Health Aff 2012;31:497–504 [DOI] [PubMed] [Google Scholar]
- 18.The National Prevention Strategy National Prevention, Health Promotion, and Public health Council. http://www.healthcare.gov/center/councils/nphpphc/index.html (accessed Jul 2011).
- 19.Shneiderman B. Computer science. Science 2.0. Science 2008;319:1349–50 [DOI] [PubMed] [Google Scholar]
- 20.Moser RP, Hesse BW, Shaikh AR, et al. Grid-Enabled Measures: using Science 2.0 to standardize measures and share data. Am J Prev Med 2011;40(Suppl 2):S134–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hardin G. Living within Limits: Ecology, Economics, and population Taboos. New York, NY: Oxford University Press, 1995 [Google Scholar]
- 22.Paxton AE, Strycker LA, Toobert DJ, et al. Starting the conversation: performance of a brief dietary assessment and intervention tool for health professionals. Am J Prev Med 2011;40:67–71 [DOI] [PubMed] [Google Scholar]
- 23.Sallis R. Developing healthcare systems to support exercise: exercise as the fifth vital sign. Br J Sports Med 2011;45:473–4 [DOI] [PubMed] [Google Scholar]
- 24.Smith PC, Schmidt SM, Allesworth-Davies D, et al. Primary care validation of a single-question alcohol screening test. J Gen Intern Med 2009;24:783–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention Behavioral risk factor Surveillance system (BRFSS) Questionnaire. Atlanta, Georgia: US DHHS, 2009 [Google Scholar]
- 26.Smith PC, Schmidt SM, Allesnworth-Davies D, et al. A single-question screening test for drug use in primary care. Arch Intern Med 2010;170:1155–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JB, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009;50:613–21 [DOI] [PubMed] [Google Scholar]
- 28.Roth AJ, Kornblith AB, Batel-Copel L, et al. Rapid screening for psychological distress in men with prostate carcinoma. Cancer 1998;15:1904–8 [DOI] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics National Health Interview Survey. Atlanta, GA: Center Disease Control and Prevention, 2012 [Google Scholar]
- 30.Quality of Life Outcomes in Neurological Disorders http://www.neuroqol.org (accessed 30 May 2011).
- 31.Velikova G, Booth L, Smith AB, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol 2004;22:714–24 [DOI] [PubMed] [Google Scholar]
- 32.Basch E, Artz D, Dulko D, et al. Patient online self-reporting of toxicity symptoms during chemotherapy. J Clin Oncol 2005;23:3552–61 [DOI] [PubMed] [Google Scholar]
- 33.Cleeland CS, Wang XS, Shi Q, et al. Automated symptom alerts reduce postoperative symptom severity after cancer surgery: a randomized controlled clinical trial. J Clin Oncol 2011;29:994–1000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Institute of Medicine Committee on Quality Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press, 2003 [Google Scholar]
- 35.Bakken S, Cimino JJ, Haskell R, et al. Evaluation of the Clinical LOINC semantic structure as a terminology model for standardized assessment measures. J Am Med Inform Assoc 2000;7:529–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bodenheimer TS, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA 2002;288:2469–75 [DOI] [PubMed] [Google Scholar]
- 37.Lorig KR, Holman HR. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 2003;26:1–7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.