Abstract
Background:
Cutaneous leishmaniasis (CL) is a widespread tropical infection which has a high incidence rate in Iran. The aim of this study was to determine some epidemiological aspects of disease in Northern Khorasan Province, Iran.
Methods:
From 2005 to 2008, data concerning 1453 patients with CL were collected and analyzed from the different districts of health service registry of the province. The statistical analyses were carried out with SPSS version 12.0 for windows.
Results:
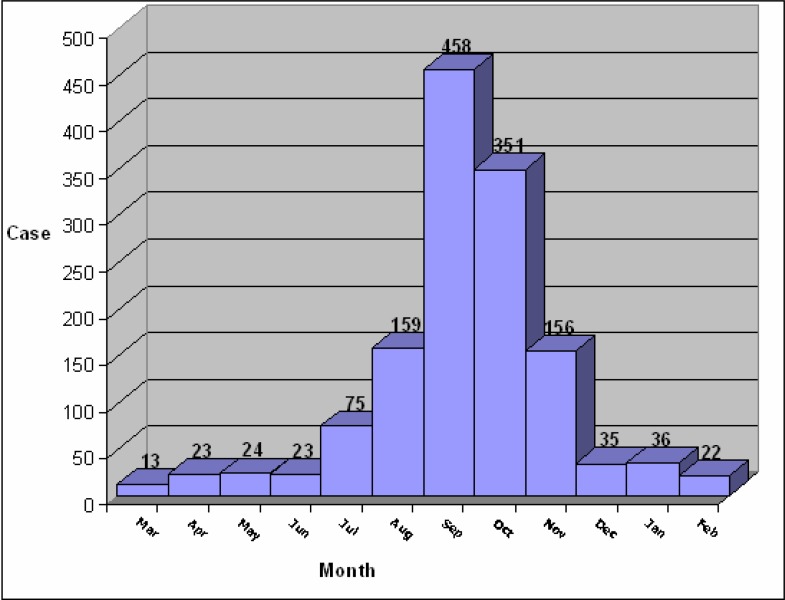
The highest number of patients was in 2005 with 555 cases in this year. 19.3% of patients aged younger than 5-year and 57.5% were older than 15 year. 37.8% had only one lesion, and 40.5% had at least three lesions. The highest incidence of disease was observed in Jajarm district in 2005 (381.1 per 100,000), and the lowest incidence rate was in Farouj district in the same year. The disease was observed in all months of the year with the highest incidence rate from September to November.
Conclusion:
Although Jajrm is a known foci in Iran, based on our knowledge there is no report in the literature on assessing the prevalence of CL in this region in recent years. We also found that the disease is endemic in Northern Khorasan Province.
Keywords: Cutaneous leishmaniasis, Epidemiology, Iran
Introduction
Cutaneous leshmaniasis (CL) is a widespread tropical infection caused mainly by two species of Leishmania, L. tropica and L. major, transmitted by phlebotomus sandflies (Oumeish 1999, Bailey Lockwood 2007). Although CL is endemic in 88 countries in Africa, Asia, Europe and North and South America (Herwaldt 1999), 90% of all cases occur in six countries including Afghanistan, Brazil, Iran, Peru, Saudi Arabia, and Syria (Desjeux 1996). There are an estimated numbers of 12 million cases worldwide, with 1.5–2 million new cases added each year (WHO 1984, 1990).
In the recent years, CL has emerged as a significant cause of morbidity and social stigma in war-torn countries such as Afghanistan (Reithinger et al. 2005). This disease is still a great health problem in Iran. The prevalence of infection has been reported as 1.8% to 37.9% in different provinces of Iran. (Yaghoobi-Ershadi et al. 2002, Talari et al. 2006). Several new foci have been reported in recent years, indicating the potential spread of disease in Iran (Razmjou et al. 2009). The prevalence of disease is high in some provinces of Iran, including Isfahan (Nadim et al. 1968, Nadim and Faghih 1968, Salimi 2000), Shiraz (Moaddeb et al. 1993), Khorasan (Javadian et al.1967), Khuzestan and Kerman (Nadim and Seyedi-Rashti 1971).
The aim of this study was to evaluate the incidence and some epidemiological aspects of cutaneous leishmaniasis in Northern Khorasan Province during 2005 – 2008.
