Abstract
Reconstruction of the lumbosacral region after surgical excision of irradiated and recurrent spinal giant cell tumours remains a challenging problem. In this case report, we describe the use of the pedicled omentum flap in reconstruction of an irradiated and infected wide sacral defect of a 19-year-old male patient. The patient had radiotherapy and subsequent wide surgical resection after recurrence of the tumour. A myocutaneous flap from the gluteal area had failed previously. Local flap options could not be used because of the recent radiotherapy to the gluteal area. Since the patient had a laparotomy for tumour resection and a colostomy, abdominal muscles were not considered reliable for reconstructive procedures. A pedicled omentum flap was chosen as a reconstructive option because of its rich blood supply, large surface area, and angiogenic capacity. This report aims to describe the use of the pedicled omentum flap for reconstruction of the lumbosacral area following surgical resection of a spinal tumour, when gluteal and abdominal flap options for reconstruction are jeopardised.
KEY WORDS: Omentum flap, radiotherapy, reconstruction, sacral tumour
INTRODUCTION
The reconstruction of sacral defects after surgical treatment of malignancies can be challenging for a plastic surgeon, particularly when complicated with osteoradionecrosis and infection. Local flap options include muscle, fasciocutaneous and skin flaps from the gluteal region, such as gluteus maximus musculocutaneous flap, gluteal fasciocutaneous flap and gluteal rotation flaps.[1] Flaps from the back and posterior thigh are the other available choices.[1]
In patients who have had radiotherapy (RT) of the gluteal region, local flap options are limited. The flap used for reconstruction should be well vascularised and have a biologic ability to fight the resistant bacterial infection due to poor vascularisation of the region seen after RT. The omentum flap has been widely used in both intraperitoneal and extraperitoneal defects because of its generous blood supply, large surface area, and angiogenic potential.[2]
We present a pedicled omental flap in the management of a complex spinal wound with the aim to describe the versatile use of the omentum flap in patients with large osteoradionecrotic defects of the sacral and gluteal area.
CASE REPORT
A 19-year-old male patient was operated by the Orthopedic Surgery and Traumatology Department for a giant cell bone tumour of the spine. Five months following sacrectomy, the tumour recurred and the patient received 34 doses of a total 7000 Gy RT for 6 weeks. One month after the last RT session, the patient was operated for the second time by the Orthopaedic Surgery Department. Re-resection was done through anterior as well as posterior approach. A sigmoid loop colostomy was done simultaneously. A myocutaneous gluteus maximus flap was used for closure of the 20 × 10 cm defect formed after resection of the tumour.
Fifteen days after surgery when Plastic Surgery consultation was sought it was observed that the sutures in the intergluteal area had given way, the raw wound surface of the dehisced area was covered with whitish yellow necrotic tissues and considerable amount of purulent discharge was coming out of the wound. The necrotic area was of 28 × 25 cm in dimension and the gluteal flap raised from the left gluteal region was completely necrosed. The surrounding tissues showed post radiotherapy changes with intense inflammation and unstable parchment like skin [Figure 1].
Figure 1.

The view of the 28 × 25 cm sacral defect before debridement. It was treated with gluteus maximus myocutaneous flap from the left gluteal area following sacrectomy. Postoperative suture detachment in the midline yielded the large defect with radionecrosis
Debridement revealed that the necrotic area extended to the muscle of the utilised left myocutaneous gluteus maximus flap, and also to the right gluteal area where no surgery was done before. As soon as 3 days after debridement, further necrosis occured on the area possibly due to the recent RT.
A second debridement followed by immediate reconstruction was planned. At the end of the second debridement neurovascular structures, distal lumbar vertebra and mesocolon were all left exposed. All of the left gluteus maximus muscle and approximately half of the right gluteus medius muscle and left gluteus medius muscle were found to be radionecrosed. For reconstruction of the defect, an omentum flap was planned.
Surgical technique
Previous abdominal incision was used for exposure. The splenic and hepatic flexuras were taken down to mobilise the transverse colon to bring the omentum into a retrocolic position. The omentum was elevated on the right gastroepiploic artery [Figure 2] together with the General Surgery team. The left gastroepiploic artery and short gastric arteries were clipped. A tunnel was formed within the Petit triangle inferior to the right kidney. The omentum flap was passed through this tunnel and adapted to the sacral defect [Figure 3]. Surface of the flap was grafted with split thickness skin graft. The abdomen was closed and drains were placed under the reconstructed area and the abdomen which in turn were removed on the postoperative 3rd day.
