Abstract
To investigate the relation between work environmental factors and the risk of major depressive disorder (MDD) over 1 year, the authors conducted a population-based longitudinal study of randomly selected employees in Alberta, Canada (January 2008 to November 2011). Participants without a current or lifetime diagnosis of MDD at baseline (n = 2,752) were followed for 1 year. MDD was assessed using the World Health Organization’s Composite International Diagnostic Interview-Auto 2.1. The overall 1-year incidence of MDD was 3.6% (95% confidence interval: 2.8, 4.6); it was 2.9% (95% confidence interval: 1.9, 4.2) in men and 4.5% (95% confidence interval: 3.3, 6.2) in women. The relations between work environmental factors and MDD differed by sex. In men, high job strain increased the risk of MDD in those who worked 35–40 hours per week; job insecurity and family-to-work conflict were predictive of MDD. Women who worked 35–40 hours per week and reported job insecurity, a high effort-reward imbalance, and work-to-family conflict were at a higher risk of developing MDD. Job strain, effort-reward imbalance, job insecurity, and work-to-family conflicts are important risk factors for the onset of MDD and should be targets of primary prevention. However, these work environmental factors appear to operate differently in men and in women.
Keywords: effort-reward imbalance, incidence, job strain, longitudinal study, major depressive disorder, population-based
Major depression is a significant public health and societal issue. It imposes considerable burden on health care systems and employers and negatively affects people’s quality of life and productivity (1–5). In recent decades, there have been an increasing number of studies indicating that work environmental factors might precipitate the onset of major depression (1, 6–11).
In general occupational health research, 3 theoretical models have been widely used: the demand-control model (12), the effort-reward imbalance (ERI) model (13), and the work-to-family conflicts model (14). The demand-control model posits that negative health outcomes, such as fatigue, depression, and other physical illnesses, result from situations in which one’s control over one’s work is low and the psychological demands imposed by one’s work are high (12). Large longitudinal studies have shown that high job strain is associated with an increased risk of psychiatric syndromes (7, 8) and major depression (10, 11, 15). However, research has shown that not all of the domains of the demand-control model are associated with mental disorders, and some domains seem to affect men and women differently in terms of the risk of mental disorders (7, 15). Using national data from Canada, Wang et al. (16) found that a combination of high demand and low control at work was associated major depression in men but not in women. The ERI model assumes that the experience of a lack of reciprocity in terms of high costs and low gains elicits negative emotions in exposed people (13). Feelings of not being appreciated in an adequate way and disappointments resulting from inappropriate rewards are paralleled by sustained strain reactions in the autonomic nervous system (13). Strong associations between ERI and depressive symptoms have been found in cross-sectional (17–20) and longitudinal (21–23) studies.
Because of the increasing rate of participation by women in the labor force and of men in family roles, there has been considerable research interest in the work-to-family interface and how it affects workers’ health. Work-to-family conflict occurs when efforts to fulfill the demands of the employee role interfere with the ability to fulfill the demands of the roles of spouse, parent, or care provider (14). Conversely, family-to-work conflict may be an obstacle to successfully meeting work-related demands and responsibilities (14). As both employee and family roles represent core components of adult identity, impediments to work- and family-related identity formation and maintenance are likely to be experienced as stressful. Therefore, work-to-family conflicts can be an important risk factor for major depression. Because men’s identities may be tied more closely to their role at work than women’s (24), work-to-family conflict may affect women more than men, whereas family-to-work conflict may affect men more than women.
Although longitudinal studies have found that high job strain is associated with the risk of psychiatric syndromes (7, 8) and major depression (10, 11, 15), the common weakness of these studies is that depression was not assessed using a high-quality diagnostic interview based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (25). These studies were not able to completely exclude people with major depressive episodes that occurred before the baseline assessment, which made the temporal relation between job strain and depression unclear. Another weakness is that an abbreviated version of the Job Content Questionnaire (JCQ) (12) was used. To our knowledge, validated instruments that measure ERI (13), demand-control ratios (12), and work-to-family conflicts (14, 26) have not been simultaneously used in population-based longitudinal studies that assessed major depression. Therefore, research has not been able to clearly demonstrate the relations between work environmental factors and major depression. Furthermore, given the sex differences in family roles and nature of work, the complex relations between workplace factors and major depression need to be examined in both men and women. The objectives of the present analysis were to investigate the relations between work environmental factors and the 1-year risk of major depressive disorder (MDD) and to examine whether the work environmental factors associated with the risk of MDD differ by sex.
MATERIALS AND METHODS
In January 2008, we started building a longitudinal cohort from the working population of the province of Alberta, Canada. The primary employers in the province are the oil and gas industry, the service industry, and the government, the 3 industries from which 66.9% of our participants were selected. The target population of the study included employees who were between 25 and 65 years of age and who were residing in Alberta at the time of the baseline survey (T0). The participants were recruited using random digit dialing. At the recruitment stage, 9,776 potentially eligible individuals were reached by telephone. These individuals were read a script that indicated that they could be considered eligible only if they were between the ages of 25 and 64 years, were currently working and residing in Alberta, would agree to be contacted for 2 annual follow-up interviews (through 2011), and would provide primary and secondary contact information. At the end of recruitment, 4,302 eligible participants completed the baseline interviews. Among the 4,302 participants, there were 3 duplications and 60 people who did not provide their names. They were excluded from the cohort, leaving 4,239 baseline participants in the cohort. As of the 12-month interview (T1), 3,280 (77%) were successfully followed. In the present analysis, participants who were free of current and lifetime MDD at T0 were included (n = 2,752).
