Abstract
Context:
Fine needle aspiration cytology (FNAC) of the lymph node is a simple diagnostic tool to diagnose suspected and unsuspected secondary and primary lymph node malignancy.
Aim:
To study the utility of FNAC in the diagnosis of clinically suspected and unsuspected lymph node malignancy.
Design:
A cross-sectional hospital based study on 50 patients diagnosed to have primary or secondary lymph node malignancy by cytology, and confirmed by histopathology.
Materials and Methods:
Lymph node aspirate smears reported as malignant were studied and the findings were correlated with histopathology. Clinical and radiological data were also noted.
Statistical Analysis:
The data were tabulated as per the involvement of the various lymph node groups and the types of secondary and primary lymph node malignancies involved.
Results:
45 cases of metastatic malignancy and five cases of lymphomas were diagnosed by FNAC of lymph nodes. Histopathological correlation was available in all cases. Malignancy was clinically unsuspected in nine cases (18%).
Conclusion:
FNAC of lymph nodes is a very useful, simple and sometimes the only tool in the diagnosis of lymph node malignancies.
Keywords: Fine needle aspiration cytology, lymph node, malignancy
INTRODUCTION
Enlarged lymph nodes are easily accessible for fine needle aspiration and hence fine needle aspiration cytology (FNAC) is a very simple and important diagnostic tool for lymph node lesions.
Malignancies in lymph nodes in our country are predominantly metastatic in nature with an incidence varying from 65.7%[1] to 80.4%[2] and lymphomas range from 2%[3] to 15.3%[2] among lymph nodes aspirated from all sites. Although histopathological examination is considered to be gold standard in diagnosis especially in lymphomas, FNAC maybe the only tool for diagnosis and further management of the patients in some cases of metastatic malignancy.
This study was undertaken with the aim of highlighting the role of FNAC's of lymph nodes in the diagnosis of suspected and unsuspected lymph node malignancies.
MATERIALS AND METHODS
This study was conducted over a 5½ year period from July 2004 to December 2009. The study material was taken from 110 malignant lymph node aspirates (15.4%) out of a total of 713 lymph nodes aspirated during that period in our hospital. Inadequate smears were excluded from the study. From the 110 cytologically diagnosed cases, only 50 cases with histopathological correlation were taken in this study. A detailed history, clinical examination and relevant investigations were documented. FNAC of the enlarged lymph node was performed taking aseptic precautions. The smears were stained with Papanicolaou and Haematoxylin–Eosin stain.
Immunohistochemistry was done later on the tissue biopsy only in four cases of lymphoma and one case of melanoma. In cases where unsuspected metastasis was given, the primary site of malignancy was searched for and subsequently biopsied. The cytological diagnosis was correlated with lymph node or primary tumor biopsy.
RESULTS
Out of the 50 cases studied, 45 (90%) were metastatic tumors and five were lymphomas (10%).
The age group varied from 4 to 82 years, with males (30 cases, 60%) being more involved than females (20 cases, 40%). The lymph nodes involved by malignancy were 1.5 cm or more in size. Malignancy was clinically unsuspected in nine cases (18%).
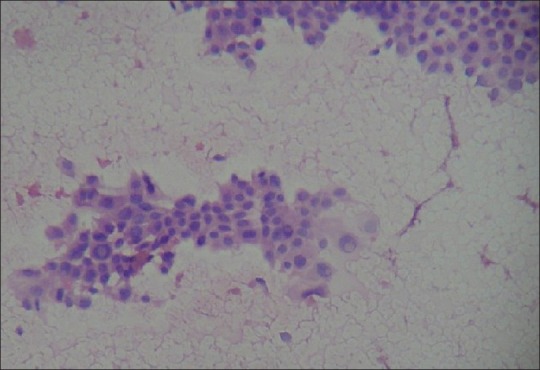
Table 1 shows the cytological diagnosis made on the lymph node aspirates. Squamous cell carcinoma was the most common metastatic tumor. The cases where cytological features were not classical of squamous cell carcinoma or adenocarcinoma were put in the category of epithelial malignancy. Among the thyroid carcinomas metastases, we could diagnose follicular, papillary, and medullary variants, and could suggest a probable thyroid primary in one case. The case of follicular carcinoma was a previously operated known case of follicular carcinoma, who later presented with lymph node enlargement, and hence the metastasis could be diagnosed. We had one case of metastatic mucocoepidermoid carcinoma from a primary in the parotid gland. One of the melanomas could be diagnosed easily. However, the other unsuspected melanoma was not very easy to diagnose on cytology as we could find pigmented cells after a very careful search among the pleomorphic cells [Figures 1–3].
