Abstract
Background:
Extensive liposuction along with limited dissection of abdominal flaps is slowly emerging as a well proven advantageous method over standard abdominoplasty.
Materials and Methods:
A retrospective study analyzed 146 patients managed for the abdominal contour deformities from March 2004 to February 2010. A simple method to project the post operative outcome by rotation of a supine lateral photograph to upright posture in 46 patients prospectively has succeeded in projecting a predictable result. All patients were encouraged to practice chest physiotherapy in ‘tummy tuck’ position during the preoperative counseling. Aggressive liposuction of entire upper abdomen, a limited dissection in the midline, plication of diastasis of rectus whenever indicated, panniculectomy and neoumblicoplasty were done in all patients.
Results:
The patients had a mean age of 43, youngest being 29 and oldest 72 years. Majority were of normal weight (94%). Twelve were morbidly obese; 57 patients had undergone previous abdominal surgeries; 49 patients had associated hernias. Lipoabdominoplasty yielded a satisfactory result in 110 (94%) patients. The postoperative patient had a definitely less heavy harmonious abdomen with improved waistline. The complications were more with higher BMI, fat thickness of more than 7 cm and prolonged operating time when other procedures were combined.
Conclusions:
Extensive liposuction combined with limited dissection method applied to all abdominoplasty patients yielded consistently safe, reliable and predictable aesthetic results with less complications and faster recovery. The simple photographic manipulation has helped project the postoperative outcome reliably. The preoperative chest physiotherapy in tummytuck position helped prevent chest complications.
KEY WORDS: Lipoabdominoplasty, liposuction, limited dissection, neoumblicoplasty, sliding flap
INTRODUCTION
The casual approach to abdominoplasty by many surgeons result in unfavourable results and unhappy patients. The abdomen bears the brunt of weight gain or loss, pregnancy and abdominal surgeries. It becomes an area with weak anterior wall which is prone for hernias and sagging panniculus. An ideal reconstructive method should address the adiposity, loose skin and stretched out musculoaponeurotic system to yield a functional and aesthetic appearing abdomen with its landmark identity-the umbilicus.
The surgical approach to improve the abdomen aesthetically as well as functionally has been of great interest to surgeons ever since the abdominoplasty was first reported in the literature.[1] The indication is usually aesthetic in western world whereas in India and Middle-East it is mostly functional till today, for easy ambulation, hygiene and relief from back pain. The technique of abdominoplasty keeps improving, functional improvement and aesthesis being the goals of these modifications. The land mark changes were the conversion from vertical incision to a low transverse incision in the 1960[2] and the addition of liposuction in 1983.[3] Various incision designs[4] and plication methods[2] have been described by many plastic surgeons. Since the introduction of liposuction by Illouz[5] for localized adiposities and its wider applications all around the trunk and abdomen, concept of approach to abdominoplasty started to change. The cautious tread of liposuction[6] has become a confident step of lipoabdominoplasty. It is apt to quote Illouz here “It is no longer conceivable to aesthetically improve an abdomen without adipoaspiration”.[5]
Daniel Brauman[7] in 2003 had emphasized the importance of intra-abdominal volume which ultimately determined the final outcome of all the steps in an abdominoplasty. Saldanha[8] in 2003, emphasized that the lipoabdominoplasty does not mean just a simple combination of liposuction and the traditional abdominoplasty.
MATERIALS AND METHODS
Retrospective analysis of 146 patients who had undergone lipoabdominoplasty was done from March 2004 to February 2010 [Table 1] Since 2003, when the author started doing lipoabdominoplasty and was well convinced about the safety and better esthetic result [Figure 1], all patients with an indication for abdominoplasty irrespective of age, quality of skin, status of musculoaponeutics strength, presence of hernia were submitted for the full lipoabdominoplasty described below. The age group varied from 28 to 70 years. Fifty-seven patients had undergone some abdominal surgeries earlier. Unlike patients reported in western literature, most of the patients were housewives, moderately obese, photoshy, sedentary with history of multiple pregnancies and multiple abdominal surgeries presented for some relief from the hanging panniculus and the discomforts associated with it.