The baseline assessment involved 2 stages. The first stage included sampling, recruitment, and screening for mental disorders. In the screening section, participants were asked the stem questions about mental disorders in the World Health Organization’s Composite International Diagnostic Interview (CIDI), which was the diagnostic instrument we used. At the second stage, participants who screened positive for mental disorders were selected for structured diagnostic interviews using the CIDI. At both stages, data were collected by trained interviewers using the computer-assisted telephone interview method. The same screening and diagnostic procedures were used in the follow-up interviews. Detailed information about the study design and recruitment has been published previously (5, 27). This study was approved by Conjoint Health Research Ethics Board of the University of Calgary.
Assessment of psychiatric disorders
The CIDI-Auto 2.1 (28) was administered to participants who screened positive for MDD, manic episodes, dysthymia, social phobia, panic disorder, or generalized anxiety disorder (e.g., participants who answered “yes” to any of the stem questions for these disorders). The lay interviewers who administered the CIDI-Auto 2.1 were recruited and trained by team members (J. L. W. and S. P.). The CIDI-Auto 2.1 is a computerized program developed and supported by the World Health Organization’s training center in Australia. After the completion of the interview, the scoring algorithm program in the CIDI-Auto 2.1 automatically generated diagnoses based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (25). The lifetime version of the CIDI-Auto 2.1 was used at T0 to assess MDD, manic episodes, dysthymia, social phobia, panic disorder, and generalized anxiety disorder in participants’ lifetimes. At T1, the 12-month version of the CIDI-Auto 2.1 was used to determine whether these mental disorders had occurred in the past 12 months.
Assessment of work environmental factors
The JCQ (12) was used to assess 5 dimensions of work stress: decision latitude (3 items), skill discretion (6 items), psychological demand (5 items), job security (3 items), and social support from supervisors and coworkers (8 items). For each question, there were 4 possible answers: strongly disagree, disagree, agree, and strongly agree. Each answer was scored on a scale of 1 (strongly disagree) to 4 (strongly agree). Reversed coding for some items was used. The dimensional scores were calculated using the formula provided in the JCQ manual (12). In the present study, the internal consistency (Cronbach’s α) values for the 5 subscales were 0.72, 0.71, 0.67, 0.52, and 0.85, respectively. The moderate internal consistency does not necessarily mean that the JCQ subscales were insensitive. A moderate internal consistency might indicate that there is no redundancy in the measurement and that each item adds new information to the measure (29). If an instrument covers several dimensions, it is reasonable to expect a moderate internal consistency (30). Higher scores on the JCQ scales indicate more job stress. We used the scores of psychological demand, skill discretion, and decision authority to compute a job strain ratio (JSR) using the equation JSR = psychological demand/[(skill discretion + decision authority)/2], which was based on the formula used by Statistics Canada (the Canadian federal statistics agency) (31). As reflected by the formula, demand exceeds control when JSR scores increase.
Determination of ERI focused on 2 elements: perceived effort (5 items) and rewards (11 items). The imbalance between effort and reward was determined by a ratio according to the formula provided by the developers (13). A higher ERI ratio indicated a higher level of imbalance. In the present study, the Cronbach’s α values of the effort and rewards scales were 0.79 and 0.80, respectively.
Other variables included sex, age (continuous variable), marital status (married/common-law partnership, single/never married, or separated/divorced/widowed), educational level (less than high school, high school and college, or university), personal annual income (<$30,000, $30,000–$59,999, $60,000–$79,999, or ≥$80,000 in Canadian dollars), average weekly number of working hours (≤35 hours, 35.5–40 hours, or ≥40.5 hours), job type (full-time, part-time, or other), job gradient (ordinary worker, supervisor, or manager/executive), and work-to-family conflicts.
Work-to-family conflicts were assessed using an 8-item work-to-family conflict scale (26). The work-to-family conflict questionnaire included separate scales for work-to-family conflict and family-to-work conflict (26), each of which contained 4 questions. Each question assessed potential conflict and had 3 possible answers: not at all, to some extent, and a great deal. Each subscale had a possible summary score that ranged from 4 to 12. The Cronbach’s α values of the 2 subscales were 0.56 and 0.73, respectively. Both work-to-family conflict and family-to-work conflict scores were highly skewed. To make meaningful comparisons, the scores were dichotomized by median values.
Statistical analysis
To be consistent with previous research (10), for this analysis, we defined the ratios of job strain and effort-reward that were over the 75th percentile values as high job strain and high ERI. As a preliminary analysis, we examined the distribution of the incidence of MDD by the quartiles of JSR and ERI (Figures 1 and 2).
Figure 1.
