Abstract
Objective
To preliminarily evaluate telephone-delivered motivational enhancement therapy (MET) in motivating unadjudicated and nontreatment seeking intimate partner violence (IPV) perpetrators, who also use substances, to self-refer into treatment.
Method
124 adult men were recruited via a multimedia marketing campaign and were randomly assigned to the intervention (MET) or comparison group following a baseline assessment. Participants in the MET condition received a personalized feedback report on their IPV and substance-use behaviors, consequences, and social norms beliefs.
Results
Results supported the likely effectiveness of MET in short-term reduction of IPV behavior, increasing motivation for treatment seeking, and changing perceived norms for IPV and substance abuse (SA).
Conclusions
Applications for brief MET interventions to facilitate voluntary treatment entry among substance-using IPV perpetrators are discussed.
Keywords: IPV perpetration, substance abuse, brief interventions, randomized controlled trials, motivational enhancement therapy, check-up model, voluntary treatment referral
A Telephone Intervention for Substance-Using Adult Male Perpetrators of Intimate Partner Violence
This article presents the primary outcomes from an initial evaluation of the Men’s Domestic Abuse Check-Up (MDACU), an early intervention with substance-using male perpetrators of intimate partner violence (IPV; Mbilinyi et al., 2008; Roffman, Edleson, Neighbors, Mbilinyi, & Walker, 2008). The purpose of this research was to preliminarily evaluate telephone-delivered motivational enhancement therapy (MET) with adult male perpetrators who were concurrently using alcohol or drugs and were neither in counseling nor undergoing adjudication. The intervention’s principal objective was to engage participants early (before arrest) and facilitate motivation for them to initiate positive changes in their IPV and/or substance abuse (SA). Similar early intervention/prevention models have not yet been tested with this target population; thus, this research was designed to fill an important gap in the literature. The study and its procedures were approved by the University ofWashington’s Institutional Review Board.
IPV
Two large national surveys have estimated that over 1 million adults in the United States are physically assaulted by an intimate partner each year (The National Violence Against Women Survey, Tjaden & Thoennes, 2000; The National Crime Victimization Survey, Catalano, 2005). The majority of the women and men (over 80% each) identified their abusive partner as male (Tjaden & Thoennes, 2000). Furthermore, IPV has devastating consequences to victims, other family members, and society more broadly in terms of economic burden. IPV has been linked to adverse physical health effects in women (Campbell et al., 2002; Centers for Disease Control [CDC], 2003; Kendall-Tackett, 2004), such as physical ailments, cuts, and burns (Loue, 2001). The study by Wisner, Gilmer, Saltzman, and Zink (1999) found a significant association between IPV, chronic pain, and chemical dependency. In terms of mental health, battered women are more likely to be diagnosed with depression than non-battered women (Danielson, Moffit, Caspi, & Silva, 1998; Wisner et al., 1999). These health and mental health effects have a direct impact on costs for the victims and society at large.
According to the CDC (2003), the annual cost of IPV exceeded $8.3 billion, which included $460 million for rape, $6.2 billion for physical assault, $461 million for stalking, and $1.2 billion in the value of lost lives (Max, Rice, Finkelstein, Bardwell, & Leadbetter, 2004). These are considered an underestimate because the costs associated with the criminal justice system have not been analyzed from a large national survey. Furthermore, victims lose nearly 8 million days of paid work, the equivalent of more than 32,000 full-time jobs and almost 5.6 million days of household productivity each year. The annual cost of lost productivity due to IPV is estimated as $727.8 million (CDC, 2003).
Finally, children exposed to IPV are more likely to exhibit cognitive and behavioral problems compared to children not exposed to IPV and for some, the effects last through adulthood (Appel & Holden, 1998; Edleson, 1999; Edleson et al., 2007; Fantuzzo & Mohr, 1999; Felitti et al., 1998; Lehmann, 2000; Rossman, 2001).
Batterer Intervention Effectiveness
For the past three decades, a variety of batterer intervention programs (BIPs) have offered weekly gender-specific group therapy sessions to IPV perpetrators (Austin & Dankwort, 1999). While there is controversy regarding their effectiveness, the majority of studies have not used experimental designs. Studies that have used experimental designs have found mixed results, with some reporting no statistical difference in recidivism rates between BIP participants and perpetrators not in treatment (Dunford, 2000; Feder & Forde, 2003; Labriola, 2008), while others have found modest, yet positive effects (Palmer, Brown, & Barrera, 1992; Taylor, Davis, & Maxwell, 2001). The most comprehensive quasi-experimental study by Gondolf (2004), supported by the CDC, found promising results in terms of recidivism rates among BIP program completers compared to non-completers. Even among researchers who found positive outcomes, however, it is unclear what BIP features or curriculum components are necessary or sufficient to produce behavior change (Bennett & Williams, 2001).
More consistent findings suggest that IPV treatments are effective with program completers, those not abusing substances, and those higher in motivation (see below). Thus, even with modest effectiveness, BIPs are estimated to protect 42,000 intimate partners from violence annually (Paymar & Barnes, 2006). Finally, most of these studies include court-mandated perpetrators and may underestimate potential treatment impact on voluntary participants.
IPV and Substance Use
Research has found considerable overlap between IPV perpetration and alcohol and/or drug use, which has led to an increased focus on SA in interventions for IPV perpetrators. In the study by Thompson and Kingree (2006), women whose partners had been drinking were more likely to be injured than were women whose partners had not been drinking. Fals-Stewart (2003) found a similar relationship, where IPV-perpetrating men were between 8 and 11 times more likely to be abusive on drinking days relative to non-drinking days. Higher rates of SA have also been reported when lifetime patterns of IPV are evaluated (Bennett, 2008; Brown, Werk, Caplan, & Seraganian, 1999). One of the earliest evaluations of an integrated SA and IPV intervention indicated greater retention (79%) in comparison to a traditional BIP program (55%) after only 1 month of service (see Goldkamp, Weiland, Collins, & White, 1996). More recently, Yale’s Substance Abuse-Domestic Violence integrated model increased participants’ motivation, improved compliance with treatment, and decreased both anger and alcohol consumption (Easton & Sinha, 2002). Overall, SA treatment has been found relatively effective in reducing or eliminating substance use (Carroll, 1998; Miller & Wilbourne, 2002), which is in turn associated with reducing IPV behavior (Easton, Mandel, Babuscio, Rounsaville, & Carroll, 2007; O’Farrell, Fals-Stewart, Murphy, & Murphy, 2003; O’Farrell& Murphy, 1995).Correcting misperceptions of norms for problematic behaviors has also been found to lead to behavior change.
Perceived Norms
Although domestic violence laws and policies have existed for decades, IPV continues to be highly prevalent and often not reported to law enforcement (Taylor & Sorenson, 2005). Perpetrators also tend to justify their IPV based on misperceptions of others’ behaviors, and many are unaware that their own behavior is “outside the norm.” Intervention research in substance use, risky sexual behaviors, and gambling among college student populations has revealed three consistent and important findings with respect to perceived social norms. First, the perceived prevalence of negative health and risk behaviors is strongly associated with one’s own behavior (e.g., Borsari & Carey, 2001). Second, individuals tend to overestimate the prevalence of negative health and risk behaviors and this is particularly true for those who engage in the behaviors (e.g., Baer, Stacy, & Larimer, 1991). Third, providing accurate prevalence information, especially in the context of personalized feedback, has been found effective in changing normative misperceptions and subsequent behavior (for reviews see Carey, Scott-Sheldon, Carey, & DeMartini, 2007; Lewis, & Neighbors, 2006; Walters & Neighbors, 2005). Similar findings have been reported for gambling, marijuana use, risky sex, and other negative health and risk-related behaviors (e.g., Chia & Gunther, 2006; Kilmer et al., 2006; Larimer & Neighbors, 2003; Lewis & Neighbors, 2004). Recently, in an analysis of baseline estimates from the current sample, we determined that IPV perpetrators overestimated IPV norms, and their estimates were associated with higher levels of violence toward their partners (Neighbors et al., 2010). No research to date has determined whether receiving feedback regarding accurate norms might be successful in correcting normative misperceptions in this population.