Materials and Methods
From 2005 to 2008, 1453 patients infected with cutaneous leishmaniasis were collected from health service registry of six districts of Northern Khorasan Province, Iran. The patients were diagnosed clinically, para-clinically or both and the diagnosis were confirmed by a physician. A questionnaire about the name, sex, habitation area, date of onset, date of diagnosis, number of lesions, and location of the lesions was completed for each patient.
The statistical analyses were carried out with SPSS version 12.0 for windows.
Results
Table 1 shows the basic characteristics of the study population. The mean age of the study population was 23.2 yr (SD= 18.7) with 19.3% younger than 5 yr, and 57.5% older than 15 yr. The most cases were observed in 2005 with 555 cases.
Table 1:
Baseline characteristics of 1453 patients with cutaneous leishmaniasis in Northern Khorasan Province, Iran: 3/2005–9/2008
| N | ||
|---|---|---|
| Age (yr) (mean ± SD) | 1453 | 23.2 ± 18.7 |
| Female (%) | 624 | 42.9 |
| Number of lesions (%) | ||
| 1 | 549 | 37.8 |
| 2 | 315 | 21.7 |
| >=3 | 589 | 40.5 |
| Location (%) | ||
| Urban | 570 | 60.8 |
| Rural | 884 | 39.2 |
| Diagnosis | ||
| Clinical | 644 | 28.3 |
| Laboratory | 397 | 44.3 |
| Both | 412 | 27.3 |
There was a significant difference between percentage of male and female with cutaneous leishmaniasis (P< 0.001). 37.8% of patients had one lesion, and 40.5% had at least 3 lesions. 42.9% of the patients had lesion on their face.
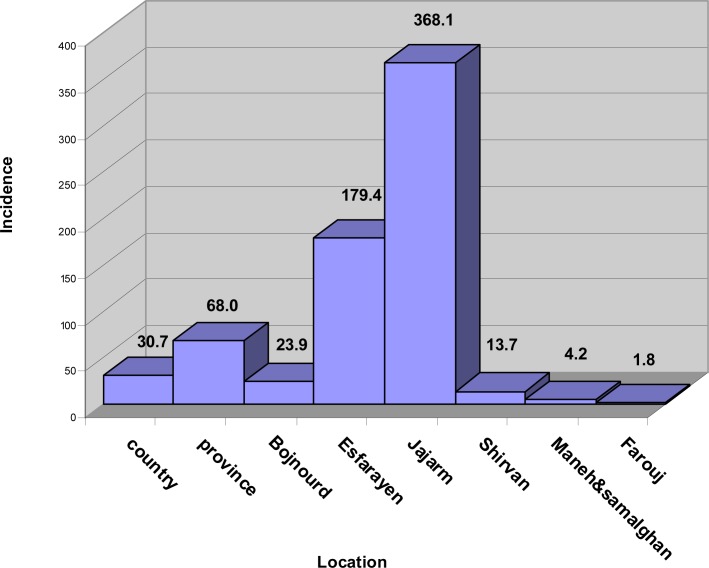
Table 2 shows the distribution of disease stratified by districts in Northern Khorasan Province from 2005 to 2008. Jajarm had the highest (45.4%) and Farouj had the lowest number of the disease (1.4%) during these years. Fig.1 shows the incidence rate of the disease for each district in the study population. The disease was reported in all months of the year with the highest rate from September to November (Fig. 2).
Table 2.
Distribution of 1453 patients with cutaneous leishmaniasis in different districts of Northern Khorasan Province from 3/2005–9/2008
| 3/2005–3/2006 | 3/2006–3/2007 | 3/2007–3/2008 | 3/2008–9/2008 | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| District | n | % | n | % | n | % | n | % |
| Bojnourd | 75 | 13.5 | 45 | 11.8 | 54 | 12.3 | 12 | 15.4 |
| Esfarayen | 235 | 42.3 | 90 | 23.6 | 150 | 34.2 | 16 | 20.5 |
| Jajarm | 218 | 39.3 | 214 | 56.2 | 196 | 44.6 | 31 | 39.7 |
| Shirvan | 22 | 4.0 | 22 | 5.8 | 24 | 5.5 | 12 | 15.4 |
| Maneh & Samalghan | 4 | 0.7 | 4 | 1.0 | 6 | 1.4 | 2 | 2.6 |
| Farouj | 1 | 0.2 | 6 | 1.6 | 9 | 2.1 | 5 | 6.4 |
| Total | 555 | 100.0 | 381 | 100.0 | 439 | 100.0 | 78 | 100.0 |
Fig. 1.