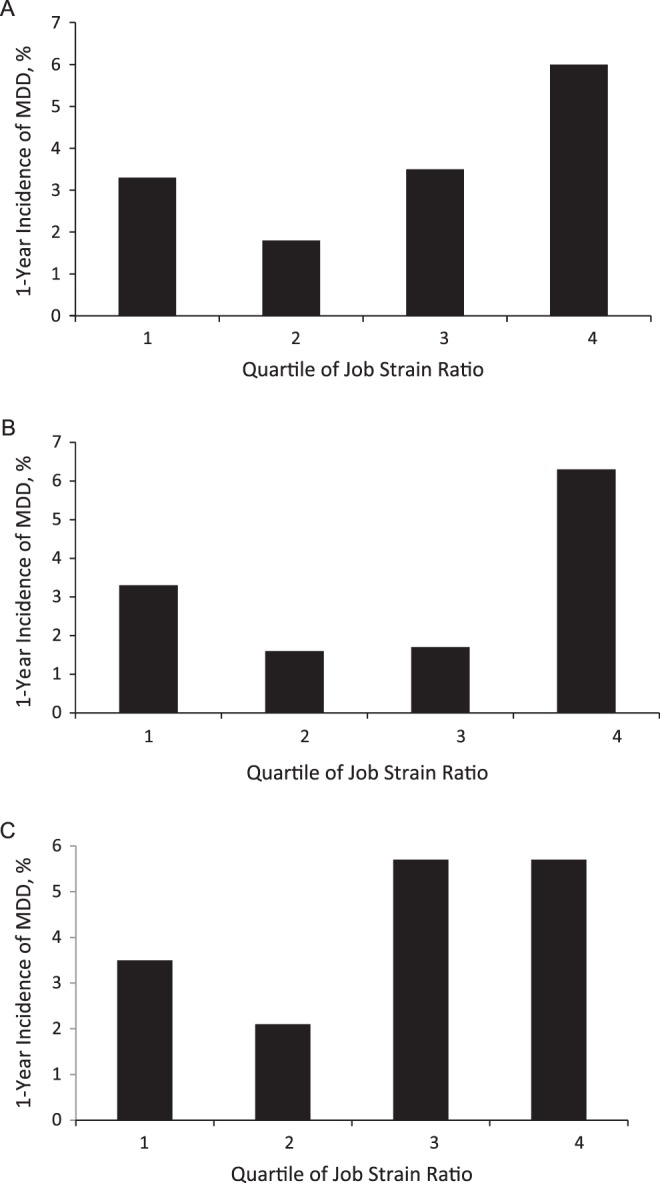
One-year incidence of major depressive disorder (MDD) according to quartile of job strain ratio, overall (A), in men (B), and in women (C), Alberta, Canada, 2008–2011. The overall incidence proportions for quartiles 1–4 were 3.3 (95% confidence interval (CI): 2.1, 5.4), 1.8 (95% CI: 1.0, 3.4), 3.5 (95% CI: 2.1, 5.8), and 6.0 (95% CI: 3.8, 9.2), respectively. In men, the incidence proportions for quartiles 1–4 were 3.3 (95% CI: 1.7, 6.9), 1.6 (95% CI: 0.7, 3.9), 1.7 (95% CI: 0.7, 4.3), and 6.3 (95% CI: 3.0, 12.7), respectively. In women, the incidence proportions for quartiles 1–4 were 3.5 (95% CI: 1.6, 7.5), 2.1 (95% CI: 0.9, 5.2), 5.7 (95% CI: 3.1, 10.0), and 5.7 (95% CI: 3.3, 9.6), respectively.
Figure 2.
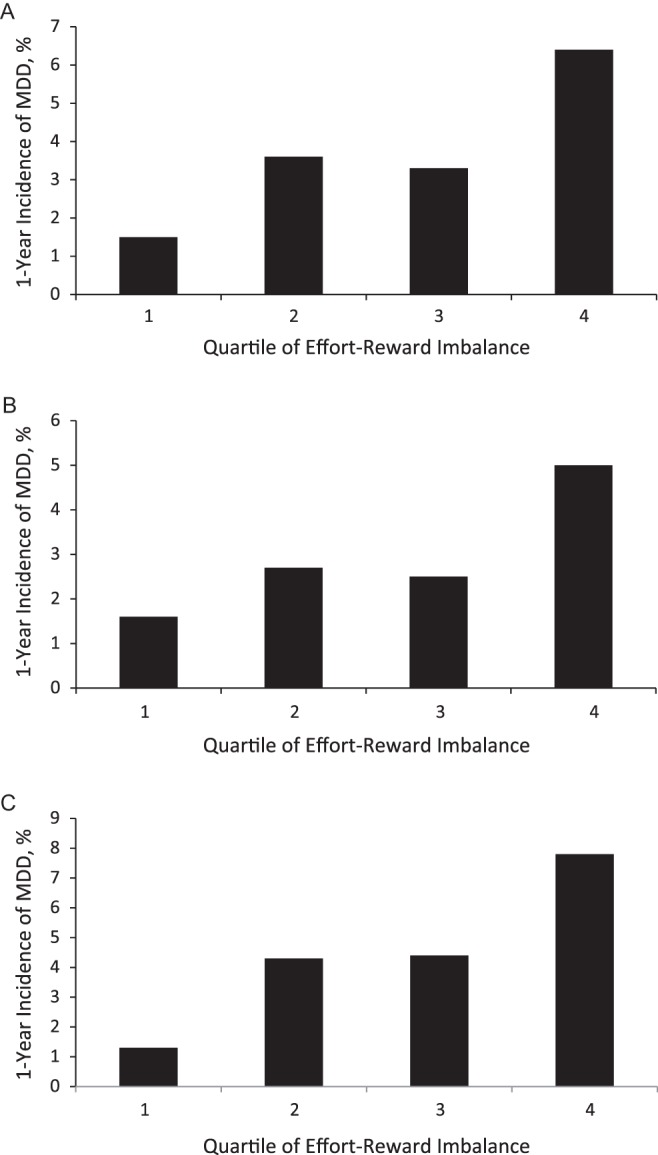
One-year incidence of major depressive disorder (MDD) according to quartile of effort-reward imbalance, overall (A), in men (B), and in women (C), Alberta, Canada, 2008–2011. The overall incidence proportions for quartiles 1–4 were 1.5 (95% confidence interval (CI): 0.8, 2.9), 3.6 (95% CI: 2.1, 5.6), 3.3 (95% CI: 1.9, 5.7), and 6.4 (95% CI: 6.3, 9.4), respectively. In men, the incidence proportions for quartiles 1–4 were 1.6 (95% CI: 0.7, 3.9), 2.7 (95% CI: 1.3, 5.7), 2.5 (95% CI: 1.0, 6.0), and 5 (95% CI: 2.6, 9.2), respectively. In women, the incidence proportions for quartiles 1–4 were 1.3 (95% CI: 0.5, 3.6), 4.3 (95% CI: 2.3, 7.8), 4.4 (95% CI: 2.2, 8.6), and 7.8 (95% CI: 4.7, 12.6), respectively.
