Abstract
Background:
The aim of this double-blind, prospective, randomized, controlled study was to compare the effect of addition of ketamine; fentanyl and saline with propofol anesthesia on hemodynamic profile and laryngeal mask airway (LMA) insertion conditions in oral clonidine premedicated children.
Methods:
180 children (age 2 - 10 years) were at first given oral clonidine (4 μg/kg) 90 minutes before operation, and then were randomly allocated to receive either ketamine 0.5 mg/kg (n=60), fentanyl 1 μg/kg (n=60) or 0.9% normal saline (n=60) before induction with propofol 3.0 mg/kg. Insertion of LMA was performed within 1 minute of injection of propofol. Heart rate and mean blood pressure were noted 1 min before induction (baseline), immediately after induction, before and after insertion of LMA for up to 3 min. Following LMA insertion, 6 subjective end points were noted-mouth opening, coughing, swallowing, patient's movement, laryngospasm, and ease of an insertion. LMA insertion summed score was prepared depending upon these variables.
Results:
LMA insertion summed score was nearly similar in ketamine and fentanyl group, which were significantly better than saline group (P<0.004). Mean blood pressure and heart rate were maintained in ketamine than with fentanyl or saline group. Incidence of prolonged apnea (>120 secs.) was higher in fentanyl group compared to ketamine and saline group.
Conclusion:
Even in oral clonidine premedicated children, addition of ketamine with propofol provides hemodynamic stability and comparable conditions for LMA insertion like fentanyl propofol with significantly less prolonged apnea.
Keywords: Fentanyl, ketamine, laryngeal mask airway insertion, oral clonidine, propofol
INTRODUCTION
Intravenous propofol can be successfully used as a sole induction agent to facilitate laryngeal mask airway (LMA) insertion even in children because of its predominant upper airway reflexes depressant action.[1] But, unwanted responses either in the form of drop in blood pressure or coughing, laryngospasm, and movement may occur.[2] These are due to reduction in sympathetic tone with higher dose or lighter plane of anesthesia with lower dose, respectively. The large central compartment volume in children makes the induction dose calculation difficult when it is used as a sole agent.[3] To combat these problems, addition of opioid (like fentanyl) prior to propofol induction gained importance.[3,4] Fentanyl pretreatment also reduces propofol requirement for LMA insertion. But, fentanyl also has problems like respiratory depression and decrease of airway reflexes as dose-related manner.[3,4]
Ketamine is well-known for its airway reflexes maintaining activity and sympathetic stimulation. Both are desirable in pediatric anesthesia.[5] Due to these properties, ketamine is now a popular induction agent of choice in pediatric anesthesia with propofol.[6]
Clonidine, an alpha-2 adrenergic agonist, produces sedation by decreasing the sympathetic nervous system activity and the level of arousal. Clonidine is rapidly and almost completely absorbed from gastrointestinal tract (oral bioavailability up to 95%). After an oral intake, onset of action starts within 30-60 minutes and peak plasma concentration is reached within 90 min.[7] It is devoid of respiratory depressant action and lacks the negative effects on cognition, memory, and behavior as seen with midazolam.[7] Previous studies have shown that an oral clonidine premedication reduces propofol requirement for LMA insertion,[8] and oral clonidine is superior to oral midazolam in pediatric patient in view of mask acceptance, parental satisfaction, and quality of sedation (similar to natural sleep).[9] Thus, clonidine has a promising role in premedication in children.
The current double-blind, prospective, randomized, controlled study was conducted with the aim to compare the effect of addition of ketamine with fentanyl and saline before propofol induction on hemodynamic profile during and immediately after LMA insertion, and to compare insertion conditions in oral clonidine premedicated children.
METHODS
With an approval of ethical committee, a written and informed consent was taken from parents of each 180 patient between age group of 2-10 years of either gender with American Society of Anesthesia physical status grading I from a group of 201 potential candidates. Patient suffering from respiratory tract infection within 6 weeks, allergy to any study medication, abnormal/difficult airway anatomy, increase risk of regurgitation, and lengthy surgery (>2 hrs) were excluded from the study.
Randomization was done by using a computer-derived random-number sequence and sealed opaque envelopes and all investigators were kept unaware of the envelope details throughout the whole study period.