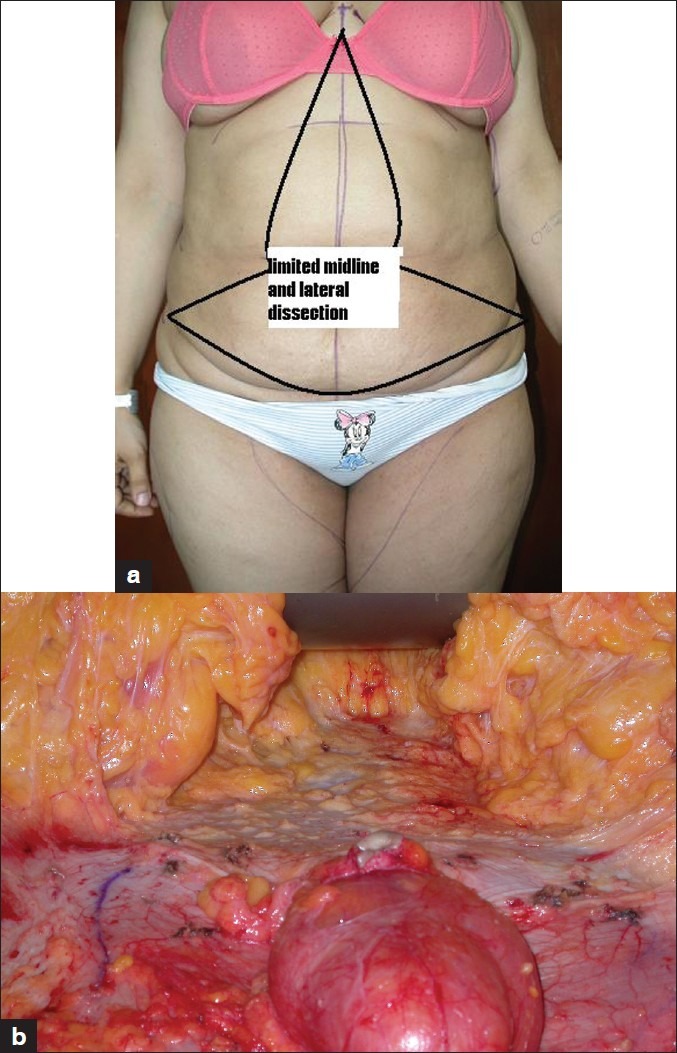
Table 1.
Patient demography
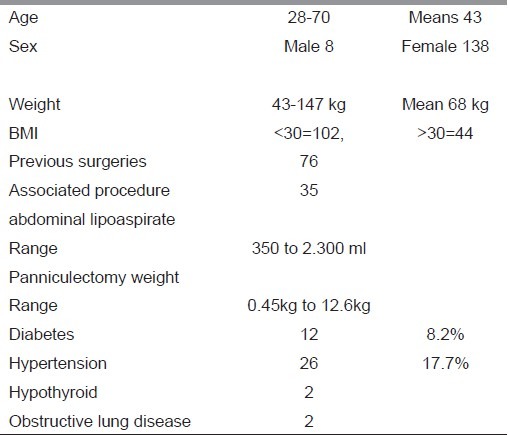
Figure 1.
(a,b,c,d) The pre and post operative result 8 months after Lipoabdominoplasty in a scarred abdomen with skin laxity,and musculoaponeurotic weakness
Minimum weight was 43 kg and maximum was 148 kg and 30% of patients had a BMI more than 30. 17.7% patients were hypertensive on medication 8.2% were diabetic [Table 1].
For the last 46 successive patients a digital picture in the supine position lateral view was taken and rotated upright to a standing position. This picture correlated well with the postoperative lateral view in standing. The patients were shown this view before the surgery [Figures 2 and 3]. The predominant intra-abdominal volume remained protuberant in the supine posture when the divarication is moderate. If there was a significant diastasis of rectus muscles, the intra-abdominal volume may give a false sense of lax abdomen leading to a protuberant abdomen even after the full abdominoplasty with good repair of diastasis.
Figure 2.
(a) Photographic manipulation-pre op profile (b) Pre-op photographic manipulation :patient supine profile (c) Pre-op photographic manipulation: Rotated upright (d) Pre-op photographic manipulation and comparison to post –op result in a flat abdomen.
Figure 3.
Pre-op photographic manipulation and comparison to post-op result in a protuberant abdomen
All patients were encouraged deep breathing exercises on the first consultation. They were taught to hold the hanging panniculus up and in (tummytuck position) [Figure 4] and breath in and out deeply by thoracic excursion. Minimum 2 weeks of this kind of chest physiotherapy was emphasized to minimize the postoperative chest complications. Currently incentive spirometer exercises were also taught during the first visit. In few patients pulmonary function test and echocardiography were also done. Ultrasound examination was done for every patient mainly for any hidden hernia in fatty abdominal wall and to screen for any surprise intra abdominal findings. All these patients were seen and operated in certified surgical centres of Middle-East and India.
Figure 4.

Pre-op chest physiotherapy counseling in ‘tummy tuck ‘ position
Procedure
Markings
In standing posture, the lowermost natural crease was marked and more importance was given to the lateral most end of the inguinal fold. No attempt was made to limit the lateral point. Fatty fold extending to waist line needed an extended excision to get a good waist curve. Fat thickness was marked in different areas planned for liposuction. The hernial sites were highlighted well [Figure 5]. The upper limit of pendulous fold was marked but this did not correspond to the excision level.The upper line of incision was decided after liposuction and the limited flap dissection in the lower lateral and in the midline. Usually the excision level was 2-4 cm higher than the approximate preoperative level.
Figure 5.

Pre-op marking in standing position-back for circumferential lipectomy
General anaesthesia was used in 128 patients. Epidural anaesthesia and sedation was used in 18 patients. Prophylactic LMW heparin was used in high-risk patients. Prophylactic antibiotic was used routinely. Urinary bladder was catheterized in all cases.
Liposuction
Liposuction of the whole upper abdomen and flanks was done in all patients irrespective of the fat thickness, aiming to achieve a fat pinch of 2.5 cm.
