Abstract
Pyogenic brain abscess is important in neurology. This infectious disease is fatal and the management is usually complicated. Here, the authors review and discuss the clinical aspects of pyogenic brain abscess found in the earlier reports from a tropical setting in Thailand. The literature review was compiled through standard reference database searching and the derived publications were further extracted to obtain clinical data. The main clinical characteristics of pyogenic brain abscess in this setting were similar to others. However, there are some specific characteristics on the nature of tropical setting.
Keywords: Abscess, Brain, Pyogenic, Tropical
Introduction
Pyogenic brain abscess is an important neurological infection. Similar to the abscess in other sites, the pyogenic brain abscess is a collection of pustular materials presenting as a mass-like lesion. The pyogenic brain abscess is an important neurological disease and can present with fatal illnesses. In some old reports, the mortality rate is up to one-third;[1] however, the current mortality of brain abscess patients is below 10%. However, this neurological disease could still be found despite improvements in medical facilities. Brain abscess is still related to high rates of neurological impairment and death.[2,3] Management of brain abscess requires good therapeutic practice. The complications of the disease could be seen and has to be closely followed and managed in the patients.
As pyogenic brain abscess is a kind of infectious disease, the disease is expected to be more common in a setting with poor sanitation and medical facilities. Infectious diseases are usually common in tropical countries. Here, the authors review and discuss the clinical aspects of pyogenic brain abscess found in the previous reports from a tropical setting in Thailand. The literature review was compiled by standard reference database searching and the derived publications were further extracted to obtain clinical data. The main clinical characteristics of pyogenic brain abscess in this setting are similar to others. However, there are some specific characteristics due to the nature of tropical setting.
Literature Review on Pyogenic Brain Abscess in Thailand
A systematic review on pyogenic brain abscess in Thailand was done with an aim to summarize the Thai reports on pyogenic brain abscess. For reviewing, standard search engines like PubMed and ThaiIndexMedicus were used and the searching key words included “Thailand,” “brain” and “abscess.” The searching term “abscess” already covered cerebral abscess, supratentorial abscess, infratentorial abscess, cerebellar abscess, etc. Both pediatric and adult populations were already covered in this search. Only the reports on pyogenic brain abscess with complete information were selected for further descriptive analysis. Since this is only a review, and not a retrospective descriptive study, complete data on all the issues could not be found from all of the selected publications and as the data were obtained from non-homogeneous groups, the complete statistical analysis could not be done. The statistical analysis was done only where it was appropriate and possible.
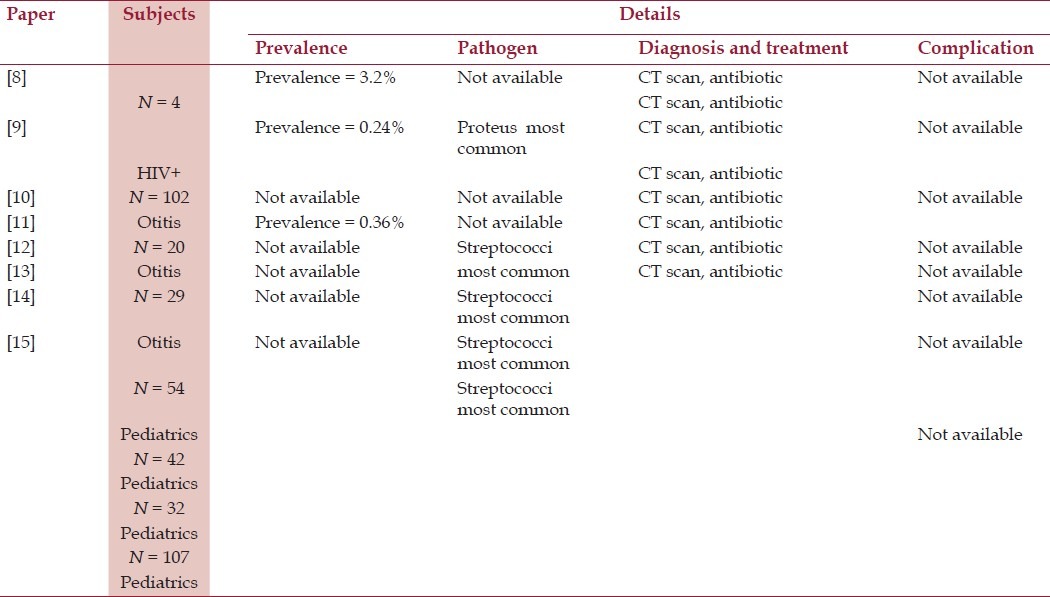
According to the literature search, there were 8 selected publications on a total of 390 patients,[4–11] which were used for further extraction of clinical data [Table 1]. The age range of the patients were between 0.25 and 54 years (median age = 11.4 years). There were 226 males and 164 females (ratio = 1.38: 1). The focused issues for review included epidemiology, microbiology, clinical diagnosis and treatment (which include therapeutic management, complications and outcome). The details of the review on various publications would be shown further.
