SUMMARY
Radial forearm free flap surgery is a versatile technique that is widely adopted for microvascular reconstruction of the oral, oropharyngeal and hypopharyngeal lining. Nowadays, the technique for harvesting is standardized, while reconstruction of the forearm donor site defect is somewhat controversial. The authors describe a modified closure technique developed to reduce skin tension that provides subsequent improvement of the cosmetic appearance of the forearm donor site. A series of 43 patients undergoing radial forearm free flap (RFFF) reconstruction is presented, carried out by our ENT department between September 2007 and December 2010. The authors used a modification of the standard triangular full-thickness skin graft (FTSG) technique to close the forearm donor site on 23 patients with a new shape similar to a dagger. Using the Stony Brook Evaluation Scale, the authors analyzed the outcomes of 23 cases employing the dagger-shaped FTSG and compared these with a standard (triangular shaped) reconstructive graft used in 20 earlier patients. The new dagger-shaped graft decreases skin tension and reduces the need of multiple slits in the graft with improved aesthetic outcome; it is an effective method for repair of the forearm donor site with low tension and without the need to harvest the skin graft from the thigh. The technique is simple, reliable and requires no more time than a standard procedure.
KEY WORDS: Radial forearm free flap, Reconstructive surgery, Cosmetic appearance, Skin graft
RIASSUNTO
Il lembo libero di avambraccio è ancora oggi ampiamente utilizzato nella ricostruzione microvascolare di cavo orale, orofaringe ed ipofaringe. La tecnica di prelievo è standardizzata, mentre la ricostruzione del sito donatore è alquanto controversa. L'autore descrive una nuova tecnica di chiusura della cute dell'avambraccio elaborata per ridurre la tensione sui margini dell'innesto. Nel periodo compreso fra settembre 2007 e dicembre 2010, 43 pazienti sono stati sottoposti ad intervento chirurgico di ricostruzione del cavo orale e dell'oroipofaringe con lembo libero rivascolarizzato di avambraccio. Negli ultimi 23 casi trattati la tecnica di chiusura con innesto triangolare V-Y a tutto spessore è stata modificata e sostituita con un nuovo modello di innesto a forma di pugnale. Utilizzando la Stony Brook Scar Evaluation Scale gli esiti cicatriziali della superficie volare dell'avambraccio sono stati analizzati e confrontati ed è emersa una differenza statisticamente significativa a favore del gruppo di pazienti sottoposti a ricostruzione con innesto modificato (p < 0,01). L'innesto a forma di pugnale riduce la tensione lungo la linea di sutura e ciò consente un numero inferiore di incisioni sull'innesto riducendo l'effetto "a maglie"; ne consegue un miglior risultato estetico a distanza. La tecnica è semplice, affidabile e non richiede un allungamento dei tempi chirurgici.
Introduction
Radial forearm free flap (RFFF) is a versatile reconstructive method, first described by Yang et al. in 1981 1. Several types of free flaps can be used to restore defects within the oral cavity and oro-hypopharynx (anterolateral thigh flap, rectus abdominis musculocutaneous flap, free deltoid flap, etc.), but a radial flap is widely preferred 2-5. Regarding the standard technique, in 1994, Liang et al. proposed to triangulate the volar donor defect of the radial forearm free flap and close it with a triangular shaped full-thickness skin graft harvested adjacent to the donor site 6 7. In addition, Shiba has standardized the features of this graft in terms of size and length 8. The advantages of this kind of flap are pliability, thinness, mostly hairless skin, large diameter, long and constant vascular pedicle, and low bulk. These characteristics are useful to repair complex three-dimensional defects, for example, small intra-oral tissue defects 3 5. Many skin closure methods have been developed to improve the aesthetic outcome of the forearm donor site but, at present, this topic is somewhat controversial. Some surgeons prefer to harvest a split thickness skin graft from the thigh or the groin for donor site closure, but this procedure may be associated with morbidities including pain, infection and hypertrophic scar formation.
The authors describe a modification of the standard triangular- shaped technique, performed in 23 cases using forearm free flap 3-dimensional microvascular reconstruction, in order to improve cosmetic appearance by lowering skin graft tension. The aesthetic outcomes of these 23 patients were analyzed using the Stony Brook Scar Evaluation Scale and compared with 20 other patients who underwent a standard V-Y closure technique.
