Abstract
Building on interpersonal theories of depression, the current study sought to explore whether early childhood social withdrawal serves as a risk factor for depressive symptoms and diagnoses in young adulthood. The researchers hypothesized that social impairment at age 15 would mediate the association between social withdrawal at age 5 and depression by age 20. This mediational model was tested in a community sample of 702 Australian youth followed from mother’s pregnancy to youth age 20. Structural equation modeling analyses found support for a model in which childhood social withdrawal predicted adolescent social impairment, which, in turn, predicted depression in young adulthood. Additionally, gender was found to moderate the relationship between adolescent social impairment and depression in early adulthood, with females exhibiting a stronger association between social functioning and depression at the symptom and diagnostic level. This study illuminates one potential pathway from early developing social difficulties to later depressive symptoms and disorders.
Keywords: social withdrawal, interpersonal functioning, social impairment, depression, community sample, longitudinal studies
Interpersonal difficulties and depression have been linked in children, adolescents, and adults (e.g., Hirschfield et al., 2000; Rudolph et al. 2000). Researchers have found that interpersonal factors such as stressful interpersonal events, loneliness, marital distress, and social skills deficits all serve as risk factors for depression (see Joiner, Coyne, & Blalock, 1999 for a review). Longitudinal studies have demonstrated that impaired or limited social relationships and poor family functioning are prospectively associated with depressive symptoms (Daley, Rizzo, & Gunderson, 2006; Dill & Anderson, 1999; Eberhart & Hammen, 2006). Interpersonal dysfunction has also been linked to the course of depression, such that levels of social support and interpersonal impairment predict depression severity, rate of recovery from a depressive episode, and depression recurrence (Hammen, Brennan, & Keenan-Miller, 2008; Lara, Leader, and Klein, 1997). Even after depression remits, the lives of individuals with a history of depression continue to be characterized by interpersonal impairment. Formerly depressed individuals report more negative interactions with family, friends, and romantic partners than their never-depressed counterparts (Zlotnick, Kohn, Keitner, & Della Grotta, 2000). Individuals with a history of depression also experience more dependent, interpersonal stressful life events, such as family arguments or romantic break-ups for which the individual was partially responsible (Cui & Vaillant, 1997; Hammen, 1991a). In light of the significant role that interpersonal difficulties play in the onset and maintenance of depression, various authors have recommended further examination of the nature of this interpersonal impairment (e.g., Hammen & Brennan, 2002). The current study applies a developmental perspective to investigate the childhood origins of interpersonal difficulties. Specifically, we examine whether early childhood social withdrawal portends interpersonal impairment in adolescence and, in turn, depression by young adulthood.
Interpersonal Consequences of Social Withdrawal
Social withdrawal is defined as the behavioral tendency to isolate oneself from peers (Rubin & Coplan, 2004). The tendency to withdraw from others appears to be moderately stable over time (from early childhood to adolescence) and across diverse social situations (Rubin, Coplan, & Bowker, 2009). Researchers have used a variety of measures to assess social withdrawal, including peer reports (e.g., Revised Class Play; Masten, Morison, & Pelligrini, 1985), observational measures (e.g., Play Observation Scale; Rubin, 2001), and parent reports (e.g., select items from the Child Behavior Checklist; Achenbach & Rescorla, 2006) (Rubin et al. 2009). There is a general consensus in the literature that the motivations behind social withdrawal are varied, ranging from a disinterest in engaging with peers to an anxious avoidance of desired social contact (e.g., Coplan, Gavinski-Molina, Lagacé-Séguin, & Wichmann, 2001).
There is an abundance of evidence to suggest that childhood disengagement from peers predicts negative social and emotional outcomes. Childhood social withdrawal is associated with peer victimization (Dill, Vernberg, Fonagy, Twemlow, & Gamm, 2004; Mayeux, Bellmore, & Cillessen, 2007) and loneliness (Cacioppo et al., 2006; Hymel, Rubin, Rowden, & LeMare, 1990; Mahon, Yarcheski, Yarcheski, Canella, & Hanks, 2006; Rubin, Hymel, & Mills, 1989), and is inversely related to observed peer acceptance and peer-reported likeability (Hart et al., 2000; Nelson, Rubin, & Fox, 2005; Strauss, Forehand, Smith, & Frame, 1986). In addition to eliciting unfavorable reactions from peers, children who withdraw from others also tend to perceive themselves as less competent in multiple domains (Hymel et al., 1990). Longitudinal data suggest that negative perceptions of one’s own social competence can exacerbate social inhibition and lead to greater chronic strain in interpersonal relationships, relationship disruptions, and peer-related stressful life events (Caldwell, Rudolph, Troop-Gordon, & Kim, 2004). These negative social outcomes reflect the types of ongoing interpersonal difficulties that may confer risk for depressive symptomatology.
This is not to say, however, that socially withdrawn children are doomed to a life of solitude, void of close friendships. In fact, previous research indicates that the majority of socially withdrawn children appear to have at least one best friend, whose friendship is maintained for at least one school year (Rubin, Wojslawowicz, Rose-Krasnor, Booth-LaForce, & Burgess, 2006). Problematically, these friendships may not be as intimate or fulfilling as those of children who are not socially withdrawn; the friendships of socially withdrawn children seem to be characterized by limited self-disclosure and are, according to friends of withdrawn children, relatively less fun and helpful than those friendships involving non-withdrawn peers (Rubin et al., 2006). This research suggests that even when withdrawn children make close friendships, these friendships may be of a lower quality than the friendships of sociable children.
Further support for the hypothesis that withdrawal in childhood leads to increased risk for interpersonal impairment in subsequent developmental periods comes from literature on the delayed life transitions of individuals who displayed shyness or limited sociability in childhood. Males rated as shy during childhood get married, become parents, and obtain occupational stability later in life than relatively less shy counterparts (Caspi, Edler, & Bem, 1988; Kerr, Lambert, & Bem, 1996). Similarly, low sociability in adulthood predicts a reduced likelihood of establishing relationships, getting married, and having children in the succeeding decade (Jokela, Kivimäki, Elovainio, & Keltikangas-Järvinen, 2009; Neyer & Lehnart, 2007). All told, social withdrawal appears to be predictive of interpersonal difficulties, such as peer rejection, peer victimization, loneliness, poor social self-concept, lower quality friendships, and delays (or difficulties) in establishing romantic and occupational relationships.