Table 1.
Cytological diagnosis of aspirated lymph nodes
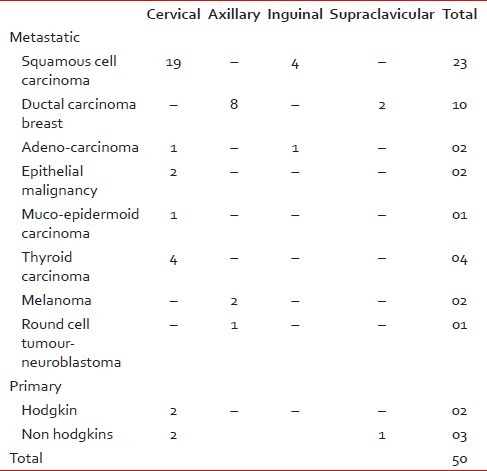
Figure 1.
Photomicrograph of smear of unsuspected melanoma, showing a pleomorphic population of tumor cells, some of which are binucleate and multinucleate. Pigment laden cell is also seen (Hematoxylin and Eosin stain, ×400)
Figure 3.
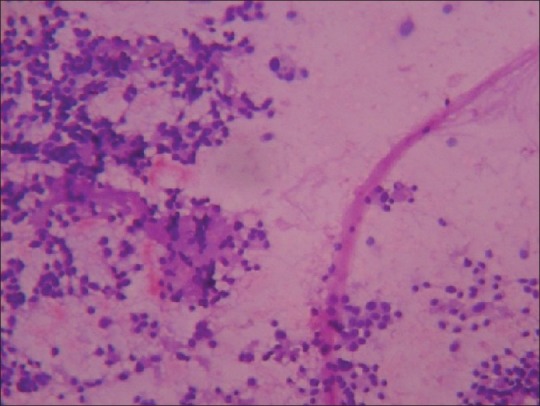
Photomicrograph of smear of medullary carcinoma thyroid, showing round cells with acellular eosinophilic material, (amyloid) in the background (Hematoxylin and Eosin stain, ×100)
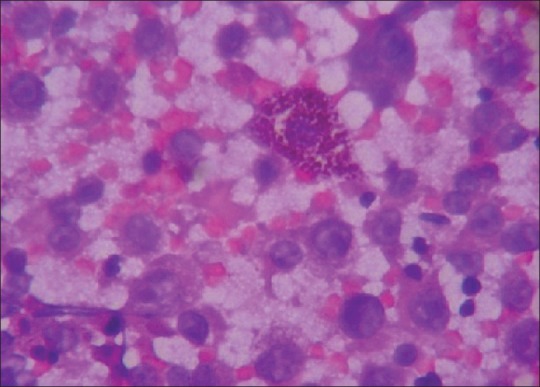
Figure 2.
Photomicrograph of smear of papillary carcinoma thyroid, showing a papillary fragment containing cells with large nuclei having intranuclear inclusion (Hematoxylin and Eosin stain, ×100)
Of the round cell tumor metastases, we had clinical (adrenal mass, orbital ecchymosis, axillary, and inguinal lymph nodes enlarged) and bone marrow biopsy correlation for the case of neuroblastoma.
Of the lymphomas, two cases were given as suspicious of Hodgkin lymphoma on cytology and both these cases had histopathological correlation as nodular sclerosis Hodgkin Disease. Of the three cases of Non-Hodgkin lymphoma diagnosed on cytology by the monomorphic population of cells, only one case was given as suspicious of lymphoproliferative lesion. All these three cases had immunohistochemical correlation confirming Non-Hodgkin lymphoma.
