Summary
Objectives/Hypotheses
There are many documented barriers to successful adherence to voice therapy. However, methods for facilitating adherence are not well understood. The purpose of this study was to determine if patient adherence could be improved by providing patients with practice support between sessions using mobile treatment videos.
Methods
Thirteen voice therapy participants were provided with portable media players containing videos of voice exercises exemplified by their therapists and themselves. A randomized crossover design of two conditions was used: (1) standard of care voice therapy where participants were provided with written homework descriptions; and (2) video-enhanced voice therapy where participants received a portable digital media player with clinician and self-videos. The duration of each condition was 1 week.
Results
Practice of voice exercises was significantly greater in the video-enhanced voice therapy condition than in the standard of care “written” condition (P < 0.05). Three aspects of participant motivation for practice-overall commitment to practice, importance of practice, and confidence in the ability to practice were also significantly greater after video-enhanced condition than after standard of care condition.
Conclusion
These results support the use of video examples and portable digital media players in voice therapy for individuals who are comfortable using such technology.
Keywords: Patient compliance, Treatment adherence, Patient adherence, Social-cognitive theory, Voice, Voice therapy, MP4 players, Mobile, Digital portable media players, Self-efficacy, Goal commitment, Persuasive technology, Behavioral informatics
INTRODUCTION
Patient compliance presents a common problem in voice therapy. Approximately half of patients referred for voice therapy do not initiate or complete treatment.1–3 Of those patients who do attend sessions, inadequate practice between sessions has been noted by clinicians4,5 and reported by patients.6 Poor maintenance of treatment gains over time has also been documented and is thought to be caused by poor long-term adherence.7 Because voice therapy is behavioral in nature, adherence is inherently important to attaining acceptable treatment outcomes. Among direct voice therapy protocols such as confidential voice and resonant voice, adherence may be a stronger predictor of outcome than the specific treatment approach used in therapy.8 Therefore, development of effective methods for improving adherence to home practice and generalization appears important in achieving desired short- and long-term outcomes of voice therapy.
Voice therapy is typically provided on a weekly basis, requiring home practice and generalization of voice technique between sessions. Written instructions and occasionally, audio recordings are provided to assist patients in their intersession adherence.9 However, patients report a variety of reasons for poor treatment adherence, including difficulty remembering the details of voice exercises and difficulty judging accuracy of practice and generalization without clinician feedback.6 This confusion results in demoralization and reduction or elimination of practice until the next session.6 By their orthographic nature, written instructions do not provide an audiovisual example of the exercise or technique. Similarly, audio recordings lack visual information about voice production mechanics. Therefore, the provision of video examples of voice therapy may be useful in improving intersession adherence of voice exercises and motivation to practice.
In addition to the logical utility of providing video examples for voice therapy practice, the approach is supported theoretically and empirically. According to social-cognitive theory, both external factors (eg, environmental and social influences) and internal factors (eg, patient beliefs and emotions) mediate behavior and can reciprocally affect each other.10 Specifically, provision of example models can influence individuals’ task-specific confidence or “self-efficacy” to complete a modeled task.10,11 Likewise, goal setting theory posits that clarification of a task improves individuals’ commitment to completing this task (ie, “goal commitment”).12–14 Together, self-efficacy and goal commitment are aspects of motivation that can increase perseverance to master a task.11,12,15–18 Video models have been shown to improve adherence to health related, social, and academic tasks.19–21 A subcategory of video modeling—video self-modeling (ie, the observation of images of oneself performing an adaptive behavior) has been shown to improve accuracy and self-efficacy for a wide variety of motor and social skills including fluent speech production.22–25 Therefore, in seeking to improve adherence via video modeling, both clinician and self-models might be used, and both self-efficacy and goal commitment may be worth investigating.
