Abstract
Objective
Fatal errors can occur in intensive care units (ICUs). Researchers claim that information integration at the bedside may improve nurses' situation awareness (SA) of patients and decrease errors. However, it is unclear which information should be integrated and in what form. Our research uses the theory of SA to analyze the type of tasks, and their associated information gaps. We aimed to provide recommendations for integrated, consolidated information displays to improve nurses' SA.
Materials and Methods
Systematic observations methods were used to follow 19 ICU nurses for 38 hours in 3 clinical practice settings. Storyboard methods and concept mapping helped to categorize the observed tasks, the associated information needs, and the information gaps of the most frequent tasks by SA level. Consensus and discussion of the research team was used to propose recommendations to improve information displays at the bedside based on information deficits.
Results
Nurses performed 46 different tasks at a rate of 23.4 tasks per hour. The information needed to perform the most common tasks was often inaccessible, difficult to see at a distance or located on multiple monitoring devices. Current devices at the ICU bedside do not adequately support a nurse's information-gathering activities. Medication management was the most frequent category of tasks.
Discussion
Information gaps were present at all levels of SA and across most of the tasks. Using a theoretical model to understand information gaps can aid in designing functional requirements.
Conclusion
Integrated information that enhances nurses' Situation Awareness may decrease errors and improve patient safety in the future.
Keywords: Alarms, clinical informatics, cognitive support, decision support, handoffs, human computer interaction, human factors, ICU, information displays, intensive care unit, nursing, nursing informatics, operating room, patient monitor development, patient monitoring, personal values, situation awareness
Patients in intensive care units (ICU) are especially at risk of errors due to the complexity and severity of their medical conditions.1 A source of error may be ICU nurses' high workload requirements. They are often engaged in more than one task at a time, and working under significant perceptual, cognitive, and physical overloads.2 3 Nurses have called repeatedly for integrated displays or systems to ease their workload.4 5 Yet the information required for such integrated displays is not yet known. The purpose of this study was thus to develop recommendations for integrated information displays for frequent ICU nursing tasks based on the theory of situation awareness (SA).
Background and significance
Patient safety and medical errors
A high number of deaths in US hospitals have been shown to be preventable.6 Patients in ICU are especially at risk of errors due to the complexity and severity of their medical conditions.1 Rothschild et al7 found a rate of 80.5 adverse events and 91.3 serious medical errors including two fatal incidents per 1000 intensive care patient days in a 2005 study. The authors also found that 61.4% of the serious errors were associated with medication ordering or the execution of medication treatment; 14.8% were with communication. These rates are considerably higher when compared with the rate of adverse events found in other clinical areas, such as Brennan et al8 (3% in acute care), Nuckols et al9 (9% incidents at an academic and a community hospital), and Thomas et al10 (2.9% inpatient environment).
Nursing and information overload
ICU nurses move constantly while obtaining and delivering information, supplies, and medications.11 They are often engaged in more than one task at a time, and working under significant perceptual, cognitive, and physical overloads.2 3 In addition, nurses need to be aware of patients' treatment goals, family, possible untoward effects of treatments and medications, and upcoming procedures. Nurses are responsible for the monitoring and detect changes in physiological functions on a minute-by-minute basis.12 Finally, nurses must document their work, give medications, and provide care coordination.13
The fact that the information nurses use to conduct these various tasks is located in many different places and in many different forms14 contributes significantly to information overload. For example, the information needed to regulate a patient's hemodynamic status requires the (electronic) medical record, the patient's physiological monitor, infusion pumps, and the ventilator. Cognitive load increases as nurses attempt to integrate these disparate sources of information and, as a result, so does the risk of errors. What is needed is information to be organized around tasks in a way that would support the formation of accurate situation mental models.
Integrated information displays
The number of devices that nurses need to use in the ICU, and the increasingly complex treatment plans with many different medications significantly increases monitoring needs. This two-pronged demand implies that integrated information displays are increasingly more important. By integrated displays, we refer to both a high level of information integration, for example, the combined display of multiple variables in one shape, as well as to system level aggregation of information, for example, combining information from pertinent multiple sources in one location.
Nurses have called repeatedly for integrated systems to ease their workload and help them reach clinical transformation.4 5 A survey among nurses at 25 leading acute care facilities across the USA found ‘that existing systems are often splintered, unable to interface and require multiple logins to access or enter data’.4 In addition, nurses want access to these integrated systems from the point of care, which is most often at the bedside.4 Such integrated displays have the potential to ‘improve staff efficiency, accelerate decisions, streamline workflow processes, and reduce oversights and errors in clinical practice’.5 15
Earlier research has shown that integrated graphical displays of multiple patient variables can improve decision-making and decrease cognitive load.16 For example, anesthesiologists detect significant changes faster using an integrated display compared with traditional displays,17 18 and displays that combine and graphically present information speed up the detection of adverse events, improve the accuracy of diagnosis, and decrease mental workload.19 Stationary dashboards at the nurses' station have limited utility because nurses move frequently.