We estimated the 1-year incidence of MDD overall and by sex among participants who had no lifetime or current MDD at T0. Bivariate analyses were conducted to identify baseline factors associated with the new onset of MDD. Logistic regression modeling was performed to examine potential effect modification factors between work environmental factors and other variables in relation to the risk of MDD. The sex-specific associations between baseline exposure variables and new onset of MDD were estimated as odds ratios and associated 95% confidence intervals. Significant demographic, socioeconomic, other work environmental, and clinical factors identified in bivariate analyses were included in multivariate logistic regression modeling as potential confounders. We decided whether to retain factors in the model based on the significance of the factors in the model and how a variable affected the model’s goodness of fit.
Sampling weights were used in proportion estimations and regression modeling, accounting for the effects of number of telephone lines in the household and sex and age distributions in Albertans who were working and who were between the ages of 25 and 65 years based on the 2006 census data collected by Statistics Canada. Over the follow-up period, some participants refused further participation and some were unable to be contacted after the baseline assessment. We compared the persons who refused, those we were unable to contact, and those who were successfully followed. There were no differences between the persons who refused and the participants in baseline demographic and socioeconomic characteristics or in the prevalence of mental disorders at T0 (32). The final weights were the product of poststratification weights and the weights that accounted for attrition. All percentages and the results of logistic regression were weighted. The analysis was conducted using Stata, version 10.0 (33). Because sampling weights were used the analyses, traditional tests for goodness of fit could not be used. We used the Stata syntax svylogitgof, which is an F-adjusted mean residual test, to assess the goodness of fit of a model.
RESULTS
Of the 2,752 participants without a current or lifetime diagnosis of MDD at T0, 2,254 (81%) provided information about MDD at T1 and 70 had developed MDD over the follow-up period. The weighted 1-year incidence of MDD was 3.6% (95% confidence interval: 2.8, 4.6). It was 2.9% (95% confidence interval: 1.9, 4.2) in men and 4.5% (95% confidence interval: 3.3, 6.2) in women. The demographic, socioeconomic, work environmental, and clinical characteristics of the participants are listed in Table 1.
Table 1.
Baseline Demographic, Socioeconomic, Work Environmental, and Clinical Characteristics of the Participants Without a Major Depressive Disorder (n = 2,752), Alberta, Canada, 2008–2011
| Variable | Weighted % | ||
| Overall | Men | Women | |
| Men | 56.2 | ||
| Women | 43.8 | ||
| Age (mean (SD)) | 42.6 (0.21) | 42.4 (0.30) | 42.8 (0.29) |
| Marital status | |||
| Married or common-law partnership | 75.9 | 79.1 | 71.8 |
| Single | 14.3 | 13.6 | 15.3 |
| Separated, divorced, or widowed | 9.8 | 7.3 | 12.9 |
| Educational level | |||
| Less than high school | 5.1 | 6.4 | 3.4 |
| High school and college | 59.1 | 61.1 | 56.5 |
| University | 35.8 | 32.5 | 40.1 |
| Personal income, Can$ | |||
| <30,000 | 10.0 | 3.4 | 18.5 |
| 30,000–59,999 | 35.4 | 27.3 | 45.8 |
| 60,000–79,999 | 21.6 | 22.9 | 20.0 |
| ≥80,000 | 33.0 | 46.4 | 15.7 |
| Job type | |||
| Full-time work | 83.9 | 93.2 | 72.0 |
| Part-time or other | 16.1 | 6.8 | 28.0 |
| Job grade | |||
| Manager/executive | 18.9 | 22.4 | 14.5 |
| Supervisor | 19.2 | 22.6 | 14.9 |
| Other | 61.9 | 55.0 | 70.7 |
| No. of weekly working hours | |||
| ≤35 | 18.0 | 6.0 | 33.4 |
| 35.5–40 | 43.9 | 42.5 | 45.8 |
| ≥40.5 | 38.1 | 51.5 | 20.8 |
| Fourth quartile of job strain ratio | 21.3 | 16.6 | 27.3 |
| Job insecurity | 20.9 | 21.9 | 19.6 |
| Stress in supervisor support | 16.7 | 15.0 | 17.5 |
| Stress in coworker support | 19.8 | 22.2 | 16.7 |
| Fourth quartile of effort-reward imbalance | 24.1 | 22.0 | 26.7 |
| Work-to-family conflict | 29.3 | 33.2 | 24.3 |
| Family-to-work conflict | 26.3 | 25.6 | 27.2 |
| Any anxiety disorders | 3.7 | 2.5 | 5.2 |
Abbreviation: SD, standard deviation.