Social Withdrawal and Depression
Prior work has provided evidence in support of a direct, positive relationship between social withdrawal and depression. A concurrent association between social withdrawal and depression has been found in children (e.g., Strauss et al., 1986), adolescents (e.g., Vargo, 1996), and young adults (e.g., Alfano, Joiner, & Perry, 1994). The prospective relationship between childhood social withdrawal and depression in later childhood or adolescence has also been demonstrated in several studies. The Waterloo Longitudinal Project, for example, aimed at determining long-term consequences of early childhood social withdrawal, revealed that social withdrawal in kindergarten, as assessed by behavioral observation, predicted self-reported depressive symptoms in fifth grade (Rubin, Hymel, & Mills, 1989). Ollendick, Greene, Weist, and Oswald (1990) found similar results following children from fourth grade to ninth grade. Caspi, Moffitt, Newman, and Silva (1996), utilizing data from the Dunedin birth cohort study, reported that the emotional consequences of childhood disengagement also extend into adulthood; they found that inhibited three-year-olds were more likely to be clinically depressed by age 21 than children who were “well-adjusted” at age 3. One limitation of this study was its lack of statistical control for internalizing problems at age 3. That is, the significant association found between childhood inhibition and early adulthood depression may be confounded by general emotional difficulties present in early childhood.
In addition to examining the direct effect of social withdrawal on internalizing problems, some researchers have sought to clarify the mechanisms through which this relationship occurs. Previous studies have identified cognitive factors (e.g., maladaptive attributional styles; Alfano, Joiner, & Perry, 1994), coping strategies (Findlay, Coplan, & Bowker, 2009), and interpersonal variables (e.g., loneliness; Joiner, 1997) that appear to mediate the relationship between social reticence and internalizing difficulties. Much of this research on pathways from withdrawal to internalizing symptoms has been cross-sectional or prospective over a relatively short (e.g., several weeks) time frame. However, Boivin, Hymel, and Bukowski (1995) examined mediators of the relationship between social withdrawal and depressed mood over a two-year interval in elementary school-aged children with promising results. These authors found support for a model in which both peer victimization and loneliness served as mediators of the withdrawal-internalizing symptoms association.
A Mediational Model of Social Withdrawal, Interpersonal Impairment, and Depression
Missing from the existing literature is an examination of a developmental model in which social withdrawal, evidenced in early childhood, confers risk for interpersonal difficulties in adolescence, which, in turn, predict subsequent depressive outcomes. The transition to adulthood is a high-risk time for the development of clinically significant depression; 25% of all lifetime cases of major depressive disorder begin by age 19 (Kessler et al., 2005). For this reason, the current study examines whether childhood social withdrawal (assessed at age 5, consistent with previous literature; e.g., Rubin, Hymel, & Mills, 1989) is an early risk factor for the development of depression during this high-risk period via its long-term effects on interpersonal functioning. Previous literature has demonstrated that the social difficulties experienced in middle adolescence predict depression in the transition to adulthood (e.g., Hammen, Shih, & Brennan, 2004), providing support for the examination of social impairment in middle adolescence and depression in early adulthood. In contrast to some previous studies (e.g., Caspi et al., 1996), the current study aims to examine the effect of childhood social withdrawal on later social and emotional outcomes, over and above the emotional difficulties that may co-occur with withdrawn behavior in childhood. In other words, by controlling for internalizing problems in early childhood, the current study seeks to identify the risks posed by social withdrawal that are independent of risk related to internalizing symptoms.
The current study aims to answer the following questions: 1) Does early childhood social withdrawal predict interpersonal impairment in adolescence? 2) Does interpersonal impairment mediate the association between childhood social withdrawal and depression in young adulthood? We hypothesize that social withdrawal, measured at age 5, predicts interpersonal difficulties at age 15. Additionally, we expect that social impairment at age 15 confers risk for major depression by age 20 and depressive symptoms in young adulthood. Finally, we predict that interpersonal impairment serves as a mediator in the indirect relationship between childhood social withdrawal and depressive symptoms and diagnoses in young adulthood.
In addition to examining this mediational model, the current study seeks to explore gender differences in the pathways from social withdrawal to interpersonal impairment and from interpersonal impairment to depression. Previous research has found that adolescent females may be more sensitive to difficulties in interpersonal relationships than adolescent males, such that females are more likely to develop depressive symptoms in response to stressful events of an interpersonal nature (see Leadbeater, Blatt, & Quinlan, 1995; Shih, Eberhart, Hammen, & Brennan, 2006). Cyranowski, Frank, Young, and Shear (2000) suggest that this gender difference in reactivity to interpersonal stressors may be due to greater affiliative needs in females compared to males. Theorists have also posited other explanations for this gender difference, including biological factors and gender differences in coping styles (Nolen-Hoeksma, 2001). In light of this research, we hypothesize that the relationship between interpersonal impairment and depressive symptoms will be stronger for females than for males. The current study will also examine gender differences in the relationship between childhood social withdrawal and adolescent interpersonal difficulties on an exploratory basis, but no a priori hypotheses are made regarding the nature of gender differences in this relationship. The current study uses a longitudinal design with three time points spanning 15 years to explore these research questions.
Method
Participants
The current sample consists of 702 individuals (339 [48.3%] males and 363 [51.7%] females) from Queensland, Australia. These individuals were part of a larger birth cohort study, the Mater-University of Queensland Study of Pregnancy (MUSP; Keeping et al., 1989), designed to examine how pregnancy, obstetric conditions, birth weight, and psychosocial conditions relate to children’s cognitive, psychological, behavioral and health-related development up to age 5. The original sample included 7,223 children born between 1981 and 1984 at the Mater Misericordiae Mother’s Hospital in Brisbane, Queensland, Australia and their mothers.
Of the birth cohort sample, 816 youth were selected for follow up at age 15 on the basis of responses to the Delusions-Symptoms-States Inventory (DDSI; Bedford & Foulds, 1978) completed by their mothers at pregnancy and three times before youth age 5. Participants were selected to represent a range of exposure to maternal depression, in terms of both severity and chronicity of maternal depressive symptoms, ranging from no depression to clinically significant depressive disorders. The sample included an overrepresentation of mothers with depression, such that 68% of mothers endorsed some depressive symptoms by youth age 5 and 11% of mothers reported severe depressive symptoms during at least two of the four assessments conducted by youth age 5. For further information regarding procedures of sample recruitment and screening, see Hammen, Shih, and Brennan (2004).