Children were adequately fasted (4-6 hrs). 90 minutes before an induction of anesthesia, all patients were premedicated using clonidine (4 μg/kg) orally mixed in 5 ml 50% dextrose solution through dropper under supervision of nurse on duty. All children who refused to take the premedication or spat it out were excluded from the study protocol. On arrival in the operation theater, a peripheral line and standard non-invasive monitoring were established. Patient received glycopyrrolate 5 μg/kg intravenously 5 minutes before an induction as per hospital protocol. Lactated ringer's solution at the rate of 5 ml/kg/hr was administered during the peri-operative period.
Patients were randomly divided into 3 groups-
-
a)
Group F – Fentanyl group – 60 patients each – received fentanyl 1 μg/kg in 5 ml normal saline IV
-
b)
Group K – Ketamine group – 60 patients each – received ketamine 0.5 mg/kg in 5 ml normal saline IV
-
c)
Group C – Control group – 60 patients each – received 5 ml of normal saline IV.
After preoxygenation for 3 min, patients were given either of assigned drugs intravenously over 10 sec followed immediately by propofol 3.0 mg/kg intravenously over 15 sec. To reduce pain on propofol administration 1 ml of 1% lidocaine was added to 100 mg of propofol. If required, further increments of propofol 0.5 mg/kg was given until loss of consciousness and loss of eye lash reflex. Insertion of LMA was performed by a same blinded anesthetist (of >3 yrs experience in pediatric airway management) 60 sec after injection of propofol using technique according to manufacturer's instruction.[10] The cuff was inflated with air until effective ventilation was established or the maximum recommended inflation volume was used. Following successful insertion, LMA position was assessed by observing chest movement, square wave capnography trace, and reservoir bag movement with both spontaneous and assisted ventilation. To prevent dislodgement, LMA was fixed properly. Roller gauze was used as bite blocker.
LMA insertion condition were graded by the same blinded anesthetist as
-
a)
Mouth opening: 1 – Full, 2 – Partial (not ideal but permits easy opening of mouth), 3 – Nil
-
b)
Coughing: 1 – Nil, 2 – Mild, 3 – Severe
-
c)
Swallowing: 1 – Nil, 2 – Mild, 3 – Severe
-
d)
Movement: 1 – Nil, 2 – Mild (Finger) (some movement but did not affect positioning of LMA), 3 – Severe (Arm/leg) (holding of LMA was required and additional dose of induction agent given).
-
e)
Laryngospasm: 1 – Nil, 2 – Mild (relieved by positive pressure ventilation), 3 – Severe (desaturation<90%)
-
f)
Ease of LMA insertion 1 - Easy, 2 - Difficult, 3 - Impossible.
If the first attempt LMA insertion was unsuccessful or resulted in malpositioning, the patient received a subsequent bolus dose of propofol 0.5 mg/kg and his/her lungs were ventilated using a face mask. LMA insertion was attempted to maximum of 3 attempts. However, insertion conditions assessment was done only for the first attempt. If LMA insertion was unsuccessful after 3 attempts, patient's trachea was intubated after using muscle relaxant. After successful LMA insertion, anesthesia was maintained with 70% N2O with 30% O2 and Halothane, using Ayres T piece for patient weight <18 kg and Bain's circuit for patients >18 kg. Throughout induction and insertion, all patients were monitored using pulse oximetry, capnography, non-invasive blood pressure, and ECG. (Philips Medical. India.)
The time from LMA placement until the return of spontaneous ventilation was recorded. The presence of apnea was defined as an absence of respiration for more than 30 sec, and prolonged apnea was defined as absence of respiration for >120 seconds. Mean blood pressure and heart rate were recorded 1 min before induction (baseline), immediately after induction of anesthesia, immediately before LMA insertion, after LMA insertion, then at every minute for up to 3 minutes by a blinded staff on duty.
All statistical analyzes were performed using SPSS for windows 15.0. (SPSS Inc., Chicago, IL, USA). Parametric data were compared using analysis of variance (ANOVA) within group comparisons at different time intervals assessed by using paired t-test. All the categorical data were compared by using chi-square test. A sample size of 20 patients per group was needed to detect an intergroup difference of at least 20% (α=0.01, two-sided, power=90%) with two sample t-test.[11] A value of P<0.05 was considered statistically significant. Most results are expressed as mean (SD), some in percentage and some in ratio (sex).
RESULTS
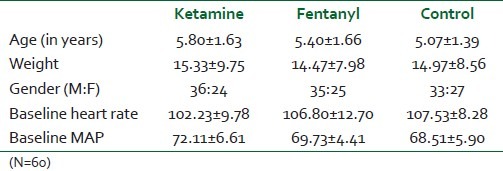
The 3 study groups were well-matched for age, gender, body weight baseline MAP, and heart rate [Table 1].