We examined the relations between the incidence of MDD and JSR (Figure 1) and MDD and ERI (Figure 2) by quartiles, overall and by sex. It appeared that participants in the first and the last JSR quartiles had a higher risk of MDD than did persons in the second and third quartiles (P = 0.02). This pattern was observed in men (P = 0.03), but in women, the difference was not significant (P = 0.2). The incidence of MDD increased with an increase in ERI, with the incidence of MDD the highest in participants in the last quartile (P = 0.001). The same trend was observed in women (P = 0.01); however, in men, the difference was not statistically significant. The results supported our decision to classify JSR and ERI relative to the 75th percentile values.
The crude associations between included variables and MDD overall and by sex are in Table 2. Age, marital status, job type, job grade, and comorbid anxiety disorders were not associated with the risk of MDD. We included all significant variables in the bivariate analysis in the same model. The results are shown in Table 3 (under model 1). In that model, only high ERI, job insecurity, and family-to-work conflict were associated with MDD. Using the repeated model fitting procedures described in the Materials and Methods section, we found that working 35–40 hours per week and having high levels of ERI, job insecurity, and family-to-work conflict were significant factors, and we therefore retained them in the model. Statistical tests showed that the both models had a good fit with the data (model 1, P = 0.41; model 2 = 1.09, P = 0.37).
Table 2.
Crude Associations Between Baseline Demographic, Socioeconomic, Work Environmental, and Clinical Variables and the Risk of Major Depressive Disorder in Participants Without a Major Depressive Disorder at Baseline (n = 2,752), Alberta, Canada, 2008–2011
| Variable | Overall | Men | Women | |||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age (continuous variable) | 0.99 | 0.96, 1.02 | 0.99 | 0.94, 1.03 | 1.00 | 0.96, 1.04 |
| Unmarried | 1.24 | 0.69, 2.25 | 1.71 | 0.68, 4.44 | 0.89 | 0.41, 1.91 |
| Less than a university education | 1.85 | 1.03, 3.35 | 1.54 | 0.61, 3.88 | 2.31 | 1.07, 4.96 |
| Personal income less than Can$ 60,000 | 1.95 | 1.15, 3.32 | 2.24 | 1.00, 5.06 | 1.47 | 0.68, 3.21 |
| Part-time work and other jobs | 0.48 | 0.22, 1.04 | 0.85 | 0.19, 3.76 | 0.30 | 0.12, 0.76 |
| Ordinary employees | 0.83 | 0.49, 1.40 | 0.70 | 0.31, 1.58 | 0.82 | 0.39, 1.73 |
| Working 35–40 hours/week | 2.06 | 1.24, 3.43 | 1.12 | 0.50, 2.55 | 3.51 | 1.73, 7.08 |
| Fourth quartile of job strain ratio | 2.12 | 1.21, 3.71 | 2.97 | 1.22, 7.23 | 1.49 | 0.73, 3.03 |
| Job insecurity | 2.99 | 1.66, 5.39 | 3.47 | 1.46, 8.25 | 2.61 | 1.17, 5.83 |
| Stress in supervisor support | 2.36 | 1.30, 4.26 | 1.73 | 0.68, 4.42 | 2.86 | 1.31, 6.20 |
| Stress in coworker support | 1.93 | 1.02, 3.64 | 1.74 | 0.64, 4.73 | 2.18 | 0.96, 4.94 |
| Fourth quartile of effort-reward imbalance | 2.44 | 1.44, 4.16 | 2.24 | 0.98, 5.13 | 2.50 | 1.26, 4.96 |
| Work-to-family conflict | 1.78 | 1.05, 3.01 | 1.25 | 0.55, 2.86 | 2.71 | 1.37, 5.38 |
| Family-to-work conflict | 2.10 | 1.24, 3.55 | 2.31 | 1.04, 5.15 | 1.90 | 0.95, 3.82 |
| Any anxiety disorders | 2.44 | 0.92, 6.45 | 1.76 | 0.22, 14.04 | 2.35 | 0.77, 7.15 |
Abbreviations: CI, confidence interval; OR: odds ratio.
Table 3.
Results of Multivariate Logistic Regression of Baseline Factors Associated With the Risk of Major Depressive Disorder, Alberta, Canada, 2008–2011
| Variable | Model 1 | Model 2 | ||
| OR | 95% CI | OR | 95% CI | |
| Less than a university education | 2.20 | 0.98, 4.95 | ||
| Personal income less than Can$ 60,000 | 1.42 | 0.80, 2.51 | ||
| High job strain | 1.33 | 0.65, 2.75 | ||
| High stress in supervisor support | 1.18 | 0.54, 2.56 | ||
| High stress in coworker support | 1.49 | 0.74, 2.98 | ||
| Working 35–40 hours/week | 1.65 | 0.88, 3.08 | 2.14 | 1.18, 3.86 |
| High effort-reward imbalance | 2.32 | 1.14, 4.73 | 2.58 | 1.40, 4.76 |
| Job insecurity | 2.11 | 1.07, 4.15 | 2.67 | 1.46, 4.88 |
| Family-to-work conflict | 2.15 | 1.11, 4.18 | 1.94 | 1.06, 3.54 |
| Goodness to fit in the model | ||||
| F-adjusted mean residual test | 1.03 | 1.09 | ||
| P value | 0.41 | 0.37 | ||
Abbreviations: CI: confidence interval; OR, odds ratio.