706 participants (87% of the sample) were retained at age 20. Attrition was due to death (2), refusal to participate (51), or failure to be located or scheduled (52); 5 participants were excluded due to incomplete data. Of these participants, 1 withdrew and 3 were excluded from analyses due to maternal history of bipolar disorder, resulting in 702 participants in the current sample. Consistent with previous research utilizing this sample, participants whose mothers had a history of bipolar disorder were omitted to ensure that any effects of maternal depression were due to unipolar, rather than bipolar, depression, as these two disorders may have different implications for offspring’s functioning. Compared to the 110 individuals that were not followed to age 20, participants included in current analyses were more likely to be female (χ2(1, n = 812) = 8.96, p < .01) and marginally less likely to have mothers with a history of major depressive disorder (χ2(1, n = 812) = 3.43, p = .06). The two groups did not differ with respect to youth depressive disorder diagnosis—dysthymia or major depressive disorder, as per the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Revised (K-SADS-E; Orvaschel, 1995)—prior to age 15 (χ2(1, n = 812) = 1.37, p = 0.24).
Procedure
When the participants were 5 years of age, mothers were asked to complete a series of questionnaires pertaining to health, attitudes, parenting style, and their children’s behavior. This battery included selected questions from the problem behavior scales of the Child Behavior Checklist (CBCL; Achenbach, 1991) as well as questions about children’s social behavior.
At ages 15 and 20, extensive interview and questionnaire sessions with participants and their mothers were held at the participants’ homes or at locations convenient for the participants and interviewer. Postgraduate students were trained to appropriately conduct and reliably score these interviews. Participants all gave informed consent, or assent in the case of minors. The institutional review/ethics panels of the University of Queensland, University of California, Los Angeles, and Emory University approved the research protocol.
Measures
Social withdrawal
Social withdrawal was assessed using selected items from questionnaires administered to mothers at participants’ age 5. Indicators of social withdrawal included 4 items that comprised a shortened Withdrawn subscale from an abbreviated Child Behavior Checklist (Achenbach, 1991), a widely used and well-validated measure of behavioral problems in children. The modified version of the CBCL used in the current study included 33 of the original 113 items on the full length CBCL, chosen for appropriateness for a 5-year-old sample (Najman et al., 2008). Reliability estimates indicate that the modified CBCL has similar psychometric properties as the original measure (see Najman et al., 2001). Strong correlations have been found between long and short form CBCL internalizing scale scores in mothers completing both forms of the measure (r = 0.89; Najman et al., 1997).
On the CBCL Withdrawn subscale, mothers reported on a scale from 0 to 2 whether their child never, sometimes, or often is “withdrawn, doesn’t get involved with others,” “sulks a lot,” “refuses to talk,” or “likes to be alone.” One additional CBCL item asked mothers to choose from four multiple choice answers about their child’s approximate number of acquaintances. In structural equation modeling analyses, these five ordinal items were considered indicators of a single latent variable representing social withdrawal.
Internalizing problems
Internalizing behaviors at age 5 were assessed using the Internalizing scale of the modified CBCL. In this modified version of the CBCL, the Internalizing scale is comprised primarily of items from the Withdrawn and Anxious/Depressed subscales of the CBCL. The CBCL Internalizing scale has adequate internal consistency in this sample (Cronbach’s alpha = 0.77). For the purposes of the current analyses, Withdrawn subscale scores were subtracted from Internalizing scale scores to create a new internalizing variable that omitted items pertaining to withdrawn behavior. This internalizing variable was included in the model to control for general emotional difficulties at age 5 and to examine the unique effect of childhood social withdrawal on later social and emotional problems.
Social impairment
Two measures were used to assess social impairment at age 15. First, a semi-structured interview for adolescents, based on the UCLA Life Stress Interview (LSI) for adults (Hammen, 1991b), was used to assess participants’ chronic stress and ongoing functioning in their peer relationships. Interviewers inquired about the participants’ social lives over the previous six months using a standard set of probes and follow up queries when necessary. Social functioning was scored on a scale of 1 to 5, with half-points permitted (e.g., 2.5), with 1 indicating superior functioning and 5 indicating significantly impaired functioning. For example, a score of 1 would be given to an individual who has many friends, engages in frequent and varied social activities, and does not experience conflict in social situations. An individual with some weekly contact with friends or some conflictual relationships with peers would score a 3. An individual who has no friends, has been rejected by peers, or experiences frequent and severe conflict with friends or acquaintances would receive a score of a 5. Reliabilities for this measure were based on independent judges’ ratings of 88 (11% of initial sample) audiotaped interviews. The intraclass correlation for ratings on this measure was 0.63. Validation of this measure was reported in Hammen, Brennan, and Keenan-Miller (2008) and included significant correlations between the interview measure of peer functioning and ratings of peer acceptance/rejection and popularity completed by homeroom teachers.
Second, participants’ mothers reported on adolescents’ level of social impairment during the past six months by completing the 8-item Social Problems subscale of the Child Behavior Checklist (Achenbach, 1991) at youth age 15. Mothers rated their children on a scale from 0 to 2 for each item, with higher scores reflecting more interpersonal difficulties. Individual item scores were summed to form a composite measure that was found to have adequate internal consistency in this sample (Cronbach’s alpha = 0.77). Sample items on this subscale include “doesn’t get along with other kids, “gets teased a lot,” and “clings to adults or too dependent.”
Depressive symptoms
Depressive symptoms were assessed at age 20 using the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996). The BDI-II is a well-validated 21-item self-report questionnaire of depressive symptoms. 78.6% of participants had scores between 0 and 10, 12.9% of participants scored between 11 and 20, and 8.5% of participants scored higher than 20. Eighty-four (12.0%) participants scored at or above the commonly used clinical cutoff of 16. Cronbach’s alpha was 0.93 at age 20, indicating strong internal consistency.
Depression diagnoses
Participants were administered a structured clinical interview at both age 15 and age 20. At age 15, participants completed the K-SADS-E (Orvaschel, 1995). Current diagnosis of major depressive disorder was assessed at age 15. Seventeen (2.4%) participants met criteria for a current major depressive episode at age 15. Independent judges’ ratings of audiotaped interviews yielded a weighted Kappa of 0.82.
The Structured Clinical Interview for DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams, 1995), administered at age 20, assessed for major depressive episodes since age 15. 25.5% (N = 179) of participants experienced onsets of a major depressive episode between ages 15 and 20. Independent judges’ ratings’ of 55 (8% of retained sample) audiotaped interviews indicated strong inter-rater reliability for current diagnostic status (weighted Kappa = 0.83) and past major depressive episodes (weighted Kappa = 0.89). Principal investigators resolved disagreements among raters based on all available information.