Figure 2.
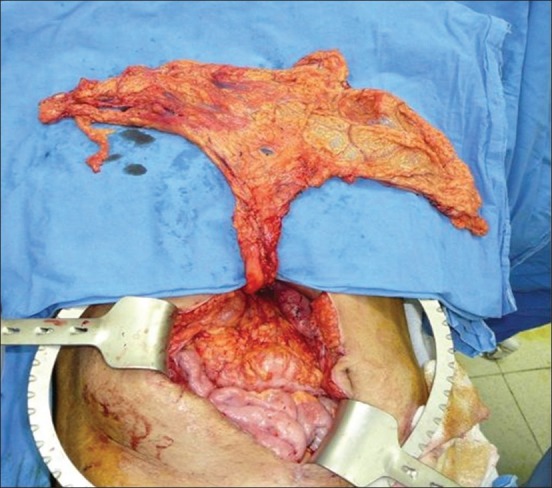
The omentum flap based on the right gastroepiploic artery was raised
Figure 3.

The omentum was passed through the Petit triangle and adapted to the sacral defect
Postoperatively the wound exhibited purulent disharge and there was partial graft loss. Frequent dressing changes and negative pressure wound dressing was applied over the split skin graft for the following 2 weeks. The most frequent bacteria isolated in cultures were Escherichia coli, Pseudomonas aeruginosa, Proteus vulgaris, and Klebsiella pneumonia. The antibiotherapy of the patient was arranged by the hospital ınfection committee according to the tissue cultures. The wound healed without any further surgical intervention, by secondary intention, in the next 6 weeks. He was mobilised at the end of the 4th postoperative week. He had a slight compromise in dorsiflexion of his right foot which recovered during the postoperative follow-up period. During the 1-year follow-up, no recurrence was encountered [Figure 4].
Figure 4.

Postoperative result of the omentum flap 1 year after reconstruction of the lumbosacral area
DISCUSSION
Radiation therapy is typically combined with wide surgical resection in large sacral giant cell tumours.[3] Total or partial en bloc sacrectomy can enhance local tumour control and overall patient survival despite potential complications and neurologic dysfunction.[3] Resection of these tumours usually results in large defects since sacral giant cell tumours usually develop in an eccentric position but commonly extend to involve both sides of the midline and into the presacral space.[3]
For reconstruction of these large sacral defects, bilateral gluteal V-Y advancement skin flaps or perforator flaps, musculocutaneous flaps and skin rotation flaps can be used.[4] It is important that both superior and inferior gluteal arteries be intact and gluteal tissues not be compromised as a result of intraoperative arterial injury or preoperative RT. In our case, gluteal tissues were severely affected by preoperative RT. Complete necrosis of the gluteal rotation flap may be the result of the effects of RT applied 1 month prior to the patient's second surgery. Miles et al.[4] have advocated using transpelvic vertical rectus abdominis muscle (VRAM) flaps in patients for whom local flap options are contraindicated. They detached the flap from the pubis and advanced the pelvis inset of the flap into the sacral defect.[4] Since our patient had colostomy and an abdominal approach incision, it was impossible to rely on the VRAM flap for reconstruction. When neither local flaps nor transplevic VRAM flap can be used, free flap reconstruction may be performed. If superior and inferior gluteal arteries cannot be used due to RT, femoral artery and vein may be used as recipient vessels. Miles et al.[4] have used vein grafts when they used the femoral vessels as the recipient artery and vein in one of their cases.
Another flap that is pliable, successfully fills dead spaces and has the ability to induce angiogenesis is the omentum flap.[5] This flap has a very good blood supply and is known to initiate immune response against an infection.[2,5] This property of the omentum flap has made it particularly useful in treating infected, irradiated and ischaemic wounds.[6] Since the local vascular network was very poor in our patient, the angiogenic properties of the omentum flap itself may have helped the wound healing process in our patient. In addition to these properties, it has great absorbtive potential[6] which we believe has helped lessen the purulant drainage of the wound of our patient.
