Abstract
Background:
This cross-sectional retrospective cephalometric study was designed to clarify whether the maxillary deficiency seen in surgically treated individuals with non-syndromic complete unilateral cleft lip and palate (UCLP) is due to inherent growth potential or iatrogenicity.
Materials and Methods:
72 adult individuals were randomly selected in the age range of 12-20 years, and were divided into two groups. Group I had 47 untreated individuals. Group II consisted of 25 surgically treated individuals. Lateral and frontal cephalograms of the selected individuals were taken and analysed using Nemoceph software.
Results:
Group II showed a marked reduction in the cranial base angle, maxillary base length, anterior and posterior maxillary positions, palatal plane angle, maxillary width, maxillary height, occlusal plane height, nasal width and nasal height.
Conclusion:
Surgical intervention does interfere with growth in the facial region. This could be attributed to the scar tissue in lip and palate region, which has a restraining effect on growth in the facial region. These altered functional matrices play a significant role in determining the growth of facial structures.
KEY WORDS: Cephalometrics, cleft lip and palate, surgically treated adults, surgically untreated adults
INTRODUCTION
Cleft lip and palate (CLP) is the second most common congenital anomaly affecting the human race. The incidence of this disorder is affected by race, with the Mongoloid race having a higher incidence than Caucasians and Caucasians have higher incidence than Negroids. Cleft lip with or without cleft palate occurs in approximately 0.91–2.69 in 1000 White births.[1] Multiple protocols for the management of CLP have been suggested over the years by various authors.
The most controversial issues in the management of cleft palate are the timing of surgical intervention, speech development after various surgical procedures and the effects of surgery on facial growth. Williams et al.[2] examined repaired cleft patients at 5 and 12 years of age and observed that 40% of the patients at 5 years of age had poor dental arch form and 70% at 12 years of age had midfacial retrusion. The abnormal facial morphology in treated cleft patients has been attributed to two factors – intrinsic developmental deficiency and iatrogenic factors introduced by treatment. Bishara,[3] Isiekwe and Sowemimo,[4] and Yoshida and Nakamura[5] claim that maxillary deficiency in cleft individuals is an intrinsic primary defect. However, Ortiz-Monasterio et al.,[6] Bishara et al.,[7] Mars and Houston[8] and Capelozza et al.[9] have written that maxillary deficiency is secondary to surgical repair. More recently, Pradip R. Shetye and Carla Evans[10] examined lateral cephalograms of adult unoperated CLP patients for the purpose of clarifying whether maxillary deficiencies observed in treated cleft patients result from intrinsic defects or surgical intervention early in life. They stated that potential for normal growth of the maxilla exists in patients with unilateral CLP (UCLP). It is likely that disturbances of maxillary growth in surgically treated cleft patients are related primarily to the surgical intervention.
The craniofacial growth in CLP is influenced by the inherent genetic growth potential, the functional abnormalities due to cleft and the surgical intervention performed to repair the cleft. The genetically determined components of craniofacial growth in cleft patients can be separated from surgical effects by investigating an unoperated sample. Hence, it was decided to conduct a study using lateral and frontal cephalometric radiographs to evaluate maxillary and mandibular morphology and to clarify whether the maxillary deficiency seen in operated cleft palate patients is due to morbidity or iatrogenic effect of the surgical act.
MATERIALS AND METHODS
The present cross-sectional retrospective study was conducted on lateral and frontal cephalograms of 72 adult individuals with non-syndromic CLP in the age range of 12–20 years. All the individuals (Group 2 cleft, according to International Confederation for Plastic and Reconstructive Surgery)[11] were selected from the Plastic Surgery Department of Sushrut Institute of Plastic Surgery (SIPS), Lucknow (Smile Train Center), and from the Out-Patient Department of Savitri Hospital, Gorakhpur (Smile Train Center).
The subjects were categorised into two groups – Group I and Group II.
Group I consisted of 47 surgically untreated individuals with 27 males and 20 females in the age range of 12–20 years with mean age of 17.65 ± 2.90 years.
Group II consisted of 25 individuals who had been surgically treated at around 14 months of age with no orthodontic intervention for the postoperative morbidity. This group had 13 males and 12 females in the age range of 12–20 years with mean age 17.50 ± 2.59 years.
All the individuals in both the groups were selected according to the following criteria:
They should not be below 12 years of age.
They should possess complete cleft on one side involving palate and lip.
No history of any other surgical procedures performed in the craniofacial region except CLP repair.
No history of previous orthodontic treatment and/or orthognathic surgery.
They should not have any other associated or non-associated congenital malformation or diseases, i.e. non-syndromic.
Only those individuals were selected in whom lip repair was done before 15 weeks and palate closure was performed not later than 14 months of age.
Ethical and written approvals for this study were obtained from the Research Committee of Uttar Pradesh Dental College and Research Center which is recognised by the B. R. Ambedkar University, Agra.