Histopathological correlation from the lymph node or other tissues was available in all 50 cases as shown in Table 2. All these cases correlated in the histopathological diagnosis.
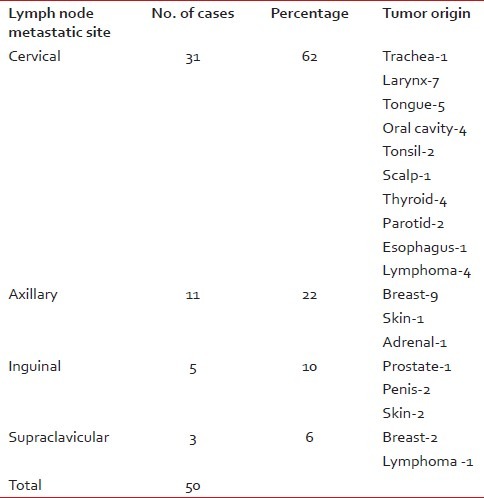
Table 2.
Aspirated lymph node sites showing the tumor origin as confirmed by biopsy
DISCUSSION
Enlarged lymph nodes are accessible for FNAC and are of importance specially to diagnose secondary or primary malignancies. It plays a significant role in developing countries like India, as it is a cheap procedure, simple to perform and has almost no complications.[1–3] The diagnosis given on the cytological material is often the only diagnosis accepted and sometimes there is no further correlation with histopathology, especially in cases of advanced malignancies. It also provides clues for occult primaries and sometimes also surprises the clinician who does not suspect a malignancy.
In our institution, 15.4% of the lymph node FNAC's yielded malignant diagnoses. Other studies have found the incidence to vary from 5.8[3] to 25.03%.[4–6] Our study showed more cases of metastatic involvement of the lymph nodes (90%) rather than lymphomas (10%). This was similar to other Indian studies[2,3] although there are variations in the percentage involved depending on the number of cases studied. However, an earlier Indian study[7] had documented 102 cases (68%) of metastases and 42 cases (32%) involved by lymphomas among 150 cases of malignancies diagnosed by lymph node FNAC. A Brazilian FNAC study on lymph nodes diagnosed 79.4% metastases and 14.2% lymphomas.[8] A study conducted in Baghdad has reported more involvement by lymphomas (58.2%) rather than metastatic disease (37.3%) and 4.4% involved by leukemia.[9] The diagnostic accuracy of FNAC in metastatic disease varies from 87% to 97.9%[2,3] and for lymphomas is 82%.[2] The sensitivity of FNAC for metastatic lesions to lymph nodes has varied from 97.9% to 100%, whereas the specificity has been found to be 100%.[2,4]
For the lymphomas the sensitivity has been found to be 80% and specificity 100%.[4]
The primary sites identified in each lymph node group in our study correlated with other similar studies.[2,10,11] A full history, radiological investigations and immunohistochemistry in difficult cases may help to arrive at a definitive diagnosis.[11] Specialized investigations such as the combination of lymphosyntigraphy and ultrasonography-guided FNAC's of sentinel lymph nodes in the head and neck area have been found to be good in picking up metastases in clinically undetectable lymph nodes.[12]
The cervical group is the most common group of lymph nodes to be involved and the primary is most often from the oral cavity[4,12] with squamous cell carcinoma being the most common histological type.[1,2,12] Rates for oral cavity/pharynx, esophagus, male larynx are highest in India, probably due to the use of multiple tobacco products.[13] Among the soft tissue tumors rhabdomyosarcoma and extra skeletal Ewing's sarcoma/primitive neuroectodermal tumor are known to metastasize to lymph nodes, the other rare tumors being malignant granular cell tumor, epithelioid hemangioendothelioma, mediastinal ganglioneuroblastoma, angiosarcoma, and epithelioid sarcoma.[14]
The improved diagnostic ability of FNAC in the diagnosis of malignant lesions of the lymph nodes is probably due to a combination of factors such as the increased use of the technique, better and easier availability of reference material of similar studies, and increased experience of the trained observers over the years.