However, research is not yet available to guide the development of integrated displays. Integrated information displays are currently rarely available in the medical domain. Lacking interoperability between devices as well as the poor understanding of requirements prevent manufacturers from offering solutions improving the work situation at ICU.
Situation awareness
SA theory links the complexity of mental models with task performance.20 Endsley20 identified three levels of SA: (1) perception, (2) comprehension, and (3) projection. Success at the higher levels depends on the success of the lower levels. Perception means that the user is aware of the current state of the system, for example, a variable of the system (a nurse can see the systolic value of the blood pressure or can visually assess respiratory distress). Comprehension refers to the user's understanding of implications of the perceived variables of the system, for example, the meaning of the variable (a nurse might understand that the blood pressure is lower than it should be, considering the patient's condition or that the respiratory distress is new or particularly severe). Projection depicts the user's expectation of consequences for the system and its future developments, for example, the implication of a variable (a nurse might anticipate that if nothing changes to stop the fall in blood pressure, the patient could go into shock or that the respiratory distress might be due to an allergic reaction that must be treated immediately). Although SA does not directly address action, it focuses on the information needed to understand the situation at each level.
Identifying requirements that support all levels of SA will guide designs that minimize mental load and prevent errors due to misjudgment of a situation. Although the theory has rarely/not been applied to studying information gaps during nursing, it is a useful method to parse out the lower level issues of perception from the higher cognitive functions of sense-making and reasoning.
The objective of this study was to develop recommendations for integrated information displays for ICU nurses based on the theory of SA. Nurses gather information from a multitude of sources as they work and must integrate them mentally in order to get the ‘big picture’.14 We aimed to: (1) identify the frequency of ICU nursing tasks; (2) identify information needs associated with high-frequency tasks for each level of SA; and (3) create requirements for improved information access to increase nurses' SA during high frequency tasks.
Materials and methods
The methods described below are presented for each research aim. Before beginning the study, we received institutional review board approval from all three sites.
Aim 1: frequency of ICU nursing tasks
Nineteen ICU nurses participated from three sites, a large academic center (n=10), an academically affiliated Veterans Administration hospital (n=5), and a large community hospital (n=5) participated. The sample size was based on the recommendations of Holtzblatt et al21 to observe at least four users per job role. We selected a convenience sample. Nurses could then agree to participate.
The observation team consisted of a biomedical informaticist with a nursing background, an information design student, a bioengineering student, and two psychology/human factors students. At each site, a team of two conducted the observation (a scribe to record field notes and an interviewer). Training was conducted until observation procedures were accomplished consistently.
Procedures were an adapted form of participant observation.22 The team wrote extensive field notes. During each of the 19 2-h observations, two team members followed a nurse and asked each person to explain the actions they were performing, and to state their goals during each task as they would towards an apprentice. The team asked clarifying questions and prompted the nurse to continue talking. No questions were asked in times of high workload in order not to jeopardize patient safety. Nurses were followed into the patient room, to the central nursing station, and into the medication storage room, but not when nurses left the ICU or requested privacy. Time periods were selected to be mainly in the timeframe between 08:00 and 12:00 hours, because a previous study found that most errors occur during this time period.23 The team met within 24 h of the observations. The scribe read each field note aloud and the observer entered each activity and associated notes into an Excel spreadsheet. The team used cued recall24 to reconstruct the situation in case of unclear notes and discussed each situation until agreement was reached.
Three members of the observation team then categorized field notes describing nurse activities from the field notes into 46 groups according to common activity characteristics by going through an iterative process of discussion. The task groups emerged from the observation data and new categories were added as needed; no template was used. Groups were developed and improved during the categorization process, and subsequently reviewed and named by three outside experienced ICU nurses. The 46 information groups were aggregated by the research team into five categories and validated independently by an ICU nurse manager and an additional three ICU nurses through discussion and consensus.
Aim 2: frequent task information needs for each level of SA
Gaps in information that nurses needed but was not directly available to complete a task were identified in two ways based on the field notes: (1) a change in location occurred for the purpose of acquiring that information, or (2) if a nurse noted verbally that the information was not available.
Missing information was then assigned to one of the levels of SA by the authors using the following criteria. Perceptional challenges (SA level 1) were identified when information was difficult to see or was not available at the location needed. Comprehension (understanding) challenges (SA level 2) were identified when several pieces of information had to be combined, or nurses were not sure about the accuracy or type of information. Projection challenges (SA level 3) were identified when information was missing to predict future developments, to understand the implications of current events, or to determine what options would be best.
Aim 3: recommendations for enhancing SA for frequent task categories
To envision opportunities and improvements for design in information flow, the ‘fit’ between the tasks, the technology, and the individual have to be taken into account simultaneously. Data analysis based only on information categorization sometimes reveals only category-specific challenges but might miss larger problems that span over multiple categories.