Maternal depression
Previous research has found a link between maternal depression and internalizing problems, especially in younger children (Goodman et al., 2011). There is also evidence to suggest that depressed mothers may be negatively biased when reporting on their child’s emotional difficulties (Goodman et al., 2011). In order to control for the possibility that early childhood social withdrawal or adolescent social problems could be an artifact of maternal depression and its concomitants (e.g., family discord) or may be overreported by depressed mothers, maternal depression was included as a covariate in analyses. Consistent with previous research on maternal depression (e.g., Hammen et al., 2008), maternal history of major depressive disorder was assessed at youth age 15. Using the SCID-IV (First et al., 1995), interviewers assessed for lifetime and current major depressive disorder diagnoses. Forty-five percent (N = 315) of mothers had a history of depression by youth age 15. Inter-rater reliability ratings, based on independent judges’ ratings of 55 (7% of initial sample) interviews, yielded weighted κ=0.87 for diagnoses of current diagnoses of depression, and weighted κ=0.84 for past depressive disorders. As with youth depression diagnosis, principal investigators resolved disagreements among raters based on all available information.
Results
Descriptive statistics and bivariate or polychoric correlations among all observed variables are presented in Table 1. In analyses examining depression diagnoses, no more than 2% of participants had missing data on any variable. Data were missing for 11% of participants on self-reported depressive symptoms. Separate structural equation models were estimated to evaluate mediational models at the diagnostic and symptom level. For each model we assumed that data were missing at random. Non-normal (positively skewed) distributions were observed for mother-reported CBCL social problems and age 20 BDI-II score. Robust maximum likelihood procedures were carried out in Mplus (Muthén & Muthén, 1998) to obtain estimates corrected for missingness and non-normality in the data.
Table 1. Correlation Matrix of Measured Variables.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age 5 | ||||||||||||
| 1. “Likes to be alone” (CBCL 1) | - | 0.31** | 0.08 | 0.35** | 0.10 | 0.17** | 0.10* | -0.02 | -0.08* | -0.03 | -0.06 | -0.02 |
| 2. “Refuses to talk” (CBCL 2) | - | 0.41** | 0.49** | 0.09 | 0.32** | 0.11* | 0.15** | 0.01 | 0.05 | 0.07 | 0.05 | |
| 3. “Sulks a lot” (CBCL 3) | - | 0.40** | 0.10 | 0.46** | 0.05 | 0.19** | 0.02 | 0.03 | 0.08 | 0.02 | ||
| 4. “Withdrawn” (CBCL 4) | - | 0.30** | 0.46** | 0.10* | 0.13** | 0.00 | 0.07 | 0.05 | 0.03 | |||
| 5. Number of friends | - | 0.14** | 0.16** | 0.08 | 0.03 | 0.11** | 0.08 | 0.05 | ||||
| 6. Internalizing problems | - | 0.11** | 0.24** | 0.01 | 0.08* | 0.10** | 0.08* | |||||
| Age 15 | ||||||||||||
| 7. Youth-reported social functioning | - | 0.40** | 0.14** | 0.08* | 0.13** | 0.09* | ||||||
| 8. Mother-reported social problems | - | 0.13** | 0.13** | 0.20** | 0.15** | |||||||
| 9. Current youth MDD diagnosis | - | 0.10** | 0.26** | 0.17** | ||||||||
| 10. Maternal depression history | - | 0.18** | 0.07 | |||||||||
| Age 20 | ||||||||||||
| 11. Depressive symptoms | - | 0.42** | ||||||||||
| 12. Depression diagnoses (ages 15-20) | - | |||||||||||
| Means | 2.59 | 2.28 | 1.66 | 7.00 | ||||||||
| (SD) | (0.48) | (0.48) | (2.37) | (8.35) |
p < .05
p < .01.
Bivariate correlation coefficients are reported for all correlations between two continuous variables. Polychoric correlation coefficients are reported for correlations including categorical variables.
Measurement Models
All items from the CBCL Withdrawn subscale, along with the item assessing number of friendships, were used as indicators of a latent variable representing childhood social withdrawal. Due to low base rates of responses indicating few child friendships on the child acquaintances item, we collapsed across the two response options indicating the fewest number of child acquaintances such that scores on this variable were either 0, 1, or 2, with higher values representing fewer friends. The variance of the latent factor was constrained to 1.0 to identify the model. A unidimensional model provided acceptable fit to the data (χ2(9) = 244.29, p < .001; comparative fit index of 0.95 [CFI; Hu & Bentler, 1999]; a root mean square error of approximation of 0.06 with a 95% confidence interval of 0.05 to 0.07 [RMSEA; Browne & Cudeck, 1993]; and a standardized root mean square residual of 0.06 [SRMSR; Muthén & Muthén, 1998]). Standardized factor loadings ranged from 0.27 to 0.75 and were all significant at the 0.01 level.
To establish that the latent social withdrawal variable was not simply indexing negative affectivity, we additionally estimated the measurement model without the CBCL “sulks a lot” item. A unidimensional model continued to provide a good fit to the data when this item was omitted (CFI = .98, RMSEA = .03, WRMR = .53) and the pattern of significant results from later mediation analyses was unaltered in both symptom and diagnosis models. Thus, this item was included in final analyses.
A second latent variable indexing social impairment at age 15 was postulated to account for the correlation between adolescents’ LSI Social Life score and mother-reported CBCL Social Problems. As there were only two indicators of this latent variable, we did not evaluate a measurement model.
Mediation Model: Depression Diagnoses
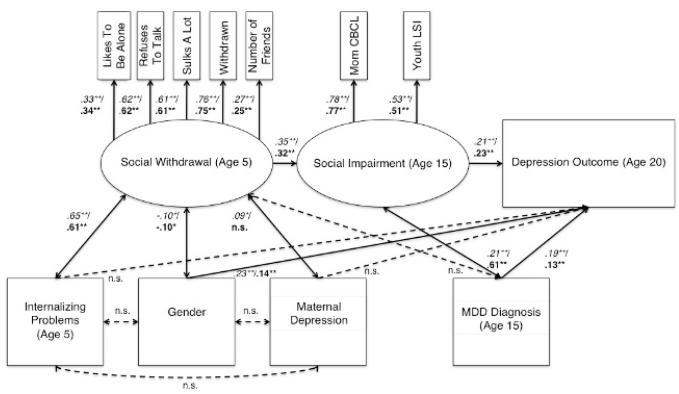
To examine the indirect effect of childhood social withdrawal on liability to depressive disorder between ages 15 and 20, diagnoses of major depression were regressed on the social impairment latent variable, which was in turn regressed on the social withdrawal latent variable. Covariates in the model included gender, maternal history of depression prior to youth age 15, and children’s score on the age 5 CBCL internalizing scale excluding all withdrawal items. Youth current diagnosis of depression at age 15 was included as a final covariate to ensure that the mediating effects of social impairment at age 15 were not due to overlap with depression. A schematic of this structural model is shown in Figure 1. This model provided an excellent fit to the data (χ2(38) = 677.96, p < .001; CFI = 0.97; RMSEA = .03 with a 95% confidence interval of 0.01-0.04; SRMSR = 0.05).