The purpose of this study was to assess whether portable video examples of voice-therapy exercises result in more frequent practice and greater motivation for practice than written homework descriptions. Our hypothesis was that practice frequency would be greater during a treatment condition where video examples of therapy exercises are provided than in a condition where written instructions are provided. In addition, we hypothesized that motivation for practice would be greater after the video than the written condition, as evidenced by greater self-efficacy and goal commitment.
METHODS
Research design
The research design used for this study was a randomized crossover trial comparing 1 week of home practice supported by written instructions (written condition) with 1 week of home practice supported by digital media players containing treatment videos (video condition) in addition to written instructions. Written instructions were included in the video condition to provide all participants with the standard of care for provision of voice therapy homework. To accomplish randomization of condition order, patients were randomized into either group 1 or group 2. Group 1 participants received the video condition in the first week of voice therapy and the written condition in the second week of therapy, whereas the reverse was true for group 2. This repeated-measures design was chosen to increase statistical power to allow detection of clinically meaningful differences between treatments by having each participant serve as his or her own control.25 Approval for this study was granted by the University of Wisconsin Minimal Risk Institutional Review Board (IRB).
Participants and clinical care
Fifteen consecutive patients referred for resonant voice therapy, aged 19–73 years, were invited to participate in this study. One patient did not return for voice therapy and was therefore not enrolled. The remaining 14 patients enrolled after an IRB-reviewed consent process. One participant dropped out after one session because the study was “too much work.” Of the 13 remaining participants, two did not complete all questionnaires, but one did yield practice count data for analysis, for a total of 12 participants. Group 1 was composed of six participants including three men and three women aged 28–64 years and included equal numbers of participants with muscle tension dysphonia (mean age 35.6 years) and presbyphonia (mean age 62.3 years). Group 2 also comprised six participants (five women and one man), including four individuals with muscle tension dysphonia (mean age 42.3 years) and two with presbyphonia (mean age 62 years).
Inclusion and exclusion criteria information were obtained from each participant via self-report. The inclusion criterion was a clinical recommendation of at least three weekly sessions of resonant voice therapy. Exclusion criteria were neurogenic dysphonia, chronic cough, a recommendation for intensive therapy such as for Lee Silverman voice treatment.26 In addition, we included only patients who felt that they: (1) were able to man ually manipulate a small object; and (2) did not have a visual impairment. These final criteria were deemed important for easy use of the portable digital media player and excluded any individuals with these limitations, including those with fine motor or vision impairment because of aging.
All therapy sessions were provided by four speech-language pathologists specializing in voice at the University of Wisconsin Voice and Swallow Clinic and did not include the authors of this article. Participating clinicians used a resonant voice therapy approach to optimize forward tone focus in increasingly longer sound sequences and utterances, and improve respiratory-phonatory control to avoid vocal fry, hyper- and hypofunction. Voice exercises included forward-focus facilitators such as lip trills, humming, voiced fricatives, and /m/ and /w/-initial voice production of syllables, words and phrases, sentences, paragraphs, and conversations. During the course of the study—the first 2 weeks of therapy—the focus was primarily on teaching patients to identify and produce resonant voice in limited phonemic contexts, rather than generalizing a healthy vocal technique to the conversational level.
Although treatment goals included both practice and generalization, the goal relevant to this study was “practicing your voice exercises three to five times per day” during the upcoming week. Measures of practice count and motivation were presented in reference to this goal.
Intervention
For the written condition, treating clinicians prepared written instructions according to the current standard of care for presenting home exercises. For the video condition, each clinician recorded digital videos of frequently used voice exercises before initiation of the study and placed these videos onto a portable digital media player for each participant. In addition, individualized voice exercises and cues, and participant practice examples were recorded during the participant's therapy session as deemed necessary by the clinician, comprising individualized clinician and self-as-model videos.