An affinity diagram21 was used to consolidate the large amounts of observational data. We built the framework by organizing observations into a wall-sized hierarchical diagram, and grouping the data into key issues under labels indicating the user's needs. The team attached field notes and comments to a wall and sorted them by relatedness, comparable goals, similar tasks, and related problems, and added memos summarizing similarities (see figure 1). Then a research nurse, a clinical interface specialist, and the observation team members ‘walked the wall’,21 reading through the descriptive notes and identifying tasks with missing information. Opportunities and ideas regarding improved information availability, improved communication, and other functions of the integrated display were recorded on post-it notes and attached to the affinity diagram. Ideas for recommendations were based on observed and imputed information gaps as identified through the affinity diagram building process. Recommendations were later discussed in the research team to select feasible options and eliminate ideas that might be less helpful for nurses. This process was iterative and consensual. Opportunities for improvement were ordered and enhanced based on information needs identified in the previous steps by one of the authors (SHK).
Figure 1.
Affinity diagram to identify recommendations for enhancing nurses' situation awareness. Data were grouped into key issues under labels indicating the user's needs, and recommendations were identified subsequently.
Results
Our findings are organized according to the three research aims: (1) the frequency of ICU nursing tasks; (2) information needs associated with high-frequency tasks for each level of SA; and (3) requirements for integrated displays to increase nurses' SA.
Aim 1: frequency of ICU nursing tasks
A total of 890 individual field notes was recorded during the observations and classified into 46 different tasks. These tasks were combined into five categories. Table 1 shows the five categories and their frequency. Using this taxonomy, nurses performed on average 23.5 tasks per hour. Patient awareness included tasks connected to physical and laboratory-based patient monitoring and related alarms.
Table 1.
Observed hourly frequency of task categories
| Category of nursing work | Tasks per hour |
| Communication | 8.6 |
| Medication management | 5.7 |
| Patient awareness | 5.3 |
| Organization | 2.0 |
| Direct patient care | 1.9 |
Table 2 shows all 46 tasks per category and their hourly frequency. The most frequent tasks were charting, checking/signing medication, and administering medication. The table includes tasks that were performed by the observed nurses—even the ones that are not normally considered a part of their job roles, such as extubation. Communication tasks were most frequent and included communicating with persons, peers and notes. Medication management tasks were the second highest frequency. Examples included checking and signing medication orders, medication administration, acquiring medication, and checks for intravenous compatibility. Patient awareness tasks, the third highest frequency, included assessing patients, checking alarms or instruments. Organization tasks included preparing, checking, and setting up equipment for procedures and awaiting pending events, for example, admissions. Direct patient care tasks included supporting the patient in activities of daily life, suctioning, bathing, oral care, and tube feeding.
Table 2.
Task frequency and categories of nursing work
| Category of nursing work | Task | Tasks/h |
| Communication | Chart | 1.7 |
| Talk to the patient | 1.0 | |
| Check/sign orders | 0.9 | |
| Talk with relatives | 0.9 | |
| Communicate with a physician | 0.8 | |
| Relay information to another nurse | 0.8 | |
| Communicate with another nurse to Organize workflow | 0.6 | |
| Ask another nurse for advice | 0.5 | |
| Communicate with respiratory therapist | 0.4 | |
| Participate in rounds | 0.3 | |
| Communicate with unit clerk | 0.2 | |
| Socialize with another nurse | 0.2 | |
| Call pharmacy | 0.2 | |
| Record nursing note | 0.1 | |
| Total | 8.6 | |
| Medication management | Check medication order/sign order | 1.6 |
| Administer medication | 1.6 | |
| Assess currently administered intravenous Medication | 1.5 | |
| Acquire medication | 0.8 | |
| Check medication compatibility | 0.2 | |
| Record nursing note | 0.1 | |
| Total | 5.7 | |
| Patient awareness | Patient assessment | 1.1 |
| Nurses rounding (at a glance assessments) | 1.1 | |
| Assess reason for alarm | 1.0 | |
| Measure urine output | 0.6 | |
| Record nursing note | 0.7 | |
| Assess wounds | 0.2 | |
| Draw arterial blood sample | 0.2 | |
| Assess patient's mental orientation | 0.2 | |
| Assess restraints | 0.1 | |
| Perform spontaneous breathing trial | 0.03 | |
| Assess endotracheal tube position | 0.03 | |
| Total | 5.3 | |
| Organization tasks | Set up equipment (intravenous pump, ventilator…) | 1.4 |
| Check equipment | 0.5 | |
| Await pending task, for example, Admission | 0.2 | |
| Total | 2.0 | |
| Direct patient care | Support patient in activities of daily life (eg, eating, drinking, toileting…) | 1.2 |
| Suction patient's airways | 0.4 | |
| Bath | 0.1 | |
| Perform oral care | 0.1 | |
| Administer tube feeding | 0.1 | |
| Pull catheter | 0.03 | |
| Extubate | 0.03 | |
| Total | 1.9 |
Aim 2: frequent task information needs for each level of SA
Table 3 shows details on missing information for each level of SA for the high frequency task categories ‘communication’, ‘medication management’, and ‘patient awareness’—infrequent categories ‘organization’ and ‘direct patient care’ are excluded. Perceptional challenges (SA level 1) shown in the first part of the table were often caused by unavailable information or information that was hard to discriminate. Challenges for nurses' comprehension (SA level 2) shown in the middle were largely a result of the need to combine multiple pieces of information from different locations, inaccurate or unclear information, or correct performance of procedures was unknown. Challenges for nurses' projection (SA level 3) shown in the bottom of the table were mainly based on either missing or inaccurate information needed to predict future developments.