Table 1.
Previous publications on brain abscess in Thailand
Epidemiology of Pyogenic Brain Abscess in Thailand
There are some reports on epidemiology of brain abscess from several countries around the world. Interestingly, without dependence on the setting of study, the cases are usually elder or pediatric male patients.[12–15] However, the trend of decreasing incidents are reported due to the improvement in world sanitation at present.[14]
Focusing on the Thai situation, there are some epidemiological reports on pyogenic brain abscess. However, there are no good systematic reports due to the lack of good neurological experts in Thailand. Few reports are present on the epidemiological data of pyogenic brain abscess relating to otological disorder.[4,5] Among the cases in those reports, most patients are usually young male patients with brain abscess as complication of suppurative otitis media.[5–7] There is a good report among the pediatric population from the biggest pediatric hospital in Thailand.[8] According to this report, the most important underlying condition of pyogenic brain abscess in Thai pediatric cases is congenital heart diseases, especially for Tetralogy of Fallot.[8] The other underlying condition is otitis media.[6] There are also some reports focusing on specific groups of patients. The reports on the human immunodeficiency virus (HIV)-infected patients are very interesting since Thailand is a country that still has the problem of increasing HIV infection. The prevalence of brain abscess among Thai HIV-infected patients is about 3.2%.[9]
As a conclusion, the report on epidemiology of pyogenic brain abscess is still limited in Thailand. The lack of good epidemiological data might be the problem for strategic planning for the control of this infectious disease.
Microbiology of Pyogenic Brain Abscess in Thailand
Several pathogens can cause pyogenic brain abscess. Commonly, the bacterial pathogens are the corresponding pathogens for brain abscess; however, some rare organisms such as fungus and parasite might cause brain abscess. In previous Thai reports, bacteria are the most common group of pathogens causing brain abscess,[5,8,10,11] similar to the reports from other countries.[12–15]
Microbiologically, a single organism (46.3%; 156 from 337 known data) is usually the etiological pathogen in Thai cases.[5,8,10,11] The 3 leading pathogens are Streptococci, Proteus and Staphylococcus aureus,[5,8,10,11] which are similar to the reports from other countries.[12–15] However, there are some interesting pathogens that are specific in this setting due to the nature of tropical countries. Those special situations would be further discussed under another specific heading in this article.
Clinical Diagnosis and Treatment of Pyogenic Brain Abscess in Thailand
The clinical diagnosis of brain abscess in Thailand is usually made by a neurologist. The confirmation of the diagnosis is usually done by a computed tomography (CT) scan after focusing on the suspicious clinical manifestation[5,8–11] like fever (87.2%), which is the most common presentation followed by headache (72.8%) and focal neurological signs (62.6%).[5,8–11] The diagnosis of brain abscess in all cases is done through the neurological imaging as already noted.[5,8–11] The lesion is usually single and is located at the parietal or temporal lobes,[5,8–11] which is noted differently in some reports from other countries where they mentioned a frontal lobe predominance.[14] Since this article is not a case report, the authors cannot provide original figures of brain abscesses. Some figures are available as original reports (but they cannot be represented since it would be considered plagiarism) and some reference websites (such as emedicine.medscape.com/article/336829-overview).
For the treatment, the standard pattern is the antibiotic treatment attempt followed by drainage in failure case.[5,8–11] Focusing on the outcome, the mortality rate among the Thai patients is about one-tenth.[5,8–11] There is no report on short- or long-term complications and outcome among the survived patients. Since there is no new observation on the clinical data from reported cases of pyogenic brain abscess in Thailand, the authors hereby only discuss briefly.
Some Important Conditions on Pyogenic Brain Abscess in Thailand
Being a tropical country, there are some concerns toward tropical medicine in pyogenic brain abscess in Thailand. Since there are fewer reports on this specific issue, the authors hereby summarize and discuss on some important conditions.