Instrumentation
Digital treatment videos were captured on a desktop computer using a 1.3 MP Webcam with built-in microphone (Logitech QuickCam Communicate MP Color Audio Hi-Speed USB 960-000240; Romanel-sur-Morges, Switzerland), and downloaded onto 2 Gb MP3/MP4 players with 1.8-inch screen display and earphones (Davis Micro, Shenzhen, China) after converting video files to a proprietary file format used by these media players. Participants borrowed the portable digital video players from the study during their participation in the video condition. Each device cost approximately $18. One participant chose to use her own digital media (MP4) player. All other participants returned the devices at the end of the video condition. At the start of the video condition, participants received hands-on instruction in using the MP4 player until they were able to demonstrate successful independent operation of the unit. In addition, they received a written instruction sheet about MP4 player operation and the PI's phone number to call for tech support.
Measures
The measures described below were obtained at three time points. Time 1 was at the end of the first treatment session (ie, the beginning of week 1), time 2 was at the end of the first week of therapy, and time 3 was at the end of the second week of therapy.
Practice frequency
Using a small plastic tally counter attached to their personal key chains, participants tracked how often they practiced their voice exercises for at least 2-minute periods. This practice count was reported after the first week of therapy (time 2) and after the second week of therapy (time 3).
Motivation
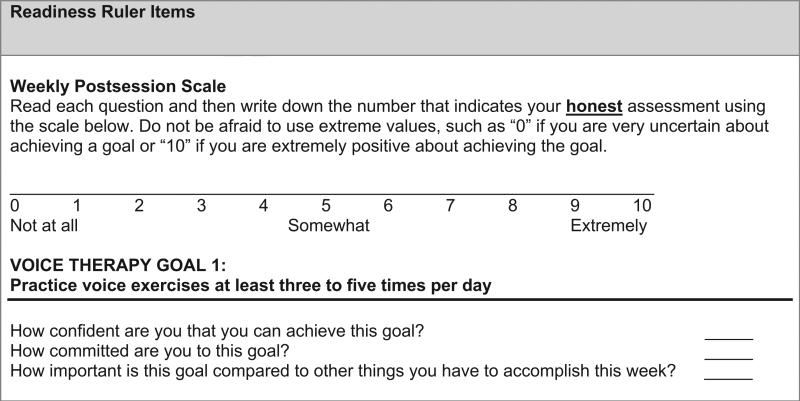
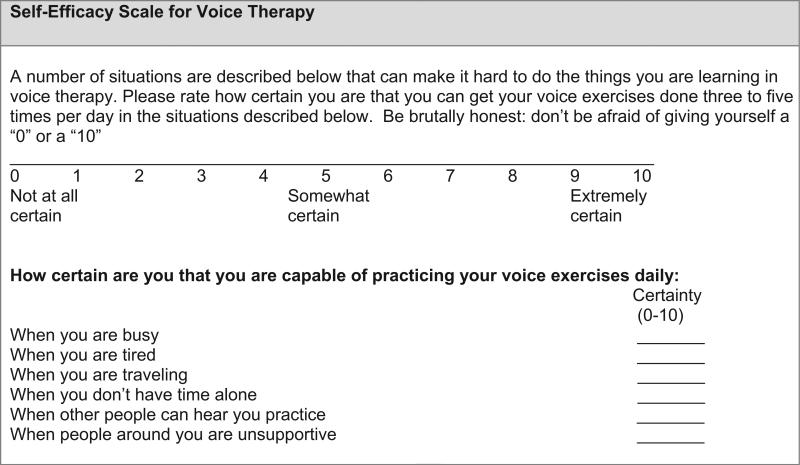
To assess participant motivation to complete daily voice exercise, participants were asked to complete the Readiness Ruler18,27 regarding this goal, and the self-efficacy scale for voice therapy section 1, which concerns voice therapy exercise practice28 regarding this goal. Both scales employed a 0–10 visual analog scale ranging from anchors “not at all” for the value 0 to “extremely” for the value 10 (Figures 1 and 2).
FIGURE 1.
Readiness Ruler items for practice.