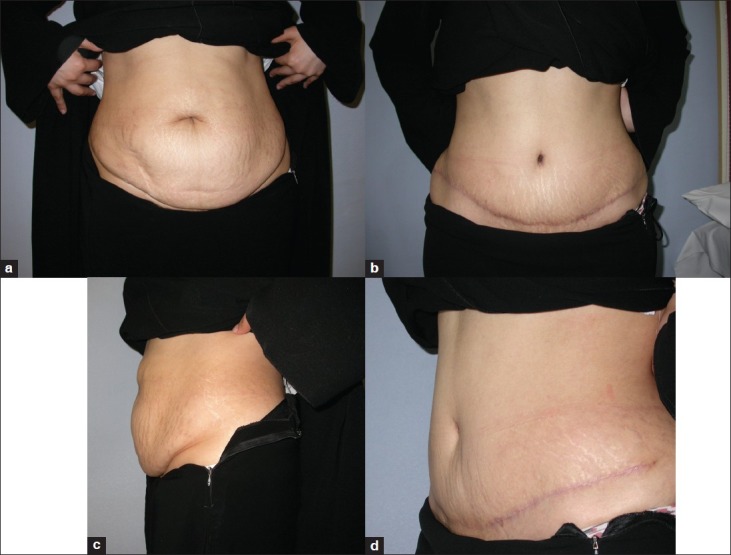
Tumescence was achieved by machine pressure infiltration and a blunt infiltration cannula (Byron's Lamis). Tumescent fluid was Normal Saline 1000 ml, warmed, with 1 ml of Adrenaline 1 in 1000 and 30 ml of 1% Lidocaine. Good turgence was achieved before liposuction. Tumescent fluid infiltration was done sequentially one area after another. Ten to 15 minutes before completion of liposuction on right side, infiltration was started on left side. These sequential steps were used to prevent volume overload and lidocaine toxicity. Both deep and superficial manual liposuction of right side of abdomen and flank, followed by left side and flank were done. Byron No 3 and 4 Accelerator III tip cannulas were used. Upper limit of liposuction was inframammary area and across the epigastrium. Below the umblicus only deep tumescent infiltration was done close to rectus sheath- (plane of dissection) taking care to avoid hernial sacs if any. Infiltration was completed by injecting along the incision line both subdermally and in depth [Figure 6]. Liposuction was not done in the lower abdomen.
Figure 6.
Schematic picture showing areas of tumescent infiltration and liposuction
Flap dissection
Once the liposuction has been completed, the abdominal flaps were incised and mobilized by scalpel dissection. Recently diathermy dissection with pencil tip microdissection needle Colorado, stryker in coagulation mode with power of 40 has helped in bloodless, fasterdissection, mainly in the midline tunnel up to the epigastrium. In patients with median or paramedian scars, the lateral virgin area was dissected first then the scarred area. The plane was superficial to the thin fascial layer above the rectus fascia. Because of the deep tumescence the plane was bloodless. The midline dissection continues up to umbilicus, bisects the pannus and circumcises the umblicus at the shortest stump length possible. The upward dissection was continued on both lateral areas about two inches above the upper limit of the pendulous abdomen. In few patients the flaps slid more than expected necessitating further lateral dissection up during the flap excision.
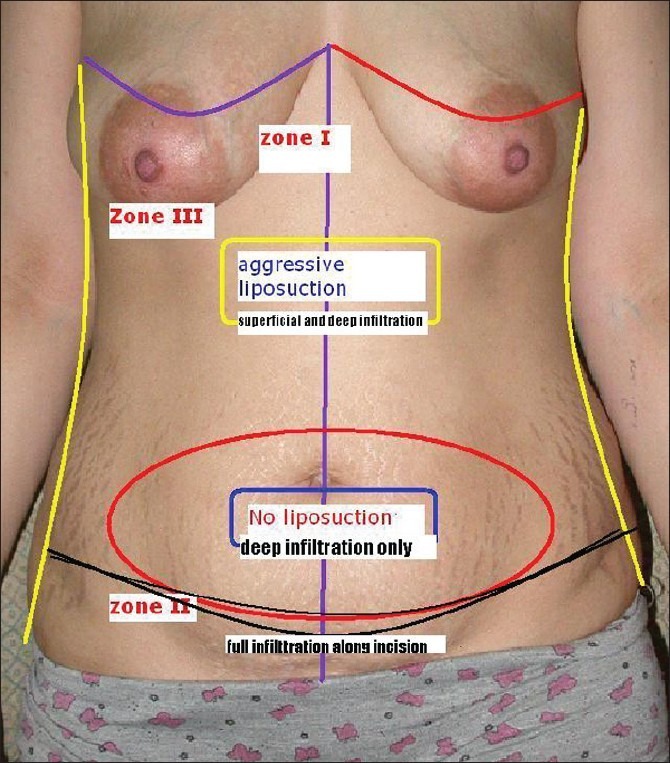
The limited midline dissection above the umbilicus usually stops just lateral to the visible diastasis. The medial border of rectus muscles were well identified. No fixed measurements for lateral extent were followed in the dissection. Midline upward dissection was carried up to a level just about the xiphoid angle. This limited midline dissection was done in all patients irrespective of presence of diastasis or not. This midline dissection probably helps in better sliding of the upper flaps [Figure 7].
Figure 7.