We found an effect modification between JSR and weekly working hours in men (Table 4). High JSR was not associated with MDD in participants who worked 35 hours or fewer per week or those who worked more than 40 hours per week. In men who worked between 35 and 40 hours per week, those who reported a high JSR had a higher risk of MDD than did others (11.0% vs. 1.5%, P = 0.0002). In the final model that included the interaction term, job insecurity and family-to-work conflict were significant factors for MDD in men. Personal income was marginally associated with MDD, but the association was not statistically significant at the level of 0.05. In women, a multivariate logistic regression model showed that working 35–40 hours per week and having high levels of ERI, job insecurity, and work-to-family conflict were significantly associated with MDD (Table 4).
Table 4.
Multivariate Analysis of Baseline Factors Associated With Major Depressive Disorder in Men and in Women, Alberta, Canada, 2008–2011
| Variables | Men | Women | ||
| OR | 95% CI | OR | 95% CI | |
| Working 35–40 hours/week | 0.48 | 0.15, 1.54 | 3.50 | 1.52, 8.06 |
| High job strain | 0.57 | 0.12, 2.79 | ||
| High effort-reward imbalance | 2.35 | 1.04, 5.30 | ||
| Job insecurity | 2.91 | 1.27, 6.70 | 2.29 | 1.05, 4.99 |
| Work-to-family conflict | 2.67 | 1.14, 6.25 | ||
| Family-to-work conflict | 2.53 | 1.07, 5.99 | ||
| Annual personal income, Can$ | ||||
| 30,000–59,999 | 0.37 | 0.08, 1.82 | ||
| 60,000–79,999 | 0.21 | 0.04, 1.28 | ||
| ≥80,000 | 0.22 | 0.04, 1.05 | ||
| Job strain × working hours | 14.07 | 1.87, 105.66 | ||
| Goodness of fit of the model | ||||
| F-adjusted mean residual test | 1.18 | 1.31 | ||
| P value | 0.31 | 0.23 | ||
Abbreviations: CI, confidence interval; OR, odds ratio.
DISCUSSION
To our knowledge, this was the first population-based longitudinal study that incorporated 3 widely used occupational health models and assessed MDD using a structured diagnostic interview. With a large sample, we were able to investigate the relations between the 3 models and the risk of MDD in men and women. We found that JSR, ERI, and work-to-family conflicts might affect the risk of MDD through different mechanisms. The relation between JSR and MDD was not linear and varied by sex. Similarly, there was a sex difference in the relation between ERI and the risk of MDD. High JSR, low job security, and family-to-work conflict lead to a higher risk of MDD in men. In women, working 35–40 hours per week and having high levels of ERI, job insecurity, and work-to-family conflict were the risk factors for the onset of MDD.
To our knowledge, the Netherlands Mental Health Survey and Incidence Study (NEMESIS) is the only population-based study that estimated the 1-year incidence of major depression (34). Our results showed a relatively higher incidence of MDD than that from the NEMESIS (3.6% vs. 2.7%). The sex-specific incidence of MDD was also higher than the NEMESIS results (2.9% vs. 1.7% in men; 4.5% vs. 3.9% in women). The discrepancies may be due to different populations and study times. The NEMESIS data were collected more than 10 years ago. Our longitudinal data were collected from 2008 to 2011. Additionally, the present study was conducted in the course of a global economic crisis that might have specifically affected the mental health of the working population (27).
Improved work environment and reduced job strain have been advocated as options for the primary prevention of mental health problems in workplaces. The results of the present study offer information relevant to this strategy. High job strain is a risk factor for MDD in men, especially in men who work 35–40 hours per week (42% of the men in this study). However, men in the very low JSR category seemed to have a relatively higher risk of MDD than those in the moderate JSR category. This suggests that men may benefit from having a moderate level of job strain in terms of the risk of MDD. It is not clear why men in the lowest JSR category had a higher risk of MDD than did those with a moderate level of JSR. It might be due to health selection, meaning that individuals who were at a high risk of mental health problems moved to low-demand jobs later in their lives (35).
The trends of MDD by levels of ERI appeared to be same in men and women. However, women in the third JSR quartile seemed to have a risk of MDD similar to that of women in the fourth quartile. This suggested that the threshold for high JSR in terms of the risk of MDD might be lower for women than for men. This may partly explain why JSR was not a significant factor for MDD in a multivariate analysis in women. More studies are needed to examine this finding.
Using a more advanced instrument for determining work-to-family conflicts in this study, we found that women were affected by work-to-family conflict and men were affected by family-to-work conflict in terms of the risk of MDD. This result indicates that sex and family roles may play an important role in the risk of MDD and that men and women might view work and family differently. Achievements at work may be a stronger part of identity formation for men (24).
The present study had several additional limitations. First, data collection relied on self-reporting. Therefore, both reporting and recall biases were possible. Second, approximately 19% of participants in the cohort did not provide information about MDD at the follow-up interviews. Although the data were weighted to account for the effects of baseline personal income and mental disorders that were related to being unable to be contacted, there may be some unmeasured characteristics that made the relations between work environmental factors and MDD differ in those with missing data about MDD and those without missing data and that were not accounted for in the weighting procedures. At the recruitment stage, we applied strict inclusion criteria for the cohort. Approximately 56% of potentially eligible participants refused to participate in the cohort. However, the current analysis was longitudinal, so selection bias was related to attrition. Given the good response rate in the follow-up and the use of weights, we believe that selection bias did not significantly affect the results. Third, the etiology of major depression is complex and multifactorial. The risk of developing major depression may be related to many factors, including chronic medical conditions, family history, help-seeking behaviors, types of work, and negative life events. These factors may confound the association between job stress and major depression. Unfortunately, collecting data related to all confounding factors is not possible in a telephone-based study. Future studies with sufficient resources and similar study designs should consider collecting information on these variables. Fourth, although participants with lifetime MDD at baseline were excluded from the analysis, some people with minor depression may have been included. The perception of the work environment could be affected by depressive symptoms, leading to confounding. On the other hand, minor depression at baseline could be the result of a negative work environment, meaning that minor depression may become part of a causal chain linking work environmental factors and MDD. Fifth, the 95% confidence intervals associated with some estimates were wide, which indicates that the statistical power in certain analyses was not sufficient. Additionally, we could not estimate and compare the risk of MDD among those with changes in work environmental factors because of the small number of MDD cases. Longitudinal studies with a larger sample size are needed. Finally, this study was conducted in a cohort recruited in Alberta, Canada. Caution should be used when generalizing these results to other populations.