FIGURE 2.
Self-efficacy Scale for voice therapy.
The Readiness Ruler contained one item capturing overall self-efficacy for achieving the treatment goal, and two items pertaining to the construct of goal commitment: commitment to the goal and relative importance of the goal compared with other tasks. The Self-efficacy Scale for Voice Therapy (section 1) asked participants to rate their confidence in overcoming six common barriers to regular practice. Items were previously developed28 using established methods of scale development and specific recommendations regarding measurement of self-efficacy as outlined by Bandura.29
Qualitative measure: brief unstructured interview
As suggested by methods of qualitative research, self-report measures of practice count and motivation were supplemented by qualitative interview data—an approach referred to as “triangulation.”30 Participants were interviewed briefly at time 3 (the end of the study period) to assess their experiences with the use of the portable digital media player and allow them to comment on any other aspect of the study. These comments were directly transcribed into electronic documents and analyzed for themes, as consistent with established qualitative analysis methods.30
Statistical analysis
Because of the small sample size, nonparametric statistics were chosen as the most conservative and appropriate method for analysis of results. The statistical significance of difference scores between conditions was tested with the matched-pair Wilcoxon signed rank test. An α-level of .05 was used to establish statistical significance. Exact P values were calculated and because of this, the sample size is noted in each comparison, rather than the degrees of freedom.31
RESULTS
Practice frequency
On average, participants practiced more than twice as often in the video condition than in the written condition: a difference that was statistically significant (Table 1). Only two individuals practiced more frequently in the written condition. However, in both conditions, the amount of practice fell short of clinician recommendations to practice at least three to five times per day. Of 12, four individuals in the video condition practiced three to five times per day, and no individuals did so during the written condition.
TABLE 1.
Differences in Practice and Practice Motivation for Written and Video Conditions
| Written Condition |
Video Condition |
||||||
|---|---|---|---|---|---|---|---|
| Measure | Mean | SD | Mean | SD | Tw* | N | P Value |
| Practice frequency per day | 0.98 | 0.76 | 2.09 | 1.4 | 72.5 | 12 | 0.0026† |
| Self-efficacy scale for practice | 4.84 | 2.57 | 5.18 | 2.18 | 40.5 | 11 | >0.05 |
| Readiness Ruler | |||||||
| Self-efficacy for practice | 6.73 | 2.24 | 7.54 | 1.86 | 51.5 | 11 | 0.03† |
| Goal commitment for practice | 7.72 | 2.45 | 8.36 | 1.69 | 54 | 11 | 0.018† |
| Relative importance of practice | 5.82 | 2.68 | 7.27 | 2.76 | 58 | 11 | 0.01† |
Abbreviation: SD, standard deviation.
Test statistic of the matched pair Wilcoxon signed rank test.
Pvalue < 0.05 indicating statistical significance.
Motivation
On the Readiness Ruler, participant ratings of overall self-efficacy for practice were significantly greater after use of the portable video examples than after a week of practice with written instructions (Table 1). Likewise, ratings of commitment to practice were significantly greater than the written condition (Table 1). Participants also rated the relative importance of practice more highly after practicing with video support than after practice in the written condition, and this difference was also significant (Table 1). Most participants performed better in the video condition, but some experienced no difference between conditions. Two individuals rated their overall self-efficacy greater in the written condition, one did so for importance, and two for commitment.
No significant difference between conditions was found for self-efficacy for practice measured using the Self-efficacy Scale for Voice Therapy although participants scored higher after the video condition than after the written condition (Table 1). These means were also lower than those indicating aspects of motivation on the Readiness Ruler.
Qualitative results: participant comments
Usability
Only one participant was familiar with using a portable digital media player before the study, whereas the remaining participants learned how to use an MP4 player for the purpose of this study. Four participants, three of whom were 60 years or older, reported some displeasure using the video player because they experienced difficulty understanding how to use the device or watching videos on a small screen. For older participants, manual and visual limitations may have been age related.