Table 1.
Age, bodyweight, sex wise distribution of cases
LMA was successfully inserted in first attempt only in 49 patients (81%) of control group while 56 patients (93.33%) and 57 patients (95%) of ketamine and fentanyl group had no problem in insertion. The difference is statistically significant. (P=0.048) [Table 2].
Table 2.
Insertion conditions of LMA
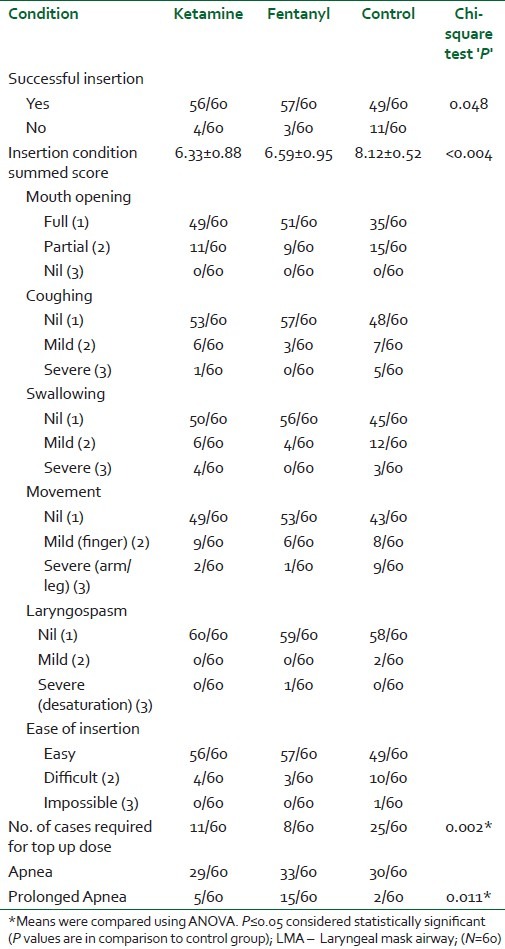
LMA insertion summed score was significantly better with ketamine 6.33±0.88 and fentanyl 6.59±0.95 than with control group 8.12±0.52 (P<0.001). No difference in summed score was observed between ketamine and fentanyl group [Table 2].
In 25 (41.66%) of the control patients, more dose of (additional 0.5 mg/kg) propofol was required as compared to 11 (18.33%) of those in ketamine group and 8 (13.33%) of subjects in fentanyl group (P=0.002) [Table 2]. However, no significant difference was noted between ketamine and fentanyl groups (P=0.72).
The incidence of prolonged apnea was significantly higher among fentanyl group 15 (25%) patients as compared to controls 2 (3.33%) (P=0.011) as well as 5 ketamine group of patients (8.33%) (P=0.08) [Table 2].
After LMA insertion, there was a rise in heart rate in control and ketamine group while in fentanyl group, there was no significant rise from the baseline [Figure 1]. Maximum heart rate was seen with ketamine (122.23±8.43/min) immediately after LMA insertion and lowest heart rate was seen with fentanyl group (96.48±6.92/min) just after induction. With induction of anesthesia, significant drop in mean arterial blood pressure was observed in control group and fentanyl group from baseline while in ketamine group, there was a rise in mean arterial pressure at all time interval (P<0.05) [Figure 2]. Maximum mean blood pressure was 84.24±2.88 mmHg with ketamine group seen 3 minutes after LMA insertion.
Figure 1.
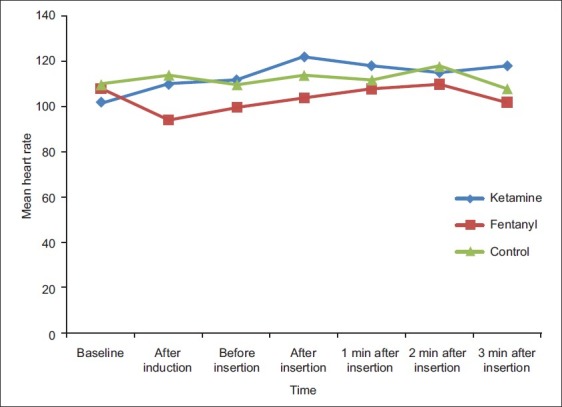
Changes in heart rate in the three groups
Figure 2.