(a) Areas of dissection (b) limited midline dissection
Repair of hernia
At this stage, the hernial repair was done. Anatomical repair was done in most patients.The sac was opened, contents reduced, defect assessed and repaired and the posterior wall reinforced. When adjacent muscles were found to be weak, a polypropyelene mesh was used to reinforce the repair by keeping it under the external oblique muscle. The mesh repair was needed in three patients with port site incisional hernias. [Figure 8].
Figure 8.
(a) A port site in right iliac fossa with incisional hernia And huge pendulous abdomen (b) hernia- mesh repaired and full lipoabdominoplasty (c) two years after surgery
Plication of diastasis recti
The diastasis if present was repaired with 1-Polypropelene. The medial margin of rectus sheath was approximated to that of other side without incising the sheath. If the diastasis was very wide multiple layer plication was done from the midline till the medial border is brought to the midline. When the umbilical stalk is preserved, the plication is done at two levels above umbilicus and below. A continuous suture starting midway between the xiphoid and umbilicus and going up to Xiphoid and returned down crisscrossing the earlier suture up to umbilicus and up to the starting point [Figure 9]. The same way it was repeated below umbilicus upto the symphysis pubis. Umbilical stalk was anchored to the rectus sheath as short as possible during the rectus plication stage and further anchoring was done using 3 0 Vicryl.
Figure 9.
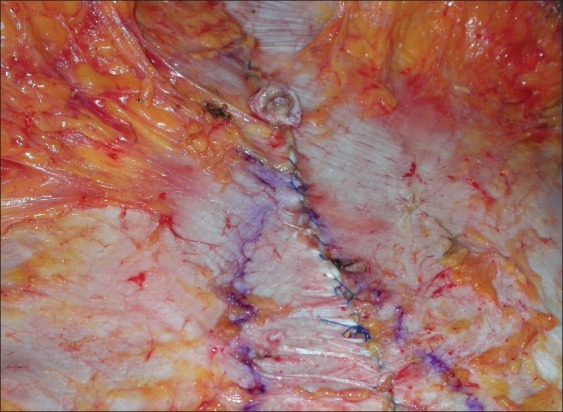
Umbilical stalk telescoped to the anterior rectus sheath
When the umbilicus was fully everted, the same was excised. The umbilical sac was closed with 2 0 vicryl and plication was completed using a single 1 prolene continuous crisscrossing suture from xiphisternum to suprapubic area [Figure 10]. This facilitated easy handling and good strength without any weak area and in less time.
Figure 10.
Diastasis repair by continuous criss cross suturing from Xiphisternum to pubis
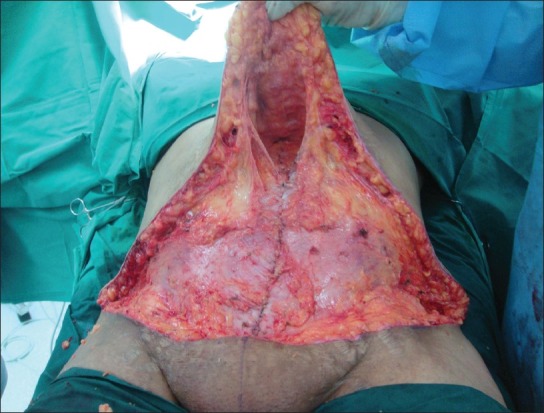
Excessive excision of the pendulous flap
The operating table was brought to semi-Fowler position and hips flexed to about 30° with pillow under the knees. With a central anchoring suture the flaps were gently pulled down and medially and marked at the level of adequate tension. The lateral-most extent of the excision did not extent beyond the initial preoperative marking. The flap was excised 2 cm above the marking and once the dermis was incised, the fat layer was excised tangentially. At this stage if the sliding was greater than the earlier lateral dissection, the flap was carefully dissected further up before excision. Temporary stapling was done from lateral to medial, taking care to adjust the flap length discrepancy.
The same was repeated on the other side.
Planned intra-abdominal procedures like laparoscopic ovarian cyst excision, uterus removal. sterilization, recanalisation, etc. were done at this juncture by releasing the temporary staples.
Sometimes the laparoscopic surgeon did the procedures first using ports below the umbilicus, followed by lipoabdominoplasty.
Neoumblicoplasty
Umblicus was reconstructed in all the patients. The location of new umbilicus was marked in the midline just above a horizontal line connecting the highest point of the iliac crest. An elliptical skin island of 1.5 × 1 cm was incised, lifted up and a cone of subcutaneous fat was excised up to rectus sheath [Figure 11]. The disc of umbilical skin with stalk was brought to the surface at the same site. The umbilical skin was sutured to the abdominal skin at four points. Small raw areas were not sutured. It helps to drain and heals by secondary intention pulling the suture line inside.
Figure 11.