Practice comparison
When asked to compare the two practice conditions, 10 of the 12 participants reported that they received benefit from using the video player. Three themes emerged from participants’ positive comments: video examples improved (1) accuracy of practice, (2) self-efficacy for practice, and (3) normalization of the practice and use of resonant voice technique. Comments exemplifying each theme are shown in Table 2. As to the three participants who did not report benefit, one felt she did not need videos because she did not find the exercises difficult; one disliked doing voice exercises and had already moved to generalization when she was provided videos in week 2, and the third found voice therapy ineffective in resolving her voice disorder, which she said was caused by “mucus” and improved by drinking tea.
TABLE 2.
Qualitative Interview Comments
| Content Theme | Participant Comment Example |
|---|---|
| Accuracy | “It helped me remember what I'm supposed to be saying” |
| “Going through the exercises was incredibly helpful” | |
| “It was helpful to see the technique she [the clinician] was doing” | |
| “It reminds you about the mouth position” | |
| “I can check myself against [my clinician's] directions.” | |
| “I thought I did them just right when I was doing them with the recording” | |
| Self-efficacy | “I immediately felt better [knowing that]” I could do it. |
| “that I can do it right...seeing that I don't sound that different from the speech therapist [when practicing correctly] is helpful” | |
| Normalization | “that I'm not weird, that my voice is not weird” [when using resonant voice] |
| “I was surprised at how tolerable I was to listen to” [in resonant voice] | |
| [I am not] “too loud” [when using resonant voice] |
Two participants found that having the plastic tally counter attached to their purses was useful in reminding and motivating them to practice.
DISCUSSION
The results of this clinical study demonstrate a modest but statistically significant positive effect of MP4 video therapy examples on practice frequency and motivation when compared with a standard of care condition. The effect was large enough to be identified in a small “real world” clinical sample of patients, and overcome the heterogeneity of patients and clinicians.
Most participants practiced at least once more daily in the video than in the written condition, and reported that videos helped them remember how to do their voice exercises. Given the importance of practice frequency and accuracy in the acquisition of voice and speech motor skills31–33 this may constitute a meaningful increase in the dose of practice. Likewise, increased participant motivation scores on the Readiness Ruler may be meaningful because they were associated with greater practice frequency and positive comments about motivation. Thus, practice count, self-report scales, and qualitative comments were triangulated30 in support of the video intervention.
The portable video examples raised self-efficacy scores on the Readiness Ruler instrument item pertaining to self-efficacy, but not on the Self-efficacy Scale for Voice Therapy section pertaining to practice. There are two possible reasons for this. First, the Readiness Ruler captures overall self-efficacy for practice (ie, without a focus on logistic practice barriers) whereas the Self-efficacy Scale for Voice Therapy assesses self-efficacy to overcome a variety of practice barriers such as being busy, tired, or not alone. Lower mean ratings on the Self-Efficacy Scale (ie, averages of 4.84 and 5.18 for written and video conditions) compared with self-efficacy ratings on the Readiness Ruler (means of 6.73 and 7.84, respectively) may indicate this difference between barrier and overall self-efficacy. Participants’ increase in practice frequency in the video condition is consistent with their increase in Readiness Ruler score, whereas their failure to practice the recommended three to five times per day is consistent with lack of significant improvement on the Self-efficacy Scale for Voice Therapy. Solutions to practice barriers may have to be found if patients are to successfully overcome such barriers, or practice frequency goals scaled down to fit patients’ self-efficacy. Second, the barrier of “confusion” about exercises, addressed by the experimental intervention, was not measured as an item on the Self-efficacy Scale for Voice Therapy. An item concerning this barrier should be developed and included in the scale for future study.