Treatment Seeking, Entry, and Retention Among IPV Perpetrators
The majority of men enter IPV treatment only after serious injury to a partner and usually following an arrest and being mandated to enroll in treatment (Gondolf, 2002). Although program completers are more likely to be nonviolent than are non-completers, many perpetrators in treatment drop out (Daly & Pelowski, 2000). Participant motivation and SA have been found to be significant predictors of treatment dropout among IPV perpetrators. Gondolf’s (2004) four-city study consisting of 840 IPV perpetrators mandated to treatment found a 50% greater overall reduction in recidivism among program completers. Additional studies have supported and extended this finding. For example, Jones and colleagues found that program completion reduced the probability of re-assault by 46% among court ordered men at 15-month follow-up (Jones, D’Agostino, Gondolf, & Heckert, 2004). Similarly, when examining completers versus non-completers of BIPs, Bennett and colleagues found completion to reduce the likelihood of rearrest by 62% over a 2.4-year period (Bennett, Stoops, Call, & Flett, 2007).
Far less is known about treatment efficacy and retention with individuals who have voluntarily entered IPV/SA treatment. MET has shown promise in promoting treatment entry, active engagement, retention, and successful behavioral outcomes.
MET, usually offered in 1–3 sessions, consists of assessment followed by personalized feedback facilitated by motivational interviewing (MI). In a number of controlled trials, MET interventions with substance abusing populations have shown promise in (a) reducing substance use (Baker, Perilla, & Norris, 2001; Stotts, Schmitz, Rhoades, & Grabowski, 2001); (b) increasing treatment attendance (Davis, Baer, Saxon, & Kivlahan, 2003; Swanson, Pantalon, & Cohen, 1999); (c) increasing active participation in the treatment process (Carey, Purnine, Maisto, & Carey, 2002; Martino, Carroll, O’Malley, & Rounsaville, 2000); and (d) reducing attrition (Lincourt, Kuettel, & Bombardier, 2002; Martino et al., 2000). Not all of the findings of MET trials with substance abusers have been positive. Some have found no effect on treatment entry (Booth, Kwiatkowski, Iguchi, Pinto, & John, 1998; Donovan, Rosengren, Downey, Cox, & Sloan, 2001; Schneider, Casey, & Kohn, 2000), retention (Donovan et al., 2001), or outcomes (Donovan et al., 2001; Miller, Yahne, & Tonigan, 2003). These mixed findings offer considerable support for continuing research focusing on MET interventions with nontreatment seekers for the purpose of motivating behavior change, including treatment entry, engagement, and retention.
Although new to IPV intervention research, clinical literature has found MET and MI to show promise for improving outcomes with IPV perpetrators (Maiuro &Murphy, 2009; Mbilinyi et al., 2009; Murphy & Eckhardt, 2005). IPV perpetrators share many characteristics with individuals who have addictive disorders, including externalizing and blaming others for their abuse and minimizing the impact of their behavior (see Roffman et al., 2008). Furthermore, MET strategies to reduce or “roll with” resistance seem relevant to IPV perpetrators whose abuse is embedded in power and control. IPV clinical literature also points to periods of perpetrators’ ambivalence that appears applicable with MI principles. Finally, preliminary IPV research has found MET’s potential for facilitating perpetrators’ motivation to change, either by decreasing their externalizing behaviors (i.e., blaming others for their abuse; Kistenmacher & Weiss, 2008); help-seeking outside their domestic violence program (Musser, Semiatin, Taft,& Murphy, 2008); and/or reducing their physical abuse (Musser et al., 2008).
The Current Study
The current study provides an evaluation of the primary outcomes for the MDACU, a preliminary randomized trial evaluating telephone-delivered MET with adult men engaging in IPV and using alcohol or drugs, who are neither in counseling nor undergoing adjudication. We expected individuals receiving MET to show greater evidence of interest and willingness to change relative to those in the comparison condition. Specifically, we hypothesized that those receiving the intervention would be more likely to attend the optional in-person learning session (OLS) to learn about treatment resources (the main outcome variable; Hypothesis 1). In addition, we hypothesized that IPV frequency and substance use would show evidence of positive change among MET intervention participants relative to participants in the comparison condition (Hypothesis 2). We further hypothesized that the MET intervention would be associated with increased treatment-seeking behaviors (Hypothesis 3). Finally, we expected that the MET intervention would be effective in correcting inaccurate perceived norms for IPV and SA (Hypothesis 4).
Method
Screening/Recruitment
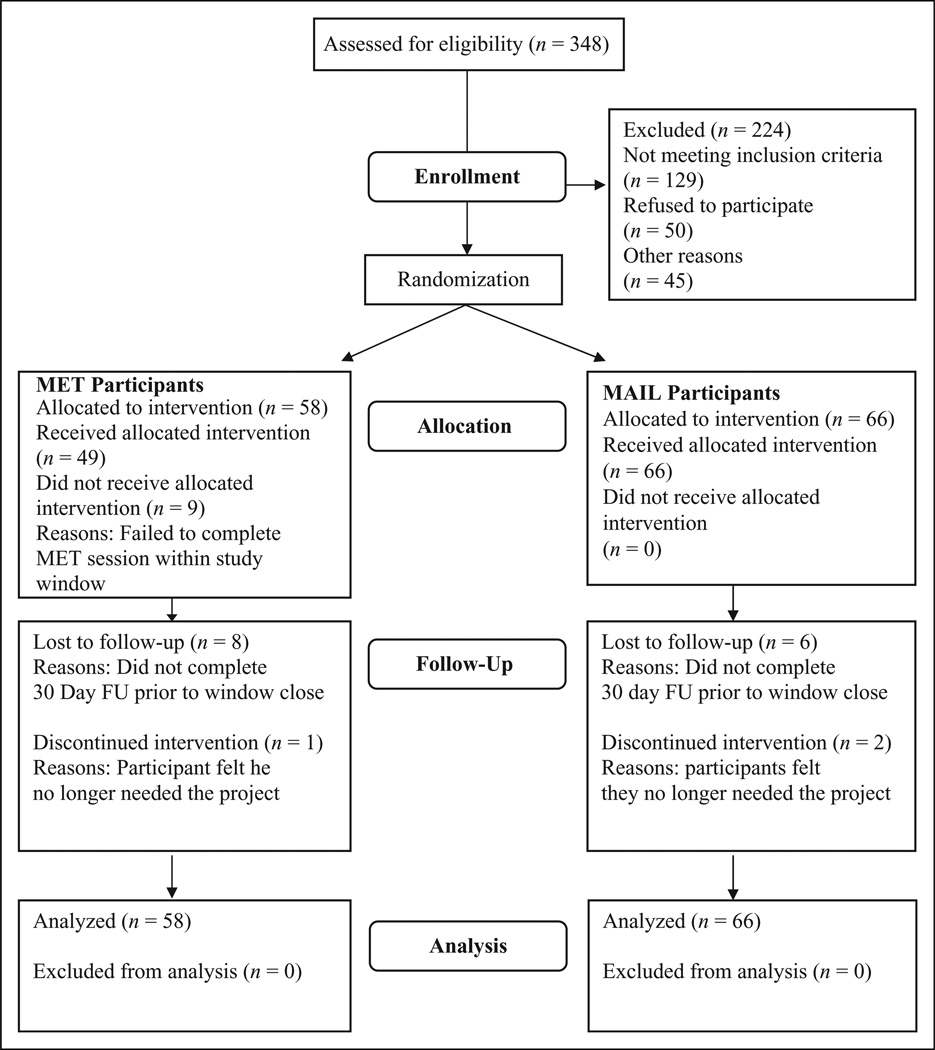
Participant flow through the study is presented in Figure 1. MDACU received 348 calls over a 64-week period, from July 2006 to October 2007, from men solicited through various forms of marketing within the community including radio, print, and multimedia advertisement. Marketing focused on capturing the attention of men concerned about their behaviors and touted MDACU’s free, nonjudgmental, brief, and anonymous services. In advertisements, images of diverse individuals and relationship type (family, partner, and same-sex relationship) were linked with hypothetical statements that reflect the thinking and experiences of men who are abusive and concerned about their behaviors. All ads included a privacy statement, the project’s logo, the toll-free phone number, and a message encouraging men to call and speak to “someone who understands” (for details see Mbilinyi et al., 2008).
Figure 1.
Participant flow.
Eligibility criteria included male in a heterosexual or same-sex relationship, 18 years or older, recent IPV behavior (measured by the revised Conflict Tactics Scale; CTS2), recent substance use (measured by the Psychoactive Substance Use Disorder [SUD] section of the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders [Fourth Edition; DSM-IV]; SCID), no recent treatment attendance for IPV or SA, no recent arrest or involvement with the courts for IPV or SA, and no imminent danger to partner (note: recent was defined as the past 90 days).