Then digital lateral and frontal cephalograms of the two selected groups were taken and analysed with the help of Nemoceph Software. Data thus obtained were subjected to statistical analysis, the detailed description of which is given below.
Radiographic procedure
The digital lateral and frontal cephalograms of the selected individuals were taken on a Cephalostat machine from Agfa Imaging Systems with KVP of 70 kV and 8 mA at a distance of 155 cm from the source to the midsagittal plane and head oriented to FH plane parallel to the floor with lips in relaxed position and teeth in maximum intercuspation.
These digitised cephalograms were then transferred to Nemoceph software (Nemotec Dental Imaging Systems 2004). On the radiographic image, points and landmarks were located. Five linear and four angular parameters were measured on lateral cephalogram and nine linear and two angular parameters were measured on frontal cephalograms using the software.
Intraoperative error
In order to minimise the error in the measurements of the observer, 10 parameters were randomly selected from lateral and frontal cephalograms and values were measured. Paired “t” test with a maximum permissibility error of 0.5 mm was applied to see the difference among the values recorded earlier and the values repeated after 20 days. No significant difference was found in any of the randomly selected parameters.
The following points and landmarks as seen on lateral cephalogram were used in the present study [Figure 1]: Nasion (N), Sella (S), Pterygomaxillare (Ptm), Point A, Anterior Nasal Spine (ANS), Posterior Nasal Spine (PNS), Orbitale (Or), Porion (Po), Articulare (Ar), Basion (Ba), Sellion (Se).
Figure 1.
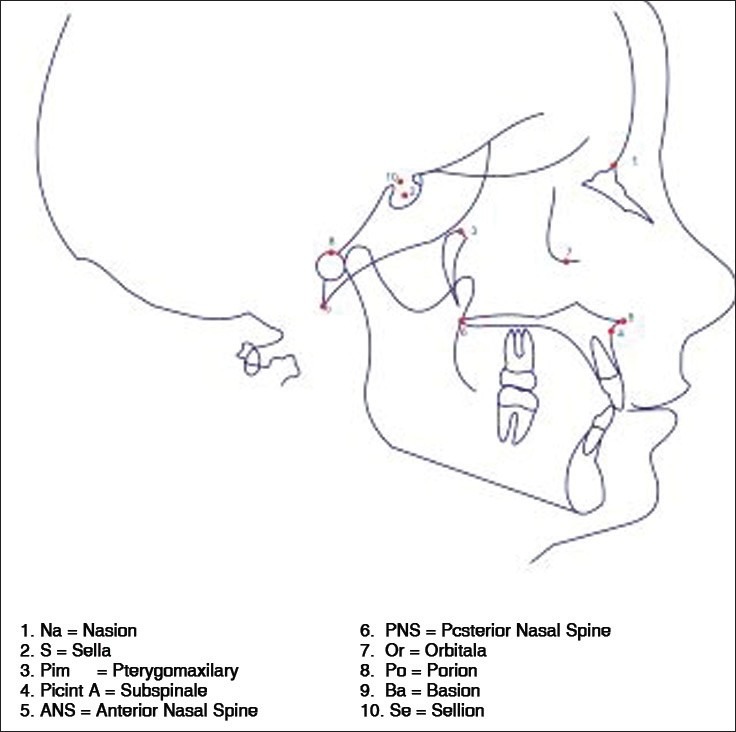
Reference points in sagittal plane
The following points and landmarks on frontal (PA) cephalograms were considered in the study, as outlined by Shah,[12] Grummons[13] and Ricketts[14] [Figure 2]: Cg, Z point ZA/AZ, NC, J/J’ point, antegonial point (AG/GA), ANS, Menton (Me).
Figure 2.
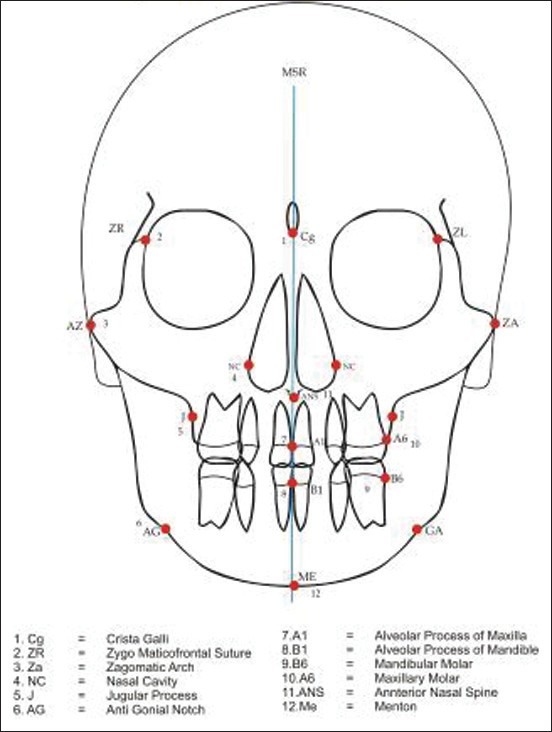
Reference points in frontal plane
Parameters
The following parameters were considered in the study:
Anterior cranial base length (N-S), posterior cranial base length (S-Ba), cranial base angle (N-S-Ba), as shown in Figure 3. Linear measurements of the nasomaxillary complex [Figure 4]. Maxillary length (PNS-ANS), anterior maxillary position, posterior maxillary position.