High JSR and ERI are common in workplaces and can contribute to the risk of MDD. However, the mechanisms may differ by sex. These sex-specific relations between work environmental factors and MDD need to be replicated by future studies. Future studies with large sample sizes should also examine how changes in work environment affect the risk of MDD. These may assist in the development of preventive strategies.
Acknowledgments
Author affiliations: Department of Psychiatry, Faculty of Medicine, University of Calgary, Calgary, Alberta, Canada (JianLi Wang); Department of Community Health Sciences, Faculty of Medicine, University of Calgary, Calgary, Alberta, Canada (JianLi Wang, Scott B. Patten); Department of Psychiatry, Faculty of Medicine, University of Calgary, Calgary, Alberta, Canada (Scott B. Patten); Mental Health Information and Evaluation Unit, Mental Health Program, Alberta Health Services, Calgary, Alberta, Canada (Shawn Currie); Department of Psychiatry, Faculty of Medicine, University of Manitoba, Winnipeg, Manitoba, Canada (Jitender Sareen); and Department of Psychiatry, Faculty of Medicine, McGill University, Montreal, Quebec, Canada (Norbert Schmitz).
This study was funded by operating grants from the Canadian Institutes of Health Research (Principal Investigator: JianLi Wang).
Conflict of interest: none declared.
Glossary
Abbreviations
- CIDI
Composite International Diagnostic Interview
- ERI
effort-reward imbalance
- JCQ
Job Content Questionnaire
- JSR
job strain ratio
- MDD
major depressive disorder
- NEMESIS
Netherlands Mental Health Survey and Incidence Study
References
- 1.Dewa CS. Mental illness and the workplace: a national concern. Can J Psychiatry. 2007;52(6):337–338. doi: 10.1177/070674370705200601. [DOI] [PubMed] [Google Scholar]
- 2.Dewa CS, Chau N, Dermer S. Examining the comparative incidence and costs of physical and mental health-related disabilities in an employed population. J Occup Environ Med. 2010;52(7):758–762. doi: 10.1097/JOM.0b013e3181e8cfb5. [DOI] [PubMed] [Google Scholar]
- 3.Stewart WF, Ricci JA, Chee E, et al. Cost of lost productive work time among US workers with depression. JAMA. 2003;289(23):3135–3144. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 4.Ustün TB, Kessler RC. Global burden of depressive disorders: the issue of duration. Br J Psychiatry. 2002;181(3):181–183. doi: 10.1192/bjp.181.3.181. [DOI] [PubMed] [Google Scholar]
- 5.Wang J, Schmitz N, Smailes E, et al. Workplace characteristics, depression, and health-related presenteeism in a general population sample. J Occup Environ Med. 2010;52(8):836–842. doi: 10.1097/JOM.0b013e3181ed3d80. [DOI] [PubMed] [Google Scholar]
- 6.Blackmore ER, Stansfeld SA, Weller I, et al. Major depressive episodes and work stress: results from a national population survey. Am J Public Health. 2007;97(11):2088–2093. doi: 10.2105/AJPH.2006.104406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stansfeld SA, Fuhrer R, Head J, et al. Work and psychiatric disorder in the Whitehall II Study. J Psychosom Res. 1997;43(1):73–81. doi: 10.1016/s0022-3999(97)00001-9. [DOI] [PubMed] [Google Scholar]
- 8.Stansfeld SA, Fuhrer R, Shipley MJ, et al. Work characteristics predict psychiatric disorder: prospective results from the Whitehall II Study. Occup Environ Med. 1999;56(5):302–307. doi: 10.1136/oem.56.5.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang J, Patten SB. Perceived work stress and major depression in the Canadian employed population, 20–49 years old. J Occup Health Psychol. 2001;6(4):283–289. doi: 10.1037//1076-8998.6.4.283. [DOI] [PubMed] [Google Scholar]
- 10.Wang J. Work stress as a risk factor for major depressive episode(s) Psychol Med. 2005;35(6):865–871. doi: 10.1017/s0033291704003241. [DOI] [PubMed] [Google Scholar]
- 11.Wang J, Schmitz N, Dewa C, et al. Changes in perceived job strain and the risk of major depression: results from a population-based longitudinal study. Am J Epidemiol. 2009;169(9):1085–1091. doi: 10.1093/aje/kwp037. [DOI] [PubMed] [Google Scholar]
- 12.Karasek R, Brisson C, Kawakami N, et al. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 13.Siegrist J, Starke D, Chandola T, et al. The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med. 2004;58(8):1483–1499. doi: 10.1016/S0277-9536(03)00351-4. [DOI] [PubMed] [Google Scholar]
- 14.Frone MR. Work-family conflict and employee psychiatric disorders: the National Comorbidity Survey. J Appl Psychol. 2000;85(6):888–895. doi: 10.1037/0021-9010.85.6.888. [DOI] [PubMed] [Google Scholar]
- 15.Wang J. Perceived work stress and major depressive episodes in a population of employed Canadians over 18 years old. J Nerv Ment Dis. 2004;192(2):160–163. doi: 10.1097/01.nmd.0000110242.97744.bc. [DOI] [PubMed] [Google Scholar]
