Abstract
Infections caused by Ewingella americana have been rarely reported in the literature. Most of the cases that have been reported were among the immunocompromised patients. We report a case of E. americana causing osteomyelitis and septic arthritis of the shoulder joint in a previous intravenous drug abuser. The causative pathogen was identified by synovial fluid analysis and culture.
1. Introduction
Ewingella americana is a rare gram negative, lactose fermenting, oxidase negative, catalase positive, indole negative, facultative anaerobic bacillus first described from clinical specimens in 1983 by Grimont et al. [1], as a new group in the Enterobacteriaceae family. It rarely causes human infections and has been identified from various clinical samples including sputum [2], conjunctiva [3, 4], blood [5–8], wound [9], and peritoneal dialysate [10]. Interestingly, it has also been isolated from the intestinal contents of snails and slugs [11], fresh nutria carcasses [12], vacuum packaged meat [13], and mushrooms [14] as well.
This case report is the first clinical description of E. americana causing osteomyelitis and septic arthritis of the shoulder joint.
2. Case Report
A 50-year-old male was admitted to the hospital, with gradual onset of pain and swelling in the right shoulder since 4 days. He denied fever, chills, or rigors. His past medical history was significant for hypertension and intravenous drug abuse. His last use of heroin was 2 months ago with an unsterilized needle contaminated by saliva, in the right arm. Physical examination revealed limited range of motion of right shoulder secondary to pain. Radiograph of the right shoulder was suggestive of osteomyelitis. A computed topographic scan of the shoulder revealed multifocal, intraarticular abscess formation involving the right upper extremity. It also showed erosion of the humeral head and the glenohumeral joint, consistent with septic arthritis (Figure 1). Arthrocentesis was done, and the cell count of the synovial fluid showed white blood cell count of 9.4 × 109/L (90% neutrophils, 1% bands). Cultures of the synovial fluid grew Ewingella americana. The antimicrobial susceptibility test carried out by disk diffusion method showed susceptibility to amikacin, ampicillin, cefazolin, gentamicin, piperacillin tazobactam, tobramycin, and trimethoprim sulfamethoxazole while was resistant to ciprofloxacin.
Figure 1.
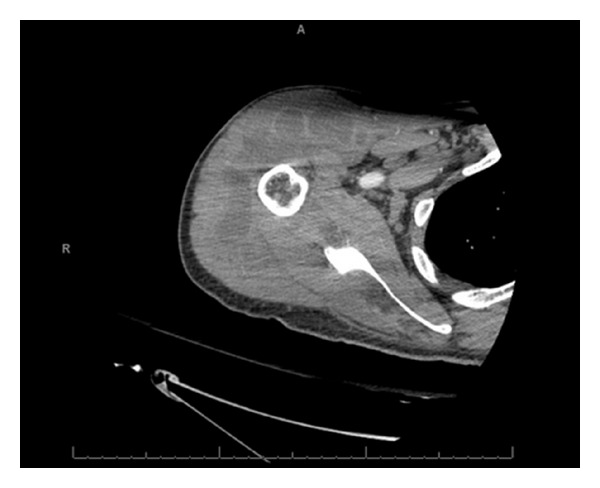
In the right upper extremity, there is a full thickness rotator cuff tear with a glenohumeral joint effusion and subacromial subdeltoid bursal fluid. Pockets of gas are noted in the glenohumeral joint effusion and the bursal fluid, suggestive of septic joint and septic bursitis with intramuscular abscesses.
The patient was started on ceftriaxone 2 gm intravenous every 24 hours. He continued to improve and was discharged home to complete 6 weeks of intravenous antibiotic therapy. He was followed 4 weeks later in the outpatient clinic and showed resolution of infection which was confirmed both clinically and by imaging. The antibiotic course was completed with no complications.
3. Discussion
Clinical infections due to E. americana have been reported to cause peritonitis [10], conjunctivitis [3, 4], bacteremia [8], and pneumonia [2, 15]. Colonization in wound [9] and sputum [2] were also reported in patients without causing clinical infection. Sepsis [5–8] and even death from Waterhouse-Friderichsen syndrome due to E. Americana [16] has also been reported.
E. Americana is seen in patients who were immunosuppressed due to diabetes mellitus [5], bone marrow transplantation, chemotherapy [7], end stage renal disease [10], and use of mercaptopurine [15]. Although, a few cases of E. americana have been reported earlier causing conjunctivitis [3, 4] and Waterhouse-Friderichsen syndrome [16] in previously healthy individuals, this is the first case of osteomyelitis involving the joint due to intravenous drug abuse. Based on this observation, clinicians may want to consider Ewingella Americana as an emerging true pathogen.
Since little information exists on the ecological niche of this organism, in our case we speculate on the source of contamination as saliva from the patient's mouth. Kati et al. [10] proposed domestic water to be a source of infection in peritonitis of a patient undergoing peritoneal dialysis. A contaminated ice bath was identified as the probable source in an outbreak of E. americana bacteremia, in patients who had undergone cardiovascular or peripheral vascular surgery [8]. Maertens et al. [7] speculated on inadequate hand hygiene as the source of infection. E. americana is an organism without nutritional needs that can survive in water and citrate solution and preferably grows at 4°C.
