Abstract
To date there have been no studies examining complicated grief (CG) in Aboriginal populations. Although this research gap exists, it can be hypothesized that Aboriginal populations may be at increased risk for CG, given a variety of factors, including increased rates of all-cause mortality and death by suicide. Aboriginal people also have a past history of multiple stressors resulting from the effects of colonization and forced assimilation, a significant example being residential school placement. This loss of culture and high rates of traumatic events may place Aboriginal individuals at increased risk for suicide, as well as CG resulting from traumatic loss and suicide bereavement. Studies are needed to examine CG in Aboriginal populations. These studies must include cooperation with Aboriginal communities to help identify risk factors for CG, understand the role of culture among these communities, and identify interventions to reduce poor health outcomes such as suicidal behavior.
Keywords: complicated grief, bereavement, Aboriginal, First Nations, indigenous, suicide
Abstract
Hasta la fecha no se han realizado estudios que examinen el duelo complicado (DC) en poblaciones aborígenes. Aunque existe esta brecha en la investigación se puede plantear la hipótesis que las poblacíones aborígenes pueden tener un mayor riesgo de DC debido a diversos factores, entre los que se incluye el aumento en la frecuencia de todas las causas de mortalidad y de las muertes por suicidio, Los pueblos aborígenes también tienen una historia pasada de múltiples estresores producto de la colonízación y la asimilación forzada (un ejemplo significative de esto es la incorporación a los colegios con sistema de internado). Esta pérdida de la cultura y la alta frecuencía de hechos traumáticos pueden colocar a los aborígenes frente a un mayor riesgo de suicidio, como también de DC producto de pérdidas traumáticas y de duelos por suicidio. Es necesario poder disponer de estudios que examinen el DC en poblaciones aborígenes. Estos estudios deben contar con la cooperación de las comunidades aborígenes para ayudar a identificar los factores de riesgo para el DC, comprender el papel de la cultura en estas comunidades e identifícar las intervenciones tendíenies a reducir los malos resultados de los indicadores de salud como la conducta suicida.
Abstract
Il n'existe aucune étude à ce jour sur le deuil compliqué (DC) chez les populations aborigènes. On peut supposer, malgré cette lacune, que ces populations présentent un risque accru pour le DC compte tenu de différents facteurs dont une augmentation des taux de mortalité toutes causes et de mort par suicide. L'histoire des Aborigènes est jalonnée de nombreux stress provoqués par la colonisation et par l'assimilation forcée, l'exemple le plus significatif en étant le placement en internat. Cette perte de culture et des taux élevés d'événements traumatisants exposeraient Ies Aborigènes à un risque augmenté de suicide, ainsi qu'à un DC succédant à une perte traumatique ou une perte par suicide. Des études sur le DC chez Ies Aborigènes sont indispensables ; elles nécessitent une coopération avec ces communautés afin d'identifier Ies facteurs de risque de DC, de comprendre le rôle de leur culture et de trouver Ies méthodes qui permettraient de réduire Ies mauvais résultats en termes de santé comme le comportement suicidaire.
Brief introduction to complicated grief
Bereavement is a common term used to describe having lost someone important or significant through death.1 This intense emotion or distress following bereavement is referred to as grief, or the emotional reaction to bereavement.1 Grief is complex, and incorporates multiple symptoms such as anger and sadness, and varies by the individual, by culture, and across time. Although the experience of grief varies by individual, some individuals experience complicated bereavement processes, more commonly known as complicated grief (CG). While most people experience bereavement over the course of their lifetime, CG is a chronic and debilitating consequence of bereavement that is associated with clinically significant distress and impairment.2 Establishing typical norms for time spent grieving and the intensity of these symptoms is difficult, and may vary for individuals of different backgrounds and cultures.1
Cultural considerations for complicated grief
CG is thought to occur in 10% of individuals who have been bereaved, and affects people worldwide.2 Individuals from all countries and cultures are affected by CG,3-20 and it has been noted that further investigation is needed to understand the specific role of cultural factors in CG.2 Although the specific role of cultural factors such as religion, language, and beliefs on the bereavement process may not be known, one can understand the important role culture has in understanding bereavement. In fact, the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV notes the importance of culture in understanding an individual's duration and expression of bereavement. It has been argued that no studies or ideas surrounding grief are truly viewed without a cultural lens.21 In this sense, cultural influences define grief, as well as the grief trajectory for each individual. This trajectory may involve the individual seeking meaning in grief, and constructing new meanings about who they are and who they must be following bereavement.22 It is important to truly understand the culturally based meanings and assumptive worlds in which individuals exist before attempting to make sense of their bereavement experience. Schemata, or assumptions, can be shattered by a traumatic change such as death, which results in grief for the bereaved individual. In this case, individuals must relearn themselves and the world cognitively following their loss, before they can change and advance emotionally.22 Western values, which view grieving as largely an individual experience, are not shared by all cultures. Rosenblatt21 discusses the idea of bereavement in a cross-cultural perspective, and highlights that for some people grief is a shared experience, which is shaped by the community's members. Other studies have also identified grief to be a collective experience, with more concern about the group and less about individual levels of coping.23 The experience of grief must be viewed using a wider cultural framework allowing for the examination of different cultural responses to grief.22 Disentangling culture and grief is a preliminary step in beginning to understand how people grieve, and what kinds of supports they need.21