- 16.Wang JL, Lesage A, Schmitz N, et al. The relationship between work stress and mental disorders in men and women: findings from a population-based study. J Epidemiol Community Health. 2008;62(1):42–47. doi: 10.1136/jech.2006.050591. [DOI] [PubMed] [Google Scholar]
- 17.Wang JL, Sareen J, Smailes E, et al. Three job-related stress models and depression: a population-based study. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):185–193. doi: 10.1007/s00127-011-0340-5. [DOI] [PubMed] [Google Scholar]
- 18.Tsutsumi A, Kayaba K, Theorell T, et al. Association between job stress and depression among Japanese employees threatened by job loss in a comparison between two complementary job-stress models. Scand J Work Environ Health. 2001;27(2):146–153. doi: 10.5271/sjweh.602. [DOI] [PubMed] [Google Scholar]
- 19.Pikhart H, Bobak M, Pajak A, et al. Psychosocial factors at work and depression in three countries of Central and Eastern Europe. Soc Sci Med. 2004;58(8):1475–1482. doi: 10.1016/S0277-9536(03)00350-2. [DOI] [PubMed] [Google Scholar]
- 20.Chandola T, Marmot M, Siegrist J. Failed reciprocity in close social relationships and health: findings from the Whitehall II Study. J Psychosom Res. 2007;63(4):403–411. doi: 10.1016/j.jpsychores.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inoue M, Tsurugano S, Yano E. Job stress and mental health of permanent and fixed-term workers measured by effort-reward imbalance model, depressive complaints, and clinic utilization. J Occup Health. 2011;53(2):93–101. doi: 10.1539/joh.l10098. [DOI] [PubMed] [Google Scholar]
- 22.Godin I, Kittel F, Coppieters Y, et al. A prospective study of cumulative job stress in relation to mental health. BMC Public Health. 2005;5(1):67. doi: 10.1186/1471-2458-5-67. (doi:10.1186/1471-2458-5-67) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kivimäki M, Vahtera J, Elovainio M, et al. Effort-reward imbalance, procedural injustice and relational injustice as psychosocial predictors of health: complementary or redundant models? Occup Environ Med. 2007;64(10):659–665. doi: 10.1136/oem.2006.031310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Griffin JM, Fuhrer R, Stansfeld SA, et al. The importance of low control at work and home on depression and anxiety: do these effects vary by gender and social class? Soc Sci Med. 2002;54(5):783–798. doi: 10.1016/s0277-9536(01)00109-5. [DOI] [PubMed] [Google Scholar]
- 25.Chandola T, Martikainen P, Bartley M, et al. Does conflict between home and work explain the effect of multiple roles on mental health? A comparative study of Finland, Japan, and the UK. Int J Epidemiol. 2004;33(4):884–893. doi: 10.1093/ije/dyh155. [DOI] [PubMed] [Google Scholar]
- 26.Wang J, Smailes E, Sareen J, et al. The prevalence of mental disorders in the working population over the period of global economic crisis. Can J Psychiatry. 2010;55(9):598–605. doi: 10.1177/070674371005500908. [DOI] [PubMed] [Google Scholar]
- 27.Clinical Research Unit for Anxiety and Depression, St. Vincent’s Hospital. Composite International Diagnostic Interview. Sydney, Australia: Clinical Research Unit for Anxiety and Depression; 2005. ( http://www.crufad.com/index.php/cidi). (Accessed November 23, 2005) [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 29.McDowell I, Newell C. Measuring Health: A Guide to Rating Scales and Questionnaires. 2nd ed. New York, NY: Oxford University Press; 1996. [Google Scholar]
- 30.Boyle GJ. Self-report measures of depression: some psychometric considerations. Br J Clin Psychol. 1985;24(pt 1):45–59. doi: 10.1111/j.2044-8260.1985.tb01312.x. [DOI] [PubMed] [Google Scholar]
- 31.Statistics Canada. Canadian Community Health Survey Mental Health and Well-Being: Cycle 1.2. Ottawa, Canada: Statistics Canada; 2010. [Google Scholar]
- 32.Wang JL, Patten SB, Currie S, et al. Predictors of 1-year outcomes of major depressive disorder among individuals with a lifetime diagnosis: a population-based study. Psychol Med. 2012;42(2):327–334. doi: 10.1017/S0033291711001218. [DOI] [PubMed] [Google Scholar]
- 33.StataCorp. Stata Corporation. College Station, TX: Stata Corporation; 2010. Stata statistical software, release 10. [Google Scholar]
- 34.Bijl RV, De Graaf R, Ravelli A, et al. Gender and age-specific first incidence of DSM-III-R psychiatric disorders in the general population: results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Soc Psychiatry Psychiatr Epidemiol. 2002;37(8):372–379. doi: 10.1007/s00127-002-0566-3. [DOI] [PubMed] [Google Scholar]
- 35.Stansfeld SA, Clark C, Caldwell T, et al. Psychosocial work characteristics and anxiety and depressive disorders in midlife: the effects of prior psychological distress. Occup Environ Med. 2008;65(9):634–642. doi: 10.1136/oem.2007.036640. [DOI] [PubMed] [Google Scholar]