Figure 3.
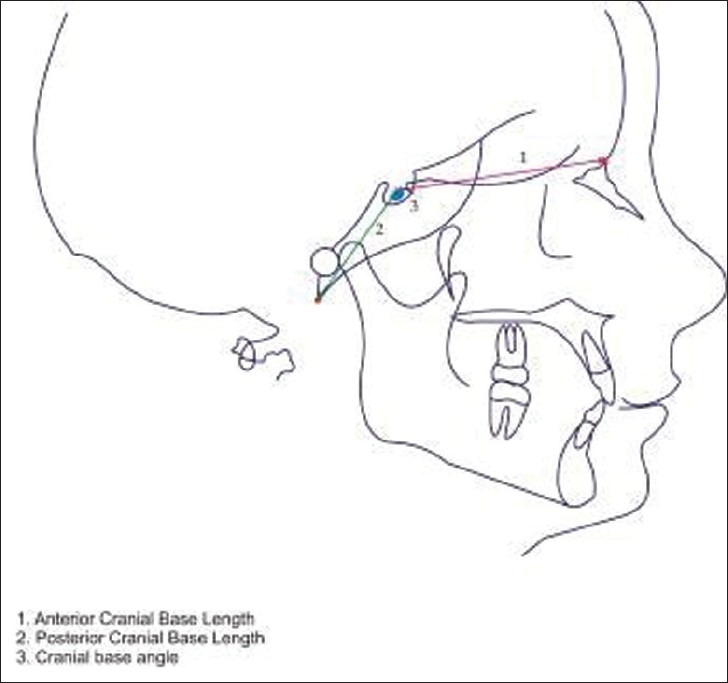
Measurements of cranial base
Figure 4.
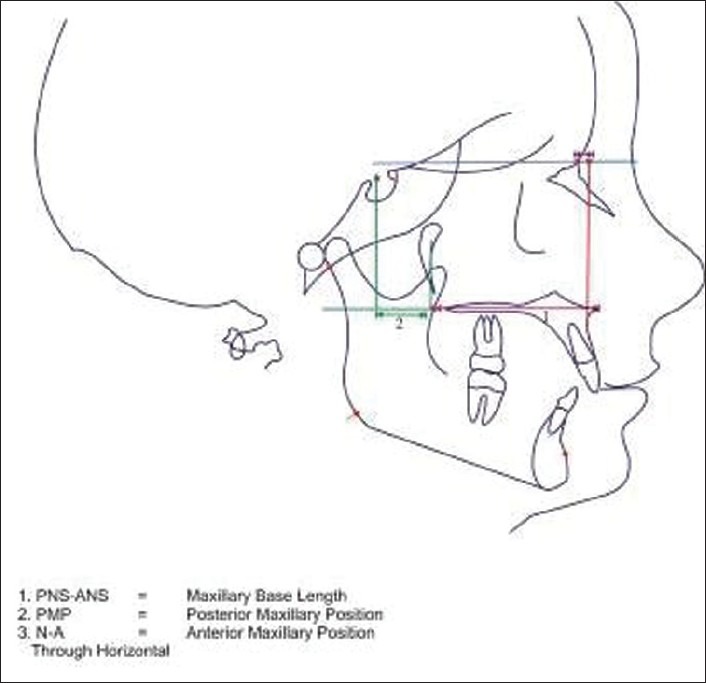
Linear measurements of nasomaxillary complex
Angular measurements of the nasomaxillary complex [Figure 5].
Figure 5.