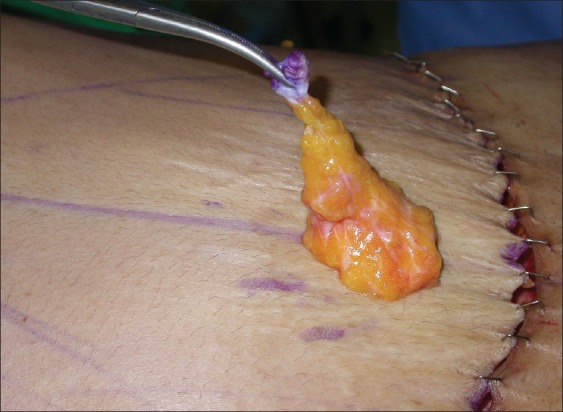
Neoumblicoplasty:disc of skin and cone of fat excision
If umbilicus was everted or part of a hernia, it was sacrificed. An ellipse of skin and a cone of fatty tissue was excised as described. The skin margins were sutured to the rectus fascia with 3 0 prolene at four points [Figure 12]. When the abdominal wall was thin and less fatty,cone of fat was not removed so that depth and the shadow of the umbilicus was maintained.
Figure 12.
(a) When umbilicus was excised,the elliptical skin window was anchored to the rectus sheath.The inflamed areas were sterile fat necrosis (b) six months later,complete resolution and well formed umblicus
Drainage
Because of the limited dissection there was no dead space in the lateral areas. There was a narrow space only in the midline. Two vacuum drains -one from midline and another from the lower space were inserted and brought out at the lateral ends of the incision.
Wound closure
Layered closure was done.2 0 Vicryl was used for the subcutaneous suture taking a good bite of scarpas fascia and the dermis. The staples were removed after good approximation of adjacent areas.A continuous 3 0 Monocryl subcticular suture completes the wound closure.
Dressing
Vertical sterisrips across the suture line and gauze dressings for the wound and the umbilical site was kept. Compression garment was applied before extubation.
The patient was transferred with slightly propped up position with pillow under the knees.
Post operative care
Sips of clear water was started once the anesthesia effect cleared usually 3-4 hours.
The urinary catheter was removed next day morning or earlier . Patient was mobilized as early as the patient felt feasible.Chest physiotherapy was also started at the earliest. Dressing was changed after 24 hours. Drains were removed when the drainage was less than 50 ml totally or usually on the third day. Knee flexion and prop up was maintained for three days.
RESULTS
Table 1 shows the general characteristics of the patients included. The mean age was 45 years and most of them opted for surgery for improvement in activity level, hygiene and appearance. All of them underwent full lipoabdominoplasty except three patients who did not undergo repair of diastasis of rectus. Port site hernias were found in three patients.
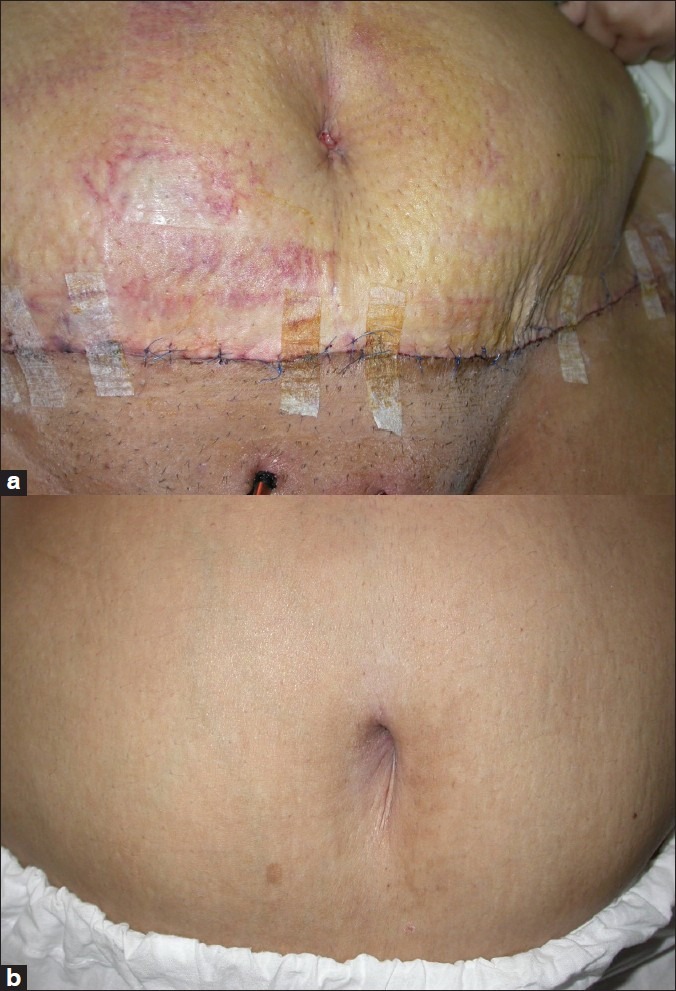
All three patients had huge pendulous abdomen. Repair was done by anatomical layered closure reinforced by polypropelene mesh deep to external oblique muscle. They had no recurrence after 4-years follow-up. A comparison of pre and postoperative photographs demonstrate the consistency of the improvement in the enhanced waist line and harmonious contour of the abdomen and aesthetic appearance of the umbilicus [Figure 13].
Figure 13.

An enhanced waistline and aesthetic umbilicus,after Lipoabdominoplasty of a featureless abdomen
The patient satisfaction was good in 92%, exceeding the expectations. The upper abdominal fullness which was anticipated and projected by the preoperative pictures happened in four patients and one patient was unhappy because of this pot belly appearance after the surgery. [Figure 14].