Several causal mechanisms may explain positive effects of the video condition on practice frequency and motivation. Video content may have directly improved motivation, resulting in increased practice. This explanation is supported by participant comments regarding increased self-efficacy (“I can do it”) in response to video viewing. Conversely, video viewing may have resulted in increased practice and consequently increased motivation. A third possibility is that both practice and motivation were simultaneously affected by video supplementation, and subsequently interacted with each other. All three explanations are viable in Social Cognitive Theory's model of triadic asymmetrical reciprocal causation.10 Regression analysis of a larger sample of data could reveal the causal and reciprocal links between video support, practice behavior, and motivation.
Relationship of study results to previous research
Positive effects of the video condition are consistent with the theoretical premises of Social Cognitive Theory and Goal Setting Theory, which posit that models and task clarification can encourage task completion, self-efficacy, and goal commitment.10–12 In addition, results can be considered to fit coherently within the body of empirical evidence supporting the use of video modeling across behavioral treatments. For example, efficacy of video modeling is widely established as an approach to increase implementation of social behaviors and academic skills of school-aged children with special needs.19,22 Although this research does not address home practice programs, it does underscore the use of observing video models to affect task completion. In health behavior adherence research, several studies have demonstrated benefit of video modeling regarding home practice. For example, provision of clinician videos increased adherence to and self-efficacy for exercises to decrease COPD20 and efficacy of a COPD self-management program compared with standard of care.21 Likewise, in speech pathology, video modeling supplementation of home therapy has demonstrated efficacy for swallowing exercise completion34 and generalization of fluent speech.31,33 These studies differed from the present study in that one integrated videos into participants’ television viewing routine,34 thus further reducing the self-regulatory demand of scheduling, and the other addressed the stage of relapse after successful treatment completion, rather than the initial stage of skill acquisition.31,33 Like the present study, effects may have in part worked through the mechanism of motivation because patient satisfaction with video therapy was high. Thus, individuals participating in voice therapy are not unique in benefiting from video examples.
Limitations
The findings of this study are causally attributed to the difference in practice conditions. However, a novelty, halo, or “Hawthorne effect”35 cannot be ruled out, such that participants may have responded to the novelty of MP4 players, rather than the MP4 video content. Comparison of MP4 therapy example videos to a “sham” MP4 video condition devoid of therapy examples would be needed to determine the effect of having an MP4 player on practice and motivation.
Because the present study used a crossover design, voice outcomes could not serve as dependent variable. Therefore, it is not known whether video-supplemented practice yielded better voice outcomes or more accurate practice than the written condition. A randomized controlled design would allow both adherence (eg, practice frequency) and voice outcome measures to serve as dependent variables. Objective measurement of practice frequency and accuracy is also needed to validate participants’ self-report of practice. Furthermore, differential effects of clinician and self-videos could not be examined, because these videos were provided as a package treatment.
A final limitation is the sample size of this study was too small to allow for analysis by gender, age, and voice disorder. A larger study would allow one to analyze whether video modeling has differential effects on participant behavior and motivation according to these factors.
Clinical implications
Results of this study support the hypotheses that both patient motivation and behavior are, at least to some degree, mutable rather than static patient characteristics. Although this is known to be fundamentally true for learning and behavioral tasks, it has not been studied in voice therapy specifically. In this study, patient adherence to voice therapy was improved without changing the content of treatment. Consequently, clinicians may be able to improve their patients’ adherence through a feasible method that does not require increased time from the patient or the clinician. Patients who express concern about remembering their voice exercises correctly between sessions may benefit from video models. In addition, patients who find that their voice sounds “unnatural” using resonant voice may benefit from viewing themselves producing both their habitual and resonant voice on video.
Because costs involved in purchasing video recording equipment and MP4 players were low, strategies used in this study can be directly implemented in clinical settings. A variety of media choices for practice videos may need to be available to patients to suit the needs and limitations of different patients. Using such popular technology, patient access to and control over voice therapy content outside of the clinic may move voice therapy from an episodic model to a continuous model of treatment and support effective patient self-management of voice disorders.
