Abstract
Objective
Although active diabetes self-management is required to achieve glycemic control, adherence is poor among ethnic minorities, especially Latinos. Research shows that individuals who report greater social-environmental support resources for disease management manage their diabetes more effectively than those with fewer support resources.
Methods
Path analysis was conducted to investigate the value of a multiple-mediator model in explaining how support resources for disease management influence hemoglobin A1c (HbA1c) levels in a sample of 208 Latinos with type 2 diabetes recruited from low-income serving community clinics in San Diego County. We hypothesized that the relationship between support resources for disease-management and HbA1c would be mediated by diabetes self-management and/or depression.
Results
Participants who perceived greater support resources for disease-management reported better diabetes self-management (β = .40, p < .001) and less depression (β = −.19, p < .01). In turn, better diabetes self-management and less depression were associated with tighter glycemic control (HbA1c; β = −.17, p < .05 and β = .15, p < .05, respectively). Once the indirect effects via diabetes self-management (95% CI [−.25; −.03]) and depression (95% CI [−.14; −.01]) were statistically controlled, the direct pathway from support resources to HbA1c was markedly reduced (p = .57).
Conclusions
These findings demonstrate the important connection that support resources for disease management can have with diabetes self-management, emotional well-being, and glycemic control among Latinos. Thus, programs targeting diabetes self-management and glycemic control in this population should consider culturally-relevant, multi-level influences on health outcomes.
Keywords: social-environmental support resources, diabetes self-management, HbA1c, depression, diabetes
Approximately 29 million, or 7.2% of individuals in the United States are expected to have a diagnosis of type 2 diabetes by the year 2050, an increase of nearly 165% from the year 2000 (Boyle, et al., 2001). Similar to other chronic conditions, type 2 diabetes is unequally distributed across ethnic groups (Centers for Disease Control and Prevention, 2008). For instance, if current trends continue, over 20% of the Latino population in the US is expected to have diabetes by the year 2031 (Mainous, et al., 2007). Individuals with uncontrolled diabetes are at risk for developing serious health complications, including hypertension, dyslipidemia, cardiovascular disease, retinopathy, nephropathy, and neuropathy. In order to delay or prevent the development and progression of these and other health problems, individuals with diabetes must maintain tight glycemic control [for a review, see (Skyler, 2004)]. Latinos with type 2 diabetes, however, commonly exhibit poorer glycemic control (Mexican-Americans, in particular: Harris, 2001), and thus, more frequent health complications, greater disease severity, and worse outcomes than non-Latino whites (Centers for Disease Control and Prevention).
Social-Environmental Support Resources for Disease Management
Research has linked social support, defined and measured in various ways, to several indicators of physical health (Uchino, 2004; Uchino, Cacioppo, & Kiecolt-Glaser, 1996) including glycemic control (Okura, Heisler, & Langa, 2009). Glasgow, Strycker, Toobert, & Eakin (2000) proposed a comprehensive, social-ecological framework that is especially relevant for assessing multiple levels of support in the context of a chronic illness. The Chronic Illness Resources Survey (CIRS) evaluates social-environmental support resources for disease management from proximal sources, such as family, friends, and healthcare providers, and from more distal sources that are infrequently considered, including the community, workplace, media and policy (Glasgow et al.). Among individuals with type 2 diabetes, greater support resources for disease management, as assessed by the CIRS, has been associated with lower levels of hemoglobin A1c (HbA1c), a widely used marker of glycemic control where lower levels indicate better control (Barrera, Toobert, Angell, Glasgow, & MacKinnon, 2006; Barrera, Strycker, Mackinnon, & Toobert, 2008). Little is known, however, about the potential mechanism(s) underlying this relationship. As such, the current study sought to understand how social-environmental support resources for disease management affects glycemic control in Latino with type 2 diabetes by examining two potential mediators of this relationship: diabetes self-management and depression.
Diabetes Self-Management
Diabetes self-management, a prerequisite for tight glycemic control (ADA, 2002), involves daily engagement in a variety of behaviors, including healthy eating, physical activity, blood glucose monitoring, taking medications, problem solving, and adaptive coping. Completing these tasks on a regular basis, however, can be demanding and limiting, and requires significant lifestyle modifications. These changes generally occur in a social context of friends, family, healthcare providers, and the greater community, all of which can influence adherence to a diabetes self-care regimen (Barrera et al., 2006). In fact, individuals with type 2 diabetes who reported receiving greater support resources for disease management from these sources exhibited better physical activity (i.e., caloric expenditure from exercise) and dietary outcomes (i.e., fat and fiber intake) than individuals with less support (Barrera et al., 2006; Barrera et al., 2008; Glasgow, Toobert, Barrera, & Strycker, 2005; King, et al., 2010). An investigation of support from proximal sources only (i.e., “support persons”) showed that support for disease management related to greater adherence to blood-glucose monitoring, which in turn predicted better glycemic control in a sample of African Americans with type 2 diabetes (Brody, Kogan, Murry, Chen, & Brown, 2008). Given these observed links between support resources for disease management and diabetes self-management, as well as the well-established connection between self-management and glycemic control, we hypothesized that the relationship between social-environmental support resources for disease management and glycemic control (i.e., HbA1c levels) would be explained, in part, by an indirect effect via diabetes self-management.