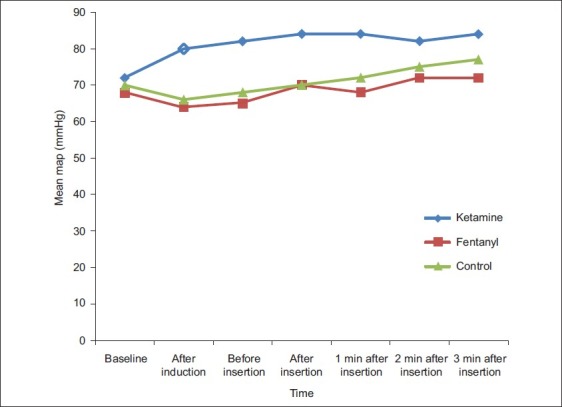
Changes in mean arterial pressure in the three groups
DISCUSSION
The main purpose of this study was to compare the hemodynamic effects of ketamine with fentanyl and saline administered prior to induction of anesthesia using propofol in oral clonidine premedicated children. Second issue was to investigate whether administration of ketamine or fentanyl improves LMA insertion conditions. In the present study, we demonstrated consistently higher heart rate and mean arterial blood pressure in ketamine group compared to fentanyl and saline group, even in clonidine premedicated patient. The indirect sympathomimetic action of ketamine on sinus node may lead to this effect.
Propofol decreases blood pressure by decrease in peripheral vascular resistance and myocardial contractility.[1,2] Heart rate may be slowed with more significant vagotonic effect at larger doses.[1,2] The combination of propofol ketamine attenuates hemodynamic depression intraoperatively without causing respiratory depression. The cardio-stimulant effect of ketamine in balances the cardio-depressant effect of propofol and this effect is utmost important in pediatric group of patients.[5] Goh et al. demonstrated that the addition of subanesthetic dose of ketamine with propofol for LMA insertion preserved hemodynamic stability in adult patient.[12] Tomatir et al. showed that ketamine 0.5 mg/kg administered before propofol 1.5 mg/kg preserved hemodynamic stability compared with propofol alone in children in short term procedure like magnetic resonance imaging.[13] In our study, ketamine 0.5 mg/kg administered before induction of anesthesia with propofol 3 mg/kg for LMA placement produced improved hemodynamic stability compared to fentanyl 1 μg/kg with same dose of propofol in children.
Goh et al. showed that the addition of fentanyl increased the depressant effects of propofol on systolic blood pressure and heart rate.[12] Cheam and Chui also deducted that fentanyl enhances the depressant effects of propofol on blood pressure and heart rate.[4] Our results are similar with these studies, with heart rate and mean blood pressure decreasing following induction of anesthesia with fentanyl–propofol in the present study.
Goyagi et al. described that oral clonidine premedication reduced propofol requirement for the LMA insertion in adults.[8] The mean dose (ED50) according to their study in adult is 2±0.2 mg/kg. A satisfaction insertion was present in 59% of our oral clonidine-premeditated control group children with a dose of 3 mg/kg propofol. This could be possible due to the fact that substantially greater volume of distribution of drug in children as compared to adults.
Still, there is no consensus regarding the criteria to assess LMA insertion condition. In our study also, we compared LMA insertion conditions using the methodology based on 6 variables/3 grade score proposed by Silivagam et al.[14] and Cheam et al.[4] Here also, we graded 4 fundamental patient responses to insertion like swallowing, coughing, movement, laryngospasm, and 2 observer-dependent variables like mouth opening with an ease of insertion. Conditions were graded as satisfactory if there was adequate mouth opening, no coughing, swallowing or laryngospasm, and no limb movement. We were able to use the score to assess both the ease of placement and patient's response. From these 6 points, a ‘summed score’ was prepared. In our study, ‘summed score’ of ketamine and fentanyl use for LMA insertion following anesthetic induction with propofol was comparable, which was significantly better than control group. Our results concur with the studies by Goh et al. in adult population.[12]
Prolonged apnea occurred more frequently with fentanyl than with ketamine or saline in our study. Our study is comparable to other studies where fentanyl was used to facilitate LMA insertion following propofol induction and prolonged the duration of apnea.[4,12]
Our study has the limitation of only one dose-response evaluation. We preferred to use a smaller dose of propofol (3 mg/kg) with oral clonidine premedicated patient that would not cause any hemodynamic side-effects. Secondly, our main concern was LMA insertion conditions and hemodynamic changes during insertion. Other concerns with addition of ketamine like emergence reactions were not followed in this study in children. However, we feel further studies with large sample size should address to solve our limitations.