Table 3.
Challenges in the frequent task categories by levels of situation awareness
| Task | Missing information |
| Perception challenges | |
| Communication |
|
| Medication management |
|
| Patient awareness |
|
| Comprehension challenges | |
| Communication |
|
| Medication management |
|
| Patient awareness |
|
| Projection challenges | |
| Communication |
|
| Medication management |
|
| Patient awareness |
|
EMR, electronic medical record.
In the following section, we make recommendations for improving SA based on the categories of missing information identified above.
Aim 3: recommendations for enhancing SA for frequent task categories
Information gaps were identified for the most frequent categories ‘communication’, ‘medication management’, and ‘patient awareness’. The less frequent categories of ‘organization’ and ‘direct patient care’ were excluded because insufficient information gaps were observed during these tasks and to keep the work focused. Recommendations are organized by the respective SA level for which they address challenges: perception, comprehension, and projection.
Enhancing communication
The perceptional challenge of finding communication partners involved long searches across the whole ICU. These communication tasks with other providers could be improved by establishing methods of information sharing from any location, including inside the patient's room. During the study we observed that at one ICU a voice communication system was available to some nurses, which increased the number of interruptions compared with the ICU without such a system. During asynchronous communication tasks, nurses' comprehension if a message was received could be improved through additional features. Such additional feature should allow clinicians to affirm receipt, to accept responsibility for a task, to target more than one recipient, and to be able to search, sort, and retrieve strings of exchanges. These communication design attributes should be included in the design of future technology.
To address challenges in the nurses' SA projection as well as the care teams' shared awareness of the patient, clinicians should easily be able to include/attach/link to selected patient data such as particular data from the patient monitor or the electronic medical record as part of the communication. These attributes could also be applied to patient requests, physician's verbal comments, and even components of shift reports.
Improving medication management
A particular salient set of information deals with medication management. Current SA perceptional challenges include the awareness of the changes of the medication orders. These orders are tightly integrated with patients' physiological status. Currently, nurses must log on to the separate electronic health record and electronic medication administration record to assess fully the patients' status and treatment plan. Consolidating this information and making it automatically available to the nurse on an integrated display inside the patient's room would improve awareness of medication management, eliminate frequent logins and wrong medication administration, and facilitate the comprehension of any changed or new medication orders for assigned patients. To ensure the patient's privacy, the integrated display should automatically detect the nurse's presence, for example, using proximity badges or similar technology—and only show information while a nurse is present. Furthermore, an integrated display could increase the nurses' perception by showing whether a medication is available in the unit's medication room or in the pharmacy. To enhance the projection of potential medication side effects and adverse events, the display could show intravenous compatibility with the currently administered medication and possible adverse effects of the new medication. Finally, perceptional challenges included the lack of being able to monitor intravenous medication checks ‘at a glance’ from the patient's doorway. Medication monitoring would be improved by providing information regarding the medication name, delivery rate, and time until empty, as well as basic vital signs in a large font readable from the doorway.