The only risk factor in our patient was that he was an intravenous drug abuser while using unsterilized needles for his heroin injections; he might have inoculated the pathogen into his blood causing transient blood stream infection which ultimately seeded into his shoulder joint.
To our knowledge, this case is the first report of osteomyelitis and septic arthritis caused by E. americana infection. Earlier reports suggested E. americana causing infections in immunocompetent host; however, in our case the infections were certainly favored by intravenous injections with contaminated material.
Consent
Informed consent is obtained from the patient for publication of this paper.
References
- 1.Grimont PAD, Farmer JJ, III, Grimont F, Asbury MA, Brenner DJ, Deval C. Ewingella Americana gen. nov., sp.Nov., a new enterobacteriaceae isolated from clinical specimens. Annales de l’Institut Pasteur. Microbiologie. 1983;134(1):39–52. doi: 10.1016/0769-2609(83)90102-3. [DOI] [PubMed] [Google Scholar]
- 2.Ryoo NH, Ha JS, Jeon DS, Kim JR, Kim HC. A case of pneumonia caused by Ewingella Americana in a patient with chronic renal failure. Journal of Korean Medical Science. 2005;20(1):143–145. doi: 10.3346/jkms.2005.20.1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Da Costa PS, Tostes MM, de Carvalho Valle LM. A case of keratoconjunctivitis due to Ewingella Americana and a review of unusual organisms causing external eye infections. The Brazilian Journal of Infectious Diseases. 2000;4(5):262–267. [PubMed] [Google Scholar]
- 4.Heizmann WR, Michel R. Isolation of Ewingella Americana from a patient with conjunctivitis. European Journal of Clinical Microbiology and Infectious Diseases. 1991;10(11):957–959. doi: 10.1007/BF02005452. [DOI] [PubMed] [Google Scholar]
- 5.Pien FD, Farmer JJ, Weaver RE. Polymicrobial bacteremia caused by Ewingella americana (family Enterobacteriaceae) and an unusual Pseudomonas species. Journal of Clinical Microbiology. 1983;18(3):727–729. doi: 10.1128/jcm.18.3.727-729.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Devreese K, Claeys G, Verschraegen G. Septicemia with Ewingella americana. Journal of Clinical Microbiology. 1992;30(10):2746–2747. doi: 10.1128/jcm.30.10.2746-2747.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maertens J, Delforge M, Vandenberghe P, Boogaerts M, Verhaegen J. Catheter-related bacteremia due to Ewingella americana. Clinical Microbiology and Infection. 2001;7(2):103–104. doi: 10.1046/j.1469-0691.2001.00195.x. [DOI] [PubMed] [Google Scholar]
- 8.Pien FD, Bruce AE. Nosocomial Ewingella americana bacteremia in an intensive care unit. Archives of Internal Medicine. 1986;146(1):111–112. [PubMed] [Google Scholar]
- 9.Bear N, Klugman KP, Tobiansky L, Koornhof HJ. Wound colonization by Ewingella americana. Journal of Clinical Microbiology. 1986;23(3):650–651. doi: 10.1128/jcm.23.3.650-651.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kati C, Bibashi E, Kokolina E, Sofianou D. Case of peritonitis caused by Ewingella americana in a patient undergoing continuous ambulatory peritoneal dialysis. Journal of Clinical Microbiology. 1999;37(11):3733–3734. doi: 10.1128/jcm.37.11.3733-3734.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muller HE, Fanning GR, Brenner DJ. Isolation of Ewingella Americana from mollusks. Current Microbiology. 1995;31(5):287–290. doi: 10.1007/BF00314581. [DOI] [PubMed] [Google Scholar]
- 12.Lyon WJ, Milliet JB. Microbial flora associated with Louisiana processed frozen and fresh nutria (Myocastor coypus) carcasses. Journal of Food Science. 2000;65(6):1041–1045. [Google Scholar]
- 13.Helps CR, Harbour DA, Corry JEL. PCR-based 16S ribosomal DNA detection technique for Clostridium estertheticum causing spoilage in vacuum-packed chill-stored beef. International Journal of Food Microbiology. 1999;52(1-2):57–65. doi: 10.1016/s0168-1605(99)00116-6. [DOI] [PubMed] [Google Scholar]
- 14.Reyes JE, Venturini ME, Oria R, Blanco D. Prevalence of Ewingella americana in retail fresh cultivated mushrooms (Agaricus bisporus, Lentinula edodes and Pleurotus ostreatus) in Zaragoza (Spain) FEMS Microbiology Ecology. 2004;47(3):291–296. doi: 10.1016/S0168-6496(03)00283-6. [DOI] [PubMed] [Google Scholar]
- 15.Pound MW, Tart SB, Okoye O. Multidrug-resistant Ewingella Americana: a case report and review of the literature. Annals of Pharmacotherapy. 2007;41(12):2066–2070. doi: 10.1345/aph.1K398. [DOI] [PubMed] [Google Scholar]
- 16.Tsokos M. Fatal Waterhouse-Friderichsen syndrome due to Ewingella Americana infection. American Journal of Forensic Medicine and Pathology. 2003;24(1):41–44. doi: 10.1097/01.PAF.0000051704.91568.A6. [DOI] [PubMed] [Google Scholar]