Melioidosis brain abscess
Melioidosis is an important bacterial infection caused by Burkholderia pseudomallei. It is common in tropical countries, especially Mekong countries in Southeast Asia (including Thailand, Laos and Cambodia). This infection has a variety of clinical spectrum and is accepted as a great mimicry pathogen.[16–18] The disease can also be present as brain abscess.[16,19] The diagnosis of this condition might be difficult if the physician in charge is not adept with it.[20]
There are some reports on pyogenic brain abscess due to melioidosis in Thailand. Based on a case series by Kasantikul et al., this disorder could be seen at any age with a male predominance. The diagnosis is primarily through CT scan and the confirmation is through culture analysis.[21] The abscess usually affects the frontoparietal area.[21] Expert recommendation on antibiotic treatment for this condition is “Ceftazidime is the treatment of choice for severe melioidosis, but response to high-dose parenteral treatment is slow.[19] ” However, a long duration of treatment is usually required and the failure rate is high.[19]
Amebic brain abscess
This kind of brain abscess occurs due to parasitic infection. It might not be an actual pyogenic brain abscess but it can be present as pustular brain lesion. Indeed, amebic brain abscess is an important invasive extraintestinal amebiasis. The causative pathogen is Entamoeba histolytica. This condition might have been common in the past but it is extremely rare in Thailand at present due to improvement of sanitation. However, undiagnosed amebic brain abscess is still reported and considered a serious condition in medical practice.[22]
Typhoid brain abscess
Typhoid is an important gastrointestinal infection due to Salmonella typhi. It is a common tropical infection and can still be seen in Thailand. The brain abscess can be an important presentation of typhoid, although it is rare. The classical presentations as seen in general pyogenic brain abscess can be seen but there may not be any gastrointestinal presentations in the patients.[23,24] There are some reports of typhoid brain abscess in Thailand. However, due to good sanitation at present, this condition has not been detected for decades.
New Findings from Reviewing the Thai Reports on Pyogenic Brain Abscess
In this work, the authors review and discuss the publications on brain abscess in Thailand. Indeed, brain abscess is a fairly common problem and is mentioned in chapters in many neurological books. In general, the findings from this work show similar clinical patterns of pyogenic brain abscess in Thailand. However, there are some specific and new findings from this specific setting.
First of all, being a tropical country, the pyogenic brain abscess from tropical infections could be seen. Of interest, the diagnosis of those infections could be missed if there is no good concern. For example, melioidosis is a very hard-to-diagnose infection that requires good history-taking and laboratory analysis.[16–18] Also, some tropical brain abscesses need specific medications such as anti-parasitic drug for amebic brain abscess. Presenting with the same clinical pictures, the underlying causative pathogens might be different and this is hard for effective management. The final diagnosis may not be reached just through imaging investigations and may usually require additional diagnostic tests. Understanding patient history is the key factor for a successful early diagnosis of uncommon tropical pyogenic brain abscess.
Furthermore, due to good transportation system at present, new cases of tropical pyogenic brain abscesses can be expected due to migrants and travelers[25,26] and this could be a more difficult situation.
Conclusion
Pyogenic brain abscess is an important neurological infection. It could be seen in Thailand with similar clinical epidemiology and characteristics to those reported in other countries. However, there are some interesting issues related to the nature of tropical countries.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Dohrmann PJ, Elrick WL. Observations on brain abscess. Review of 28 cases. Med J Aust. 1982;2:81–3. doi: 10.5694/j.1326-5377.1982.tb124234.x. [DOI] [PubMed] [Google Scholar]
- 2.Gelabert-González M, Serramito-García R, García-Allut A, Cutrín-Prieto J. Management of brain abscess in children. J Paediatr Child Health. 2008;44:731–5. doi: 10.1111/j.1440-1754.2008.01415.x. [DOI] [PubMed] [Google Scholar]