Figure 1.
Schematic of the structural equation model testing the indirect effect of childhood social withdrawal on depression in early adulthood via adolescent social impairment. Path coefficients in italics represent values from the model with major depression diagnosis as the outcome variable. Path coefficients in boldface represent values from the model with depressive symptoms as the outcome variable. Standardized path coefficients are presented. Paths that were nonsignificant in both models are represented by dotted lines. *p<0.05, **p <0.001
It is important to note that no direct effect of social withdrawal on depression diagnosis (or depressive symptomatology) was hypothesized. Modern guidelines for testing mediation do not require a significant association between the independent variable and the outcome variable if the predictor-mediator and mediator-outcome associations are hypothesized to be comparatively stronger than the association between the predictor and outcome variables (see Collins, Graham, & Flaherty, 1998; MacKinnon, 2000). Consistent with this conceptualization of age 5 social withdrawal as a distal and indirect risk factor for depression in late adolescence, no main effect of withdrawal on risk for depression diagnoses between ages 15 and 20, b = 0.18, SE = 0.33, z = 0.56, p = .58.
In support of our hypothesis, childhood social withdrawal exerted a significant prospective effect on social impairment in adolescence, b = 0.36, SE = 0.10, z = 3.61, p < .001. It is noteworthy that this result was obtained despite a sizeable and significant correlation between the social withdrawal latent variable and the CBCL Internalizing scale (with Withdrawn items omitted), b = 0.38, SE = 0.08, z = 4.80, p < .001. Social impairment at age 15, in turn, was longitudinally associated with greater likelihood of onset of a major depressive disorder between ages 15 and 20, b = 0.82, SE = 0.24, z = 3.43, p < .001. The point estimate of the indirect effect of childhood social withdrawal on risk for depression was 0.29, and the 95% confidence interval around this value ranged from 0.07-0.51, indicating that adolescent social impairment significantly mediated this association.
Mediation Model: Depressive Symptoms
Results from the model predicting depressive symptoms differed only in degree from those produced by the diagnosis-level analysis. Overall, the model provided adequate fit to the data (χ2(38) = 621.30, p < .001; CFI = 0.93; RMSEA = .05 with a 95% confidence interval of 0.04-0.06; SRMSR = 0.05). Again, no main effect of withdrawal on age 20 depressive symptoms was detected, b = 0.90, SE = 2.04, z = 0.44, p = .66. Also, consistent with the previous model, childhood social withdrawal was a significant predictor of adolescent social impairment, b = 0.41, SE = 0.12, z = 3.33, p < .001. Further, a strong longitudinal association between adolescent social impairment and depressive symptoms at age 20 was observed, b = 6.79, SE = 1.25, z = 5.45, p < .001. Examination of the indirect effect of social withdrawal on depressive symptoms via adolescent social impairment again revealed significant mediation, point estimate = 2.76, 95% CI = 0.96-4.56.
Gender Moderation
A multiple-group structural equation modeling approach was employed to evaluate the consistency of the mediational paths across gender. Two models were compared to examine gender moderation of each structural path. In one, the path coefficient was constrained to be equal for males and females. In the other, the magnitude of the coefficient was free to vary across gender. A Satorra-Bentler chi-square difference test was used to compare the fit of these two models (Satorra & Bentler, 2001). This procedure was carried out for each mediation path in both depression diagnosis and symptom models. Chi-square difference tests revealed that constraining the path from early withdrawal to later social impairment to equality across gender did not significantly degrade fit of either the depression diagnosis, χ2(1, n = 703) = 0.31, p = .58, or depressive symptom, χ2(1, n = 703) = 0.23, p = .63, models. This suggests that the effect of withdrawal on subsequent social impairment is equally potent for males and females.
Regarding the structural path linking adolescent social impairment and depression, the chi-square difference test indicated that constraining the association of social impairment and depression diagnosis to be equal for males and females resulted in a significant deterioration in model fit, χ2(1, n = 703) = 8.71, p < .01. Consistent with hypotheses, the regression of depression diagnosis on social impairment was nonsignificant for males, b = 0.43, SE = 0.29, z = 1.50, p = .13, whereas for females a strong positive association was observed, b = 1.86, SE = 0.40, z = 4.65, p < .001.
This pattern of results was even more robust in the depressive symptom model. The chi-square difference test clearly indicated that gender moderated the relationship between social impairment and later depressive symptoms, χ2(1, n = 703) = 15.31, p < .001. In contrast to the diagnosis model, the association between social impairment and depressive symptoms was significant and in the expected direction for males, b = 5.08, SE = 1.28, z = 3.98, p < .001. However, again consistent with expectations, this association was more pronounced among females, b = 16.98, SE = 2.80, z = 6.06, p < .001.
Discussion
The current study sought to evaluate a developmental model linking early social maladjustment to depressive symptoms and diagnosis in the transition to adulthood. In line with previous literature addressing the negative outcomes for children who are socially withdrawn, it was hypothesized that childhood social withdrawal would serve as a risk factor for adolescent interpersonal impairment, which would in turn portend risk for depressive symptoms and diagnoses in young adulthood. The current results provide strong support for this mediational pathway. These findings are consistent with previous research demonstrating a longitudinal relationship between social withdrawal and negative social outcomes (Rubin, Coplan, & Bowker, 2009) as well as a prospective link between interpersonal difficulties and depression (Hammen, 2005). It is important to note that the risk conferred by early childhood social withdrawal was significant despite controls for gender, maternal depression, internalizing problems at age 5, and depression diagnosis at age 15. By controlling for childhood internalizing symptoms, we demonstrated the unique contribution of early disengagement from peers, rather than the emotional problems that may underlie this behavior, to the development of poor social functioning and depression. By controlling for youth current depression diagnosis at age 15, we were able to demonstrate that the mediating effect of social impairment in adolescence in the pathway from childhood withdrawal to young adult depression was not an artifact of the correlation between social impairment and adolescent depression.