Intergenerational trauma and complicated grief in Aboriginal populations
To date there have been no studies examining CG in Aboriginal populations. Although this research gap exists, it can be hypothesized that Aboriginal populations may be at increased risk for CG, given a variety of factors including increased rates of all-cause mortality and death by suicide.24-26 First Nations people in North America face concurrent stressors and hardships, including adverse childhood events, poverty, unemployment, and witnessing traumatic events such as violence and homicide.24,27 First Nations people also have a past history of multiple stressors resulting from the effects of colonization and forced assimilation; a significant example being residential school placement, where Aboriginal children were forced to leave their homes and were separated from their culture, families, and communities.24,25 This acculturation resulted in cultural oppression, damaged social support, loss of tradition, and experiences of physical, sexual, and emotional abuse for many First Nations children.24,25 Australian Aboriginal people have also experienced intergenerational transmission of violence, abuse, and loss.28 This loss of culture and high rates of traumatic events may place Aboriginal individuals at increased risk for suicide, as well as CG resulting from traumatic loss and suicide bereavement.
While little information is available on Aboriginal populations and CG, some authors have discussed the concept of a “soul wound” or historical trauma and their impact on health and grief. Duran et al discuss the soul wound, and the symptoms that sometimes accompany such trauma.29 For example, symptoms of pain, suffering, guilt, and psychological stress have been thought to reflect survivor syndrome, or outcomes resulting from colonialism.30 Brave Heart also argues that Aboriginal populations such as the Lakota (Teton Sioux) experience impaired grief, and that this grief results from massive cumulative traumas.30 It may be that impaired grief and CG share or reflect similar concepts and characteristics. Brave Heart defines impaired grief as resulting from the prohibition of indigenous spiritual practices, which inhibits the culturally specific ways or modes of working through normative grief. This cultural bereavement can lead to poor health outcomes such as posttraumatic stress disorder and anxiety disorders.31 Brave Heart also discusses the traditional bereavement or grief process of the Lakota, and highlights traditional mourning practices, including visible signs of grief, in that close relatives cut their hair to symbolize the emotional pain of losing the loved one. Because the bereaved were identified by short hair, their community treated them respectfully and recognized the mourning process. During this time, spirit-keeping ceremonies are also conducted, enabling the grief process for a year after the death. “Releasing of the spirit” and “wiping of the tears” ceremonies are also held to help resolve grief and to welcome the bereaved into their community. Due to the effects of historical trauma, Brave Heart argues that the Lakota were not able to resolve their grief, and experienced impaired grief.30 While impaired and complicated grief may share similarities in that grief responses are complex, it is understandable how the prohibition of spiritual practices and high rates of traumatic events may place First Nations individuals at increased risk for poor health outcomes.
Suicide rates are an important and serious health outcome and public health issue that are linked to CG, and are extremely high for First Nations people. Suicide rates among First Nations individuals are between 3 and 6 times that of the general population.27 Canadian First Nations suicide rates are higher than in the general population in both the United States and Canada.25 In a population-based examination of the Province of Manitoba, individuals living in Northern communities (largely consisting of First Nations individuals) were also at increased likelihood for suicide and suicide attempts.32 The link between complicated grief and increased risk for suicidal behavior has also been demonstrated,33,34 as well as the increased likelihood for CG among individuals bereaved by suicide.35-38 Although these relationships have not been examined in First Nations populations, the role of acculturation and multiple traumas may play a role in these relationships. Chandler and Lalonde highlight the role of cultural continuity as a protective factor against youth suicide in First Nations.39 Residential school survivors have been found to experience adverse outcomes such as poor mental health, substance abuse, and criminal activity.25 Although First Nations individuals have higher suicide rates compared with other non-First Nations groups, these rates may vary depending on the community as well as individuals in the community. A study by Bolton et al analyzed two American Indian samples and found that American Indians from Northern Plains and Southwest tribes were less likely to have suicidal thoughts as compared with the US general population.40 The authors also found that the Northern Plains tribe had a greater likelihood of attempting suicide. Although some differences were found between tribes, overall American Indian samples were at greater risk for suicide attempts than the US general population.