The omentum flap has been used as a pedicled flap in chest wall reconstruction,[7] pelvic floor reconstruction,[5] penile[8] and scrotal reconstruction,[9] and knee reconstruction with two lengthening techniques.[10] Omentum flap interposition has also been used in complex vesicovaginal fistula repair where good-quality tissue interposition for complex fistula is essential for a successful outcome.[11] We have advocated using this flap in reconstruction of an irradiated large sacral wound due to its properties such as good blood supply and easy dissection.
Reconstructive solutions for any soft tissue defect associated with RT are limited. In cases where local flaps and free tissue transfers do not work for large-scale sacral defects, the omentum flap with its rich blood supply, contourability and pliability should be kept in mind by the reconstructive surgeons.
Footnotes
This work was presented at the 6th congress of the World Society for Reconstructive Microsurgery (WSRM) in 2011.
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Strauch B, Vasconez LO, Hall-Findlay EJ, Lee BT. Grabb's Encylopedia of Flaps. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2009. pp. 1283–321. [Google Scholar]
- 2.O’Shaughnessy BA, Dumanian GA, Liu JC, Ganju A, Ondra SL. Pedicled omental flaps as an adjunct in the closure of complex spinal wounds. Spine (Phila Pa 1976) 2007;15(32):3074–80. doi: 10.1097/BRS.0b013e31815cffe2. [DOI] [PubMed] [Google Scholar]
- 3.Ruggieri P, Mavrogenis AF, Ussia G, Angelini A, Papagelopoulos PJ, Mercuri M. Recurrence after and complications associated with adjuvant treatments for sacral giant cell tumor. Clin Orthop Relat Res. 2010;468:2954–61. doi: 10.1007/s11999-010-1448-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miles WK, Chang DW, Kroll SS, Miller MJ, Langstein HN, Reece GP, et al. Reconstruction of large sacral defects following total sacrectomy. Plast Reconstr Surg. 2000;105:2387–94. doi: 10.1097/00006534-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Hultman CS, Sherrill MA, Halvorson EG, Lee CN, Boggess JF, Meyers MO, et al. Utility of the omentum in pelvic floor reconstruction following resection of anorectal malignancy: patient selection, technical caveats, and clinical outcomes. Ann Plast Surg. 2010;64:559–62. doi: 10.1097/SAP.0b013e3181ce3947. [DOI] [PubMed] [Google Scholar]
- 6.Schmidek AK, Warren SM, Tantillo MB, Morris DJ. Salvage treatment of an irradiated, infected lumbosacral wound. Ann Plast Surg. 2005;55:531–4. doi: 10.1097/01.sap.0000178805.90185.59. [DOI] [PubMed] [Google Scholar]
- 7.Aquilina D, Darmanin FX, Briffa J, Gatt D. Chest wall reconstruction using an omental flap and Integra. J Plast Reconstr Aesthet Surg. 2009;62:e200–2. doi: 10.1016/j.bjps.2009.01.089. [DOI] [PubMed] [Google Scholar]
- 8.Sarlak AY, Buluc L, Alc T, Alponat A. Degloving injury of pelvis treated by internal fixation and omental flap reconstruction. J Trauma. 2006;61:749–51. doi: 10.1097/01.ta.0000222548.24368.6c. [DOI] [PubMed] [Google Scholar]
- 9.Isken T, Alagoz S, Unal C, Onyedi M, Utkan Z, Dillioglugil O. A new technique for reconstruction of the avulsed scrotum: The ‘3D- prefabricated omental flap’. J Plast Reconstr Aesthet Surg. 2009;62:410–2. doi: 10.1016/j.bjps.2008.04.065. [DOI] [PubMed] [Google Scholar]
- 10.Sarlak AY, Tosun B, Buluc L, Cubukcu A. A comparison of two omental lengthening techniques by pedicled omentum to close a knee disarticulation defect: A case report. Eur J Plast Surg. 2008;30:239–43. [Google Scholar]
- 11.Ockrim JL, Greenwell TJ, Foley CL, Wood DN, Shah PJ. A tertiary experience of vesico-vaginal and urethro-vaginal fistula repair: Factors predicting success. BJU Int. 2009;103:1122–6. doi: 10.1111/j.1464-410X.2008.08237.x. [DOI] [PubMed] [Google Scholar]