- 3.Gelabert-González M, Serramito-García R, Aran-Echabe E. Supratentorial and infratentorial brain abscess. Acta Neurochir (Wien) 2012;154:1117. doi: 10.1007/s00701-012-1336-y. [DOI] [PubMed] [Google Scholar]
- 4.Kongsiriwattanakul S, Suankratay C. Central nervous system infections in HIV-infected patients hospitalized at King Chulalongkorn Memorial Hospital. J Med Assoc Thai. 2011;94:551–8. [PubMed] [Google Scholar]
- 5.Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S. Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J Laryngol Otol. 1993;107:999–1004. doi: 10.1017/s0022215100125095. [DOI] [PubMed] [Google Scholar]
- 6.Chotmongkol V, Sangsaard S. Intracranial complications of chronic suppurative otitis media. Southeast Asian J Trop Med Public Health. 1992;23:510–3. [PubMed] [Google Scholar]
- 7.Kangsanarak J, Navacharoen N, Fooanant S, Ruckphaopunt K. Intracranial complications of suppurative otitis media: 13 years’ experience. Am J Otol. 1995;16:104–9. [PubMed] [Google Scholar]
- 8.Ratanasiri B. Ten year review of brain abscess in Children's Hospital Bangkok, Thailand. J Med Assoc Thai. 1995;78:37–41. [PubMed] [Google Scholar]
- 9.Raksadawan N, Balankura K, Charoenchonvanich S. Brain abscesses in children. Siriraj Hosp Gaz. 1995;47:9–19. [Google Scholar]
- 10.Charoenchonvanich S. Retrospective study of brain abscess in children in Siriraj Hospital. Thai J Pediatr. 1994;33:s6. [Google Scholar]
- 11.Auvichayapat N, Auvichayapat P, Aungwarawong S. Brain abscess in infants and children: A retrospective study of 107 patients in northeast Thailand. J Med Assoc Thai. 2007;90:1601–7. [PubMed] [Google Scholar]
- 12.Gutiérrez-Cuadra M, Ballesteros MA, Vallejo A, Miñambres E, Fariñas-Alvarez C, García-Palomo JD, et al. Brain abscess in a third-level hospital: Epidemiology and prognostic factors related to mortality. Rev Esp Quimioter. 2009;22:201–6. [PubMed] [Google Scholar]
- 13.Tsou TP, Lee PI, Lu CY, Chang LY, Huang LM, Chen JM, et al. Microbiology and epidemiology of brain abscess and subdural empyema in a medical center: A 10-year experience. J Microbiol Immunol Infect. 2009;42:405–12. [PubMed] [Google Scholar]
- 14.Sharma R, Mohandas K, Cooke RP. Intracranial abscesses: Changes in epidemiology and management over five decades in Merseyside. Infection. 2009;37:39–43. doi: 10.1007/s15010-008-7359-x. [DOI] [PubMed] [Google Scholar]
- 15.Roche M, Humphreys H, Smyth E, Phillips J, Cunney R, McNamara E, et al. A twelve-year review of central nervous system bacterial abscesses: Presentation and aetiology. Clin Microbiol Infect. 2003;9:803–9. doi: 10.1046/j.1469-0691.2003.00651.x. [DOI] [PubMed] [Google Scholar]
- 16.Thummakul T, Wilde H, Tantawichien T. Melioidosis, an environmental and occupational hazard in Thailand. Mil Med. 1999;164:658–62. [PubMed] [Google Scholar]
- 17.Limmathurotsakul D, Peacock SJ. Melioidosis: A clinical overview. Br Med Bull. 2011;99:125–39. doi: 10.1093/bmb/ldr007. [DOI] [PubMed] [Google Scholar]
- 18.Inglis TJ, Sousa AQ. The public health implications of melioidosis. Braz J Infect Dis. 2009;13:59–66. doi: 10.1590/s1413-86702009000100013. [DOI] [PubMed] [Google Scholar]
- 19.White NJ. Melioidosis. Lancet. 2003;361:1715–22. doi: 10.1016/s0140-6736(03)13374-0. [DOI] [PubMed] [Google Scholar]
- 20.Cheng AC. Melioidosis: Advances in diagnosis and treatment. Curr Opin Infect Dis. 2010;23:554–9. doi: 10.1097/QCO.0b013e32833fb88c. [DOI] [PubMed] [Google Scholar]
- 21.Kasantikul V, Lerdlum S, Suwanwela N. Cerebral abscesses due to Pseudomonas pseudomallei. J Med Assoc Thai. 1992;75:536–41. [PubMed] [Google Scholar]
- 22.Viriyavejakul P, Riganti M. Undiagnosed amebic brain abscess. Southeast Asian J Trop Med Public Health. 2009;40:1183–7. [PubMed] [Google Scholar]
- 23.Viriyavejakul A, Poungvarin N, Aswapokee N, Ladplee S. Salmonella typhi brain abscess: Report of a case. Siriraj Hosp Gaz. 1982;34:655–6. [Google Scholar]
- 24.Hongprapas J, Phonprasert J, Techolarn C. Salmonella typhi brain abscess: Report of a case. Chula Med J. 1980;24:337–41. [Google Scholar]
- 25.Ahlm C, Olsen B, Koskinen LO, Monsen T. Brain abscess caused by methicillin-resistant Staphylococcus aureus. Scand J Infect Dis. 2000;32:562–3. doi: 10.1080/003655400458901. [DOI] [PubMed] [Google Scholar]
- 26.Dietz R, Schanen G, Kramann B, Erpelding J. Intracranial amebic abscesses: CT and MR findings. J Comput Assist Tomogr. 1991;15:168–70. doi: 10.1097/00004728-199101000-00032. [DOI] [PubMed] [Google Scholar]