In another study examining suicidal behavior in First Nations, Mota et al investigated the correlates of suicidal behavior among a Manitoba sample of First Nations adolescents.41 The goal of this study was to examine the individual, friend/family, and community/tribe correlates of suicidal behavior among on-reserve adolescents. The authors found that several factors were found to increase the likelihood of suicidal behavior including female sex, depressed mood, abuse or fear of abuse, hospital stay, and substance use. In this study, perceived community caring played a protective role, in that adolescents were less likely to engage in suicidal behavior if they perceived their community as caring, as determined by a combination of factors regarding community life. Although further investigation is needed to understand the role of community support and suicidal behavior in First Nations, these two studies suggest that the community may play an important role in understanding suicide, as well as the bereavement experience among some First Nations populations.
The importance of culture in healing and resilience
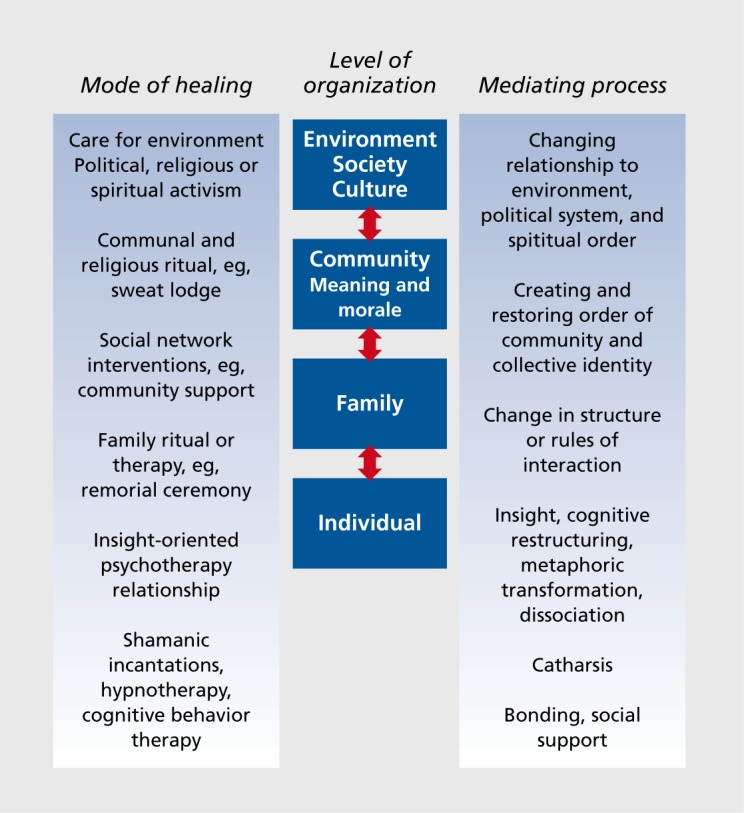
Despite the impact of colonization on Aboriginal peoples and collective traumas, Aboriginal cultures have endured.27 Understanding the role of healing and bereavement in Aboriginal populations necessitates the inclusion of cultural and healing traditions (Figure 1). Kirmayer investigates the symbolic aspects of healing among individuals of different cultures. Using metaphor theory, the author argues that one can understand the course of healing by examining metaphorical concepts.42 Kirmayer discusses a hierarchy of metaphors where there are multiple modes of healing and mediating processes interacting with many levels, such as society and the environment, the community, family, and biological factors. While this hierarchy of metaphors allows a thorough examination of the factors that may impact the course of bereavement in diverse populations, it can be tailored to help understand grief and bereavement in diverse Aboriginal populations (Figure 2). Future research, nevertheless, is needed to examine bereavement among Aboriginal populations, including the development of theoretical models that best explains CG as an outcome of bereavement.