Materials and methods
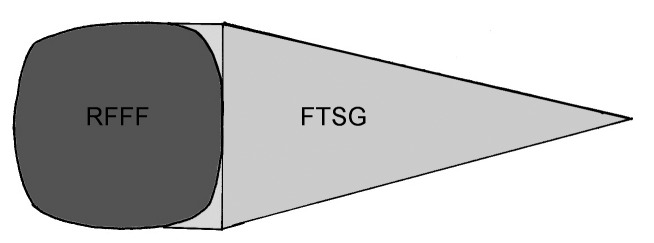
In the period between September 2007 and December 2010, 43 patients underwent RFFF reconstruction for a variety of head and neck surgical defects due to squamocellular carcinoma ablation at the Department of Otorhinolaryngology, "San Raffaele" Hospital, Milan. This study conformed to the ethical standards according to the Declaration of Helsinki published in 1964 in its present version. All patients were assessed preoperatively with the Allen test and colour Doppler ultrasonography to investigate collateral circulation (ulnar artery and vein) of the forearm and neck. Each RFFF was harvested in a similar fashion with forearm fascia, radial artery, cephalic vein and vena comitans; none of the patients had a radial osteocutaneous free flap. In total, 35 flaps were harvested from the left and 8 from the right forearm based on hand dominance and vascular test results. The flaps were elevated with a pneumatic tourniquet inflated to 250 mmHg for a maximum of 90 min; the flaps ranged in size from 8 x 8 cm to 5 x 5 cm with an average surface area of 38.4 cm2. In all patients, we used the V-Y technique with a skin graft whose height was twice the RFFF length in the direction of the forearm axis. According to Shiba's statement, the width of the graft was shorter than half of the wrist circumference. The full thickness skin graft (FTSG) was finally elevated with a scalpel, defatted using a scissors and then stored in saline. Multiple slits in the graft were made to prevent fluid collection beneath the graft and to allow the graft to be stretched to cover a larger area. The dressing was maintained for about 6 days. The forearm donor site skin defect consisted of the defect attributable to both RFFF and FTSG harvesting; the distal side of the defect area was covered with the FTSG, while the proximal side of the defect area was primarily closed. In 20 consecutive patients, a standard FTSG shaped like an isosceles triangle was adopted for skin closure, while in the other 23 patients, reconstruction was performed with a new model of FTSG, shaped like a dagger. As shown in Figure 1, the RFFF is usually drawn with rounded edges and as a consequence, two triangles (triangles between RFFF and FTSG) are usually sacrificed when the pyramidal FTSG is translated to close the total donor site defect (Fig. 1).
Fig. 1.
Radial forearm flap (RFFF) with standard full thickness skin graft (FTSG): triangles between RFFF and FTSG are usually sacrificed because the flap is drawn with round edges.
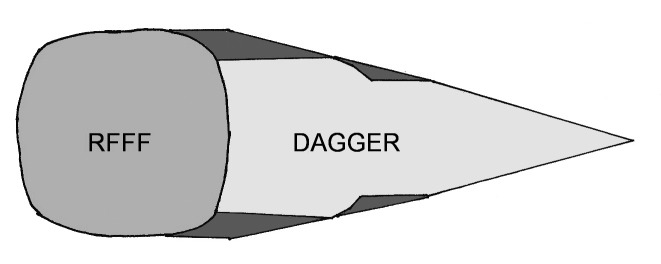
Accordingly, the authors devised a new dagger-shaped FTSG with a particular perimeter that matches the skin defect of the donor site by reducing the surface tension and preserving the two triangles of skin (Fig. 2).
Fig. 2.
Full thickness skin graft with the new shape that preserves more skin (dark grey triangles) compared to the standard technique.
As shown in the following demonstration, this new shape can be approximated to a geometric construction whose area is given by the sum of six different polygons. Comparison of this new shape with the previous FTSG showed a savings of 8.3% of the skin graft.