Depression and Diabetes Outcomes
Depression is two times more prevalent among persons with type 2 diabetes than in the general population (Anderson, Freedland, Clouse, & Lustman, 2001). Emotional distress is even more common among Latinos than blacks and non-Latino whites with the same condition (Spencer, et al., 2006). Further, consistent relationships have been observed between depression and glycemic control (Lustman, et al., 2000), including prospective positive associations between depression and HbA1c levels (Richardson, Egede, Mueller, Echols, & Gebregziabher, 2008). Co-morbid depression has also been linked to more frequent diabetes complications (Black, Markides, & Ray, 2003; de Groot, Anderson, Freedland, Clouse, & Lustman, 2001) and increased mortality risk in patients with diabetes (Katon et al., 2005). Although the mechanisms underlying these associations are still under investigation, and likely include a combination of complex physiological and behavioral processes, research suggests depression exerts at least some of its influence impairing diabetes self-management (Gonzalez, et al., 2008). Notably, individuals with type 2 diabetes who experience co-morbid depression exhibit poorer adherence to medication regimens (Ciechanowski, Katon, & Russo, 2000; Katon et al., 2009), and are less likely to follow diet, exercise, and blood glucose monitoring recommendations than are non-depressed individuals (Egede & Osborn, 2010; Lin, et al., 2004; McKellar, Humphreys, & Piette, 2004).
Notably, previous research has identified social support (not health specific) as protecting against the development of depression among individuals with chronic illness (Connell, Davis, Gallant, & Sharpe, 1994). In fact, research has shown that individuals with type 2 diabetes who report receiving more social support are less likely to exhibit co-morbid depression than those with relatively less support (Egede & Osborn, 2010; Pineda Olvera, Stewart, Galindo, & Stephens, 2007). Multi-level support systems may play an especially important role in self-management, and thus glycemic control in the Latino population, due to the cultural value placed on personal relationships and family (Marin, 1993; Sanchez-Burks, Nisbett, & Ybarra, 2000). As such, we hypothesized that at least some of the association between support resources for disease management and glycemic control would be accounted for by reduced depression.
Current Aims
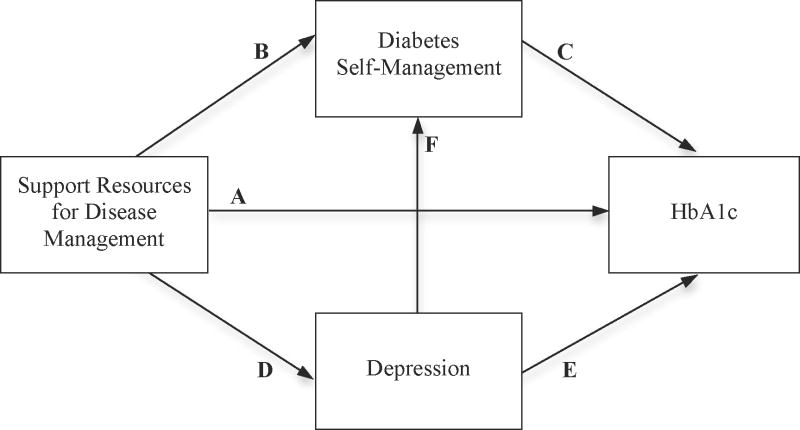
The present study investigated the value of a multiple mediator model (see Figure 1) in explaining how support resources for disease management (defined in the current study as social-environmental support and resources for disease management from proximal and distal sources) influences HbA1c levels in a sample of Latino men and women (majority of Mexican descent) with type 2 diabetes. We examined the direct pathway from support resources to HbA1c (Arrow A), and also investigated whether this relationship could be explained, in part, by indirect effects via self-management (Arrows B and C) and depression (Arrows D and E). In addition, we investigated a double-mediator pathway from support resources to HbA1c via both depression (primary mediator) and self-management (secondary mediator; Arrows D, F, and C). We hypothesized that with control for these indirect paths, the direct relationship between support resources for disease management and HbA1c would be substantially reduced.
Figure 1.
Multiple mediator model, including all possible indirect pathways from support resources for disease management to HbA1c. Arrow A depicts the direct pathway from support resources for disease management to HbA1c. Arrows B and C represent a potential indirect pathway from support resources for disease management to HbA1c via diabetes self-management. Arrows D and E show that depression may partially account for the relationship between support resources for disease management and HbA1c. Arrows B, F, and E represent a double-mediator pathway from support resources for disease management to HbA1c, via both diabetes self-management and depression.
Methods
Participants
Participants were part of a larger, randomized trial of a culturally tailored, community health worker-led psychoeducation intervention designed to promote blood glucose control and reduce diabetes complications, i.e., “Project Dulce” (Philis-Tsimikas et al., 2004). The sample consisted of 208 Latino men and women between the ages of 21 and 75 years old, with type 2 diabetes and HbA1c greater than 8%, who were un- or under-insured patients (or willing to enroll) at low-income serving community clinics in San Diego County. Individuals with a physical or mental health condition that would preclude fulfilling the requirements of the study were ineligible to participate.
Procedures
Participants were recruited through a variety of methods, including provider referrals, medical chart reviews, waiting room demonstrations, and flyers posted in the clinics. Individuals who expressed an interest in participating were screened for eligibility via phone or in person by a bi-lingual, bi-cultural clinical trials assistant. Those who met eligibility criteria heard a thorough explanation of the study requirements, and once all questions were answered, provided written informed consent. All procedures were approved by the San Diego State University and Western Institutional Review Boards.