Figure 14.

An unsatisfied patient with pot belly appearance
Complications
The reported complications after lipoabdominoplasty ranges from 9 to 14%. Lipoabdominoplasty has shown a marked reduction in overall complications.[9] In our series, [Table 2] one young patient 29-year-old had deep calf vein thrombosis who had prolonged surgery over 10 hours for huge breasts along with lipoabdominoplasty. She had associated complications like scalp tenderness due to prolonged pressure followed by patchy alopecia. She recovered from both without sequlae.
Table 2.
Complications
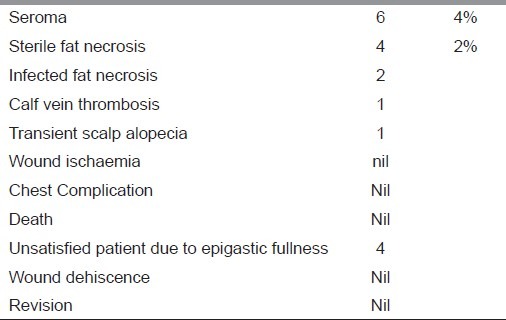
Seroma after abdominoplasty has been reported between 10-12%.[10] In our series six patients (4%) had seroma which needed aspiration three times to dry out the seroma. All these patients had a fatty abdominal wall more than 6-cm thick. Recently before closure, open liposuction was done to get the fat thickness about 3 cm and we found the seroma was observed less in these 16 patients [Figure 15] and drain could be removed early in 3-4 days.
Figure 15.

Open liposuction for reduction of fat thickness
Sterile Fat necrosis was observed in three patients around umbilicus as hyperemic tender nodules which resolved in six months. Infected fat necrosis happened in two patients which got drained through umbilicus and a debridement through the umbilical opening resulted in complete healing in three weeks. All this five patients were over BMI 35 and the thickness of the abdominal wall was above 8 cm even after good liposuction. Open liposuction had not been done in these patients.
None of the patients had ischaemia or necrosis of the flaps inspite of primary reconstruction of the umbilicus, in one patient umbilical site was about 5 cm above the inferior margin.
Thirty-five patients had associated procedures performed – mainly laparoscopy and hysterectomy. There was no increase in incidence of complications in these patients.
The tumescence for liposuction and deep infiltration along the plane of dissection and incision gave a bloodless field and none of the patients received blood transfusion.
The lipoaspirate ranged from 350 to 2300 ml. The excised tissue was 450 g least and 12.6 kg heaviest.
Previously liposuctioned areas were difficult for reliposuction but the sliding movement was not affected. The sliding of the suctioned flap was very limited in one patient who had previous traditional abdominoplasty followed by liposuction. The tough fibrosis following extensive dissection would explain this.
DISCUSSION
Approach to abdominoplasty keeps changing. Safety and aesthetics were the two parameters of concern for these endless efforts. When extensive dissection and aggressive tightening was contemplated unexpected grave complications resulted. When less aggressive approach was followed, the result was not satisfactory.
The benefits of liposuction have been proved well when the indications are correct. Its positive effect on the skin retraction and redraping even in patients older than 40 years have been reported.[11] The liposuction helps the flaps to slide down without the need for the extensive subcostal dissection.[7] Liposuction creates a mesh undermining[5] which results in a sliding flap.
The conventional abdominoplasty is the back bone of this whole concept. The main component is the extensive dissection of the abdominal flap which gives the final result. The same dissection is the cause of various grave complications of conventional abdominoplasty. The individual advantages of liposuction and abdominoplasty when combined judiciously, the resultant benefit was observed to be more than the added benefit of each. This exponential advantage is mainly based on the robust vascularity as proved by the Doppler studies done by Ruth Graf[12] of the abdominal flap which is liposuctioned and minimally dissected. This helps to sculpt the abdominal flap better and reconstruct the umbilicus primarily in all patients with minimal complications. On the contrary when aggressive liposuction was combined with extensive dissection, the inherent risks of each are not simply added but multiplied to produce a cascading effect of all complications.
Inspite of these safety and advantage, the final outcome was not satisfactory in all the patients because of the protuberant appearance in some of them.
It is well mentioned in the Practise parameter[13] that those with a scaphoid abdomen in supine position can expect good flattening following surgery. An abdomen which is still convex due to intrabdominal fat content will not achieve a flat contour postoperatively. The grade of divarication also influences the profile appearance. With large intra-abdominal fat and wide lax divariaction, profile abdomen will look flat or scaphoid.
There is no objective method reported in literature to show the patient who seemed to understand at the time of preoperative counseling, but failed to remember this when she returns unsatisfied about the upper abdominal fullness later. This simple photographic manipulation has consistently helped to project the final results and to remind the patient if comes unsatisfied. When the abdomen was tensely protuberant and not falling freely on supine position, no aggressive repair of the diasatasis was attempted.
Diastasis of rectus muscles, if found more than 2 cm, fascial approximation from xiphisternum to pubic region was done. The author believes that the rectus muscle can effectively work as an support for intra abdominal contents only when their vector is parallel to the midline.[14] When they were grossly separated, each contraction tends to deviate away from the midline and protrude the intrabdominal contents as a ventral hernia and this produces a cascading effect which will accentuate the protrusion [Figure 16].