Demonstration:
A minimum post-operative time period of 3 months was required before collecting aesthetic outcome data. The quality of scars was evaluated with the Stony Brook Scar Evaluation Scale. This scale, proposed in 2007 by Singer et al. 9, measures cosmetic outcome of the wound through its width, height, colour, suture mark and overall appearance. Objective, blinded evaluation of aesthetic outcome of forearm reconstructions was done by two head and neck surgeons from our department. High-resolution digital photographs of the operative site were taken in a standardized setting on a sky-blue background. The final score for cosmetic outcome ranged from 0 (worst) to 5 (best). The median values of the two subgroups (20 standard FTSG vs. 23 dagger-shaped FTSG) were compared in terms of aesthetic results. Moreover, four other features of scar healing (i.e. hand swelling, tendon exposure, rate of graft infection and wrist stiffness) were evaluated during follow up (after 3-6 months). Statistical analysis was performed with Minitab Statistical software; all p-values were two-sided and p-values < 0.01 were considered significant.
Results
In terms of reconstructive surgery procedures, there were no differences between the two methods of donor site skin closure after RFFF harvesting (20 standard FTSG vs. 23 dagger-shaped FTSG). In the 20 cases performed before the application of the new skin closure method, we noticed excessive suture tension in the middle portion of the forearm with some cases of partial detachment of the skin graft due to excessive edge traction. Specifically, the larger the skin defect, the more difficult the closure. The last 23 cases were treated with the new dagger-shaped skin graft in a proportion of 2:3, between FTSG and total skin defect, which was always respected; these defects presented better outcomes with no tendon exposure (30% vs. 0%) and no infections recorded (25% vs. 0%). Similarly, hand swelling (55% vs. 13%) and wrist stiffness (40% vs. 17%) decreased in this group of patients. Comparison between standard and dagger-shaped grafts showed a statistical difference for all features analysed except wrist stiffness (chi-square test, Fisher's exact test, p < 0.01) (Table I). Moreover, an analysis of aesthetic outcomes, in terms of colour thickness and width of the wound measured with the Stony Brook Scar Evaluation Scale, showed a statistical difference between groups (Student's t-test, p < 0.01). In the first group (with standard FTSG; Fig. 3), the mean value among the 20 patients was 2.05, while in the second group of 23 patients (with dagger-shaped FTSG; Fig. 4), it was 3.56, which corresponds to a better aesthetic outcome (range: 0, worst to 5, best).
Table I.
Comparison of outcomes between standard graft and dagger-shaped graft groups.
| Standard shaped | Dagger-shaped | p-value | |
|---|---|---|---|
| Number of patients | 20 | 23 | |
| Hand swelling | 55% | 13% | < 0.01* |
| Persistent wrist stiffness | 40% | 17% | 0.099* |
| Scar infection (skin graft healing) | 30% | 0% | < 0.01† |
| Tendon exposure | 25% | 0% | < 0.01† |
| Aesthetic outcome (mean value with Stony Brook Scar Evaluation Scale) | 2.05 ± 0.83 | 3.56 ± 0.79 | < 0.01‡ |
Chi-square test;
Fisher's exact test;
Student's t-test
Fig. 3.
Aesthetic outcome with a standard technique.
Fig. 4.
Aesthetic outcome with the dagger-shaped graft.
Discussion
Donor site complications, reported in the literature by several authors, can be divided into functional and aesthetic problems. The former are caused by skin graft healing in 19-53%, hand swelling in 60%, persistent wrist stiffness in 27%, impaired hand sensation in 17-47%, cold intolerance in 8-40%, reduced hand strength in 40% and partial loss of the graft with exposure of the forearm flexor tendon in 23-55% 5 10-13. Tendon exposure can be caused by the creation of disruptive skin forces under the graft, due to the continuous movement of the forearm tendon 14. Aesthetic complications reported include scar infection, skin tension and hypertrophic scar formation, causing patient dissatisfaction with the aesthetic outcome of the donor site (17-50%) 15. Comorbidities, such as malignancy, tobacco and alcohol abuse, poor nutrition, diabetes and peripheral vascular disease are common in this patient population and may affect wound healing 14.