Following the consenting process, a baseline assessment was scheduled, during which a trained, bi-lingual, bi-cultural clinical trials assistant performed a clinical assessment with fasting blood draw and administered psychosocial measures. Participants were then randomized either to a treatment condition consisting of eight, peer-led diabetes self-management classes and subsequent monthly support groups, or to a usual care (i.e., control) condition. Labs and psychosocial assessments were also collected at the end of the intervention period (Month-4), and six months later (Month-10); however, only data collected at the baseline assessment are included in the current study.
Measures
Surveys were available in both Spanish and English; however, all participants reported Spanish as their preferred language, and thus, completed the battery in Spanish.
Social-Environmental Support Resources for Disease Management
Support resources for disease management were measured using 13 items from the Chronic Illness Resources Survey (CIRS; Glasgow, et al., 2000; Glasgow, et al., 2005). Respondents reported, on a five-point scale (“not at all” to “a great deal”), the amount of support resources received over the past three months from family and friends (e.g., “Have family or friends exercised with you?”), healthcare providers (e.g., “Has your doctor or other health care advisor listened carefully to what you had to say about your illness?”), the community (e.g., “Have you eaten at a restaurant that offered a variety of tasty, low-fat food choices?”), and from within (i.e., personal support; e.g., “Have you arranged your schedule so that you could more easily do the things you needed to do for your illness?”). To reduce participant burden, and because these sources of support were not targeted by the intervention, the media/policy, organizational, and work/volunteer CIRS subscales were not administered. Responses to all other items were averaged to create an overall support resources score for each participant. The CIRS has demonstrated good internal consistency (α =.79), test-retest reliability (.89 over 4 weeks), and convergent validity, and has been shown to predict quality of life and behavioral adherence in longitudinal research, among patients with chronic illnesses (Glasgow, et al., 2000). The Spanish version has also exhibited good internal consistency (α =.78), test-retest reliability (.89 over two weeks), and validity, and was deemed appropriate for use among Latinos and patients with varied education levels (Eakin, et al., 2007). The abbreviated 13-item version of the Spanish CIRS that was used in the current study exhibited good internal consistency (α =.86).
Diabetes Self-Management
Diabetes self-management was measured with 6 items from the Summary of Diabetes Self-Care Activities scale (SDSCA; Toobert, Hampson, & Glasgow, 2000). Participants reported the number of days in the past week (0–7) they had completed self-management behaviors (e.g., blood-glucose monitoring, diet, and exercise). Responses were averaged to create a self-management score for each participant. The SDSCA has demonstrated adequate test-retest reliability and evidence of construct validity in the form of theoretically consistent associations with other measures of diet and exercise (Toobert et al.); the SDSCA measure has also been translated into Spanish, and the Spanish version has been shown to have adequate psychometric properties (Borges & Ostwald, 2008).
Depression
Participants also completed the PHQ-9 (Kroenke, Spitzer, & Williams, 2001), a widely used measure of depression in primary care and other populations. Respondents indicate on a 4-point scale (“not at all” to “nearly every day”) the extent to which they have experienced each of the nine criteria for Major Depressive Disorder over the past 2 weeks (American Psychiatric Association, 1994). The items are summed to create a summary indicator of depression severity. The PHQ-9 has exhibited good internal consistency (α = .86 – .89), test-retest reliability (r = .84) and validity (Kroenke, et al.) and has also been translated and validated in Spanish (Wulsin, Somoza, & Heck, 2002). The Spanish PHQ-9 demonstrated good reliability in the current sample (α = .84).
Glycemic Control
Glycemic control was assessed via HbA1c, an integrated marker of glycemic control, where higher levels indicate worse control. HbA1c reflects an individual’s average plasma glucose concentration over the previous two to three months; values less than 6.5% are considered optimal (American Diabetes Association, 2010).
Sociodemographic Characteristics
Participants self reported gender, date of birth, national origins, marital status, educational attainment (according to four categories: some elementary school/5 years or less, some middle school/6–8years; some high school/9–12 years without diploma; high school diploma/GED or greater), monthly income (according to 17 categories, ranging from < $500 to ≥ $8000 per month), and whether or not they had health insurance.
Statistical Analyses
Analyses were performed using SPSS 17.0 and MPlus. Descriptive statistics were calculated, and all model residuals were plotted and examined. No evidence of substantial deviations from normality or heterogeneous error variances was observed. Because age, gender, and educational attainment were related to depression, these variables were controlled for in all analyses. Income was not included as a covariate because it was not associated with any variable under investigation, and due to the range restriction observed in this sample.
Simple Mediation Models
Two simple mediation models were examined to determine whether depression and/or self-management partially accounts for the relationship between support resources for disease management and HbA1c. Bootstrap estimates based upon 5000 resamples were obtained for each indirect effect using the SPSS Macro for Simple Mediation (Preacher & Hayes, 2004). The use of bootstrapping is recommended over the Sobel test (Sobel, 1982, 1986) and the causal steps approach (Baron & Kenny, 1986; Kenny, Kashy, & Bolger, 1998) since it does not impose the assumption of normality of the sampling distribution, and has greater power while maintaining reasonable control of the Type I error rate (Mackinnon, Lockwood, & Williams, 2004; Preacher & Hayes, 2008).