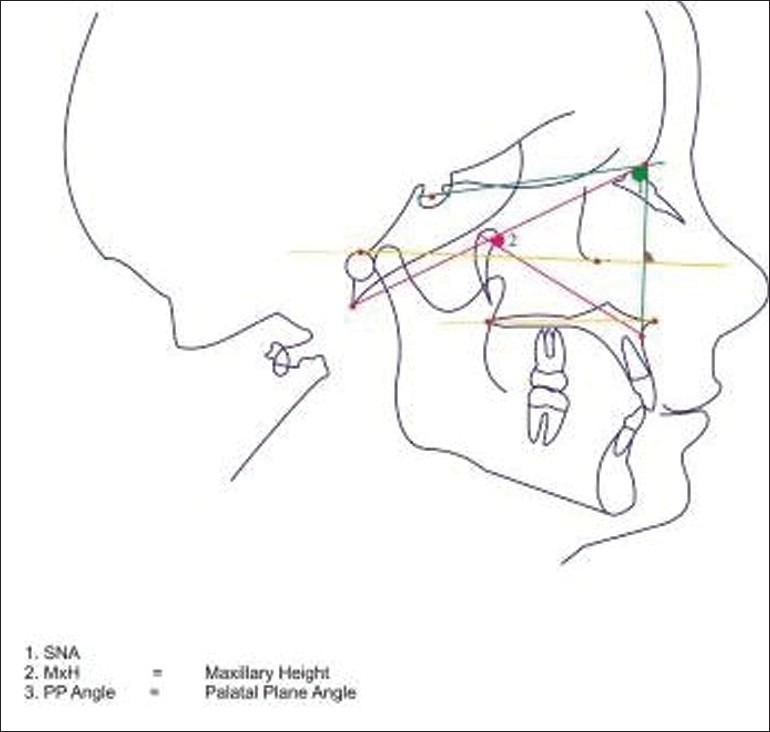
Angular measurements of the maxilla
SNA (SN^NA) convexity (N-A-Pog), maxillary height, palatal plane angle (PNS-ANS – FH).
The following parameters were measured on frontal (PA) cephalograms [Figure 6].
Figure 6.
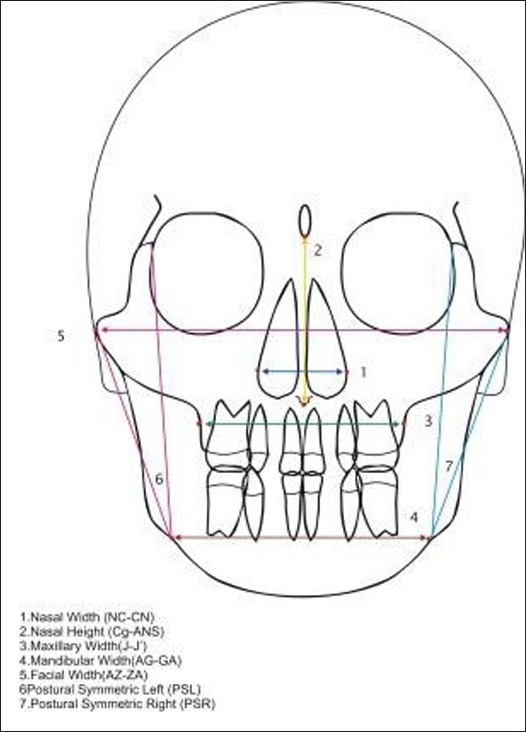
Measurements of nasomaxillary complex in frontal plane
Maxillary width (J-J’ point), mandibular width (AG-GA), facial width (ZA-AZ), nasal width (NC-CN), nasal height, postural symmetric left and right (ZL-AG-AZ).
Additional parameters
To measure these parameters, a real size print out of the tracing was taken on a plane piece of paper. A horizontal plane (HP) was drawn joining lateral orbitale points of left and right sides (LO/LO’), defined as lateral most point on the outer border of orbit, respectively. The midpoint was marked on the HP and a perpendicular was drawn through it and named as midsagittal perpendicular (MSP). All the additional parameters were measured from this constructed MSP. This procedure has been described by Kyrkanides et al.[15] and used by Molsted and Dahl (1990)[16] and other authors.
The parameters measured were: Juglar process height on cleft side, juglar process height on non-cleft side, occlusal plane height on cleft side, occlusal plane height non-cleft side [Figure 7].
Figure 7.
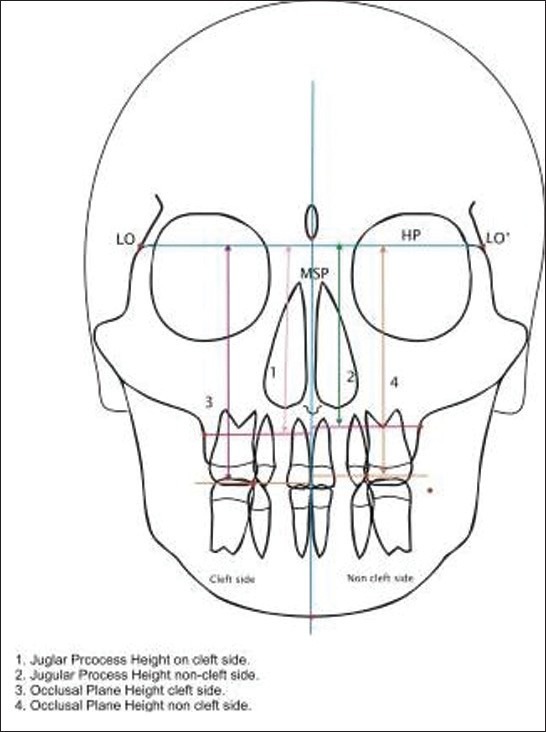
Additional parameters considered in the study
The measurements from the digital frontal and lateral cephalograms of the two groups were recorded and subjected to Student's “t” test to determine the level of significance (P) of the parameters amongst the groups. In order to minimise the error in the measurements of the observer, 10 parameters were randomly selected from lateral and frontal cephalograms and the values were measured. Student's “t” test was applied to see the difference between the values recorded earlier and the values repeated after 20 days. No significant difference was found in any of the randomly selected parameters.