Significant associations were not found between the latent variable indexing social withdrawal and the depression outcomes. Thus, the findings do not support a direct pathway from social withdrawal to depression. Rather, social withdrawal exerts its influence on depressive disorders or symptoms only to the extent that it contributes to ongoing social difficulties that, in turn, portend negative emotional outcomes. The current findings suggest that social withdrawal may be considered a distal risk factor. That is, socially withdrawn children may be no more likely than non-withdrawn children to experience depression in early adulthood; however, they are at risk for more interpersonal problems, which, as evidenced in the current analyses and previous research, place individuals at risk for problems with depression.
A second aim of the current study was to examine the moderating role of gender in both the longitudinal relationship between social withdrawal and social impairment and the prospective relationship between social impairment and depression. No gender differences were found in the strength of the relationship between childhood social withdrawal and interpersonal difficulties in adolescence, suggesting that the social lives of male and female teenagers are equally affected by the degree to which they evidence social withdrawal in childhood. In contrast, consistent with prior work showing greater depressive reactivity among females in the face of interpersonal stress (Shih et al., 2006), the association between social difficulties in adolescence and depression in young adulthood was found to be stronger for females than males. In the diagnostic outcome models, a significant relationship between social impairment and depression emerged for females but not for males. This finding suggests that while individuals of both genders may experience emotional difficulties following impairment in social functioning, females may have greater depressive reactivity to social difficulties than males. Further, the tendency for social difficulties to portend a clinically significant, major depressive episode may be unique to female populations. Whereas males may develop depressive symptoms following interpersonal problems, these social difficulties may only rarely trigger a major depressive episode.
One surprising finding of the current study was the significant relationship between social withdrawal and gender. Males exhibited more withdrawn behavior than females. This finding differs from previous research on early childhood social behavior, which has tended to find no differences in the prevalence of social withdrawal between the sexes (Rubin, Burgess, & Coplan, 2002). Further research is needed to corroborate and examine this sex difference.
The current study expands upon existing literature by revealing a pathway from social withdrawal to depression across a 15-year period. While previous studies have demonstrated that childhood social withdrawal serves as a risk factor for depressive symptoms in adolescence (e.g., Rubin, Chen, McDougall, Bowker, & McKinnon, 1995), the current study suggests that the risk conferred by childhood social withdrawal extends into early adulthood as well. Boivin, Hymel, and Bukowski (1995) similarly found support for a model in which social withdrawal predicts negative social experiences and subsequent depressed mood. However, they examined these processes over a span of only two years during childhood. Using three separate time points, the current study revealed that this pathway—withdrawal to depressed mood via social impairment—also traverses developmental stages spanning childhood, adolescence, and early adulthood. Additional study strengths include the large community sample, multi-informant assessment in adolescence, and the use of structural equation modeling to reduce measurement error.
Several limitations should be noted that may be important for guiding future research. First, as the study was not originally designed to test a hypothesis concerning the effects of childhood social withdrawal, no established, previously validated measure of withdrawal behavior was administered at participants’ age 5. Ideally, observational measures would have been included to allow for an objective observer’s account of social withdrawal in children. Instead, the current study used latent variable modeling to establish a latent social withdrawal construct defined by four indicators of social withdrawal from an abridged Withdrawn subscale of a modified Child Behavior Checklist (Achenbach, 1991) plus one additional indicator reflecting the child’s number of acquaintances. Although these five items did not comprise a previously validated measure of social withdrawal, relevant items from the Child Behavior Checklist have been used in previous literature to assess social withdrawal (Rubin et al., 2009). Furthermore, analyses demonstrated that all five items loaded significantly onto one latent factor and that the overall model provided an adequate fit to the data. Thus, there was evidence that the measure of social withdrawal utilized in the study was a moderately cohesive construct with significant predictive validity.
A second limitation was the fact that the current study did not discriminate between the various types of social withdrawal (i.e., solitary-active withdrawal; solitary-passive withdrawal; reticence) that have been associated with diverse trajectories (e.g., Coplan et al., 2001). Thus, we cannot draw any conclusions regarding the motivations behind withdrawal behavior; we can only assert that this behavioral marker may be an early indicator of chronic interpersonal difficulties and, in some cases, later emotional problems. Along the same lines, the limited information gathered about children’s social behavior at age 5 prevented statistical control for early childhood general social functioning in the latent variable modeling procedures. Thus, no definitive conclusions can be drawn regarding the unique predictive power of early childhood social withdrawal behavior over and above global social deficits. However, the statistical control of internalizing problems at age 5 suggests that the link between social withdrawal and later difficulties is not merely an artifact of early negative affectivity.
Third, the current study did not assess anxiety disorders or internalizing problems more broadly at age 20. Thus, it is unknown whether this developmental model would apply to anxiety outcomes as well as depression. Future research should examine the role of anxiety in this developmental model.
The findings of the current study have significant implications for understanding the etiology of depression. While previous literature has suggested that interpersonal difficulties serve as a predictor of depressive symptoms (e.g., Hammen et al., 2004), more research is needed to determine the specific nature of the interpersonal difficulties characteristic of individuals prone to depression. The current study suggests that there may be a behavioral tendency to withdraw from peers that is evidenced in early childhood and that contributes to ongoing difficulties in peer relationships that can subsequently lead to depression. Thus, interpersonal difficulties that precipitate and maintain depression may be related to difficulties that are present during early years of social interaction. It is possible that social withdrawal reflects a temperament or personality trait that can initiate and maintain the cycle of negative social experiences and depressive symptoms. The current study provides support for a developmental pathway that begins early in life with social withdrawal and culminates in elevated depressive symptoms, and, in some cases, major depressive disorder by early adulthood.
Acknowledgments
This research was supported by the National Health and Medical Research Council, the Mater Misericordiae Mothers’ Hospital in Queensland, Australia, and the National Institute of Mental Health grant R01 MH52239. We are thankful for the work of project coordinators, Robin LeBrocque, Cheri Dalton Comber, and Sascha Hardwicke, and the many members of the MUSP, M900, and M20 research teams. We gratefully acknowledge William Bor, Michael O’Callaghan, and Gail Williams, principal investigators of the original Mater-University of Queensland Study of Pregnancy. Special thanks to the parents and youth in the Mater cohort, without whom this research would not have been possible.