Multiple Mediator Model
Path analysis (Kerlinger & Pedhazur, 1973) was conducted to evaluate all indirect pathways from support resources for disease management to HbA1c in a single multiple mediator model. Specifically, diabetes self-management and depression were regressed on support resources for disease management, self-management was regressed on depression, and then HbA1c was regressed on all three variables. Chi-square, root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR) test-statistics were evaluated to determine model fit. Bootstrap estimates based upon 5000 resamples were obtained to investigate each indirect effect.
Results
Descriptive Statistics
Participants (N = 208) ranged in age from 21 to 75 years (M = 50.61, SD = 10.93); the majority was female (71%), born in Mexico (88%), and uninsured (67%). Approximately 25% of the sample exhibited PHQ-9 scores ≥10, a cut-off that has demonstrated a sensitivity of 88% and a specificity of 88% for major depression in previous research (Kroenke, Spitzer, & Williams, 2001). Table 1 provides additional demographic characteristics for the sample, and descriptive statistics for HbA1c and all psychosocial variables.
Table 1.
Demographic Statistics
| Variable | n (%) |
|---|---|
| Gender | |
| Female | 147 (70.7) |
| Male | 61 (29.3) |
| Marital status | |
| Married | 104 (50.0) |
| Unmarried | 104 (50.0) |
| Country of origin | |
| Mexico | 182 (87.5) |
| United States | 18 (8.7) |
| Other | 8 (3.8) |
| Insurance coverage | |
| Insured | 68 (32.7) |
| Uninsured | 140 (67.3) |
| Education | |
| ≤ 5 years/elementary | 56 (26.9) |
| 6–8 years/middle school | 64 (30.8) |
| 9–12 years/some high school | 53 (25.5) |
| ≥ High school diploma/GED | 35 (16.8) |
| Monthly income | |
| <$1000/month | 103 (49.5) |
| $1001–$1999/month | 79 (38.0) |
| ≥$2000/month | 26 (12.5) |
| Variable | N | Min | Max | M | SD |
|---|---|---|---|---|---|
| HbA1c (%) | 208 | 7.9a | 15.3 | 10.4 | 1.7 |
| Support resources for disease management | 208 | 1.00 | 5.00 | 3.04 | 0.94 |
| Diabetes self-management | 207b | 0.33 | 7.00 | 3.15 | 1.41 |
| Depression | 207b | 0 | 23.00 | 5.90 | 5.45 |
Note. Income categories are presented for descriptive purposes, but the full continuum was used in analyses.
Minimum observed value for HbA1c was 7.9%, because an exception to the inclusion criterion of HbA1c >8% was made for one patient whose HbA1c exceeded 8% at screening and enrollment, but decreased to 7.9% by the baseline assessment.
One participant did not complete depression items, and another omitted diabetes self-management items, resulting in N = 207 for each of these variables.
Correlations
Bivariate associations between all study variables are shown in Table 2. All correlations were statistically significant, with coefficients ranging from small (self-management and depression: r = −.15) to large (self-management and support resources for disease management: r = .41) in magnitude.
Table 2.
Bivariate Associations Among Study Variables
| Variable | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| 1. HbA1c | --- | |||
| 2. Support resources for disease management | −.16* | --- | ||
| 3. Diabetes self-management | −.22** | .41** | --- | |
| 4. Depression | .19** | −.18** | −.15* | --- |
Note.
p < .05.
p < .01.
Simple Mediation Models
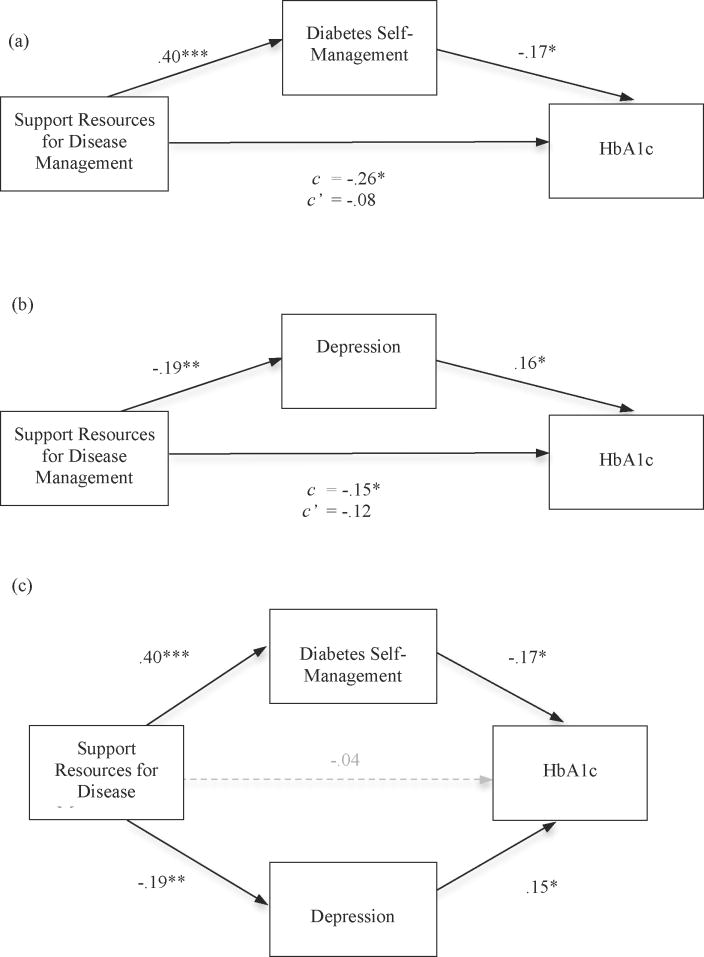
Two simple mediation models were investigated to determine whether the relationship between support resources for disease management and HbA1c was partially accounted for by either or both of the proposed mediators (see Figure 2a–b). Bootstrap estimates revealed significant indirect effects via both self-management (95% CI [−.24; −.02]) and depression (95% CI [−.15; −.01]).