The screening process was split into two brief phone calls. During the first call, the men were introduced to the project, asked some basic demographic questions, and given an opportunity to talk about concerns that led them to call. Men who were eligible at the completion of this call were scheduled to complete a second screening call. The second screening call assessed the men’s substance use, domestic violence behaviors, and further informed the men about the study. Men who met eligibility criteria at the end of this call were asked whether they wished to enroll in the project and were then verbally consented and scheduled for their baseline assessment within the next week (additional details regarding screening procedures and research protocols can be found in Roffman et al., 2008).
Of the 348 calls, 134 men met eligibility criteria and expressed intent to enroll in the project. Of the 134 eligible men, 124 completed the baseline assessment and were enrolled and randomized. Of the 224 individuals who were excluded, 129 did not meet eligibility criteria, 50 refused participation, and 45 were excluded for other reasons such as not completing their baseline assessment. The target sample of 124 participants was chosen based on power analyses reflecting the ability to detect medium effect sizes.
Demographics
The men were primarily non-Hispanic (94%) and heterosexual (95%). Of the 124 participants, 65% were White/Caucasian and 35% Men of Color. The 124 men ranged in age from 18 to 67 (see Table 1 for demographic details). Eighty percent worked full-time (at least 30 hr a week) and 64% had a household income of $40,001 or more. Seventy-four percent reported having children (mean = 2.4) and 59% reported having children currently living in their home. Nine percent reported ever having received IPV services and 22% reported receiving substance use services in the past. A majority (57%) reported primarily growing up in a two-parent household, with 48% reporting excessive substance use by at least one adult in their household. Seventy-six percent reported seeing abusive behaviors by adults in their household at least once per year.
Table 1.
Demographics
| Variable |
N = 124 Participants |
|---|---|
| Race | |
| White/Caucasian | 65% |
| Black/African American | 17% |
| Asian | 2% |
| American Indian/Alaska Native | 4% |
| Native Hawaiian/Other Pacific Islander | 3% |
| Multiracial | 2% |
| Other | 7% |
| Ethnicity | |
| Non-Hispanic | 94% |
| Hispanic | 6% |
| Sexual preference | |
| Heterosexual | 95% |
| Other | 5% |
| Mean age | 39.4 years |
| Education | |
| At least some college | 77% |
| High school/general equivalency diploma (GED) or less | 23% |
Procedures
Baseline assessments were scheduled within 1 week of completion of the two-step screening process. At the completion of the baseline assessment, participants were randomized into one of two treatment conditions—the experimental condition (MET) or comparison condition (Mail; see below). A computerized Urn randomization procedure was utilized (Stout, Wirtz, Carbonari, & Del Boca, 1994). Four variables were used for blocking: severity of violence, severity of substance use, race/ethnicity (White vs. non-White), and whether the participant met diagnostic criteria for a SUD.
Men who were randomized to MET were scheduled immediately for a phone Feedback Session with a project Counselor. The Feedback Session consisted of one 60- to 90-min telephone conversation within 1 to 3 weeks of the baseline assessment. Counselors created a Personal Feedback Report (PFR) immediately following the baseline assessment and sent it by mail to MET participants. The participant was asked not to open the PFR prior to the phone session. The PFR provided information that was personally tailored based on the participant’s responses during assessments, including history of perpetrator’s abusive behavior, IPV normative data, consequences to the perpetrator of his IPV, family history of IPV, children’s exposure to IPV, current alcohol use patterns, alcohol normative data, estimated blood alcohol concentrations, risk factors for developing an alcohol problem, alcohol consequences, current drug use patterns, drug normative data, and consequences related to drug use. The PFR was printed in booklet format with graphics and accompanying descriptions of risk factors for perpetrating IPV and for developing problems with alcohol or drugs. Participants who were randomized to the Mail condition received educational materials via mail that discussed health, psychological, legal, and social consequences of substance use and domestic violence but provided no personalized information.
Included in the mailings for both conditions was an invitation to attend an OLS: “Learning About and Considering Options in the Community.” Attendance at the OLS served as an outcome measure indicating motivation for treatment seeking/entry. This optional session was described as a private, in-person meeting with a counselor to learn about IPV, and/or SA treatment resources available in the community. The OLS was delivered in a case management and didactic style. Counselors did not use MI techniques in this session to avoid exposing the Mail participants to a MET experience. The 20- to 45-min OLS session was focused on providing detailed information about treatment resources such as length, format, fees/cost, and location. The participant also viewed a 10-min video of interviews with men who had completed IPV treatment programs.
Counselor Training and Supervision
Two master’s level and three bachelor’s level counselors conducted the interventions. Training and supervision were conducted by the clinical co-directors (D.D.W. and J.Z.). The counselor training process included a 2-day training on MET, 1-day training on IPV, 2 pilot cases with individualized supervision, and reading the treatment manual, Miller and Rollnick’s Motivational Interviewing (2002) book, and selected readings on IPV. MET training included didactic presentation of MI principles and techniques and experiential exercises.
The counselors attended individual supervision with both supervisors weekly to discuss and plan for pilot cases. All sessions (both pilot and trial) were digitally recorded. Session recordings were listened to by both supervisors. Using an adapted version of the Motivational Interviewing Treatment Integrity coding system, MITI (Moyers, Martin, Manuel, & Miller, 2003), tapes were specifically coded for behavior counts of reflections (parsed by repeat, rephrase, paraphrase, and summary), open and closed-ended questions, and affirmations. Counselors were provided general and personalized feedback based on the coding results of the sessions. When the counselors demonstrated acceptable behavior counts on the sessions and a mastery of implementing the sessions in accordance with the manual, they were approved to work with enrolled study participants. Each counselor’s first two to three sessions were supervised carefully by each supervisor. Counselors attended group supervision sessions weekly for 1.5 hours. One or two session tapes were chosen at random and listened to by supervisors each week. Sessions were discussed and feedback was given to maintain treatment adherence, high level of competence, and to avoid therapist drift. Of the 49 MET sessions completed by MET participants, recordings of 45 (92%) were listened to by at least one supervisor.
Follow-Up Assessments
Two telephone follow-up assessments were completed, one at 1-week and another at 30-days post-intervention (each follow-up assessment battery was adjusted for its respective timeframe, with no overlap of time). At the 1-week assessment, each participant was invited verbally to attend the OLS. Participants had until they completed their 30-day assessment to participate in the optional session. Eighty-four percent of men completed their 1-week follow-up, and 80% of participants completed their 30-day follow-up (see measures below for a description of instruments implemented during the baseline and follow-up assessments).
Measures
IPV
The revised Conflict Tactics Scale, CTS2 (Straus, Hamby, Boney-McCoy, & Sugarman, 1996) is a widely used measure in IPV research. Results using various forms of the CTS have been reported in studies involving over 70,000 participants. Its use in two national surveys (Straus & Gelles, 1990; Tjaden & Thoennes, 2000) provided comparison data against which to assess participants in this research project. The scale has five subscales: (a) Negotiation; (b) Psychological aggression; (c) Physical assault; (d) Sexual coercion; and (e) Injury. For the purposes of the current study, the scale was modified to assess the frequency of violent behaviors perpetrated over the previous 90 days at baseline and 30 days at the 30-day follow-up assessment. A CTS summary score was created as the mean of all CTS items where frequency counts were capped at 90 for each item. Reliability (α) of the CTS summary score was .74 at baseline and .72 at 30-day follow-up. We also specifically created a variable combining physical assault and injurious behavior items (physical/injurious behavior) due to the relative low frequency of these behaviors over the past 90 days at baseline and the past 30 days at the 30-day follow-up. Psychological abuse was assessed with eight items (e.g., insulted or swore at partner; destroyed something that belonged to partner). Scores represent the sum of the 8 items with each item capped at 90. Reliability of the psychological abuse variables was .82 at baseline and .86 at 30-day follow-up. Physical violence/injurious behavior was assessed with 18 items (e.g., slammed partner against wall and broke partner’s bone). Because frequency counts were relatively low for these behaviors, we scored this measure as a sum of dichotomously coded items indicating whether or not they had engaged in each of the 18 behaviors. Reliability for physical violence/injurious behavior was .84 at baseline and .82 at 30-day follow-up. The low frequency of sexual assault over the brief time periods assessed prevented the creation of a meaningful subscale for this behavior.
Substance use
Psychoactive Substance Use Disorder section of the Structured Clinical Interview for DSM-IV (SCID). The SCID was developed to improve interrater diagnostic reliability and kappas for SA and dependence disorders have typically ranged from .75 to .84. It was used in this research to characterize the sample in terms of current diagnoses of SUD for various classes of drugs, including poly-drug dependence.
The Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985; Kivlahan, Marlatt, Fromme, Coppel, & Williams, 1990) asks the average number of standard drinks consumed and the time period of consumption for each day of the week over the previous month. Scores represent the sum for each of the 7 days. Alphas were .84 and .91 at baseline and follow-up, respectively. It also assesses for peak alcohol consumption by asking the most drinks consumed and time period of consumption. Participants completed the DDQ at baseline and the 30-day follow-up assessment.
Other drug use was assessed using a modified version of the Form 90. This detailed structured interview uses a timeline follow-back (TLFB) procedure (Sobell, Maisto, Sobell, & Cooper, 1979) to elicit detailed daily information on the use of alcohol and other drugs. Adequate reliability of the timeline method has been demonstrated (see Sobell & Sobell, 1992) and recent data with other drug-abusing populations show strong test–retest reliability, convergent validity with other drug use measures, and agreement with both collateral informant and urinalysis data (Fals-Stewart, O’Farrell, Freitas, McFarlin, & Rutigliano, 2000). At baseline, participants were asked about their drug use during the past 30 days. At 30-day follow-up, participants were asked about drug use since their date of treatment (MET date or 1 week post-baseline for Mail participants), which ranged from 30 to 40 days depending on participants’ availability. Scores represent the number of days on which participants reported using any drug other than alcohol.
Treatment seeking
The treatment seeking and preparation questionnaire was created to assess participants’ steps toward seeking IPV and/or SA treatment. Items included contacting an agency, requesting information, and attending an intake or treatment session. Participants were also asked whether they had discontinued any treatment during the specified timeframe. Behaviors were assessed separately for IPV and SA treatment. The treatment-seeking assessment was part of the baseline, 1-week, and 30-day follow-up. Treatment seeking was scored dichotomously as the presence or absence of any treatment-seeking behaviors during the past 90 days at baseline, the past week at the 1-week follow-up, and the past 30 days at the 30-day follow-up assessment.
Perceived norms IPV
Participants were asked at the baseline, 1-week, and 30-day assessments to estimate the percentage of men who engaged in seven abusive behaviors. The seven behaviors were selected from the CTS2 and used in the National Violence Against Women Survey (NVAWS). Scores represent the average estimated for each of the seven behaviors. Alphas were .91, .92, and .94 at baseline, 1-week, and 30-day follow-up, respectively. Behaviors ranged in severity from throwing something at a partner that could hurt to threatening their partner with a gun (for additional details about the use of norms in this research, see Neighbors et al., 2010).
Perceived norms alcohol
Participants’ perceptions of substance use among typical men were assessed with the Drinking Norms Rating Form (DNRF; Baer, et al., 1991; Dimeff, Baer, Kivlahan, & Marlatt, 1999). The DNRF mirrors the DDQ. Participants were asked at baseline, 1 week, and 30 days to estimate the number of drinks per day of the week. Scores represent the average estimated number of drinks on each day of the week. Alphas were .86, .88, and .90 at baseline, 1-week, and 30-day follow-up, respectively. Perceived norms were also assessed for other substances for men who reported using other substances but low base rates prevented us from performing meaningful analyses for perceived norms for other substances.
Results
Analyses
Data were analyzed with a series of generalized linear models, which extend general linear models to include outcomes with nonnormal distributions including binary and Poisson. Models evaluated outcomes, with appropriate distributional specifications, as a function of group assignment. With the exception of the evaluation of OLS attendance, baseline outcome scores were entered as covariates in all analyses. Given the preliminary nature of the study and our expectations that the MET intervention would result in positive outcomes, alpha was set at .05 (one-tailed)/.10 (two-tailed).
Hypothesis 1 examined OLS attendance as a function of treatment condition where OLS was specified as a binary outcome. Hypothesis 2 was evaluated by comparing outcome differences (IPV frequency and substance use) between individuals receiving brief MET and individuals in the comparison group where baseline values of the dependent variables were included as covariates. Baseline outcomes were included as covariates rather than using a repeated measures approach for these outcomes because the time frame assessed for these measures at baseline (past 3 months) differed from the time frame assessed at follow-up (past month). Poisson distributions were specified for all IPV and substance use outcomes. Hypothesis 3 evaluated changes in the proportion of individuals who reported treatment-seeking behavior as a function of treatment condition. In evaluating this hypothesis, we used a repeated measures approach for evaluating within-group changes in proportions (Wilcoxin z). Between-group differences in the proportion of participants seeking treatment were examined at each time point with chi-square tests. These tests were followed by the primary evaluation of the hypothesis using generalized linear models following the same approach used to evaluate Hypothesis 2 with the exception that the distributional specification was binary. Finally, Hypothesis 4 evaluated changes in perceived norms (IPV frequency and substance use) as a function of treatment group. Because measures of perceived norms were directly comparable at baseline and follow-up and because they were relatively normally distributed, we used traditional repeated measures analyses of variance (ANOVAs) to evaluate this hypothesis.
Effect sizes as well as tests of significance are presented for each hypothesis. For ease of interpretation, the effect size r was used in each case. Formulas for converting tests to this common measure of effect size were taken from Rosenthal, Rosnow, and Rubin (2000). Small, medium, and large effects for r are .10, .30, and .50, respectively (Cohen, 1992).
OLS Attendance
Among control participants, 18 of the 66 (27.27%) attended the OLS. In comparison, 24 of the 58 (41.38%) MET participants attended the OLS. This difference approached significance, χ2(N = 124, df = 1) = 2.71, p < .10. This corresponds to a relatively small effect size (r = √[χ2/N]) of .15 in the expected direction.
IPV
Intervention effects on IPV were evaluated at the overall level (CTS summary score) and by type of violence (psychological and physical + injury). Sexual assault was not examined specifically because of insufficient variance at follow-up. Five men reported any incidence of sexual assault at follow-up, all of whom were in the control group. Results, of generalized linear models with Poisson distributions evaluating follow-up outcomes controlling for baseline outcomes, are summarized in Table 2. Findings revealed that men in the intervention group reported engaging in IPV less frequently at 30-day follow-up in comparison to men in the Mail condition. Effect sizes (r) for CTS summary, psychological, and physical + injury were .27, .26, and .21, respectively.
Table 2.
Poisson Regression Results for Intervention Effects on Intimate Partner Violence (IPV) and Substance Use at 30-Day Follow-Up
| Criterion at Follow-Up | Predictor | B | SE B | χ2 | r |
|---|---|---|---|---|---|
| CTS summary | Baseline CTS | 0.006 | .002 | 9.39** | .32 |
| Intervention | −0.949 | .358 | 7.02** | .27 | |
| Psychological abuse | Baseline Psychological abuse | 0.008 | .002 | 14.82*** | .39 |
| Intervention | −1.001 | .399 | 6.31** | .26 | |
| Physical + injurious violence | Baseline Physical + injurious violence | 0.010 | .018 | 0.34 | .06 |
| Intervention | −1.362 | .664 | 4.21* | .21 | |
| Drinks per week | Baseline drinks per week | 0.039 | .006 | 38.26*** | .62 |
| Intervention | 0.028 | .273 | 0.01 | .01 | |
| Drug use (past 30 days) | Baseline drug use (past 90 days) | 0.057 | .009 | 42.59*** | .65 |
| Intervention | −0.046 | .126 | 0.13 | .04 |
Note. CTS = Conflict Tactics Scale.
p < .001.
p < .02.
p < .05.
Substance Use
At screening, 43% of the 124 participants met diagnostic criteria for a SUD within the past 90 days. Intervention effects on substance use were evaluated separately for alcohol and other substances. For alcohol use, the average number of drinks per week in the past 30 days at follow-up was lower than the average number of drinks per week in the past 90 days at baseline as indicated by results of a paired samples t test, t (98) = −2.30, p < .05, r = .23. Caution is recommended in interpreting this finding, given that alcohol use was considerably skewed. Drug use was assessed as total number of days used in the past 30 days at baseline and at 30-day follow-up as days used since the intervention (MET participants) or 1 week after the baseline assessment (Mail participants), thus a direct comparison was not appropriate as it could range from 30–40 days at follow-up. Raw means are presented by intervention group in Table 3. Results of generalized linear models with Poisson distributions evaluating follow-up outcomes controlling for baseline outcomes are summarized in Table 2. Findings indicated that follow-up substance use was strongly associated with baseline substance use and had no relationship with intervention condition.
Table 3.