Acknowledgments
The authors gratefully acknowledge the contributions of Heather Geye, Dr. Glen Leverson, and the voice clinicians at the University of Wisconsin Voice and Swallow Clinic to the completion of this work. In addition, Dr. Edie Hapner contributed to the development of the self-efficacy scale for voice therapy. This work was funded in part by a pre-doctoral fellowship grant awarded to Eva van Leer (NIDCD F31DC009526).
REFERENCES
- 1.Portone C, Johns MM, 3rd, Hapner ER. A review of patient adherence to the recommendation for voice therapy. J Voice. 2008;22:192–196. doi: 10.1016/j.jvoice.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Hapner E, Portone-Maira C, Johns MM., III A study of voice therapy dropout. Journal of Voice. 2009;23:337–340. doi: 10.1016/j.jvoice.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Smith BE, Kempster GB, Sims HS. Patient factors related to voice therapy attendance and outcomes. J Voice. doi: 10.1016/j.jvoice.2009.03.004. In press. [DOI] [PubMed] [Google Scholar]
- 4.Behrman A. Facilitating behavioral change in voice therapy: the relevance of motivational interviewing. Am J Speech Lang Pathol. 2006;15:215–225. doi: 10.1044/1058-0360(2006/020). [DOI] [PubMed] [Google Scholar]
- 5.van Leer E, Hapner ER, Connor NP. Transtheoretical model of health behavior change applied to voice therapy. J Voice. 2008;22:688–698. doi: 10.1016/j.jvoice.2007.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Leer E, Connor NP. Patient perceptions of voice therapy adherence. J Voice. 2009;24:458–469. doi: 10.1016/j.jvoice.2008.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Lierde KM, Claeys S, De Bodt M, van Cauwenberge P. Long-term outcome of hyperfunctional voice disorders based on a multiparameter approach. J Voice. 2007;21:179–188. doi: 10.1016/j.jvoice.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Verdolini-Marston K, Katherine Burke M, Lessac A, Glaze L, Caldwell E. Preliminary study of two methods of treatment for laryngeal nodules. J Voice. 1995;9:74–85. doi: 10.1016/s0892-1997(05)80225-5. [DOI] [PubMed] [Google Scholar]
- 9.Roy N, Weinrich B, Gray SD, Tanner K, Stemple JC, Sapienza CM. Three treatments for teachers with voice disorders: a randomized clinical trial. J Speech Lang Hear Res. 2003;46:670–688. doi: 10.1044/1092-4388(2003/053). [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 11.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 12.Locke EA, Latham GP. A Theory of Goal Setting and Task Performance. Prentice Hall International; Englewood Cliffs, NJ: 1990. [Google Scholar]
- 13.Hollenbeck JR, Klein HJ. Goal commitment and the goal-setting process: problems, prospects, and proposals for future research. J Appl Psychol. 1987;72:212–220. [Google Scholar]
- 14.Tubbs ME. Goal setting: a meta-analytic examination of the empirical evidence. J Appl Psychol. 1986;71:474–483. [Google Scholar]
- 15.Strecher VJ, Seijts GH, Kok GJ, et al. Goal setting as a strategy for health behavior change. Health Educ Q. 1995;22:190–200. doi: 10.1177/109019819502200207. [DOI] [PubMed] [Google Scholar]
- 16.Earley PC, Lituchy TR. Delineating goal and efficacy effects: a test of three models. J Appl Psychol. 1991;76:81–98. [Google Scholar]
- 17.Hollenbeck JR, Williams CR, Klein HJ. An empirical examination of the antecedents of commitment to difficult goals. J Appl Psychol. 1989;74:18–23. [Google Scholar]
- 18.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. Guilford Press; New York, NY: 2002. [Google Scholar]