Figure 16.

Gross diastasis with protrusion of intraabdominal Volume.Repair of diastasis corrected this protrusion
The durability of diastasis repair has been well-documented.[15] The effect of intra-abdominal fat content resulting in the protruded appearance after the surgery has been highlighted by only few authors.[14] The classification based on intra-abdominal fat volume by Daniel[7,16] was an important parameter for evaluation of postoperative outcome.
Although abdominoplasty is considered as a cosmetic surgery procedure, most of the patients had a huge panniculus and associated diastasis. Full lipoabdominolasty was needed to get an aesthetically acceptable harmonious abdomen. It is essentially a functional surgery. Extensive liposuction has been done in all patients irrespective of their age and fat content of the abdominal wall. Even in very thin abdominal wall liposuction was done because it was to facilitate sliding of the flap.
The excessive excision of the pendulous abdomen helped to get an even suture line with no protuberance or curtaining effect later due to weight loss or gain.[17] Due to the poor quality of skin if it failed to redrape later, the excess fold would appear ugly. This excessive excision prevented this possible unfavourable result. None of patients required a revision to correct this overhanging.
The tumescent injection in the deep layers of lower abdomen close to rectus sheath and along the incision lines helped to get a bloodless field of dissection. None of these patients received blood transfusion.
The umbilical reconstruction was done primarily in all the patients and even when the site was very close to the margin of the flap there was no occurrence of vascular compromise of the skin flaps.
The new umbilicus, created out of skin and subcutaneous excision and left to heal by secondary healing, has given an aesthetically good looking umbilicus. When one considers the fact that the umbilicus is the only acceptable scar in the body, it is rather natural or proper on the part of the Plastic surgeon to replace one scar by another to get a similar or better natural looking one compared to the one which has suffered the brunt of aging, trauma of surgery and hernia, etc.[18]
A delicate balance exists between the extent of surgery and the result. Aggressive liposuction, when combined with conventional abdominoplasty but with limited dissection, yielded a safer and more harmonious abdomen than any other methods described so far. Literature also proves this experience of many authors. The overall outcome is exponentially more aesthetic and safer than the individual advantages of both procedures added together. The robust vascularity of the suctioned flap is the prime factor. The limited dissection of this sliding cobweb not only protects the vascularity but also retains the sensation of the flaps and eliminates most of the dead space which can not collect blood or serum. The liposuction removes the extra load of fat, releases the fibrous attachments and stretches the neurovascular bundles resulting in a sensate sliding flap.[16]
This robust flap emboldens one to remove extra inch of panniculus and primary reconstruction of umbilicus.
Previous surgeries did not influence the procedure much.[19,20]
Most of the surgeries were below the umbilicus and the scarred area was difficult to dissect, the tumescent infiltration helped to get a bloodless clean field and faster dissection.
Various tension sutures described[21,22] were not practiced here and the incidence of seroma is not high. Although the higher BMI did not increase the wound or systemic complications in women,[10] seroma and fat necrosis were commoner both in men and women when fat thickness was more than 8 cm. The open liposuction before skin closure to achieve a fat thickness between 3 and 5 cm reduced the incidence of fat necrosis and seroma. This concept needs a study with more number of patients to substantiate this result.
The preservation of sensation by this method was proved beyond doubt because after conventional abdominoplasty, women used to complain that they could not feel the loosening of the traditional saree which is tied in the hip region. After lipoabdominoplasty, this complaint was not there. Evidence based on many reports[6,8,19,23,24] stands to show that a good outcome with less incidence of major complications can be achieved by a carefully done lipoabdominoplasty.
CONCLUSIONS
The advantages of lipoabdominoplasty are becoming more obvious and popular.