Means and Standard Deviations for Baseline and Follow-Up Variables by Intervention Condition
| Control Condition | Intervention Condition | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Assessment Point | N | M | SD | N | M | SD |
| Intimate partner violence | |||||||
| CTS summary | Baseline | 66 | 59.98 | 90.87 | 58 | 68.30 | 107.01 |
| CTS summary | 30-day Follow-up | 53 | 18.85 | 51.08 | 42 | 6.50 | 8.48 |
| Psychological violence | Baseline | 66 | 49.72 | 78.39 | 58 | 58.34 | 91.62 |
| Psychological violence | 30-day Follow-up | 53 | 17.83 | 50.62 | 42 | 6.29 | 8.29 |
| Physical and injurious violence | Baseline | 66 | 5.36 | 3.80 | 58 | 4.83 | 3.27 |
| Physical and injurious violence | 30-day Follow-up | 53 | .54 | 1.61 | 42 | 0.17 | 0.58 |
| Substance use | |||||||
| Drinks per week | Baseline | 65 | 7.61 | 12.15 | 58 | 12.69 | 14.55 |
| Drinks per week | 30-day Follow-up | 55 | 6.11 | 10.61 | 45 | 7.66 | 9.58 |
| Days used drugs | Baseline | 66 | 11.73 | 11.50 | 58 | 12.69 | 14.55 |
| Days used drugs | 30-day Follow-up | 55 | 14.56 | 15.91 | 45 | 19.13 | 14.44 |
Note. CTS = Conflict Tactics Scale.
Treatment Seeking
Overall, a modest proportion of participants reported treatment seeking during the trial. The proportion of participants who reported any treatment-seeking behavior with respect to IPV was 15.3%, 22.1%, and 27.3% at baseline, 1-week, and 30-days, respectively. Across conditions, the proportion of participants engaging in treatment-seeking behaviors for IPV increased from baseline to 1-week follow-up (Wilcoxin z = −2.07, p < .05) and from baseline to 30-day follow-up (Wilcoxin z = −2.60, p < .01) but not from 1-week to 30-day follow-up (Wilcoxin z = −1.35, p = ns). The proportion of participants reporting any treatment-seeking behavior for substance use was 7.3%, 7.8%, and 9.2% at baseline, 1-week, and 30-days, respectively. Overall, there were no significant changes in the proportion of participants engaging in treatment-seeking behaviors for substance use across conditions.
Evaluation of treatment seeking by intervention condition using chi-square tests revealed no significant differences for IPV at baseline, 1-week, or 30-day follow-up. Similarly, for substance use there were no differences by intervention condition in treatment seeking at baseline or 30-day follow-up. There was, however, a significant unexpected difference at 1-week follow-up with seven participants reporting treatment seeking in the Mail condition versus only one participant reporting treatment seeking in the MET condition, χ2(df = 1, N = 103 = 4.05, p < .05). A series of generalized linear models with binary distributional specification (i.e., logistic regression analyses) examining group differences in treatment seeking at both follow-up points, controlling for baseline behavior and treatment seeking at baseline, were consistent with the chi-square tests. For IPV, there were no differences at 1-week or 30-day follow-up. For substance use, more Mail participants reported treatment seeking at 1-week follow-up assessment, but there were no differences at 30-day follow-up.
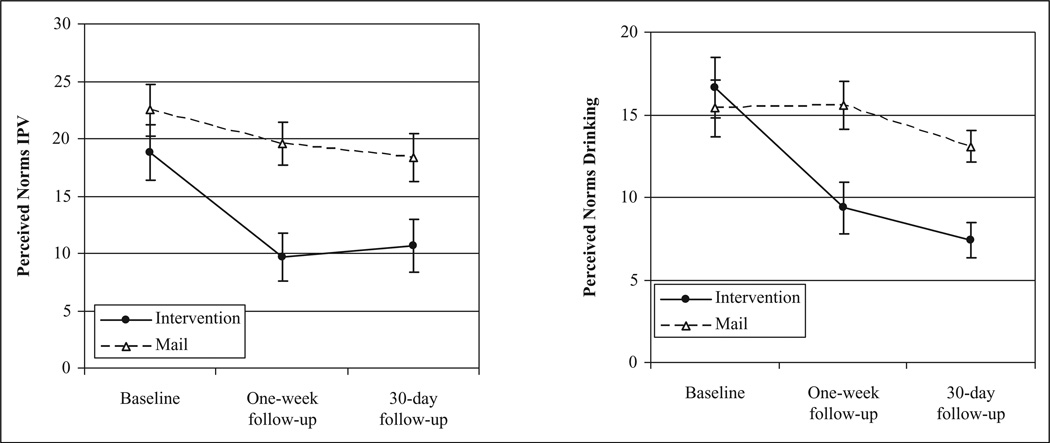
Perceived Norms for IPV
Results indicated that IPV-perpetrating men overestimated the prevalence of seven specific violent behaviors and that their perceptions/misperceptions were associated with their behavior. Moreover, the more they overestimated, the more they themselves reported engaging in psychological abuse and physical violence including injurious behavior (see Neighbors et al., 2010, for more information on norms and IPV behavior). A repeated measures ANOVA was conducted to evaluate changes in perceived norms for IPV as a function of intervention condition. Results revealed that across all participants, perceptions of the frequency with which men engage in IPV reduced over time, F(2, 182) = 19.52, p < .001, r = .31. A time by group interaction revealed that reductions in perceived norms for IPV were larger in the MET group relative to the Mail group, F(2, 182) = 3.92, p < .05, r = .15. There was also a significant between-subjects effect for group, indicating that across all time points, perceived norms were lower among MET participants relative to Mail participants, F(1, 91) = 6.58, p = .01, r = .26. Figure 2 (left) presents means and standard errors for perceived IPV norms over time as a function of intervention condition.
Figure 2.
Perceived norms for IPV and drinking as function of intervention group.
Perceived Norms for Drinking
We also performed a repeated measures ANOVA to examine changes in perceived drinking norms, operationalized as perceived number of drinks consumed per week, as a function of intervention condition. Results revealed that across all participants, perceived drinking norms reduced over time, F(2, 174) = 20.31, p < .001, r = .32. The time by group interaction was significant and revealed that reductions in perceived drinking norms were larger in the MET group relative to the Mail group, F(2, 174) = 10.30, p < .01, r = .24. The between-subjects effect for group was also significant, indicating that across all time points, perceived drinking norms were lower among MET participants, F(1, 87) = 3.93, p = .05, r = .21. Figure 2 (right) presents means and standard errors for perceived norms over time as a function of intervention condition. We were again unfortunately unable to effectively evaluate changes in perceived norms for other substance use (drug of choice) because of the relatively small proportion of participants reporting abuse of other substances.
Discussion and Applications to Social Work
Reaching and motivating IPV perpetrators to self-refer into treatment is urgent due to continued high rates of violence in intimate relationships, low treatment self-referral rates among perpetrators, and high drop-out rates in the small percentage of perpetrators who are in treatment. The Check-Up model and MET have been successful with other populations (such as substance abusers) in reaching and motivating treatment engagement, retention, and successful program completion in addition to behavior change (Baker et al., 2001; Carey, et al., 2002; Davis et al., 2003; Walker, Roffman, Stephens, Kim & Berghuis, 2006). The Check-Up model, however, had not been tested previously with substance-abusing IPV perpetrators. While MI has been integrated in some work with victims and perpetrators (Daniels & Murphy, 1997; Maiuro & Murphy, 2009; Murphy & Baxter, 1997; Murphy & Eckhardt, 2005; Ogle & Baer, 2003), IPV intervention research to date has typically focused on convenience samples of court-mandated IPV perpetrators in treatment. There has not been a randomized controlled trial evaluating the effectiveness of MET in motivating unadjudicated and nontreatment seeking IPV perpetrators to self-refer into treatment. The current study, the MDACU, filled this gap by adapting the Check-Up model incorporating MET to engage and motivate substance using male perpetrators to self-refer into treatment, in a randomized controlled trial.
Overall, the MDACU attracted a demographically diverse community sample, the majority of whom had been exposed to IPV in their families of origin. All reported engaging in psychological violence and at least minimal physical violence directed at the partner and half reported engaging in one or more instances of severe physical violence such as kicking. The MDACU’s ability to reach and enroll this population in the trial is an important finding in itself, given that a very small percentage of perpetrators self-refer into treatment (Gondolf, 2002) and at baseline, most of the participants in the trial (88%) were not taking steps toward IPV or SA treatment.
Developing successful strategies to reach IPV perpetrators early has important implications for social workers. Within existing BIPs, our findings have the potential to facilitate self-referral and early engagement in treatment among unadjudicated perpetrators. Incorporating MI as part of an already existing intake provides BIP social workers the opportunity to (a) engage with the client which may facilitate treatment retention and (b) understand perpetrators’ motivation vis-à-vis treatment, the impact of SA on perpetrators’ treatment seeking, and perpetrators’ perceptions of IPV prevalence.