Figure 1. Squamish Nation welcome figure in Vancouver, British Columbia. The figure represents strength, and the importance of carrying on Aboriginal teachings and traditions.

Figure 2. Metaphorical model of healing in Aboriginal populations. Adapted from ref 42: Kirmayer LJ. The cultural diversity of healing: meaning, metaphor and mechanism. Br Med Bull. 2004;69:33-48. Copyright © Oxford University Press 2004.
Future directions
Such studies must include full partnership with Aboriginal communities to help identify risk factors for CG, understand the role of culture among these communities, as well as identify interventions to reduce poor health outcomes such as suicidal behavior. In Manitoba, Canada, the Swampy Cree Suicide Prevention Team has been established to lead such research.43 The team is comprised of international experts, researchers, and community members, and aims to advance the understanding of effective suicide-prevention strategies for First Nations people. Guidance from community members is an essential component of this research team, and is a necessary element of future research in the area of CG. Given the paucity of research examining the dimensions of complicated grief in Aboriginal populations, more research is required. This research must consider the role of culture, intergenerational trauma, and traditional healing practices in order to address this important public health issue.
Acknowledgments
Preparation of this article was supported by research grants from the Canadian Institutes of Health Research (Dr Bolton #102682) and Manitoba Health Research Council (Dr Bolton), a Manitoba Health Research Council Chair Award (Dr Sareen), a CIHR/PHAC Applied Public Health Chair Award (Dr Martens), a SSHRC Joseph-Armand Bombardier Canada Doctoral Scholarship (Ms Spiwak), and a Canadian Institutes of Health Research New Investigator Award (Dr Bolton #113589; Dr Elias # 80503).
Contributor Information
Rae Spiwak, Department of Psychiatry, University of Manitoba, Winnipeg, Manitoba, Canada; Department of Community Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada.
Jitender Sareen, Departments of Psychiatry, Psychology, and Community Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada.
Brenda Elias, Department of Community Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada.
Patricia Martens, Department of Community Health Sciences, University of Manitoba, Winnipeg, Manitoba, Canada.
Garry Munro, Cree Nations Tribal Health Centre, Executive Director.
James Bolton, Department of Psychiatry and Psychology, University of Manitoba, Winnipeg, Manitoba, Canada.
REFERENCES
- 1.Stroebe M., Hansson R., Shut H., Stroebe W. Handbook of Bereavement Research and Practice. Washington, DC: American Psychological Association; 2008 [Google Scholar]
- 2.Shear MK., Simon N., Wall M., et al. Complicated grief and related bereavement issues for DSM-5. Depress Anxiety. 2011;28:118–126. doi: 10.1002/da.20780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cruz M., Scott J., Houck P., Reynolds CF. 3rd, Frank E., Shear MK. Clinical presentation and treatment outcome of African Americans with complicated grief. Psychiatr Serv. 2007;58:700–702. doi: 10.1176/appi.ps.58.5.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fujisawa D., Miyashita M., Nakajima S., Ito M., Kato M., Kim Y. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352–358. doi: 10.1016/j.jad.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Ghaffari-Nejad A., Ahmadi-Mousavi M., Gandomkar M., Reihani-Kermani H. The prevalence of complicated grief among Bam earthquake survivors in Iran. Arch Iran Med. 2007;10:525–528. [PubMed] [Google Scholar]
- 6.Goldsmith B., Morrison RS., Vanderwerker LC., Prigerson HG. Elevated rates of prolonged grief disorder in African Americans. Death Stud. 2008;32:352–365. doi: 10.1080/07481180801929012. [DOI] [PubMed] [Google Scholar]