RESULTS
Tracings of digital lateral and frontal cephalograms were performed on Nemoceph software. Five linear and 4 angular variables were recorded on the lateral cephalograms, and 11 linear and 2 angular variables measurements were recorded on P-A cephalograms and the measurements obtained were tabulated [Tables 1 and 2] and subjected to statistical analysis.
Table 1.
Group I versus Group II in sagittal plane
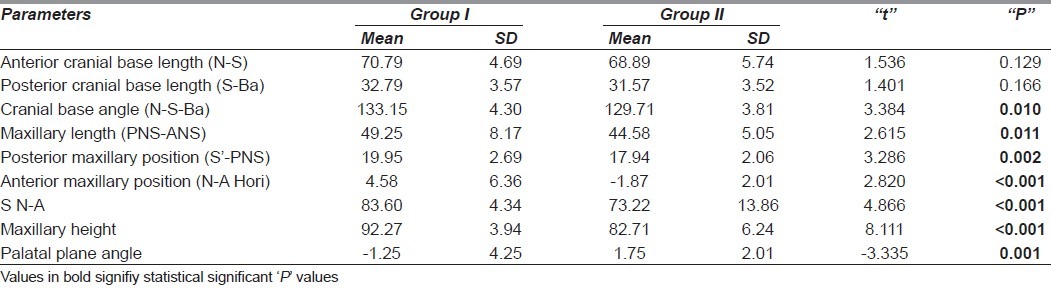
Table 2.
Group I versus Group II in frontal plane
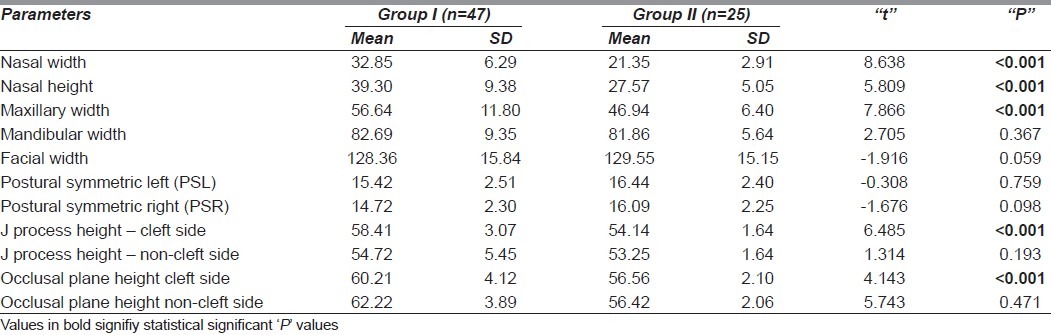
Table 1 shows the overall comparison between Group I and Group II. Table 2 shows the overall comparison between variables in frontal plane.
Cranial base
Among the selected parameters, the cranial base angle showed statistically significant changes in surgically treated individuals (Group II), with a reduction of 3.73°.
Nasomaxillary complex
The maximum changes in maxilla were anticipated and were also found. Maxillary length and spatial positioning of maxilla as depicted by posterior maxillary position and anterior maxillary position showed statistically significant differences between Group I and Group II. The angular measurement also showed significant differences in Group II. There was decrease in the SNA angle, maxillary height angle, convexity and ANB angle. Significant changes were also seen in the palatal plane angle, which reflects a caudal tipping of the palate.
In the transverse plane, the maxillary height, maxillary width, nasal width and nasal height showed marked reduction in their values, reflecting that size of maxilla in the transverse plane is relatively small thereby reducing the nasal height and width. The maxillary height as depicted by juglar process height and occlusal plane height on the cleft side showed significant differences in Group II.
DISCUSSION
The results of our study showed differences in the measurements of the craniofacial skeleton between surgically treated and untreated adults with complete UCLP. The morphology of craniofacial structures in unoperated cleft was more favourable than that observed in surgically treated cleft patients, indicating that surgical intervention interferes with the growth process in CLP patients by altering peri-oral functional matrix.
While evaluating the measurements on lateral cephalograms in the present study, the cranial base angle (N-S-Ba) showed significant difference in the surgically treated UCLP cases as compared to untreated UCLP subjects. The probable cause is ascertained as the flexural angle establishes much before the surgical intervention, though Harris[17] observed a similar finding whereas the observations of Ross[18] and Dahl[19] were contrary to our study.
Maximum changes were observed in maxilla and maxillary dento-alveolar arch, as anticipated. The size, position and rotation of maxilla showed a significant change in surgically treated patients. Maxillary length was found to be significantly reduced in surgically treated UCLP patients. The spatial position of the maxilla, as depicted by posterior maxillary position, showed significant differences. The posterior maxillary position was found to be reduced in surgically treated cases showing posterior shift of the maxillary base. Similar finding was observed when Point A was related to SN plane and FH plane. The facial convexity showed negative values in surgically treated cases as compared to the normal values in surgically non-treated cases.