The preoperative counseling with an objective evidence of the picture of the probable result and the chest physiotherapy in the tummytuck position prepares the patient well both psycologically and physically. The extended use of tumescence, excessive excision of the flap, open liposuction of flap fat and the primary reconstruction of the umbilicus helped us achieve a consistently safe, aesthetically appealing outcome in our series of patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kelly HA. Excision of the fat of the abdominal wall-lipectomy. Surg Gynaecol Obstet. 1910;10:229. [Google Scholar]
- 2.Pitanguy V. Abdominal lipectomy: An approach to it through an analysis of 300 consecutive cases. Plast. Reconstr. Surg. 1967;40:384. [Google Scholar]
- 3.Illouz YG. Body Contouring by Lipolysis: A 5-Year Experience with over 3000 Cases. Plast Reconstr Surg. 1983;72:591–7. doi: 10.1097/00006534-198311000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Pechter EA. The Grid/Staple Adjunct to Abdominoplasty. Plast Reconstr Surg. 2006;118:1624–30. doi: 10.1097/01.prs.0000242505.93367.86. [DOI] [PubMed] [Google Scholar]
- 5.Illouz YG. A new safe and aesthetic approach to suction abdominoplasty. Aesthetic Plast Surg. 1992;16:237. doi: 10.1007/BF00190070. [DOI] [PubMed] [Google Scholar]
- 6.Matarasso A. Liposuction as an adjunct to a full abdominoplasty revisited. Plast Reconstr Surg. 2000;106:1197–102. doi: 10.1097/00006534-200010000-00035. discussion 1203-5. [DOI] [PubMed] [Google Scholar]
- 7.Brauman D. Liposuction Abdominoplasty: An evolving concept. Plast Reconstr Surg. 2003;112:288–98. doi: 10.1097/01.PRS.0000066371.34978.F0. [DOI] [PubMed] [Google Scholar]
- 8.Saldanha OR, de Souza Pinto EB, Matos WN, Jr, Lucon RL, Magalhães F, Bello ÉM. Lipoabdominoplasty without undermining. Aesthetic Surg J. 2001;21:518. doi: 10.1067/maj.2001.121243. [DOI] [PubMed] [Google Scholar]
- 9.Samra S, Sawh-Martinez R, Barry O, Persing JA. Complication Rates of Lipoabdominoplasty versus Traditional Abdominoplasty in High-Risk Patients. Plast Reconst Surg. 2010;125:683–90. doi: 10.1097/PRS.0b013e3181c82fb0. [DOI] [PubMed] [Google Scholar]
- 10.Shermak MA, Rotellini-Coltvet LA, Chang D. Seroma Development following Body Contouring Surgery for Massive Weight Loss: Patient Risk Factors and Treatment Strategies. Plast Reconst Surg. 2008;122:280–8. doi: 10.1097/PRS.0b013e31817742a9. [DOI] [PubMed] [Google Scholar]
- 11.Bank DE, Perez MI. Skin retraction after liposuction in patients over the age of 40. Dermatol Surg. 1999;25:673–766. doi: 10.1046/j.1524-4725.1999.99105.x. [DOI] [PubMed] [Google Scholar]
- 12.Graf R, Araujo LR, Rippel R, Neto LG, Pace DT, Cruz GA. Lipoabdominoplasty: Liposuction with reduced undermining and traditional abdominal skin flap resection. Aesth Plast Surg. 2006;30:1–8. doi: 10.1007/s00266-004-0084-7. [DOI] [PubMed] [Google Scholar]
- 13.Practice parameter for Abdominoplasty and Panniculectomy Unrelated to obesity or massive weight loss: Coding updated. 2007 Jan [Google Scholar]
- 14.Brauman D. Diastasis Recti: Clinical anatomy. Plast Reconst Surg. 2008;122:1564–9. doi: 10.1097/PRS.0b013e3181882493. [DOI] [PubMed] [Google Scholar]
- 15.van Uchelen JH, Kon M, Werker PM. The long-term durability of plication of the anterior rectus sheath assessed by ultrasonography. Plast Reconstr Surg. 2001;107:1578. doi: 10.1097/00006534-200105000-00046. [DOI] [PubMed] [Google Scholar]
- 16.Brauman D, Capocci J. Liposuction Abdominoplasty: An Advanced Body Contouring Technique. Plast Reconst Surg. 2009;124:1685–95. doi: 10.1097/PRS.0b013e3181b98c5d. [DOI] [PubMed] [Google Scholar]
- 17.Uebel CO. Lipoabdominoplasty: Revisiting the superior pull down abdominal flap and new Approaches. Aesthetic Plast Surg. 2009;33:366–76. doi: 10.1007/s00266-009-9318-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramirez OM. Abdominoplasty and abdominal wall rehabilitation: A comprehensive approach. Plast Reconstr Surg. 2000;105:425. doi: 10.1097/00006534-200001000-00069. [DOI] [PubMed] [Google Scholar]
- 19.Heller JB, Teng E, Knoll BI, Persing J. Outcome Analysis of Combined Lipoabdominoplasty versus Conventional Abdominoplasty. Plast Reconst Surg. 2008;121:1821–9. doi: 10.1097/PRS.0b013e31816b1350. [DOI] [PubMed] [Google Scholar]
- 20.El-Khatib HA, Bener A. Abdominal dermolipectomy in an abdomen with pre-existing scars: A different concept. Plast Reconstr Surg. 2004;114:992. doi: 10.1097/01.prs.0000133201.07767.5e. [DOI] [PubMed] [Google Scholar]
- 21.Lockwood T. High-lateral-tension abdominoplasty with superficial fascial system suspension. Plast Reconstr Surg. 1995;96:603. doi: 10.1097/00006534-199509000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Pollock H, Pollock T. Progressive tension sutures:A technique to reduce the local complications in Abdominoplasties. Plast Reconstr Surg. 2000;105:2583–6. doi: 10.1097/00006534-200006000-00047. [DOI] [PubMed] [Google Scholar]
- 23.Avelar JM. Abdominoplasty without panniculus undermining and resection: Analysis and 3-year follow-up of 97 consecutive cases. Aesthetic Surg J. 2002;22:16. doi: 10.1067/maj.2002.121961. [DOI] [PubMed] [Google Scholar]
- 24.Shestak KC. Marriage abdominoplasty expands the mini-abdominoplasty concept. Plast Reconstr Surg. 1999;103:1020–31. doi: 10.1097/00006534-199903000-00042. [DOI] [PubMed] [Google Scholar]