- 7.Langner R., Maercker A. Complicated grief as a stress response disorder: evaluating diagnostic criteria in a German sample. J Psychosom Res. 2005;58:235–242. doi: 10.1016/j.jpsychores.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 8.Laor N., Wolmer L., Kora M., Yucel D., Spirman S., Yazgan Y. Posttraumatic, dissociative and grief symptoms in Turkish children exposed to the 1999 earthquakes. J Nerv Ment Dis. 2002;190:824–832. doi: 10.1097/00005053-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Momartin S., Silove D., Manicavasagar V., Steel Z. Complicated grief in Bosnian refugees: associations with posttraumatic stress disorder and depression. Compr Psychiatry. 2004;45:475–482. doi: 10.1016/j.comppsych.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 10.Morina N., Rudari V., Bleichhardt G., Prigerson HG. Prolonged grief disorder, depression, and posttraumatic stress disorder among bereaved Kosovar civilian war survivors: a preliminary investigation. Int J Soc Psychiatry. 2010;56:288–297. doi: 10.1177/0020764008101638. [DOI] [PubMed] [Google Scholar]
- 11.Prigerson H., Ahmed I., Silverman GK., et al. Rates and risks of complicated grief among psychiatric clinic patients in Karachi, Pakistan. Death Stud. 2002;26:781–792. doi: 10.1080/07481180290106571. [DOI] [PubMed] [Google Scholar]
- 12.Boelen PA., van den Bout J. Complicated grief, depression, and anxiety as distinct postloss syndromes: a confirmatory factor analysis study. Am J Psychiatry. 2005;162:2175–2177. doi: 10.1176/appi.ajp.162.11.2175. [DOI] [PubMed] [Google Scholar]
- 13.Chiu YW., Huang CT., Yin SM., Huang YC., Chien CH., Chuang HY. Determinants of complicated grief in caregivers who cared for terminal cancer patients. Support Care Cancer. 2010;18:1321–1327. doi: 10.1007/s00520-009-0756-6. [DOI] [PubMed] [Google Scholar]
- 14.Schaal S., Jacob N., Dusingizemungu JP., Elbert T. Rates and risks for prolonged grief disorder in a sample of orphaned and widowed genocide survivors. BMC Psychiatry. 2010;10:55. doi: 10.1186/1471-244X-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schaal S., Elbert T., Neuner F. Prolonged grief disorder and depression in widows due to the Rwandan genocide. Omega. 2009;59:203–219. doi: 10.2190/OM.59.3.b. [DOI] [PubMed] [Google Scholar]
- 16.Forstmeier S., Maercker A. Comparison of two diagnostic systems for Complicated Grief. J Affect Disord. 2007;99:203–211. doi: 10.1016/j.jad.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Fujisawa D., Miyashita M., Nakajima S., Ito M., Kato M., Kim Y. Prevalence and determinants of complicated grief in general population. J Affect Disord. 2010;127:352–358. doi: 10.1016/j.jad.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Bonanno GA., Papa A., Lalande K., Zhang N., Noll JG. Grief processing and deliberate grief avoidance: a prospective comparison of bereaved spouses and parents in the United States and the People's Republic of China. J Consult Clin Psychol. 2005;73:86–98. doi: 10.1037/0022-006X.73.1.86. [DOI] [PubMed] [Google Scholar]
- 19.Kersting A., Kroker K., Horstmann J., et al. Complicated grief in patients with unipolar depression. J Affect Disord. 2009;118:201–204. doi: 10.1016/j.jad.2009.01.033. [DOI] [PubMed] [Google Scholar]
- 20.Kersting A., Kroker K., Steinhard J., et al. Complicated grief after traumatic loss: a 14-month follow up study. Eur Arch Psychiatry Clin Neurosci. 2007;257:437–443. doi: 10.1007/s00406-007-0743-1. [DOI] [PubMed] [Google Scholar]
- 21.Rosenblatt P. Grief across cultures: a review and research agenda. In: Stroebe M, Hansson R, Shut H, Stroebe W, eds. Handbook of Bereavement Research and Practice. Washington, DC: American Psychological Association. 2008 [Google Scholar]
- 22.Neimeyer R., Prigerson H., Davies B. Mourning and meaning. Am Behav Sic. 2002;46:235–251. [Google Scholar]
- 23.Walker AC. Grieving in the Muscogee Creek tribe. Death Stud. 2008;32:123–141. doi: 10.1080/07481180701801238. [DOI] [PubMed] [Google Scholar]
- 24.Bombay A., Matheson K., Anisman H. The impact of stressors on second generation Indian residential school survivors. Transcult Psychiatry. 2011;48:367–391. doi: 10.1177/1363461511410240. [DOI] [PubMed] [Google Scholar]
- 25.Kirmayer LJ., Brass G., Holton T., Paul K., Simpson C., Tait C. Suicide Among Aboriginal People in Canada. Ottawa, Canada: Aboriginal Healing Foundation. 2007 [Google Scholar]