The reduction in maxillary base length and posterior shift in position might be due to altered peri-oral functional matrix formed by lip, tongue and cheek musculature anteriorly and the pull affect created by postsurgical fibrosis of hard and soft palate. According to Melvin Moss,[20] the growth and maturation of the skeletal component is determined by interplay of genetic and environmental factors, but it is the soft tissue component like lips, tongue and cheek musculature which plays a significant role in the morphogenesis of the nasomaxillary complex.
According to Bardach,[21–23] there is persistent rise in labial pressure in repaired CLP group, which hampers/interferes with the physiological growth process of nasomaxillary complex. Also, Genaro[24] had concluded that there is enhanced electromyographic activity of repaired upper lip muscle during function. Sakuda and Yashuda[25] had claimed a reduction in the cheek pressure after expansion of the buccal segments in repaired CLP group. These studies suggest that alteration in any component of peri-oral matrix can hamper the growth of the related skeletal component.
Comparison of the palatal plane between operated and unoperated cases showed significant differences. This change reflects the rotation of the palatal plane with posterior cranial and anterior caudal tipping and shows the clockwise rotation as the repercussion of surgical repair. The above findings are supported by Ross,[17] Dahl[18] and Smahel and Mullarova,[26] who also reported that maxilla in children with UCLP was in more retruded position. These findings are corroborated by Bardach[21–23] who reported that major source of maxillary growth disturbance is attributed to lip and palate surgery. Hagerty and Hill,[27] Bardach and Eisbach,[28] Bardach and Mooney[29] and Bardach and Kelly[30] also supported this hypothesis. These conclusions are contrary to the findings of Mars and Houston[8] who reported from a similar study that lip surgery without palate surgery did not significantly interfere with antero-posterior position of the maxillary growth. Dahl[19] and Yoshida[5] also found substantial reduction in maxillary prominence in patients with UCLP, who had received lip surgery only.
In the present study, the frontal cephalograms were considered for evaluating the changes in the transverse and vertical plane in complete UCLP patients. No such study had been conducted in the past.
On comparing the transverse measurements of the nasomaxillary complex in surgically treated UCLP with those of non-treated UCLP, very highly significant reduction was observed in nasal width, nasal height and maxillary width in surgically treated UCLP. This could be attributed to the formation of fibrous scar tissue in the palatal region which has significant restraining effect on the transverse maxillary growth. There was no effect on overall facial width and mandibular width. These findings are supported by Smahel and Brejcha[31] who also found the reduced maxillary width with disturbed palatal sutural system. Fogh-Anderson[32] also found that in complete unilateral clefts, the median palatine sutural system has an abnormal position lateral to midline.
The postural symmetry showed no significant differences in surgically treated UCLP and non-operated UCLP cases. This could be due to points taken into consideration as postural symmetry was constructed by the line joining zygomatic arch, antegonial notch and zygomaticofrontal suture on both right and left sides, thus showing statistically no significant changes on zygomatic arch, antegonial notch and zygomaticofrontal suture in UCLP patients.
Additional parameters were considered to segregate the cleft and non-cleft sides in surgically treated and non-surgically treated patients with UCLP. The maxillary height and the occlusal plane on the cleft side showed very highly significant differences in surgically treated individuals with UCLP. The probable explanation to above finding could be that the cleft side contributed to lesser segment with lesser amount of muscular attachments; hence, it was vulnerable to the abnormal muscle pull created post surgically, whereas on the non-cleft side, the differences were insignificant.
To summarise, we can say that surgical intervention does interfere with growth in facial region. This could be attributed to the scar tissue in lip and palate region which has a restraining effect on growth in facial region. These altered functional matrices play a significant role in determining the growth of facial structures.
Within the limitation of this cross-sectional study, we can presume that nasomaxillary complex is the area most affected by surgical intervention in antero-posterior plane and frontal plane. In the antero-posterior plane, the size, position and rotation of maxilla showed definite changes in surgically treated groups compared to untreated groups. These findings suggest that negative effects of surgery do occur, but these iatrogenic effects should be weighed upon the beneficial effects of the surgery that restore the speech function and aesthetics and improve personality of these patients. The surgical act should have minimal tissue manipulation and mobilisation to reduce the formation of fibrous scar tissue, thereby minimising the iatrogenicity. The manipulation or revision of the existing scar by surgery or chemicals should also be considered in a timely manner to minimise the untoward effects of altered growth on nasomaxillary complex.