- 19.Bellini S, Akullian J. A meta-analysis of video modeling and video self-modeling interventions for children and adolescents with autism spectrum disorders. Except Child. 2007;73:264–287. [Google Scholar]
- 20.Ng JYY, Tam SF, Yew WW, Lam WK. Effects of video modeling on self-efficacy and exercise performance of COPD patients. 1999:475. [Google Scholar]
- 21.Stellefson ML, Chaney BH, Chaney JD. Examining the efficacy of DVD technology compared to print-based material in COPD self-management education of rural patients. Californian J Health Promot. 2009;7:26–42. [PMC free article] [PubMed] [Google Scholar]
- 22.Hitchcock CH, Dowrick PW, Prater MA. Video self-modeling intervention in school-based settings: a review. Remedial and Special Education. 2003;24:36–46. [Google Scholar]
- 23.Cream A, O'Brian S, Jones M, et al. Randomized controlled trial of video self-modeling following speech restructuring treatment for stuttering. J Speech Lang Hear Res. 2009;53:887–897. doi: 10.1044/1092-4388(2009/09-0080). [DOI] [PubMed] [Google Scholar]
- 24.Cream A, O'Brian S, Onslow M, Packman A, Menzies R. Self-modeling as a relapse intervention following speech-restructuring treatment for stuttering. Int J Lang Commun Disord. 2009;44:587–599. doi: 10.1080/13682820802256973. [DOI] [PubMed] [Google Scholar]
- 25.Siegel S, Castellan NJ. Nonparametric Statistics for the Behavioral Sciences. 2nd ed. McGraw-Hill; New York, NY: 1988. The case of one sample, two measures or paired replicates: the Wilcoxon signed rank test. p. 87. [Google Scholar]
- 26.Ramig L, Countryman S, Thompson L, Horii Y. Comparison of two forms of intensive speech treatment for Parkinson disease. J Speech Hear Res. 1995;38:1232–1251. doi: 10.1044/jshr.3806.1232. [DOI] [PubMed] [Google Scholar]
- 27.Rollnick S, Mason P, Butler C. Health Behavior Change: A Guide for Practitioners. Churchill Livingstone; Edinburgh, UK: New York, NY: 1999. [Google Scholar]
- 28.van Leer E, Hapner ER. Validation of a self-efficacy scale for voice therapy. Presentation. 2005 Jun; [Google Scholar]
- 29.Bandura A. Guide for constructing self-efficacy scales. In: Pajares F, Urdan T, editors. Self-Efficacy Beliefs of Adolescents. 1st ed. Information Age Publishing; Greenwich, CT: 2006. pp. 307–337. [Google Scholar]
- 30.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 31.Verdolini K. On the voice: learning science applied to voice training: the value of being “in the moment”. Choral Journal. 2002;42:47–51. [Google Scholar]
- 32.Maas E, Robin DA, Austermann Hula SN, et al. Principles of motor learning in treatment of motor speech disorders. Am J Speech Lang Pathol. 2008;17:277–298. doi: 10.1044/1058-0360(2008/025). [DOI] [PubMed] [Google Scholar]
- 33.Verdolini K, Lee TD. Optimizing motor learning in speech intervention: theory and practice. In: Sapienza C, Casper J, editors. For Clinicians by Clinicians: Vocal Rehabilitation in Medical Speech-Lanaguage Pathology. 1st ed. PRO-ED; Austin, TX: 2001. pp. 403–446. [Google Scholar]
- 34.Lemoncello R, Sohlberg MM, Fickas S, Albin R, Harn BE. Phase I evaluation of the television assisted prompting system to increase completion of home exercises among stroke survivors. Disabil Rehabil Assist Technol. 2010 doi: 10.3109/17483107.2010.542571. [DOI] [PubMed] [Google Scholar]
- 35.Cook TD, Campbell DT. Quasi-Experimental Design and Analysis Issues for Field Settings. 1st ed. Wadsworth; New York, NY: 1979. Chapter 2: validity. pp. 50–58. [Google Scholar]