References
- Achenbach TM. Integrative guide to the 1991 CBCL, YSR, and TRF profiles. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Multicultural Understanding of Child and Adolescent Psychopathology: Implications for Mental Health Assessment. Guilford; New York: 2006. [Google Scholar]
- Alfano MS, Joiner TE, Perry M. Attributional style: a mediator of the shyness-depression relationship? Journal of Research in Personality. 1994;28(3):287–300. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bedford A, Foulds G. Delusions-Symptoms-States Inventory of Anxiety and Depression. NFER; Windsor, England: 1978. [Google Scholar]
- Boivin M, Hymel S, Bukowski WM. The roles of social withdrawal, peer rejection, and victimization by peers in predicting loneliness and depressed mood in childhood. Development and Psychopathology. 1995;7:765–785. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, Spiegel D. Loneliness within a nomological net: an evolutionary perspective. Journal of Research in Personality. 2006;40:1054–1085. [Google Scholar]
- Caldwell MS, Rudolph KD, Troop-Gordon W, Kim D. Reciprocal influences among relational self-views, social disengagement, and peer stress during early adolescence. Child Development. 2004;75:1140–1154. doi: 10.1111/j.1467-8624.2004.00730.x. [DOI] [PubMed] [Google Scholar]
- Caspi A, Elder GH, Jr., Bem DJ. Moving away from the world: life-course patterns of shy children. Developmental Psychology. 1988;24:824–831. [Google Scholar]
- Caspi A, Moffitt TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders: longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- Collins LM, Graham JW, Flaherty BP. An alternative framework for defining mediation. Multivariate Behavioral Research. 1998;33:295–312. doi: 10.1207/s15327906mbr3302_5. [DOI] [PubMed] [Google Scholar]
- Coplan RJ, Gavinski-Molina MH, Lagacé-Séguin D, Wichmann C. When girls versus boys play alone: gender differences in the associates of nonsocial play in kindergarten. Developmental Psychology. 2001;37:464–474. doi: 10.1037//0012-1649.37.4.464. [DOI] [PubMed] [Google Scholar]
- Cui X, Vaillant GE. Does depression generate negative life events? Journal of Nervous and Mental Disease. 1997;185:145–150. doi: 10.1097/00005053-199703000-00003. [DOI] [PubMed] [Google Scholar]
- Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Archives of General Psychiatry. 2000;57:21–27. doi: 10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- Daley SE, Rizzo CJ, Gunderson BH. The longitudinal relation between personality disorder symptoms and depression in adolescence: the mediating role of interpersonal stress. Journal of Personality Disorders. 2006;20(4):352–368. doi: 10.1521/pedi.2006.20.4.352. [DOI] [PubMed] [Google Scholar]
- Dill EJ, Vernberg EM, Fonagy P, Twemlow SW, Gamm BK. Negative affect in victimized children: the roles of social withdrawal, peer rejection, and attitudes toward bullying. Journal of Abnormal Child Psychology. 2004;32(2):159–173. doi: 10.1023/b:jacp.0000019768.31348.81. [DOI] [PubMed] [Google Scholar]
- Dill JC, Anderson CA. Loneliness, shyness, and depression: the etiology and interrelationships of everyday problems in living. In: Joiner T, Coyne JC, editors. The Interactional Nature of Depression. American Psychological Association; Washington, D. C.: 1999. pp. 93–125. [Google Scholar]
- Eberhart NK, Hammen CL. Interpersonal predictors of onset of depression during the transition to adulthood. Personal Relationships. 2006;13:195–206. [Google Scholar]
- Findlay LC, Coplan RJ, Bowker A. Keeping it all inside: shyness, internalizing coping strategies and socio-emotional adjustment in middle childhood. International Journal of Behavioral Development. 2009;33:47–54. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders. American Psychiatric Press; Washington: 1995. [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clinical Child and Family Psychology Review. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Hammen C. The generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991a;100(4):555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C. Depression runs in families: The social context of risk and resilience in children of depressed mothers. New York; Springer-Verlag: 1991b. [Google Scholar]
- Hammen C. Stress and depression. Annual Reviews of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Interpersonal dysfunction in depressed women: impairments independent of depressive symptoms. Journal of Affective Disorders. 2002;72(2):145–156. doi: 10.1016/s0165-0327(01)00455-4. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Keenan-Miller D. Patterns of adolescent depression to age 20: the role of maternal depression and youth interpersonal dysfunction. Journal of Abnormal Child Psychology. 2008;36:1189–1198. doi: 10.1007/s10802-008-9241-9. [DOI] [PubMed] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72(3):511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Hart CH, Yang C, Nelson LJ, Robinson CC, Olsen JA, Nelson DA, Porter CL, Jin S, Olsen SF, Wu P. Peer acceptance in early childhood and subtypes of socially withdrawn behaviour in China, Russia, and the United States. International Journal of Behavioral Development. 2000;24(1):73–81. [Google Scholar]
- Hirschfield MD, Montgomery SA, Keller MB, Kasper S, Schatzberg AF, Möller H, Healy D, Baldwin D, Humble M, Versiani M, Montenegro R, Bourgeois M. Social functioning in depression: a review. Journal of Clinical Psychiatry. 2000;61(4):268–275. doi: 10.4088/jcp.v61n0405. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hymel S, Rubin KH, Rowden L, LeMare L. Children’s peer relationships: longitudinal prediction of internalizing and externalizing problems from middle to late childhood. Child Development. 1990;61(6):2004–2021. [Google Scholar]
- Joiner T, Coyne JC, Blalock J. On the interpersonal nature of depression: overview and synthesis. In: Joiner T, Coyne JC, editors. The Interactional Nature of Depression. American Psychological Association; Washington, D. C.: 1999. pp. 3–19. [Google Scholar]
- Joiner TE., Jr. Shyness and low social support as interactive diatheses, with loneliness as mediator: testing an interpersonal-personality view of vulnerability to depressive symptoms. Journal of Abnormal Psychology. 1997;106(3):386–394. doi: 10.1037//0021-843x.106.3.386. [DOI] [PubMed] [Google Scholar]
- Jokela M, Kivimäki M, Elovainio M, Keltikangas-Järvinen L. Personality and having children: a two-way relationship. Journal of Personality and Social Psychology. 2009;96(1):218–230. doi: 10.1037/a0014058. [DOI] [PubMed] [Google Scholar]