Social workers in mental health, SA, and similar agencies can use our findings to develop self-referral and early intervention strategies to reach their clientele early. Finally, social workers focusing on prevention, public health, or social change efforts can use similar marketing strategies to reach out to underserved populations.
Although we did not include alcohol or drug use in our marketing messages or images (see Mbilinyi et al., 2008), a substantial percentage (43%) of men enrolled in the trial had a concurrent SUD. The overlap between IPV and SA has been documented by others (see Easton et al., 2007; O’Farrell et al., 2003) and this finding confirms the importance of addressing both behavioral problems simultaneously. Addressing SA when intervening early with IPV perpetrators has practice implications for social workers whose clientele are increasingly impacted by multiple disorders, which can interfere with treatment completion.
Two key outcomes from the trial indicate that the MDACU shows promise in interrupting violence in the home earlier: a trend toward greater motivation for treatment seeking and a greater reduction in self-reported IPV. As hypothesized, participants receiving the MET showed greater interest and willingness to change and to attend the OLS. Although the effect size corresponding to the treatment effect on OLS attendance was small, it may be related to the short window (average 3 weeks) in which to attend the OLS. It may also be due to the fact that in the MET sessions, conversation about readiness for treatment and treatment entry were avoided. As participation in the OLS session was included as a key outcome (indicating motivation for treatment seeking/entry), the OLS session was the vehicle for delivering treatment resource information. Future studies should evaluate the unique contributions of discussing treatment seeking/entry in the MET session toward treatment seeking.
The impact of the intervention on IPV behaviors is also encouraging. MET participants showed a greater reduction in self-reported IPV compared to participants in the comparison condition. Although direct comparisons are difficult because this is a unique intervention for nonadjudicated IPV perpetrators, it is consistent with previous findings evaluating brief MET interventions for substance abusers (Miller & Wilbourne, 2002). Given the nature of the study sample and brevity of the intervention, these findings provide potential for IPV behavior change in the short term.
Intervention effects on substance use were evaluated separately for alcohol and other substances. Results indicated that follow-up substance use was strongly associated with baseline substance use and had no relationship with intervention condition. Caution is urged in interpreting these findings, since (a) alcohol use was considerably skewed; (b) at baseline, drug use was assessed as total number of days used in past 30 days, whereas follow-up was days used since the intervention (30–40 days), making a direct comparison not appropriate; and (c) although 43% of participants met substance use disorder diagnostic criteria without mention of SA in the marketing, that percentage still equates to a small sample of 53 participants and only 25 or so in either condition.
A modest proportion of participants reported treatment seeking during the trial and treatment seeking by intervention condition revealed no significant differences between baseline and follow-up. Nevertheless, participants’ steps toward treatment seeking were in the right direction at each time point, which is encouraging considering the lack of treatment self-referral for the target population and the short follow-up time frame of this trial (30 days post-intervention). The potential for increased treatment-readiness and motivation for treatment-seeking has important research and practice applications, since motivation is a key ingredient for successful IPV treatment completion, which contributes to successful treatment outcomes, including cessation of violence (Maiuro & Murphy, 2008).
Contrary to expectations, there was a significant difference at 1-week follow-up with seven participants reporting treatment seeking in the Mail condition versus only one participant reporting treatment seeking in the MET condition. One explanation is that participants in the Mail condition who did not initially receive a MET session were “yearning” for something, which led them to seek treatment at a higher rate than MET participants, who may have felt satisfied with what they received. Another explanation concerns a methodological constraint in the study. The OLS session was conducted in a didactic manner and avoided using an MI style. MET participants who chose to attend an in-person OLS had the experience of expressing their motivation and thoughts to their counselor during the MET session but were then provided information on resources in a didactic and matter-of-fact manner during the OLS. This shift in counseling style may have decreased MET participants’ enthusiasm for subsequently entering treatment by stifling exploration of reasons for seeking treatment.
Our study was also interested in investigating the impact of the intervention on the likelihood of attending the OLS, IPV frequency, and substance use being mediated by factors associated with MET effectiveness, such as perceived norms. As hypothesized, at follow-up, reductions in misperceived norms for IPV and alcohol were larger in the MET group relative to the Mail group. (Note: We were unable to effectively evaluate changes in perceived norms for other drugs of choice due to the small proportion of participants reporting abuse of other substances.) These findings are significant for at least two reasons: (a) intervention and treatment approaches in alcohol use, which have been successful in changing perceived norms have been relatively successful in changing behavior (see Lewis & Neighbors, 2007; Neighbors, Larimer, & Lewis, 2004) and (b) this approach (changing men’s perceptions of other men’s use of violence as part of an intervention strategy) would have been untimely without first documenting this study’s finding that misperceptions exist in relation to IPV norms and that they are associated with behavior (see Neighbors et al., 2010). Furthermore, normative data have been an essential component of MET for early intervention and treatment of risky behaviors such as alcohol and drug abuse and show promise for its applicability with IPV perpetrators (see Neighbors et al., 2010).
To our knowledge, this research represents the first study using a randomized controlled trial to reach and motivate unadjudicated and nontreatment seeking substance-abusing IPV perpetrators to enter treatment. There are several limitations to consider in interpreting the findings. Data were drawn from a relatively small community sample of substance-using, unadjudicated, and nontreatment seeking IPV perpetrators. While this makes generalizability difficult, the purpose of the study was to develop and preliminarily evaluate a brief intervention. With promising findings included in this article and further evaluation of suggested intervention enhancements, the study should be replicated in an efficacy trial with a larger sample size. The follow-up period (1 month) may not have been adequate to assess treatment effects or evaluate the stability of the findings. Additional research is needed to evaluate the current promising findings with longer follow-up periods.
Reliance on self-report data is another potential limitation. Although the guarantee of confidentiality and use of reliable and well-validated measures reduces the risk of biased data (Babor, Steinberg, Anton, & Del Boca, 2000), intervention research with IPV perpetrators still presents complex issues with respect to self-report validity. Previous IPV research (see Easton et al., 2007; Gondolf, 2004) has found partner self-report to be more accurate compared to client self-report. Arrest records are the most easily documentable data available on IPV perpetrators’ recidivism and while they do not capture all repeat IPV offenses or behavior, they are the most frequently used objective recidivism measure (see Babcock, Green, & Robie, 2004; Gondolf, 2004) in addition to partner corroboration. Due to our study’s targeting nonadjudicated and nontreatment seeking IPV perpetrators from the community, we purposely avoided partner or agency corroboration in the case that it may have dissuaded enrollment in the trial. However, our success at reaching and enrolling participants is promising for future studies, which should evaluate the feasibility of partner, agency, and arrest-record corroboration. Other suggestions to improve future social work research in this area include increasing the sample size, evaluating treatment effects using a longer follow-up time frame than 30 days, comparing equivalent sample sizes of participants meeting SUD as well as IPV diagnostic criteria, including a similar time frame for drug use, and incorporating treatment readiness into the MET session, which would be a more natural and effective manner for encouraging treatment entry among participants. Despite limitations, the current research has several strengths and adds significantly to the IPV and SA literature. Although effect sizes on outcomes were small, the findings are important considering the underserved target population and innovation of the approach. Furthermore, given that IPV is typically addressed only after serious injury or death and criminal justice action, the intervention (with several enhancements) has the potential for interrupting violence in the home much earlier, thus saving lives and averting social damage. Finally, this novel intervention may provide a first step, low burden, and effective option for reaching nontreatment seeking and unadjudicated IPV perpetrators to self-refer into treatment.
Acknowledgment
The authors would like to thank Guy Ashmore, Devon Bushnell, Dawn Fabian, Edward Gignoux, Teryl Neil, Carolyn Speidel, and Avry Todd.
Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: A grant from the National Institute on Drug Abuse, 1 RO1 DA017873.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no conflicts of interest with respect to the authorship and/or publication of this article.