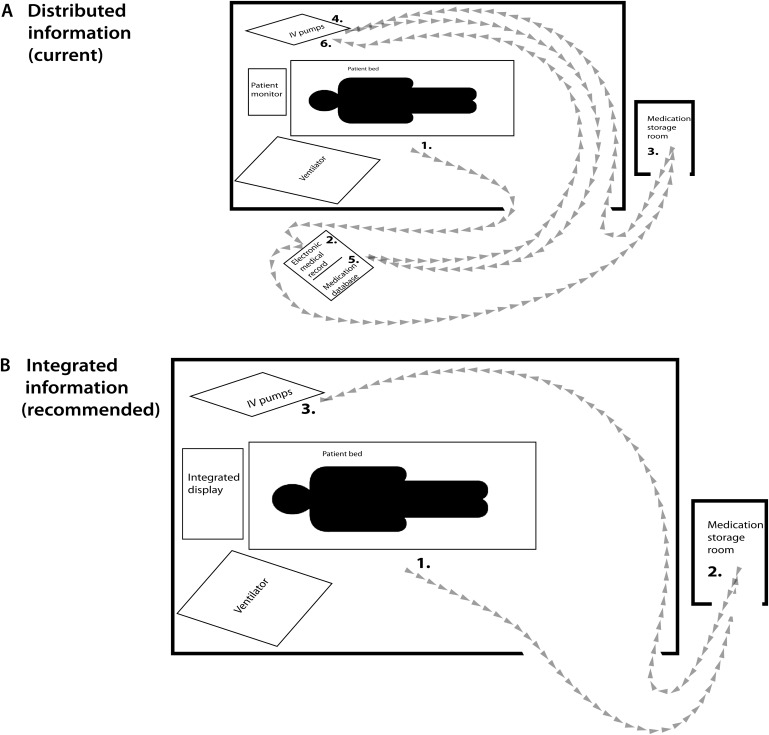
Including medication management activities would improve efficiencies. Figure 2 demonstrates a compression between the current situation and a simulated situation in which information is integrated. In the integrated state, medication orders, intravenous compatibility, and adverse effects are all available at the bedside. Having integrated information could reduce the number of times nurses walk between work stations from as frequent as five trips to as few as two per medication administration. In fact, some of the observed ICU had the medication administration record and medication database located outside of the patient's room as shown in the sequence in figure 2A. If the nurse is inside the patient's room (1) and decides to check whether a new medication needs to be given, an electronic medical record outside of the room needs must be consulted—a perception challenge (2). A new medication must be obtained from the medication storage room (3). To check if the new medication can run through the same intravenous line as one of the current medications, the nurse must remember the current medication (4) and check the intravenous compatibility in a reference system online—a projection challenge (5a). Furthermore, the nurse must check if the new medication might cause adverse effects that need to be monitored (5b), then administers the medication (if compatible) and checks the patient's vital signs on the monitor—a comprehension challenge of the patient's reaction (6). In this scenario the nurse has made five trips. In the integrated scenario, figure 2B, the nurse gets notified through the integrated information display about a new scheduled medication (perception), if it would be available at the medication storage room and was compatible with current medication (projection) (1). The nurse gets the medication from the medication storage room (2), administers it and checks the patient's reaction on the monitor (comprehension) (3). This scenario would require nurses to take only two trips.
Figure 2.
Example for reduced physical workload by the results of the intervention to display integrated information at the bedside to increasing the fit between medication administration and technology by introducing an integrated information display at the bedside: When administering medication (A) a nurse travels up to five trips with the currently used displays (B) if an integrated display at the patient's head bedside would consolidate information, a nurse would only take two trips.
Patient awareness
To increase nurses' perception of the patient's vital signs on the patient monitors, and the subsequent comprehension of potential changes, pertinent information should be visible and easily readable from the room doorway. In addition, to allow a nurse perceiving and comprehending the state of his or her other patient (normally located in a different room), relevant alarms and vital signs with significant deviations should be automatically shown at the nurses' present location in a way that ensures the nurses' comprehension that this information is about the other patient. To allow predictions in the patient's development during drug administration improve titration of medications to the desired effect, direct review of the patient's past vital signs alongside the respective past drug delivery rate is recommended.
Discussion
We found that nurses experience significant challenges in navigating and integrating their information environment. Information gaps exist at all three levels of SA, in particular for frequent nursing tasks. Nurses' SA perception was challenged by the visibility of essential information, either because it was not easily accessible (eg, drug–drug compatibility, or drug–disease and drug–patient interactions) or because it was simply difficult to see at a distance as the nurse moved around the ICU. In addition, our observations showed that audible information was enveloped into background noise and so was not accurately perceived. Comprehension was also not well supported. To understand the correlation between the patients' status and current treatments, nurses needed to gather and integrate information from multiple devices such as the vital signs monitor, intravenous pumps, the ventilator, and electronic medical records simultaneously. Furthermore, equipment settings were often altered by others without notification, so nurses spent significant time double-checking settings, orders and clinical notes for congruency. Finally, SA projection was often difficult because information about the risk of adverse events or the likelihood of successful treatment required communication about care goals, expected results from treatments and the rate of change of key information. This kind of high-level information was not often available and took considerable effort to acquire.
Some of our task categories overlap with the categories as defined by other research: direct care, organization, medication management, and patient awareness.13 25 26 However, when compared with the work of Hendrich et al13 our work could show the relevance of information communication for nurses. We defined a communication category—with the focus on exchange of information and included documentation as we thought the main purpose of documentation was communicating information.
Our results are congruent with nursing theories that address nursing actions. The nursing intervention lexicon and taxonomy of Grobe et al26 identifies seven categories of nursing interventions based on a qualitative analysis of nursing statements. Their categories of ‘care need determination’ and ‘care vigilance’ are comparable to our category called ‘patient awareness’. Their category entitled ‘care environment management’is similar to our ‘organization’ category. In addition, informatics theories were not a part of the early work of Grobe et al26 but the early work of Graves and Corcoran27 and the model of human–computer interaction of Staggers and Parks,28 as well as later work by Staggers29 represent the device interaction components of ICU nurses' work. The informatics research organizing model of Effken,30 which takes into account nursing practice, cognitive decision-making, context and the patient's health in a broad sociotechnical perspective, is closest to this work. The current work expands the work cited above because it focuses on information gaps, determines critical information for integrated displays based upon frequent nursing tasks, and uses SA as a theoretical basis.