- Keeping JD, Najman JM, Morrison J, Western JS, Andersen MJ, Williams GM. A prospective longitudinal study of social, psychological, and obstetrical factors in pregnancy: Response rates and demographic characteristics of the 8,556 respondents. British Journal of Obstetrics and Gynaecology. 1989;96:289–297. doi: 10.1111/j.1471-0528.1989.tb02388.x. [DOI] [PubMed] [Google Scholar]
- Kerr M, Lambert WW, Bem DJ. Life course sequelae of childhood shyness in Sweden: comparison with the United States. Developmental Psychology. 1996;32(6):1100–1105. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Lara ME, Leader J, Klein DN. The association between social support and course of depression: is it confounded with personality? Journal of Abnormal Psychology. 1997;103(3):478–482. doi: 10.1037//0021-843x.106.3.478. [DOI] [PubMed] [Google Scholar]
- Leadbeater BJ, Blatt SJ, Quinlan DM. Gender-linked vulnerabilities to depressive symptoms, stress, and problem behaviors in adolescents. Journal of Research on Adolescence. 1995;5:1–29. [Google Scholar]
- MacKinnon DP. Contrasts in multiple mediator models. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Erlbaum; Mahwah, NJ: 2000. pp. 141–160. [Google Scholar]
- Mahon NE, Yarcheski A, Yarcheski TJ, Cannella BL, Hanks MM. Meta-analytic study of predictors for loneliness during adolescence. Nursing Research. 2006;55(5):308–315. doi: 10.1097/00006199-200609000-00003. [DOI] [PubMed] [Google Scholar]
- Masten AS, Morison P, Pelligrini DS. A revised class play method of peer assessment. Developmental Psychology. 1985;3:523–533. [Google Scholar]
- Mayeux L, Bellmore AD, Cillessen AHN. Predicting changes in adjustment using repeated measures of sociometric status. Journal of Genetic Psychology. 2007;168(4):401–424. doi: 10.3200/GNTP.168.4.401-424. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Muthén & Muthén; Los Angeles: 1998. [Google Scholar]
- Najman JM, Behrens BC, Andersen M, Bor W, O’Callaghan M, Williams GM. Impact of family type and family quality on child behavior problems: a longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1357–1365. doi: 10.1097/00004583-199710000-00017. [DOI] [PubMed] [Google Scholar]
- Najman JM, Heron MA, Hayatbakhsh MR, Dingle K, Jamrozik K, Bor W, O’Callaghan MJ, Williams GM. Screening in early childhood for risk of later mental health problems:a longitudinal study. Journal of Psychiatric Research. 2008;42:694–700. doi: 10.1016/j.jpsychires.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Najman JM, Williams GM, Nikles J, Spence S, Bor W, O’Callaghan M, Shuttlewood GJ. Bias influencing maternal reports of child behaviour and emotional state. Social Psychiatry and Psychiatric Epidemiology. 2001;36:186–194. doi: 10.1007/s001270170062. [DOI] [PubMed] [Google Scholar]
- Nelson LJ, Rubin KH, Fox NA. Social withdrawal, observed peer acceptance, and the development of self-perceptions in children ages 4 to 7 years. Early Childhood Research Quarterly. 2005;20:185–200. [Google Scholar]
- Neyer FJ, Lehnart J. Relationships matter in personality development: evidence from an 8-year longitudinal study across young adulthood. Journal of Personality. 2007;75(3):535–568. doi: 10.1111/j.1467-6494.2007.00448.x. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Gender differences in depression. Current Directions in Psychological Science. 2001;10:173–176. [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115:424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Greene RW, Weist MD, Oswald DP. The predictive validity of teacher nominations: a five-year follow up of at-risk youth. Journal of Abnormal Child Psychology. 1990;18:699–713. doi: 10.1007/BF01342755. [DOI] [PubMed] [Google Scholar]
- Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic version-5. Nova Southeastern University, Center for Psychological Studies; Ft. Lauderdale, FL: 1995. [Google Scholar]
- Rubin KH. The Play Observation Scale (POS) University of Maryland; College Park: 2001. [Google Scholar]
- Rubin KH, Burgess KB, Coplan RJ. Social withdrawal and shyness. In: Smith PK, Hart CH, editors. Blackwell handbook of childhood social development. Blackwell; Malden, MA: 2002. pp. 329–352. [Google Scholar]
- Rubin KH, Chen X, McDougall P, Bowker A, McKinnon J. The Waterloo Longitudinal Project: predicting adolescent internalizing and externalizing problems from early and mid-childhood. Development and Psychopathology. 1995;7:51–64. [Google Scholar]
- Rubin KH, Coplan RJ. Paying attention to and not neglecting social withdrawal and social isolation. Merrill-Palmer Quarterly. 2004;50(4):506–534. [Google Scholar]
- Rubin KH, Coplan RJ, Bowker JC. Social withdrawal in childhood. Annual Review of Psychology. 2009;60:141–171. doi: 10.1146/annurev.psych.60.110707.163642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin KH, Hymel S, Mills RSL. Sociability and social withdrawal in childhood: stability and outcomes. Journal of Personality. 1989;57(2):237–255. doi: 10.1111/j.1467-6494.1989.tb00482.x. [DOI] [PubMed] [Google Scholar]
- Rubin KH, Wojslawowicz JC, Rose-Krasnor L, Booth-LaForce C, Burgess KB. The best friendships of shy/withdrawn children: prevalence, stability, and relationship quality. Journal of Abnormal Child Psychology. 2006;34:143–157. doi: 10.1007/s10802-005-9017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, Daley SE. Toward an interpersonal life-stress model of depression: the developmental context of stress generation. Development and Psychopathology. 2000;12:215–234. doi: 10.1017/s0954579400002066. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih JH, Eberhart NK, Hammen CL, Brennan PA. Differential exposure and reactivity to interpersonal stress predict sex differences in adolescent depression. Journal of Clinical Child and Adolescent Psychology. 2006;35(1):103–115. doi: 10.1207/s15374424jccp3501_9. [DOI] [PubMed] [Google Scholar]
- Strauss CC, Forehand R, Smith K, Frame CL. The association between social withdrawal and internalizing problems of children. Journal of Abnormal Child Psychology. 1986;14(4):525–535. doi: 10.1007/BF01260521. [DOI] [PubMed] [Google Scholar]
- Vargo B. Are withdrawn children at risk? Canadian Journal of School Psychology. 1996;11(2):166–177. [Google Scholar]
- Zlotnick C, Kohn R, Keitner G, Della Grotta SA. The relationship between quality of interpersonal relationships and major depressive disorder: findings from the National Comorbidity Survey. Journal of Affective Disorders. 2000;59(3):205–215. doi: 10.1016/s0165-0327(99)00153-6. [DOI] [PubMed] [Google Scholar]