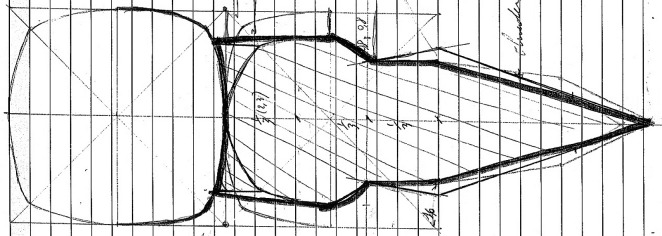
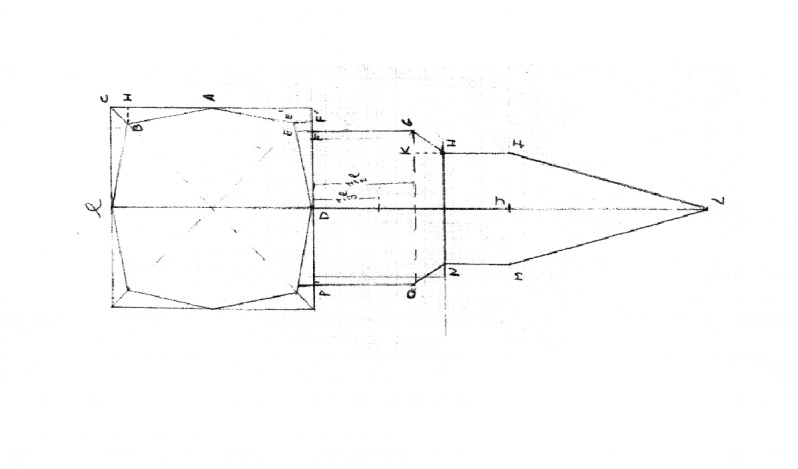
Various methods of reconstruction have been developed to minimize functional and aesthetic morbidity associated with RFFF donor site closure. The techniques include split thickness skin graft (STSG), FTSG and STSG overlying an acellular dermal matrix, although we usually prefer FTSG. Initially in our experience, the forearm donor site was repaired with a standard isosceles triangle of FTSG as described by Liang, and the technical modification proposed by Van Der Lei and Shiba; in detail, we used the V-Y technique with a skin graft shaped like an isosceles triangle whose height was twice the RFFF length in the direction of the forearm axis, and whose width was shorter than half of the forearm circumference 8. However, in some cases of partial detachment of the skin graft due to excessive edge traction was observed. Specifically in the middle portion of the forearm border, there was excessive suture tension due to the fact that a triangle had to replace a rectangular space. Thus, a new shape was proposed. We analysed our previous failures and developed a daggershaped FTSG that reduced border suture tension by creating a precise correspondence between the FTSG and the total donor skin defect that assumed the same geometric shape and saved 8.3% of the skin graft. It is extremely important to place the first seven stitches accurately as shown in Figure 5.
Fig. 5.

(a) Design of the flap with the dagger-shaped FTSG; (b) Preparation of the graft after placement of the first seven stitches; (c) Outcome and comparison with the pre-operative template.
Using the Stony Brook Scar Evaluation Scale, we compared the aesthetic outcomes of the 23 cases who received the dagger-shaped graft with a group of 20 patients who underwent a standard FTSG closure technique. This new scale of cosmetic appearance is composed of five dichotomous categories that include width (> 2 mm), relief/flatness of scar, colour (darker or the same as surrounding skin), presence of suture marks and overall appearance of the scar. The total score is derived by adding the scores (0 or 1) for the presence or absence of these five items. The scar evaluation scale ranges from 0 (worst) to 5 (best). Using the Stony Brook Scale, the group with the dagger-shaped FTSG showed higher overall values because the lesser traction on the graft margins gave a reduction in the width of the wound, a good colour match with the surrounding skin and a flat scar. Unfortunately, suture marks remained unchanged in both groups, while the lesser tension on the edges allowed a lower number of multiple slits cut into the graft. This latter feature decreased the 'meshed effect' of the graft, and accordingly, the overall appearance improved. In detail, the statistical analysis of the two groups showed a significant mean difference (3.56 vs. 2.05; p < 0.01) in favour of the dagger-shaped graft group. Statistical analysis of other features such as hand swelling, tendon exposure and scar infection in skin graft healing also showed a clear improvement in the dagger group (p < 0.01). This is an empirical shape derived from surgical experience. Figure 6 shows the graft template with a side of 2.5 cm, although it should be drawn with larger dimensions. The authors usually prefer a RFFF with a side of 7 cm.
Fig. 6.
Template of the dagger-shaped FTSG.
Conclusions
Our modified V-Y closure method involves the use of a dagger-shaped FTSG for closing the radial forearm free flap donor site with fewer slits in the graft, less complications, better aesthetic results and, consequently, higher patient satisfaction. The technique is recommended for defects smaller than 50 cm2 and is a simple and cost-effective method that avoids harvesting skin grafts from the abdomen or thigh. This change in surgical technique does not lengthen surgical time. However, when the forearm flap width is half of the wrist circumference or larger, a skin graft from a second donor site is mandatory to cover the RFFF defect.