CONCLUSION
FNAC of lymph nodes is a very useful and simple tool in the diagnosis of lymph node malignancies. It may be the only tool in the diagnosis of metastatic lesions in the lymph nodes and can help to detect occult primary malignancies. For the diagnosis of lymphomas, it can suggest a preliminary diagnosis, which can be followed by histopathology and immunohistochemistry for confirmation. Hence, the cytopathologist plays a vital role in the diagnosis of lymph node malignancies.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bagwan IN, Kane SV, Chinoy RF. Cytologic evaluaton of the enlarged neck node: FNAC utility in metastatic neck disease. Int J Pathol. 2007;6:2. [Google Scholar]
- 2.Alam K, Khan A, Siddiqui F, Jain A, Haider N, Maheshwari V. Fine needle aspiration cytology (FNAC): A handy tool for metastatic lymphadenopathy. Int J Pathol. 2010;10:2. [Google Scholar]
- 3.Khajuria R, Goswami KC, Singh K, Dubey VK. Pattern of lymphadenopathy on fine needle aspiration cytology in Jammu. JK Sci. 2006;8:157–9. [Google Scholar]
- 4.Hirachand S, Lakhey M, Akhter P, Thapa B. Evaluation of fine needle aspiration cytology of lymph nodes in Kathmandu Medical College, Teaching hospital. Kathmandu Univ Med J. 2009;7:139–42. doi: 10.3126/kumj.v7i2.2707. [DOI] [PubMed] [Google Scholar]
- 5.Ahmad T, Naeem M, Ahmad S, Samad A, Nasir A. Fine needle aspiration cytology (FNAC) and neck swellings in the surgical outpatient. JAMC. 2008;20:30–2. [PubMed] [Google Scholar]
- 6.Paul PC, Goswami BK, Chakraborti S, Giri A, Pramanik R. Fine needle aspiration cytology of lymph nodes: An Institutional study of 1448 cases over a five year period. J Cytol. 2004;21:187–90. [Google Scholar]
- 7.Arora B, Beena KR, Arora DR. Utility of fine needle aspiration cytology in lymphadenopathies. J Cytol. 1999;16:61–6. [Google Scholar]
- 8.Martins MR, Santos GC. Fine-needle aspiration cytology in the diagnosis of superficial lymphadenopathy: A 5-year Brazilian experience. Diagn Cytopathol. 2006;34:130–4. doi: 10.1002/dc.20373. [DOI] [PubMed] [Google Scholar]
- 9.AlAlwan NA, AlHashmi AS, Salman MA, AlAttar EA. Fine needle aspiration cytology versus histopathology in diagnosing lymph node lesions. East Mediterr Health J. 1996;2:320–5. [Google Scholar]
- 10.Sinha SK, Basu K, Bhattacharya A, Banerjee U, Banerjee D. Aspiration cytodiagnosis of metastatic lesions with special reference to primary sites. J Cytol. 2003;20:16–8. [Google Scholar]
- 11.Gupta N, Rajwanshi A, Srinivasan R, Nijwahan R. Pathology of supraclavicular lymphadenopathy in Chandigarh, north India: An audit of 200 cases diagnosed by fine needle aspiration. Cytopathology. 2006;17:94–6. doi: 10.1111/j.1365-2303.2006.00285.x. [DOI] [PubMed] [Google Scholar]
- 12.Hoft S, Muhle C, Brenner W, Sprenger E, Maune S. Fine-needle aspiration cytology of the sentinel lymph node in head and neck cancer. J Nucl Med. 2002;43:1585–90. [PubMed] [Google Scholar]
- 13.Rastogi T, Devesa S, Mangtani P, Mathew A, Cooper N, Kao R, et al. Cancer incidence rates among South Asians in four geographic regions: India, Singapore, UK and US. Int J Epidemiol. 2008;37:147–60. doi: 10.1093/ije/dym219. [DOI] [PubMed] [Google Scholar]
- 14.Loya AC, Prayaga AK, Arora A, Sundaram C, Rao S, Uppin SG, et al. Lymph node metastasis of soft tissue tumors: A cytomorphologic study. Acta Cytol. 2007;51:153–60. doi: 10.1159/000325708. [DOI] [PubMed] [Google Scholar]