Most of the previous studies have either considered the individuals of different cleft types[8,33] or compared the cleft individuals with normal population.[34,35] Also, comparison was made between the parents of cleft individuals and the parents of non-cleft individuals.[36–38] The degree of retrusion is proportional to the nature of the surgery, its healing and complications thus incurred. This study is an attempt to quantify the iatrogenic consequence of the surgical act to morbid anatomy with no surgical intervention. However, the degree of insult and methods to avoid or reduce the iatrogenic effects need an extensive detailed protocol which is beyond the realms of the present study.
To further validate the results of our study, a 3D CT scan could be used to compare the findings among the two groups, and a longitudinal study on a larger scale with a larger sample size should be carried out. Even the effect of surgery should be observed among different cleft subtypes to find the effects of surgical intervention on a broader scale.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Vanderas AP. Incidence of cleft lip, cleft palate and cleft lip and palate: A review. Cleft Palate J. 1987;24:216–25. [PubMed] [Google Scholar]
- 2.Williams AC, Bearn D, Mildinhall S, Murphy T, Sell D, Shaw WC, et al. Cleft lip and palate care in the United Kingdom—the Clinical Standards Advisory Group (CSAG) Study. Part 2: Dentofacial outcomes and patient satisfaction. Cleft Palate J. 2001;38:24–9. doi: 10.1597/1545-1569_2001_038_0024_clapci_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 3.Bishara SE. Cephalometric evaluation of facial growth in operated and non-operated individuals with isolated clefts of the palate. Cleft Palate J. 1973;10:239–46. [PubMed] [Google Scholar]
- 4.Isiekwe MC, Sowemimo GO. Cephalometric findings in normal Nigerian population sample and adult Nigerians with unrepaired clefts. Cleft Palate J. 1984;21:323–8. [PubMed] [Google Scholar]
- 5.Yoshida H, Nakamura A, Michi K, Wang GM, Liu K, Qiu WL. Cephalometric analysis of maxillofacial morphology in un-operated cleft palate patients. Cleft Palate Craniofac J. 1992;29:419–24. doi: 10.1597/1545-1569_1992_029_0419_caommi_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 6.Ortiz-Monasterio F, Serrano A, Barrera G, Rodriguez-Hoffman H, Vinageras E. A study of untreated adult cleft patients. Plast Reconstr Surg. 1966;38:36–41. doi: 10.1097/00006534-196607000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Bishara SE, Jakobsen JR, Krause JC, Sosa-Martinez R. Cephalometric comparisons of individuals from India and Mexico with un-operated cleft lip and palate. Cleft Palate J. 1986;23:116–25. [PubMed] [Google Scholar]
- 8.Mars M, Houston WJ. A preliminary study of facial growth and morphology in un-operated males unilateral cleft lip and palate subjects over 13 years of age. Cleft Palate J. 1990;27:7–10. doi: 10.1597/1545-1569(1990)027<0007:apsofg>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 9.Capelozza Júnior L, Taniguchi SM, da Silva Júnior OG. Craniofacial morphology of adult un-operated complete unilateral cleft lip and palate patients. Cleft Palate Craniofac J. 1993;30:376–81. doi: 10.1597/1545-1569_1993_030_0376_cmoauc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 10.Shetye PR, Evans CA. Midfacial morphology in adult unoperated complete unilateral cleft lip and palate patients. Angle Orthod. 2006;76:810–6. doi: 10.1043/0003-3219(2006)076[0810:MMIAUC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Millard DR., Jr . Cleft Craft. 1st ed. Vol. 1. Boston: Little, Brown; 1976. [Google Scholar]
- 12.Shah SM, Joshi MR. An assessment of asymmetry in normal craniofacial complex. Angle Orthod. 1978;48:141–8. doi: 10.1043/0003-3219(1978)048<0141:AAOAIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Grummons DC, Kappeyne Van de Coppello MA. A frontal asymmetry analysis. J Clin Orthod. 1987;21:448–65. [PubMed] [Google Scholar]
- 14.Ricketts RM, Bench RW, Hilgers JJ, Schulhof R. An overview of computerized cephalometrics. Am J Orthod. 1972;61:1–28. doi: 10.1016/0002-9416(72)90172-8. [DOI] [PubMed] [Google Scholar]
- 15.Kyrkanides S, Bellohusen R, Subtenly J. Skeletal asymmetries of the Naso maxillary complex in non-cleft and post-surgical unilateral cleft lip and palate. Cleft Palate Craniofac J. 1995;34:411–6. doi: 10.1597/1545-1569_1995_032_0428_saotnc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 16.Mølsted K, Dahl E. Asymmetry of the maxilla in children with complete unilateral cleft lip and palate. Cleft Palate J. 1990;27:184–90. doi: 10.1597/1545-1569(1990)027<0184:aotmic>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 17.Harris EF. Size and form of the cranial base in isolated cleft lip and palate. Cleft Palate Craniofac J. 1993;30:170–4. doi: 10.1597/1545-1569_1993_030_0170_safotc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 18.Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate: Part 2 repair of lip. Cleft Palate J. 1987;24:5–77. [PubMed] [Google Scholar]