Figure 2.
Results of simple mediation models indicating diabetes self-management (a) and depression (b) as partial mediators of the relationship between support resources for disease management and HbA1c. c = direct relationship between support resources for disease management and HbA1c. c′ = direct relationship between support resources for disease management and HbA1c, after controlling for the proposed mediator. (c) Results of path analysis evaluating the revised model (pathway from depression to self-management removed). Age, gender, and educational attainment were included as covariates in all analyses. Standardized path coefficients are presented.
*p < .05. **p < .01. *** p < .001.
Multiple Mediator Model
In order to evaluate the relative magnitude of each indirect effect, path analysis was conducted to simultaneously investigate all possible pathways (as shown in Figure 1) from support resources for disease management to HbA1c. In addition to the two indirect effects examined previously, a double-mediator pathway [the effect of support resources on HbA1c via depression (primary mediator), via self-management (secondary mediator)] was also tested in the multiple mediator model. Results indicated, however, that the path between depression and self-management (and hence the double-mediator pathway) was not significant. Because this model was over-saturated, the non-significant path was removed, and the analysis was repeated to evaluate the more parsimonious model.
The revised model (shown in Figure 2c) fit the data well [χ2(1) = 1.06, p =.30; RMSEA = .02, SRMR = .01]. All individual pathways reached statistical significance except the direct path between support resources for disease management and HbA1c (β = −.04, p = .57). Participants who perceived greater support resources for disease management reported better diabetes self-management (β = .40, p < .001) and less depressive symptomatology (β = −.19, p < .01) than those reporting less support resources. In turn, better diabetes self-management and less depression were both associated with tighter glycemic control (HbA1c; β = −.17, p < .05 and β = .15, p < .05, respectively). Bootstrap estimates indicated that both indirect effects were statistically significant in the multiple mediator model. This suggests that the relationship between support resources for disease management and HbA1c was in part explained by indirect effects via both diabetes self-management (95% CI [−.25; −.03]) and depression (95% CI [−.14; −.01]). Although the cross-sectional nature of these analyses precludes inferences about causation, the proposed model was a better fit to the data than an alternative model in which the pathways were reversed (i.e., from HbA1c to support resources for disease management via diabetes self-management and/or depression; RMSEA >.08).
Discussion
Substantial research has shown that Latinos exhibit a higher prevalence of type 2 diabetes, as well as poorer glycemic control (Harris, 2001), more frequent complications, greater disease severity, and worse health outcomes than non-Latino whites (Centers for Disease Control and Prevention, 2008). Less is known, however, about the psychosocial factors associated with glycemic control in this population. The current study investigated the relationship between social-environmental support resources for disease management and HbA1c among Latino men and women (majority of Mexican descent) with type 2 diabetes, and examined whether diabetes self-management and depression contributed to this association. Findings showed that individuals reporting greater support resources for disease management also reported more adaptive self-management behaviors and less depressive symptomatology, which in turn were associated with lower HbA1c levels.
Notably, based on estimates from previous research, the magnitude of the effect of support resources is likely to have clinically significant implications. Stratton and colleagues (2000) reported that a 1% decrease in HbA1c was associated with a reduction in the relative risk by 21% for any end point related to diabetes, 21% for diabetes-related mortality, 14% for myocardial infarction, and 37% for microvascular complications. In the present study, a one standard-deviation increase in support resources was associated with roughly a 0.3% decrease in HbA1c. Drawing on findings from the UK prospective diabetes study (Stratton et al.), an improvement of this magnitude translates to a relative risk reduction of approximately 7% for mortality, and from about 5 to 12% for a variety of other adverse diabetes-related health outcomes.
Diabetes Self-Management
Glycemic control is partly dependent upon the regular completion of several self-management behaviors, including exercise, dietary modification, foot-care, self-monitoring of blood glucose, and medication adherence (American Diabetes Association, 2002). A variety of interventions aimed at improving self-management in individuals with diabetes have resulted in significant decreases in HbA1c over time (Chiu, et al., 2009; Gold, et al., 2008; Ruggiero, et al., 2010). Consistently, we identified an inverse association between diabetes self-management and HbA1c levels in the present study, highlighting the importance of implementing effective diabetes self-management training programs to achieve better health outcomes among individuals with type 2 diabetes. Such programs may be especially critical in Latinos, who often lack access to healthcare services (Anders et al., 2008), and who frequently exhibit poor adherence to treatment recommendations even when they do have access. For instance, less than 60% of Latino adults with type 2 diabetes receive annual eye and foot exams, and participate in daily blood glucose monitoring (Centers for Disease Control, 2005). Moreover, Latinos with type 2 diabetes perceive self-monitoring of blood glucose as more difficult and have more negative perceptions about future health and well-being relative to Asians, African-Americans, and non-Latino whites with the same condition (Misra & Lager, 2009).