CONCLUSION
Administration of low dose of ketamine balanced the cardio depressant effect of propofol, even in clonidine-premedicated children. The combination is of significant hemodynamic benefit and better LMA insertion condition when compared with placebo. It is also seen that ketamine-propofol provide comparable conditions for LMA insertion like fentanyl-propofol with significantly less prolonged apnea and hemodynamic stability in clonidine-premedicated children.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bahk JH, Han SM, Kim SD. Management of paediatric difficult airway with a laryngeal mask airway under propofol anaesthesia. Paediatr Anaesth. 1999;9:163–6. doi: 10.1046/j.1460-9592.1999.9220305.x. [DOI] [PubMed] [Google Scholar]
- 2.Scalon P, Carey M, Power M, Kirby F. Patient response to laryngeal mask insertion after induction of anaesthesia with propofol or thiopentone. Can J Anaesth. 1993;40:816–8. doi: 10.1007/BF03009250. [DOI] [PubMed] [Google Scholar]
- 3.Goyagi T, Tanaka M, Nishikawa T. Fentanyl decreases propofol requirement for laryngeal mask airway insertion. Acta Anaesthesiol Scand. 2003;47:771–4. doi: 10.1034/j.1399-6576.2003.00123.x. [DOI] [PubMed] [Google Scholar]
- 4.Cheam EW, Chui PT. Randomised double-blind comparison of fentanyl, mivacurium or placebo to facilitate laryngeal mask airway insertion. Anaesthesia. 2000;55:323–6. doi: 10.1046/j.1365-2044.2000.01214.x. [DOI] [PubMed] [Google Scholar]
- 5.Furuya A, Mastukawa T, Ozaki M, Nishiyama T, Kume M, Kumazawa T. Intravenous ketamine attenuates arterial pressure changes during the induction of anaesthesia with propofol. Eur J Anaesthesiol. 2001;18:88–92. doi: 10.1046/j.0265-0215.2000.00784.x. [DOI] [PubMed] [Google Scholar]
- 6.Bahk JH, Sung J, Jang IJ. A comparison of ketamine and lidocaine spray with propofol for the insertion of LMA in children: A double blinded randomized trial. Anesth Analg. 2002;95:1586–9. doi: 10.1097/00000539-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Basker S, Singh G, Jacob R. Clonidine in paediatrics: A review. Indian J Anaesth. 2009;53:270–80. [PMC free article] [PubMed] [Google Scholar]
- 8.Goyagi T, Tanaka M, Nishikawa T. Oral clonidine premedication reduces propofol requirement for laryngeal mask airway insertion. Can J Anaesth. 2000;47:627–30. doi: 10.1007/BF03018994. [DOI] [PubMed] [Google Scholar]
- 9.Almenrader N, Passariello M, Coccetti B, Haiberger R, Pietropaoli P. Premedication in children: A comparison of oral midazolam and oral clonidine. Paediatr Anaesth. 2007;17:1143–9. doi: 10.1111/j.1460-9592.2007.02332.x. [DOI] [PubMed] [Google Scholar]
- 10.San Diego, CA 92122: LMA North America, Inc., The Laryngeal Mask Company Limited; 2005. LMA™ Airway Instruction Manual. revised. [Google Scholar]
- 11.Murphy KR, Myors B. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. Statistical power analysis: A simple and general model for traditional and modern hypothesis tests. [Google Scholar]
- 12.Goh PK, Chiu CL, Wang CY, Chang YK, Loo PL. Randomized double-blind comparision of ketamine-propofol, fentanyl-propofol and propofol-saline on haemodynamics and laryngeal mask airway insertion conditions. Anaesth Intensive Care. 2005;33:223–8. doi: 10.1177/0310057X0503300211. [DOI] [PubMed] [Google Scholar]
- 13.Tomatir E, Atalay H, Gurses E, Erbay H, Bozkurt P. Effects of low dose ketamine before induction on propofol anesthesia for pediatric magnetic resonance imaging. Pediatr Anesth. 2004;14:845–50. doi: 10.1111/j.1460-9592.2004.01303.x. [DOI] [PubMed] [Google Scholar]
- 14.Sivalingam P, Kandasamy R, Madhaven G, Dhakshinamoorthi P. Conditions for laryngeal mask insertion. A comparison of propofol versus sevoflurane with or without alfentanil. Anaesthesia. 1999;54:271–6. doi: 10.1046/j.1365-2044.1999.00663.x. [DOI] [PubMed] [Google Scholar]