- 26.Health Canada. A Statistical Profile on the Health of First Nations in Canada. Ottawa: Health Canada Publications. 2011 [Google Scholar]
- 27.Kirmayer L., Simpson C., Cargo M. Healing traditions: Culture, community and mental health promotion with Canadian Aboriginal peoples. Australas Psychiatry. 2003;11:s15–s23 (supplement). [Google Scholar]
- 28.Raphael B., Swan P., Martinek N. Intergenerational aspects of trauma for Australian Aboriginal people. In: Danieli Y, ed. International Handbook of Multigenerational Legacies of Trauma. New York, NY: Plenum Press. 1998 [Google Scholar]
- 29.Duran E., Duran B., Yellow Horse Brave Heart M., Yellow Horse-Davis S. Healing the American Indian Soul Wound In: Danieli Y, ed. International Handbook of Multigenerational Legacies of Trauma. New York, NY: Plenum Press. 1998 [Google Scholar]
- 30.Brave Heart MYH. Healing the historical trauma and historical unresolved grief response among the lakota through a psychoeducational group intervention. Smith College Studies in Social Work. 1998;68:287–305 (0037-7317). [Google Scholar]
- 31.Gagne M. The Role of Dependency and Colonialism is Generating Trauma in First Nations Citizens. In: Danieli Y, ed. International Handbook of Multigenerational Legacies of Trauma. New York, NY: Plenum Press. 1998 [Google Scholar]
- 32.Martens P., Fransoo R. the Need To Know Team. What Works? A First Look at Evaluating Manitoba 's Regional Health Programs and Policies at the Population Level. Winnipeg, Canada: Manitoba Centre for Health Policy. 2008 [Google Scholar]
- 33.Ajdacic-Gross V., Ring M., Gadola E., et al. Suicide after bereavement: an overlooked problem. Psychol Med. 2008;38:673–676. doi: 10.1017/S0033291708002754. [DOI] [PubMed] [Google Scholar]
- 34.Stroebe M., Stroebe W., Abakoumkin G. The broken heart: suicidal ideation in bereavement. Am J Psychiatry. 2005;162:2178–2180. doi: 10.1176/appi.ajp.162.11.2178. [DOI] [PubMed] [Google Scholar]
- 35.de Groot M., de Keijser J., Neeleman J., Kerkhof A., Nolen W., Burger H. Cognitive behavior therapy to prevent complicated grief among relatives and spouses bereaved by suicide: cluster randomized controlled trial. BMJ. 2007;334:294. doi: 10.1136/bmj.39161.457431.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vessier-Batchen M., Douglas D. Coping and complicated grief in survivors of homicide and suicide decendents. J Forensic Nurs. 2006;2:25–32. doi: 10.1111/j.1939-3938.2006.tb00050.x. [DOI] [PubMed] [Google Scholar]
- 37.Mitchell AM., Kim Y., Prigerson HG., Mortimer M. Complicated grief and suicidal ideation in adult survivors of suicide. Suicide Life Threat Behav. 2005;35:498–506. doi: 10.1521/suli.2005.35.5.498. [DOI] [PubMed] [Google Scholar]
- 38.Mitchell M. Complicated grief in survivors of suicide. Crisis. 2004;25:12–18. doi: 10.1027/0227-5910.25.1.12. [DOI] [PubMed] [Google Scholar]
- 39.Chandler M., Lalonde C. Cultural continuity as a protective factor against suicide in First Nations youth. Horizons. 2008;10:68–72. [Google Scholar]
- 40.Bolton S., Elias B., Enns M., et al. A comparison of the prevalence and risk factors of suicidal ideation and suicide attempts in two American Indian and a general population sample. Transcult Psychiatry. In press. doi: 10.1177/1363461513502574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mota N., Elias B., Tefft B., Medved M., Munro G., Sareen J. Swampy Cree Suicide Prevention Team. Correlates of suicidality: investigation of a representative sample of Manitoba First Nations adolescents. Am J Pub Health. In press. doi: 10.2105/AJPH.2011.300385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kirmayer LJ. The cultural diversity of healing: meaning, metaphor and mechanism. Br Med Bull. 2004;69:33–48. doi: 10.1093/bmb/ldh006. [DOI] [PubMed] [Google Scholar]
- 43.Katz LY., Elias B., O'Neil J., et al. Aboriginal suicidal behaviour research: from risk factors to culturally-sensitive interventions. J Can Acad Child Adolesc Psychiatry. 2006;15:159–167. [PMC free article] [PubMed] [Google Scholar]