These findings demonstrate the need to identify effective resources for promoting more adaptive self-care in this at-risk population. Integration in a supportive social network can serve this purpose (Barrera et al., 2008), and could be particularly facilitative in Latinos given cultural norms emphasizing the importance of close interpersonal relationships (Marin, 1993; Sanchez-Burks et al., 2000). For instance, encouragement from family members was associated with greater intention to complete blood glucose, cholesterol, and blood pressure screenings in a sample of Mexican-American adults (Ashida, Wilkinson, & Koehly, 2010). Consistent with these findings, individuals in the present study who reported receiving greater support resources for disease management reported better adherence to self-management behaviors, and in turn, exhibited lower HbA1c levels. As such, support resources represent an important potential target for interventions aiming to improve diabetes self-management, and thus, glycemic control among Latinos with type 2 diabetes. In fact, Barrera et al. (2006) evaluated an intervention that directly targeted social-environmental support resources for disease management as a mechanism to improve health behaviors and outcomes, and found that increases in support mediated positive intervention effects on fat consumption, exercise, and glycemic control at a 6-month follow-up. In addition to representing a target for change, support resources for disease management may also represent a mechanism that, once mobilized, helps to sustain the effects of an intervention long after treatment has ended. In a follow-up to their initial investigation, Barrera and colleagues (2008) reported that changes in support resources during year one influenced changes in some outcomes for up to two years post-baseline.
Depression
In addition to being more common among individuals with type 2 diabetes, depression has also been associated with poor glycemic control (Lustman, et al., 2000), increased diabetic symptoms, more frequent complications, and poorer health outcomes (Black et al., 2003; de Groot et al., 2001; Katon et al., 2005). In a study conducted by Gross and colleagues (2005), over 30% of Latino participants with diabetes reported depressive symptoms in the moderate to severe range; these participants exhibited significantly higher HbA1c levels than participants without elevated depression. Consistent with these and other previous findings (for a review, see Lustman et al.), greater depressive symptomatology was associated with higher HbA1c levels in the present study. One potential explanation that has been put forth to explain this relationship is that depression leads to poorer diabetes self-management (Gonzalez, et al., 2008), which in turn, results in poorer glycemic control. Specifically, symptoms that characterize depression, such as low energy and motivation, may interfere with individuals’ ability to follow diabetes treatment recommendations. However, although greater depression symptomatology was associated with poorer diabetes self-management in the present study, the indirect effect of depression on HbA1c via diabetes self-management was not statistically significant. Further research is needed to investigate the mechanisms underlying the link between depression and glycemic control (Lustman et al.), which are likely to involve a complex combination of both behavioral and physiological factors. In regard to the latter, depression has consistently been associated with physiological alterations including activation of the hypothalamic-pituitary-adrenal axis, sympathetic nervous system, and proinflammatory responses, which can induce insulin resistance and contribute to poorer diabetes-related health outcomes (Golden, 2007).
Regardless of the underlying mechanism, the present findings speak to the value of early and frequent screenings for depression in individuals with diabetes. The associations of depression with diabetes self-management and poor glycemic control also highlight the importance of developing and implementing interventions in the primary care setting to intervene in the deleterious reciprocal relationship between depression and type 2 diabetes (Mezuk, Eaton, Albrecht, & Golden, 2008). Consistent with previous research (e.g., Connell et al., 1994), the present findings point to support resources as an important protective factor in the development of depression in individuals with a chronic illness. Specifically, greater support resources for disease management was associated with fewer depressive symptoms, and thus lower HbA1c levels.
Limitations
There are several caveats that should be considered in the interpretation of these findings. First, the cross-sectional design of this study precludes inferences about causation. The proposed causal sequence was a better statistical fit to the data than was the reverse sequence (i.e., from HbA1c to support resources for disease management via depression and/or diabetes self-management); however, additional (prospective) research is needed to determine whether increasing support resources for disease management consistently results in better diabetes self-management, less depression, and thus, better glycemic control over time. Second, because information about medication use was not available, analyses did not control for potential effects of medication on glycemic control or reported depressive symptoms. Third, the results should be interpreted in the context of sample characteristics (i.e., majority were female, low income, and low U.S.-acculturated as indicated by language preference). Because our sample was relatively homogeneous, we were unable to investigate gender, socioeconomic status, or acculturation as potential moderators of the direct or indirect effects in this model. Further, the fact that the majority (but not all) of the participants were of Mexican descent may limit the generalizability of the findings to other segments of the Latino population, and prevent an examination of potential ethnic or cultural differences. Additional research is needed to determine whether or not the links among support resources for disease management, diabetes self-management, depression, and ultimately, glycemic control, persist outside of the studied population.
Conclusions
Despite these limitations, the present study provides additional support for the well-established link between health and social support, extends the research base on social-environmental support and resources specifically related to managing a chronic health condition, and suggests two potential mechanisms underlying the link between support and resources for disease management and glycemic control in individuals with type 2 diabetes: diabetes self-management and depression. Importantly, these findings also point to support resources for disease management as a potential target for efforts aiming to improve diabetes self-management, reduce depression, and thus, improve glycemic control. Due to the importance of family interdependence and close social relationships in the Latino culture, especially in the context of adverse circumstances such as managing one’s diabetes, social-environmental support and resources for disease management may represent an especially important area for interventions aiming to improve the mental and physical health of this population.
Acknowledgments
This research was supported by the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases (Grant 1 R18 DK070666-01).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea
Contributor Information
Addie L. Fortmann, San Diego State University/University of California, San Diego, Joint Doctoral Program in Clinical Psychology
Linda C. Gallo, San Diego State University/University of California, San Diego, Joint Doctoral Program in Clinical Psychology
Athena Philis-Tsimikas, Scripps Whittier Diabetes Institute.