References
- Appel AE, Holden GW. The co-occurrence of spouse and physical child abuse: A review and appraisal. Journal of Family Psychology. 1998;12:578–599. [Google Scholar]
- Austin JB, Dankwort J. Standards for batterer intervention programs: A review and analysis. Journal of Interpersonal Violence. 1999;14:152–168. [Google Scholar]
- Babcock JC, Green CE, Robie C. Does batterers’ treatment work? A meta analytic review of domestic violence treatment. Clinical Psychology Review. 2004;23:1023–1053. doi: 10.1016/j.cpr.2002.07.001. [DOI] [PubMed] [Google Scholar]
- Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Baer JS, Stacy A, Larimer ME. Biases in the perception of drinking norms among college students. Journal of studies on Alcohol. 1991;52:580–586. doi: 10.15288/jsa.1991.52.580. [DOI] [PubMed] [Google Scholar]
- Baker CK, Perilla JL, Norris FH. Parenting stress and parenting competence among Latino men who batter. Journal of Interpersonal Violence. 2001;16:1139–1157. [Google Scholar]
- Bennett L, Stoops C, Call C, Flett H. Program completion and re-arrest in a batterer intervention system. Research on Social Work Practice. 2007;17:42–54. [Google Scholar]
- Bennett L, Williams OJ. Controversies and recent studies of batterer intervention effectiveness. Harrisburg, PA: National Electronic Network on Violence Against Women; 2001. [Retrieved June 21, 2007]. (VAWnet, PCADV/NRCDV). from http://www.vawnet.org. [Google Scholar]
- Bennett LW. Substance abuse by men in partner abuse intervention programs: Current issues and promising trends. Violence and Victims. 2008;23(2):236–248. doi: 10.1891/0886-6708.23.2.236. [DOI] [PubMed] [Google Scholar]
- Booth RE, Kwiatkowski C, Iguchi MY, Pinto F, John D. Facilitating treatment entry among out-of-treatment injection drug users. Public Health Reports. 1998;113:116–128. [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey KB. Peer influences on college drinking: A review of the research. Journal of Substance Abuse. 2001;13:391–424. doi: 10.1016/s0899-3289(01)00098-0. [DOI] [PubMed] [Google Scholar]
- Brown TG, Werk A, Caplan T, Seraganian P. Violent substance abusers in domestic violence treatment. Violence and Victims. 1999;14:179–190. [PubMed] [Google Scholar]
- Campbell J, Jones AS, Dienemann J, Kub J, Schollenberger J, O’Campo P, Wynne C. Intimate partner violence and physical health consequences. Archives of Internal Medicine. 2002;162:1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- Carey KB, Purnine DM, Maisto SA, Carey MP. Correlates of stages of change for substance abuse among psychiatric outpatients. Psychology of Addictive Behaviors. 2002;7:211–218. [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: A meta-analytic review. Addictive Behaviors. 2007;32:2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM. Treating drug dependence: Recent advances and old truths. In: Miller WR, Heather N, editors. Treating addictive behaviors. New York, NY: Plenum; 1998. pp. 217–230. [Google Scholar]
- Catalano SM. Criminal victimization, 2004. Washington, DC: U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; 2005. [Google Scholar]
- Centers for Disease Control and Prevention. Costs of intimate partner violence against women in the United States. Atlanta, GA: CDC, National Center for Injury Prevention and Control; 2003. Available from www.cdc.gov/ncipc/pub-res/ipv.htm. [Google Scholar]
- Chia SC, Gunther AC. How media contribute to misperceptions of social norms about sex. Mass Communication & Society. 2006;9:301–320. [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Daly J, Pelowski S. Predictors of dropout among men who batter: A review of studies with implications for research and practice. Violence and Victims. 2000;15:137–160. [PubMed] [Google Scholar]
- Daniels JW, Murphy CM. Stage and processes of change in batterers’ treatment. Cognitive and Behavioral Practice. 1997;4:123–145. [Google Scholar]
- Danielson KK, Moffitt TE, Caspi A, Silva PA. Comorbidity between abuse of an adult and DSM-III-R mental disorders: Evidence from an epidemiological study. American Journal of Psychiatry. 1998;155:131–133. doi: 10.1176/ajp.155.1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TM, Baer JS, Saxon AJ, Kivlahan DR. Brief motivational feedback improves post-incarceration treatment contact among veterans with substance use disorders. Drug and Alcohol Dependence. 2003;69:197–203. doi: 10.1016/s0376-8716(02)00317-4. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students. New York, NY: Guilford; 1999. [Google Scholar]
- Donovan DM, Rosengren DB, Downey L, Cox GC, Sloan KL. Attrition prevention with individuals awaiting publicly funded drug treatment. Addiction. 2001;96:1149–1160. doi: 10.1046/j.1360-0443.2001.96811498.x. [DOI] [PubMed] [Google Scholar]
- Dunford FW. The San Diego Navy Experiment: An assessment of interventions for men who assault their wives. Journal of Consulting and Clinical Psychology. 2000;68:468–476. doi: 10.1037//0022-006x.68.3.468. [DOI] [PubMed] [Google Scholar]
- Easton CJ, Mandel D, Babuscio T, Rounsaville BJ, Carroll KM. Differences in treatment outcome between male alcohol dependent offenders of domestic violence with and without positive drug screens. Addictive Behaviors. 2007;32:2151–2163. doi: 10.1016/j.addbeh.2007.01.031. [DOI] [PubMed] [Google Scholar]
- Easton CJ, Sinha R. Treating the addicted male batterer: Promising directions for dual-focused programming. In: Wekerle C, Wall A, editors. The violence and addiction equation: Theoretical and clinical issues in substance abuse and relationship violence. New York, NY: Brunner-Routledge; 2002. pp. 275–292. [Google Scholar]
- Edleson JL. Children’s witnessing of adult domestic violence. Journal of Interpersonal Violence. 1999;14:839–870. [Google Scholar]
- Edleson JL, Ellerton AL, Seagren EA, Kirchberg SL, Schmidt SO, Ambrose AT. Assessing child exposure adult domestic violence. Children and Youth Services Review. 2007;29:961–971. [Google Scholar]
- Fals-Stewart W. The occurrence of partner physical aggression on days of alcohol consumption: A longitudinal diary study. Journal of Consulting and Clinical Psychology. 2003;71:41–52. doi: 10.1037//0022-006x.71.1.41. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The Timeline Follow back reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting and Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- Fantuzzo JW, Mohr WK. Prevalence and effects of child exposure to domestic violence. The Future of Children. 1999;9:21–32. [PubMed] [Google Scholar]
- Feder L, Forde DR. The Broward experiment. In: Jackson S, Feder L, Forde DR, Davis RC, Maxwell CD, Taylor BG, editors. Batterer intervention programs: Where do we go from here? Washington, DC: National Institute of Justice; 2003. pp. 5–13. (2003) [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamnson DF, Spitz AM, Edwards V, Koss MP. The relationship of adult health status to childhood abuse and household dysfunction. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Goldkamp JS, Weiland D, Collins M, White M. The role of drug and alcohol abuse in domestic violence and its treatment: Dade county’s domestic violence court experience: Final report. Philadelphia, PA: Crime and Justice Research Institute; 1996. [Google Scholar]
- Gondolf EW. Batterer intervention systems: Issues, outcomes, and recommendations. Thousand Oaks, CA: SAGE; 2002. [Google Scholar]
- Gondolf EW. Evaluating batterer counseling programs. Aggression and Violent Behavior. 2004;9:605–631. [Google Scholar]
- Jones AS, D’Agostino RB, Jr, Gondolf EW, Heckert A. Assessing the effect of batterer program completion on reassault using propensity scores. Journal of Interpersonal Violence. 2004;19:1002–1020. doi: 10.1177/0886260504268005. [DOI] [PubMed] [Google Scholar]
- Kendall-Tackett KA. Health consequences of abuse in the family: A clinical guide for evidence-based practice. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- Kilmer JR, Walker DD, Lee CM, Palmer RS, Mallett KA, Fabiano P, Larimer ME. Misperceptions of College Student Marijuana use: Implications for prevention. Journal of Studies on Alcohol. 2006;67:277–281. doi: 10.15288/jsa.2006.67.277. [DOI] [PubMed] [Google Scholar]
- Kistenmacher BR, Weiss RL. Motivational interviewing as a mechanism for change in men who batter: A randomized controlled trial. Violence and Victims. 2008;23:558–570. doi: 10.1891/0886-6708.23.5.558. [DOI] [PubMed] [Google Scholar]
- Kivlahan DR, Marlatt GA, Fromme K, Coppel DB, Williams E. Secondary prevention with college drinkers: Evaluation of an alcohol skills training program. Journal of Consulting and Clinical Psychology. 1990;58:805–810. doi: 10.1037//0022-006x.58.6.805. [DOI] [PubMed] [Google Scholar]
- Labriola M, Rempel M, Davis RC. Do batterer programs reduce recidivism? Results from a randomized trial in the Bronx. Justice Quarterly. 2008;25:252–282. [Google Scholar]