- 19.Dahl E. Craniofacial morphology in congenital clefts of the lip and palate. An X-ray cephalometric study of young adult males. Acta Odontol Scand. 1970;28(Suppl 57):1–61. [PubMed] [Google Scholar]
- 20.Moss ML. The functional matrix hypothesis revisited. 4. The epigenetic antithesis and the resolving synthesis. Am J Orthod Dentofacial Orthop. 1997;112:410–7. doi: 10.1016/s0889-5406(97)70049-0. [DOI] [PubMed] [Google Scholar]
- 21.Bardach J. The influence of cleft lip repair on facial growth. Cleft Palate J. 1990;27:76–8. doi: 10.1597/1545-1569(1990)027<0076:tioclr>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 22.Bardach J, Roberts DM, Yale R, Rosewall D, Mooney M. The influence of simultaneous cleft lip and palate repair on facial growth in rabbits. Cleft Palate J. 1980;17:309–18. [PubMed] [Google Scholar]
- 23.Bardach J, Klausner EC, Eisbach KJ. The relationship between lip pressure and facial growth after cleft lip repair: An experimental study. Cleft Palate J. 1979;16:137–46. [PubMed] [Google Scholar]
- 24.Genaro KF, Trindade Júnior AS, Trindade IE. Electromyographic analysis of lip muscle function in operated cleft subjects. Cleft Palate Craniofac J. 1994;31:56–60. doi: 10.1597/1545-1569_1994_031_0056_eaolmf_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 25.Sakuda M, Yoshida K, Wada K, Kuroda Y, Hayashi I. Changes of cheek pressure during swallowing following expansion of the maxillary dental arch in repaired cleft palates. J Oral Rehabil. 1975;2:145–56. doi: 10.1111/j.1365-2842.1975.tb01525.x. [DOI] [PubMed] [Google Scholar]
- 26.Smahel Z, Müllerová Z. Facial growth and development in unilateral cleft lip and palate during the period of puberty: Comparison of the development after periosteoplasty and after primary bone grafting. Cleft Palate Craniofac J. 1994;31:106–15. doi: 10.1597/1545-1569_1994_031_0106_fgadiu_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 27.Hagerty RF, Hill MJ. Facial growth and dentition in un-operated cleft palate. J Dent Res. 1963;42:412–21. [Google Scholar]
- 28.Bardach J, Eisbach KJ. The influence of primary unilateral cleft lip repair. Cleft Palate J. 1977;14:88–97. [PubMed] [Google Scholar]
- 29.Bardach J, Mooney MP. The relationship between lip pressure following lip repair and craniofacial growth: An experimental study in beagles. Plast Reconstr Surg. 1984;73:544–55. doi: 10.1097/00006534-198404000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Bardach J, Kelly KM. The influence of lip pressure with and without soft tissue undermining on facial growth in beagles. Plast Reconstr Surg. 1988;82:747–5. doi: 10.1097/00006534-198811000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Smahel Z, Brejcha M. Difference in craniofacial morphology between complete and incomplete unilateral cleft lip and palate. Cleft palate J. 1983;20:113–27. [PubMed] [Google Scholar]
- 32.Fogh–Andersen P. Inheritance of hare lip and cleft palate. Cleft Palate Craniofac J. 1999;36:54–65. [Google Scholar]
- 33.Bishara SE, de Arrendondo RS, Vales HP, Jakobsen JR. Dento-facial relationship in persons with unoperated clefts: Comparison between three cleft types. Am J Orthod. 1985;87:481–507. doi: 10.1016/0002-9416(85)90086-7. [DOI] [PubMed] [Google Scholar]
- 34.Sandham A, Cheng L. Cranial base and cleft lip and palate. Angle Orthod. 1988;58:163–8. doi: 10.1043/0003-3219(1988)058<0163:CBACLA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 35.Capelozza Filho L, Normando AD, da Silva Filho OG. Isolated influences of lip and palate surgery on facial growth: Comparison of un-operated and operated male adults with UCLP. Cleft Palate Craniofac J. 1996;33:51–6. doi: 10.1597/1545-1569_1996_033_0051_iiolap_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 36.Nakasima A, Ichinose M. Characteristics of craniofacial structures of parents of children with cleft lip and/or palate. Am J Orthod. 1983;84:140–6. doi: 10.1016/0002-9416(83)90178-1. [DOI] [PubMed] [Google Scholar]
- 37.Suzuki A, Takenoshita Y, Honda Y, Matsuura C. Dento craniofacial morphology in parents of children with cleft lip and/or palate. Cleft Palate Craniofac J. 1999;36:131–8. doi: 10.1597/1545-1569_1999_036_0131_dmipoc_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 38.Raghavan R, Sidhu SS, Kharbanda OP. Craniofacial pattern of children having cleft lip and/or cleft palate anomaly. Angle Orthod. 1994;64:137–44. doi: 10.1043/0003-3219(1994)064<0137:CPOPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]