References
- American Psychological Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2002;25(1):213–229. doi: 10.2337/diacare.25.1.213. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association. Standards of medical care in diabetes - 2010. Diabetes Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anders RL, Olson T, Wiebe J, Bean NH, DiGregorio R, Guillermina M, et al. Diabetes prevalence and treatment adherence in residents living in a colonia located on the West Texas, USA/Mexico border. Nursing and Health Sciences. 2008;10:195–202. doi: 10.1111/j.1442-2018.2008.00397.x. [DOI] [PubMed] [Google Scholar]
- Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- Ashida S, Wilkinson AV, Koehly LM. Motivation for health screening: evaluation of social influence among Mexican-American adults. American Journal of Preventive Medicine. 2010;38:396–402. doi: 10.1016/j.amepre.2009.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Socical Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrera M, Toobert DJ, Angell KL, Glasgow RE, Mackinnon DP. Social support and social-ecological resources as mediators of lifestyle intervention effects for type 2 diabetes. Journal of Health Psychology. 2006;11:483–495. doi: 10.1177/1359105306063321. [DOI] [PubMed] [Google Scholar]
- Barrera M, Strycker LA, Mackinnon DP, Toobert DJ. Social-ecological resources as mediators of two-year diet and physical activity outcomes in type 2 diabetes patients. Health Psychology. 2008;27(2 Suppl):S118–125. doi: 10.1037/0278-6133.27.2(Suppl.).S118. [DOI] [PubMed] [Google Scholar]
- Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26:2822–2828. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- Borges WJ, Ostwald SK. Improving foot self-care behaviors with Pies Sanos. Western Journal of Nursing Research. 2008;30:325–341. doi: 10.1177/0193945907303104. [DOI] [PubMed] [Google Scholar]
- Boyle JP, Honeycutt AA, Narayan KM, Hoerger TJ, Geiss LS, Chen H, et al. Projection of diabetes burden through 2050: impact of changing demography and disease prevalence in the U.S. Diabetes Care. 2001;24:1936–1940. doi: 10.2337/diacare.24.11.1936. [DOI] [PubMed] [Google Scholar]
- Brody GH, Kogan SM, Murry VM, Chen YF, Brown AC. Psychological functioning, support for self-management, and glycemic control among rural African American adults with diabetes mellitus type 2. Health Psychology. 2008;27(1 Suppl):S83–90. doi: 10.1037/0278-6133.27.1.S83. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2007. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. [Google Scholar]
- Chiu YW, Chang JM, Lin LI, Chang PY, Lo WC, Wu LC, et al. Adherence to a diabetic care plan provides better glycemic control in ambulatory patients with type 2 diabetes. Kaohsiung Journal of Medical Sciences. 2009;25:184–192. doi: 10.1016/S1607-551X(09)70059-2. [DOI] [PubMed] [Google Scholar]
- Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Archives of Internal Medicine. 2000;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- Connell CM, Davis WK, Gallant MP, Sharpe PA. Impact of social support, social cognitive variables, and perceived threat on depression among adults with diabetes. Health Psychology. 1994;13:263–273. doi: 10.1037//0278-6133.13.3.263. [DOI] [PubMed] [Google Scholar]
- de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosomatic Medicine. 2001;63:619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- Eakin EG, Reeves MM, Bull SS, Riley KM, Floyd S, Glasgow RE. Validation of the Spanish-language version of the chronic illness resources survey. International Journal of Behavioral Medicine. 2007;14:76–85. doi: 10.1007/BF03004172. [DOI] [PubMed] [Google Scholar]
- Egede LE, Osborn CY. Role of motivation in the relationship between depression, self-care, and glycemic control in adults with type 2 diabetes. Diabetes Educator. 2010;36:276–283. doi: 10.1177/0145721710361389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Strycker LA, Toobert DJ, Eakin E. A social-ecologic approach to assessing support for disease self-management: the Chronic Illness Resources Survey. Journal of Behavioral Medicine. 2000;23:559–583. doi: 10.1023/a:1005507603901. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Toobert DJ, Barrera M, Strycker LA. The Chronic Illness Resources Survey: cross-validation and sensitivity to intervention. Health Education Research. 2005;20:402–409. doi: 10.1093/her/cyg140. [DOI] [PubMed] [Google Scholar]
- Gold R, Yu K, Liang LJ, Adler F, Balingit P, Luc P, et al. Synchronous provider visit and self-management education improves glycemic control in Hispanic patients with long-standing type 2 diabetes. Diabetes Educator. 2008;34:990–995. doi: 10.1177/0145721708323744. [DOI] [PubMed] [Google Scholar]
- Golden SH. A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Current Diabetes Review. 2007;3:252–259. doi: 10.2174/157339907782330021. [DOI] [PubMed] [Google Scholar]
- Gonzalez JS, Safren SA, Delahanty LM, Cagliero E, Wexler DJ, Meigs JB, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabetes Medicine. 2008;9:1102–1107. doi: 10.1111/j.1464-5491.2008.02535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross R, Olfson M, Gameroff MJ, Carasquillo O, Shea S, Feder A, et al. Depression and glycemic control in Hispanic primary care patients with diabetes. Journal of General Internal Medicine. 2005;20:460–466. doi: 10.1111/j.1525-1497.2005.30003.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care. 2001;24:454–459. doi: 10.2337/diacare.24.3.454. [DOI] [PubMed] [Google Scholar]