- Larimer ME, Neighbors C. Normative misperceptions and the impact of description and injunctive norms on college student gambling. Psychology of Addictive Behaviors. 2003;17:235–243. doi: 10.1037/0893-164X.17.3.235. [DOI] [PubMed] [Google Scholar]
- Lehmann P. Post traumatic stress disorder (PTSD) and child witnesses to mother-assault: A summary and review. Children and Youth Services Review. 2000;22:275–306. [Google Scholar]
- Lewis MA, Neighbors C. Gender-specific misperceptions of college student drinking norms. Psychology of Addictive Behaviors. 2004;18:334–339. doi: 10.1037/0893-164X.18.4.334. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Social norms approaches using descriptive drinking norms education: A review of the research. Journal of American College Health. 2006;54:213–218. doi: 10.3200/JACH.54.4.213-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Optimizing personalized normative feedback: The use of gender-specific referents. Journal of Studies on Alcohol and Drugs. 2007;68:228–237. doi: 10.15288/jsad.2007.68.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincourt P, Kuettel TJ, Bombardier CH. Motivational interviewing in a group setting with mandated clients: A pilot study. Addictive Behaviors. 2002;27:381–391. doi: 10.1016/s0306-4603(01)00179-4. [DOI] [PubMed] [Google Scholar]
- Loue S. Intimate partner violence: Societal, medical, legal, and individual responses. New York, NY: Kluwer Academic/Plenum; 2001. [Google Scholar]
- Maiuro R, Murphy C, editors. Motivational interviewing and stages of change in intimate partner violence. New York, NY: Springer; 2009. [Google Scholar]
- Martino S, Carroll KM, O’Malley SS, Rounsaville BJ. Motivational interviewing with psychiatrically ill substance abusing patients. American Journal of Addictions. 2000;9:88–91. doi: 10.1080/10550490050172263. [DOI] [PubMed] [Google Scholar]
- Max W, Rice DP, Finkelstein E, Bardwell RA, Leadbetter S. The economic toll of intimate partner violence against women in the United States. Violence and Victims. 2004;19:259–272. doi: 10.1891/vivi.19.3.259.65767. [DOI] [PubMed] [Google Scholar]
- Mbilinyi L, Walker D, Neighbors C, Roffman R, Zegree J, Edleson J. Motivating substance-involved perpetrators of intimate partner violence to seek treatment: A focus on fathers. In: Maiuro R, Murphy C, editors. Motivational interviewing and stages of change in intimate partner violence (chap. 8) New York, NY: Springer; 2009. [Google Scholar]
- Mbilinyi LF, Zegree J, Roffman RA, Walker D, Neighbors C, Edleson J. Development of a marketing campaign to recruit non-adjudicated and untreated abusive men for a brief telephone intervention. Journal of Family Violence. 2008;23:343–351. doi: 10.1007/s10896-008-9157-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford; 2002. [Google Scholar]
- Miller WR, Wilbourne PL. Mesa Grande: A methodological analysis of clinical trials of treatment for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Yahne CE, Tonigan SJ. Motivational interviewing in drug abuse services: A randomized trial. Journal of Consulting and Clinical Psychology. 2003;71:754–763. doi: 10.1037/0022-006x.71.4.754. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin TM, Manuel JK, Miller WR. The motivational interviewing treatment integrity (MITI) code. 2nd ed. University of New Mexico; 2003. Unpublished manual. Retrieved from http://casaa.unm.edu/download/miti.pdf. [Google Scholar]
- Murphy CM, Baxter VA. Motivating batterers to change in the treatment context. Journal of Interpersonal Violence. 1997;12:607–619. [Google Scholar]
- Murphy CM, Eckhardt CI. Treating the abusive partner: An individualized cognitive-behavioral approach. New York, NY: Guilford; 2005. [Google Scholar]
- Musser PH, Semiatin JN, Taft CT, Murphy CM. Motivational interviewing as a pregroup intervention for partner-violent men. Violence and Victims. 2008;23:539–557. doi: 10.1891/0886-6708.23.5.539. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer-delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Walker D, Mbilinyi L, O’Rourke A, Edleson JL, Zegree J, Roffman RA. Normative misperceptions of abuse among perpetrators of intimate partner violence. Violence Against Women. 2010;16:370–386. doi: 10.1177/1077801210363608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Fals-Stewart W, Murphy M, Murphy CM. Partner violence before and after individually based alcoholism treatment for male alcoholic patients. Journal of Consulting and Clinical Psychology. 2003;71:92–102. doi: 10.1037//0022-006x.71.1.92. [DOI] [PubMed] [Google Scholar]
- O’Farrell T, Murphy C. Marital violence before and after alcoholism treatment. Journal of Consulting & Clinical Psychology. 1995;63:256–262. doi: 10.1037//0022-006x.63.2.256. [DOI] [PubMed] [Google Scholar]
- Ogle R, Baer J. Addressing the service linkage problem: Increasing substance abuse treatment engagement using personalized feedback interventions in heavy-using female domestic violence shelter residents. Journal of Interpersonal Violence. 2003;18:1311–1324. doi: 10.1177/0886260503256659. [DOI] [PubMed] [Google Scholar]
- Palmer SE, Brown RA, Barrera ME. Group treatment program for abusive husbands: Long term evaluation. American Journal of Orthopsychiatry. 1992;62:276–283. doi: 10.1037/h0079336. [DOI] [PubMed] [Google Scholar]
- Paymar M, Barnes G. Countering confusion about the Duluth Model. Minneapolis, MN: Special Report for the Battered Women’s Justice Project; 2006. Available from www.bwjp.org or www.duluth-model.org/recentresearch. [Google Scholar]
- Roffman R, Edleson J, Neighbors C, Mbilinyi L, Walker D. The men’s domestic abuse check-up: A protocol for reaching the non-adjudicated and untreated man who batters and abuses substances. Journal of Violence Against Women. 2008;14:589–605. doi: 10.1177/1077801208315526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R, Rosnow RL, Rubin DB. Contrasts and effect sizes in behavioral research: A correlational approach. Cambridge, England: Cambridge University Press; 2000. [Google Scholar]
- Rossman BBR. Longer term effects of children’s exposure to domestic violence. In: Graham-Bermann S, editor. Domestic violence in the lives of children. Washington, DC: American Psychological Association; 2001. pp. 35–65. [Google Scholar]
- Schneider RJ, Casey J, Kohn R. Motivational versus confrontational interviewing: A comparison of substance abuse assessment practices at employee assistance programs. Journal of Behavioral Health Services and Research. 2000;27:60–74. doi: 10.1007/BF02287804. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Stotts AM, Schmitz JM, Rhoades HM, Grabowski J. Motivational interviewing with cocaine-dependent patients: A pilot study. Journal of Consulting and Clinical Psychology. 2001;69:858–862. doi: 10.1037//0022-006x.69.5.858. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol. 1994;55(12):70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Straus M, Gelles R. Physical violence in American families—Risk factors and adaptations to violence in 8,145 families. New Brunswick, NJ: Transaction Publishers; 1990. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2). Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Swanson AJ, Pantalon MV, Cohen KR. Motivational interviewing and treatment adherence among psychiatric and dually-diagnosed patients. Journal of Nervous & mental Disease. 1999;187:630–635. doi: 10.1097/00005053-199910000-00007. [DOI] [PubMed] [Google Scholar]
- Taylor BG, Davis RC, Maxwell CD. The effects of a group batterer treatment program in Brooklyn. Justice Quarterly. 2001;18:170–201. [Google Scholar]
- Taylor CA, Sorenson SB. Community-based norms about intimate partner violence: Putting attributions of fault and responsibility into context. Sex Roles. 2005;53:573–589. [Google Scholar]
- Thompson MP, Kingree JP. The roles of victim and perpetrator alcohol use in intimate partner violence outcomes. Journal of Interpersonal Violence. 2006;21:163–177. doi: 10.1177/0886260505282283. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. Full report of the prevalence, incidence, and consequences of violence against women. Washington, DC: Office of Justice Programs, U.S. Department of Justice; 2000. Retrieved from http://www.ncjrs.gov/pdffiles1/nij/183781.pdf. [Google Scholar]
- Walker DD, Roffman RA, Stephens RS, Kim W, Berghuis J. Motivational enhancement therapy for adolescent marijuana users: A preliminary randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Neighbors C. Feedback interventions for college alcohol misuse: What, why and for whom? Addictive Behaviors. 2005;30:1168–1182. doi: 10.1016/j.addbeh.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisner C, Gilmer T, Saltzman L, Zink T. Intimate partner violence against women. Journal of Family Practice. 1999;48:439–443. [PubMed] [Google Scholar]