Concerning the information needs of nurses, our work expands current knowledge by listing detailed information deficits. Other research supports findings that nurses need to perform extensive information gathering,3 31 32 that their awareness of the patient and treatment is sometimes challenged,2 33–35 current devices do not support them adequately,3 23 33 and similarly demands for improved information access,3 5 36 and improved communication.25 35 37 However, expanding current knowledge, our research provides specific details about which information is missing during frequent task categories. We could identify specific information needs of nurses that are currently not sufficiently met and challenge the different levels of nurses' SA. This information advances current knowledge about current information deficits and can be used during the development and improvement of medical devices and information systems.
To prioritize task-specific support through new devices, our hourly frequencies of ICU nursing tasks add to the literature. Different to the percentages of nursing time spent for different tasks, as identified by Hendrich et al,13 these findings allow prioritizing new device development for tasks that are performed frequently by nurses.
When using the SA taxonomy to categorize information needs and to derive opportunities for the development of new integrated displays, devices better support the user's work. Situational awareness is the key to be able to act adequately and continuously assess the importance, urgency and details of tasks and combine them to a workflow. Nurses continuously need to react adequately on changes in the patients' status, to call a doctor in critical situations and to organize the less important tasks around urgent tasks. Therefore, our identification of requirements for integrated displays for nurses, based on the framework of SA, could lead to the development of better devices—devices that improve nurses' understanding, planning and execution of their daily work and lead to a higher awareness.
Implications
Integrated displays would better support nurses as they perform medication management tasks, provide more efficient information exchange between care providers, and enhance nurses' SA and context-sensitive decision-making.
Implications for error
We found that current devices at the ICU bedside do not adequately support nurses' activities. Such inadequate support might contribute to the high number of errors found by previous research, such as the high number of serious errors (61.4%) of Rothschild et al7 associated with medication management, and the 14.8% related to inadequate reporting or communication. Improving communication of clinical goals of care might significantly improve care, efficiency, and decrease errors. In one study, only 10% of ICU staff understood the goals of care on a daily basis; after implementation of a daily white board, 95% of the staff reported understanding the goals of care. One result was a significant decrease in the days of stay by 1.5 days.38 In another study, the quality of the nurse–physician communication was significantly related to medication errors overall.39 Finally, communication between physicians and nurses was involved in 43% of errors.23 The rate of errors peaked after shift changes and rounds,23 and nurses were found to forget what they were looking for while moving from one patient room to another.2
Implications for design
The results of this study support the need to incorporate critical information into bedside displays that go beyond the content of the monitor itself. Information should be organized around medication tasks, communication of critical information, and patient awareness to support efficient information exchange. Medication management tasks are performed frequently, and involve significantly more complex information needs than are met by current devices. Therefore, medication management information should be extremely accessible, including instant access to orders, notifications whenever orders have been changed, medication compatibility, medication-specific monitoring needs, and likely adverse side effects.
Synchronous communication between nurses and physicians increases shared knowledge and nurses' understanding of the patients' state.40 Particularly important is a shared display regarding the location of other clinicians, access information, and timing for assumed responsibilities.
Limitations/comment on methods
Our results are based on an adaptation of the participant observation method, questionnaires, and brainstorming to define design implications and recommendations based on theory. Other researchers have used cognitive work analysis41 42 or expert consultation to identify requirements for nurses' bedside displays.12 43 44 Cognitive work analysis might have resulted in more in-depth findings than our results but would have been more intrusive for nurses' workflow. An expert consultation method might have limited results to problems the users could recall without being in the context of work, a method that could have significant bias.21 Our methods have the advantage of integrating across three institutions with a variety of nurses and time slots. Similar to cognitive work analysis, we looked at the tasks nurses performed, the decisions they made, information searching behavior, and the overall context in which they performed their work. A limitation of the study is that the results were not validated by member checking. This study is also limited due to a restricted geographical area and a relatively few number of nurses, who were not selected randomly.
Future studies might include observations during the night shifts when accessibility of doctors and colleagues might be more limited, and different communication and decision support needs could prevail. Future work could additionally use our identification of tasks and information needs as a foundation to apply the fit between individuals, task, and technology framework or incorporate a model of work analysis45 or workload theory as the conceptual basis. Future research should focus on the detailed design of such integrated systems, to provide manufacturers with concrete design guidelines combining the ‘what’ with the ‘how’.
Conclusion
Current cognitive support for nurses' tasks is suboptimal—essential information is missing at the point needed, and even when it is present, the information is not integrated at the task level. The information environment does not keep pace with the constantly changing condition of the patient and team membership. The result is deficits at all levels of SA and an increased likelihood of errors. Our recommendations are directly linked to our theory-based observations and further the development of devices that better suit the users' needs.
Acknowledgments
The authors acknowledge the contributions, advice, and support of John Hurdle, Eric Boam, Amanda Sheeren, Laureen Whitaker (University of Utah), Kai Kück (Draeger), and the ICU nurses who participated.