- Katon W, Russo J, Lin EH, Heckbert SR, Karter AJ, Williams LH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medication adherence or lack of treatment intensification? Psychosomatic Medicine. 2009;71:965–972. doi: 10.1097/PSY.0b013e3181bd8f55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. In: Gilbert D, Fiske S, Lindzey G, editors. The handbook of social psychology. 4. Vol. 1. Boston, MA: McGraw-Hill; 1998. [Google Scholar]
- King DK, Glasgow RE, Toobert DJ, Strycker LA, Estabrooks PA, Osuna D, et al. Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care. 33:751–753. doi: 10.2337/dc09-1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King DK, Glasgow RE, Toobert DJ, Strycker LA, Estabrooks PA, Osuna D, et al. Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care. 2010;33:751–753. doi: 10.2337/dc09-1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–2160. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- Lustman PJ, Anderson RJ, Freedland KE, de Groot M, Carney RM, Clouse RE. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000;23:934–942. doi: 10.2337/diacare.23.7.934. [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mainous AG, 3rd, Baker R, Koopman RJ, Saxena S, Diaz VA, Everett CJ, et al. Impact of the population at risk of diabetes on projections of diabetes burden in the United States: an epidemic on the way. Diabetologia. 2007;50(5):934–940. doi: 10.1007/s00125-006-0528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin G. Influence of acculturation on familialism and self-identification among Hispanics. In: Bernal ME, Knight GP, editors. Ethnic identity: Formation and transmission among Hispanics and other minorities. Albany, NY: SUNY Press; 1993. pp. 181–196. [Google Scholar]
- McKellar JD, Humphreys K, Piette JD. Depression increases diabetes symptoms by complicating patients’ self-care adherence. Diabetes Educator. 2004;30:485–492. doi: 10.1177/014572170403000320. [DOI] [PubMed] [Google Scholar]
- Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31:2383–2390. doi: 10.2337/dc08-0985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misra R, Lager J. Ethnic and gender differences in psychosocial factors, glycemic control, and quality of life among adult type 2 diabetic patients. Journal of Diabetes and its Complications. 2009;23:54–64. doi: 10.1016/j.jdiacomp.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Okura T, Heisler M, Langa KM. Association between cognitive function and social support with glycemic control in adults with diabetes mellitus. Journal of the American Geriatrics Society. 2009;57:1816–1824. doi: 10.1111/j.1532-5415.2009.02431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philis-Tsimikas A, Walker C, Rivard L, Talavera G, Reimann JOF, Salmon M, et al. A community-based, culturally appropriate nurse case management and peer education diabetes care model. Diabetes Care. 2004;27:110–115. doi: 10.2337/diacare.27.1.110. [DOI] [PubMed] [Google Scholar]
- Pineda Olvera AE, Stewart SM, Galindo L, Stephens J. Diabetes, depression, and metabolic control in Latinas. Cultural Diversity and Ethnic Minority Psychology. 2007;13:225–231. doi: 10.1037/1099-9809.13.3.225. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavioral Research Methods, Instruments, and Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavioral Research Methods. 2008;40:879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Richardson LK, Egede LE, Mueller M, Echols CL, Gebregziabher M. Longitudinal effects of depression on glycemic control in veterans with Type 2 diabetes. General Hospital Psychiatry. 2008;30:509–514. doi: 10.1016/j.genhosppsych.2008.07.001. [DOI] [PubMed] [Google Scholar]
- Ruggiero L, Moadsiri A, Butler P, Oros SM, Berbaum ML, Whitman S, et al. Supporting diabetes self-care in underserved populations: a randomized pilot study using medical assistant coaches. Diabetes Educator. 2010;36:127–131. doi: 10.1177/0145721709355487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez-Burks J, Nisbett RE, Ybarra O. Cultural styles, relational schemas, and prejudice against out-groups. Journal of Personality and Social Psychology. 2000;79:174–189. doi: 10.1037//0022-3514.79.2.174. [DOI] [PubMed] [Google Scholar]
- Skyler JS. Effects of glycemic control on diabetes complications and on the prevention of diabetes. Clinical Diabetes. 2004;22:162–166. [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological Methodology. San Francisco: Jossey-Bass; 1982. pp. 290–312. [Google Scholar]
- Sobel ME. Some new results on inirect effects and their standard errors in covariance structure models. In: Tuma N, editor. Sociological Methodology. Washington, DC: American Sociological Association; 1986. pp. 159–186. [Google Scholar]
- Spencer MS, Kieffer EC, Sinco BR, Palmisano G, Guzman JR, James SA, et al. Diabetes-specific emotional distress among African Americans and Hispanics with type 2 diabetes. Journal of Health Care for the Poor and Underserved. 2006;17(2 Suppl):88–105. doi: 10.1353/hpu.2006.0095. [DOI] [PubMed] [Google Scholar]
- Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. British Medical Journal. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- Uchino BN. Social support and physical health: Understanding the health consequences of relationships. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychological Bulletin. 1996;119:488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- Wulsin L, Somoza E, Heck J. The Feasibility of Using the Spanish PHQ-9 to Screen for Depression in Primary Care in Honduras. Primary Care Companion to the Journal of Clinical Psychiatry. 2002;4:191–195. doi: 10.4088/pcc.v04n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]