References
- 1.Yang GF, Chen PJ, Gao YZ, et al. Forearm free skin flap transplantation: a report of 56 cases, 1981. Br J Plast Surg. 1997;50:162–165. doi: 10.1016/s0007-1226(97)91363-1. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez-Garcia R, Naval-Gias L, Rodriguez-Campo F, et al. Reconstruction of oromandibular defects by vascularized free flaps: the radial forearm free flap and fibular free flap as major donor sites. J Oral Maxillofac Surg. 2009;67:1473–1477. doi: 10.1016/j.joms.2006.06.286. [DOI] [PubMed] [Google Scholar]
- 3.Karimi A, Mahy P, Reychler H. Closure of radial forearm free flap donor site defect with a local meshed full-thickness skin graft: a retrospective study of an original technique. J Cranio-Maxillofac Surg. 2007;35:369–373. doi: 10.1016/j.jcms.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Moazzam A, Gordon DJ. Cross-suturing as an aid to wound closure: a prospective randomised trial using the forearm flap donor site as a model. Br Ass Plast Surg. 2003;56:695–700. doi: 10.1016/s0007-1226(03)00213-3. [DOI] [PubMed] [Google Scholar]
- 5.Ho T, Couch M, Carson K, et al. Radial forearm free flap donor site outcomes comparison by closure methods. Otolar Head Neck Surg. 2006;134:309–315. doi: 10.1016/j.otohns.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 6.Liang MD, Swartz WM, Jones NF. Local full-thickness skingraft coverage for the radial forearm flap donor site. Plast Reconstr Surg. 1994;93:621–625. [PubMed] [Google Scholar]
- 7.Lei B, Spronk CA, Visscher JGAM. Closure of radial forearm free flap donor site with local full-thickness skin graft. Br J Oral Maxillofac Surg. 1999;37:119–122. doi: 10.1054/bjom.1997.0088. [DOI] [PubMed] [Google Scholar]
- 8.Shiba K, Iida Y, Numata T. Ipsilateral full-thickness forearm skin graft for covering the radial forearm flap donor site. Laryngoscope. 2003;113:1043–1046. doi: 10.1097/00005537-200306000-00023. [DOI] [PubMed] [Google Scholar]
- 9.Singer AJ, Blavantray A, Dagum A, et al. Development and validation of a novel scar evaluation scale. Plast Reconstr Surg. 2007;120:1892–1897. doi: 10.1097/01.prs.0000287275.15511.10. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez-Garcia R, Ruiz-Laza L, Manzano D, et al. Combined local triangular full-thickness skin graft for the closure of the radial forearm free flap donor site: a new technique. J Oral Maxillofac Surg. 2009;67:1562–1567. doi: 10.1016/j.joms.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Avery C, Pereira J, Brown AE. Suprafascial dissection of the radial forearm flap and donor site morbidity. Int J Oral Maxillofac Surg. 2001;30:37–41. doi: 10.1054/ijom.2000.0016. [DOI] [PubMed] [Google Scholar]
- 12.Brown M, Couch M, Huchton D. Assessment of donor-site functional morbidity from radial forearm fasciocutaneous free flap harvest. Arch Otolaryngol Head Neck Surg. 1999;125:1371–1374. doi: 10.1001/archotol.125.12.1371. [DOI] [PubMed] [Google Scholar]
- 13.Chang S, Miller G, Halbert C, et al. Limiting donor site morbidity by suprafascial dissection of the radial forearm flap. Microsurgery. 1996;17:136–140. doi: 10.1002/(SICI)1098-2752(1996)17:3<136::AID-MICR7>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 14.Andrews B, Smith R, Chang C, et al. Management of the radial forearm free flap donor site with the vacuum-assisted closure (VAC) system. Laryngoscope. 2006;116:1918–1922. doi: 10.1097/01.mlg.0000235935.07261.98. [DOI] [PubMed] [Google Scholar]
- 15.Toschka H, Feifel H, Erli HJ, et al. Aesthetic and functional results of harvesting radial forearm flap, especially with regard to hand function. Int J Oral Maxillofac Surg. 2001;30:42–48. doi: 10.1054/ijom.2000.0005. [DOI] [PubMed] [Google Scholar]