Footnotes
Contributors: Conception and design: SHK, CW, MH, NS, JA and DW. Data collection: SHK, MG, as well as the research assistants Eric Boam, Amanda Sheeren and Laureen Whitaker. Analysis of the data: SHK, CW, MG, Amanda Sheeren, Laureen Whitaker. Interpretation of the data: SHK, CW, MH, JA, DW, MG, N Staggers. Drafting of the article: SHK, CW, NS, DW. Critical revision of the article for important intellectual content and final approval of the article: SHK, CW, MH, NS, JA, MG, DW.
Funding: The study was partly funded by a grant from Draeger, Lübeck, Germany, the manufacturer of Draeger monitoring devices.
Competing interests: SHK, NS, MG, MH, JA and DW received part of their salary through the grant by Draeger when this study was conducted. CW has no conflict of interest to report.
Ethics approval: Ethics approval was provided by the institutional review boards of the University of Utah, VA Salt Lake City, and Intermountain Healthcare Salt Lake City.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kaushal R, Bates DW, Franz C, et al. Costs of adverse events in intensive care units. Crit Care Med 2007;35:2479–83 [DOI] [PubMed] [Google Scholar]
- 2.Potter P, Wolf L, Boxerman S, et al. Understanding the cognitive work of nursing in the acute care environment. J Nurs Adm 2005;35:327–35 [PubMed] [Google Scholar]
- 3.DeLucia PR, Ott TE, Palmieri PA. Performance in nursing. Rev Hum Factors Ergon 2009;5:1–40 [Google Scholar]
- 4.Bolton LB, Gassert CA, Cipriano PF. Smart technology, enduring solutions: technology solutions can make nursing care safer and more efficient. J Healthc Inf Manag 2008;4:24–30 [PubMed] [Google Scholar]
- 5.Egan M. Clinical dashboards: impact on workflow, care quality, and patient safety. Crit Care Nurs Q 2006;29:354–61 [DOI] [PubMed] [Google Scholar]
- 6.Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Institute of Medicine. Washington, DC: National Academy Press, 1999 [PubMed] [Google Scholar]
- 7.Rothschild JM, Landrigan CP, Cronin JW, et al. The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med 2005;33:1694–700 [DOI] [PubMed] [Google Scholar]
- 8.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients. Results of the Harvard Medical Practice Study I. N Engl J Med 1991;324:370–6 [DOI] [PubMed] [Google Scholar]
- 9.Nuckols TK, Bell DS, Liu H, et al. Rates and types of events reported to established incident reporting systems in two US hospitals. Qual Saf Health Care 2007;16:164–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas EJ, Studdert DM, Burstin HR, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care 2000;38:261–71 [DOI] [PubMed] [Google Scholar]
- 11.Görges M, Markewitz BA, Westenskow DR. Improving alarm performance in the medical intensive care unit using delays and clinical context. Anesth Analg 2009;108:1546–52 [DOI] [PubMed] [Google Scholar]
- 12.Miller A, Sanderson P. Clinical information use by medical and nursing staff in an ICU: a coded tables analysis. Proceedings of the 49th Annual Meeting of the Human Factors and Ergonomics Society (HFES2005). Loews Royal Pacific Resort, Orlando, FL, 26–30 September 2005:984–8 doi:10.1177/154193120504901130 [Google Scholar]
- 13.Hendrich A, Chow M, Skierczynski B, et al. A 36-hospital time and motion study: how do medical-surgical nurses Spend their time? Perm J 2008;12:25–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alexander G, Staggers N. A systematic review of the designs of clinical technology: findings and recommendations for future research. Adv Nurs Sci 2009;32:252–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leape L, Berwick D, Clancy C, et al. Transforming healthcare: a safety imperative. Qual Saf Health Care 2009;18:424–8 [DOI] [PubMed] [Google Scholar]
- 16.Miller RA, Gardner RM, Johnson KB, et al. Clinical decision support and electronic prescribing systems: a time for responsible thought and action. J Am Med Inform Assoc 2005;12:403–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michels P, Gravenstein D, Westenskow DR. An integrated graphic data display improves detection and identification of critical events during anesthesia. J Clin Monit 1997;13:249–59 [DOI] [PubMed] [Google Scholar]
- 18.Zhang Y, Drews F, Westenskow D, et al. Effects of integrated graphical displays on situation awareness in anaesthesiology. Cognit Tech Work 2002;4:82–90 [Google Scholar]
- 19.Görges M, Staggers N. Evaluations of physiological monitoring displays: a systematic review. J Clin Monit Comput 2008;22:45–66 [DOI] [PubMed] [Google Scholar]
- 20.Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum Factors 1995;37:32–64 [Google Scholar]
- 21.Holtzblatt K, Wendell JB, Wood S. Rapid Contextual Design: A How-to Guide to Key Techniques for User-centered Design. San Francisco: Morgan Kaufmann Pub, 2005 [Google Scholar]
- 22.Douglas JD. Investigative Social Research. Beverly Hills, CA: Sage Publications, 1976 [Google Scholar]
- 23.Donchin Y, Gopher D, Olin M, et al. A look into the nature and causes of human errors in the intensive care unit. Qual Saf Health Care 2003;12:143–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jabine TB, Straf ML, Tanur JM, et al. Cognitive Aspects of Survey Methodology: Building a Bridge Between Disciplines. Report of the Advanced Research Seminar on Cognitive Aspects of Survey Methodology. Washington, DC: National Academy Press, 1984 [Google Scholar]
- 25.Tang Z, Mazabob J, Weavind L, et al. A time-motion study of registered nurses' workflow in intensive care unit remote monitoring. AMIA Annu Symp Proc 2006;2006:759–63 [PMC free article] [PubMed] [Google Scholar]
- 26.Grobe SJ, Hughes LC. The conceptual validity of a taxonomy of nursing interventions. J Adv Nurs 1993;18:1942–61 [DOI] [PubMed] [Google Scholar]
- 27.Graves J, Corcoran S. Design of nursing information systems: conceptual and practice elements. J Prof Nurs 1988;4:168–77 [DOI] [PubMed] [Google Scholar]
- 28.Staggers N, Parks PL. Description and initial applications of the Staggers & Parks nurse–computer interaction framework. Comput Nurs 1993;11:282–90 [PubMed] [Google Scholar]
- 29.Staggers N. Human-computer interaction in health care organizations. In: Englebardt S, Nelson R, eds. Information Technology in Health Care: An Interdisciplinary Approach. Orlando, FL: Harcourt Science Company, 2000:321–45 [Google Scholar]
- 30.Effken JA. An organizing framework for nursing informatics research. Comput Inform Nurs 2003;21:316–23; quiz 324–5. [DOI] [PubMed] [Google Scholar]
- 31.Potter P, Wolf L, Boxerman S, et al. An analysis of nurses' cognitive work: a new perspective for understanding medical errors. In: Henriksen K, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation. Rockville, MD: Agency for Healthcare Research and Quality, 2005 [PubMed] [Google Scholar]
- 32.Doig AK. Graphical Cardiovascular Display for Hemodynamic Monitoring. PhD thesis. Salt Lake City: The University of Utah, 2006 [Google Scholar]
- 33.Gurses AP, Carayon P. Exploring performance obstacles of intensive care nurses. Appl Ergon 2009;40:509–18 [DOI] [PubMed] [Google Scholar]
- 34.Donchin Y, Gospher D, Olin M, et al. A look at the nature and causes of human errors in the intensive care unit. Crit Care Med 1995;23:299–300 [DOI] [PubMed] [Google Scholar]
- 35.Thomas EJ, Sexton JB, Helmreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med 2003;31:956–9 [DOI] [PubMed] [Google Scholar]
- 36.Di Pietro T, Coburn G, Dharamshi N, et al. What nurses want: diffusion of an innovation. J Nurs Care Qual 2008;23:140–6 [DOI] [PubMed] [Google Scholar]
- 37.Vandenkerkhof EG, Hall S, Wilson R, et al. Evaluation of an innovative communication technology in an acute care setting. Comput Inform Nurs 2009;27:254–62 [DOI] [PubMed] [Google Scholar]
- 38.Pronovost P, Berenholtz S, Dorman T, et al. Improving communication in the ICU using daily goals. J Crit Care 2003;18:71–5 [DOI] [PubMed] [Google Scholar]
- 39.Manojlovich M, DeCicco B. Healthy work environments, nurse-physician communication, and patients' outcomes. Am J Crit Care 2007;16:536–43 [PubMed] [Google Scholar]
- 40.Beuscart-Zephir MC, Pelayo S, Anceaux F, et al. Cognitive analysis of physicians and nurses cooperation in the medication ordering and administration process. Int J Med Inform 2007;76(Suppl 1):S65–77 [DOI] [PubMed] [Google Scholar]
- 41.Rasmussen J. Information Processing and Human-Machine Interaction: An Approach to Cognitive Engineering. New York, NY: Elsevier Science Inc, 1986 [Google Scholar]
- 42.Rasmussen J. Cognitive Systems Engineering. New York, NY: Wiley-Interscience, 1994 [Google Scholar]
- 43.Wachter SB, Agutter J, Syroid N, et al. The employment of an iterative design process to develop a pulmonary graphical display. J Am Med Inform Assoc 2003;10:363–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Doig AK, Albert RA, Syroid N, et al. Graphical arterial blood gas visualization tool supports rapid and accurate data interpretation. Comput Inform Nurs 2010;29:204–11 [DOI] [PubMed] [Google Scholar]
- 45.Ammenwerth E, Iller C, Mahler C. IT-adoption and the interaction of task, technology and individuals: a fit framework and a case study. BMC Med Inform Decis Mak 2006;6:3. [DOI] [PMC free article] [PubMed] [Google Scholar]