Incidence rate of the cutaneous leishmaniasis in 1453 patients from different districts of Northern Khorasan Province compared with incidence rate in Iran: 3/2005–9/2008
Fig. 2.
Month distribution of 1375 patients with cutaneous leishmaniasis in Northern Khorasan Province-3/2005–3/2008
Discussion
The results showed that Northern Khorasan Province is an endemic area of cutaneous leishmaniasis. We also assessed the prevalence of this disease in details in Jajarm as a known focus in Iran.
Some limitations should be taken into account in this study. First of all, we used the data from health service archive. It is possible that some patients with cutaneous leishmaniasis are visited and treated by physicians out of the province. Based on our knowledge the number of these cases is low and can be ignored. Secondly, since this disease is a self-limited one, some patients might have been cured without any medications. Unfortunately the information about the number of these patients is not available; therefore it is possible that the incidence of the disease were underestimated in the present study. Thirdly, as we used the data about the patients, finding the relationship between the disease and the potential risk factors were not possible.
Age distribution of the disease through this province showed that 19.3% of the patients are under the age of 5 yr. Analyzing the incidence of disease in Iran showed more than 2 times higher incidence in this province. The most likely reason is an increase in human–sandfly contact. This is attributed to the development of villages and the spread of the human population into the habitats of the local vectors.
Although another study has introduced Esfarayen district as a focus of cutaneous leishmaniasis (Javadian et al. 1976), we found Jajarm district as an active focus of the disease in Iran.
We found a significant sex difference for the incidence of cutaneous leishmaniasis. The low incidence of the disease among females could be due to the way of dressing among women in Iran. Another reason is that men normally work outside, considering the reservoirs of the disease, we expect higher incidence of the disease among men.
The month distribution of the disease through the province reflects the rural type of the disease, which is more prominent in two districts (Esfarayen and Jajarm). The month distribution assessment of the disease in each districts showed also some urban foci of disease in the province. These two patterns of distribution of disease are caused by the duration of the disease, which is much longer in the urban type (Nadim 1969). Therefore, the highest number of patients could be found in all month in urban type.
It could be concluded that for successful measures against the cutaneous leishmaniasis in Northern Khorasan Province, we should pay attention more in two districts with high incidence rate, Esfarayen and Jajarm.
Acknowledgments
The authors are grateful for the support of the Deputy of Health of Northern Khorasan University of Medical Sciences who provided data for this paper. The authors declare that they have no conflicts of interest.
References
- Bailey MS, Lockwood DN. Cutaneous leishmaniasis. Clin Dermatol. 2007;25(2):203–11. doi: 10.1016/j.clindermatol.2006.05.008. [DOI] [PubMed] [Google Scholar]
- Desjeux P. Leishmaniasis, Public health aspects and control. Clin Dermatol. 1996;14(5):417–23. doi: 10.1016/0738-081x(96)00057-0. [DOI] [PubMed] [Google Scholar]
- Herwaldt BL. Leishmaniasis. Lancet. 1999;354(9185):1191–9. doi: 10.1016/S0140-6736(98)10178-2. [DOI] [PubMed] [Google Scholar]
- Javadian E, Nadim A, Tahvildare-Bidruni G, Assefi V. Epidemiology of cutaneous leishmaniasis in Iran: B. Khorassan Part V: Report on a focus of zoonotic cutaneous leishmaniasis in Esferayen. Bull Soc Pathol Exot Filiales. 1976;69(2):140–3. [PubMed] [Google Scholar]
- Javadian E, Nadim A, Tahvildari A, Assefi V. Epidemiology of cutaneous leishmaniasis in Korassan Iran. Bull Soc Path Exot. 1967;69:140–143. [PubMed] [Google Scholar]
- Moaddeb A, Gettner S, Ardehali S. Studies on the causative agent of cutaneous leishmaniasis in Shiraz Iran. Iran J Med Sci. 1993;18:28–33. [Google Scholar]
- Nadim A, Mesghali A, Amini H. Epidemiology of cutaneous leishmaniasis in the Isfahan province of Iran. Trans R Soc Trop Med Hyg. 1968;62(4):543–9. doi: 10.1016/0035-9203(68)90141-7. [DOI] [PubMed] [Google Scholar]
- Nadim A, Faghih M. The epidemiology of cutaneous leishmaniasis in Isfahan province of Iran. Trans R Soc Trop Med Hyg. 1968;62:534–542. doi: 10.1016/0035-9203(68)90140-5. [DOI] [PubMed] [Google Scholar]
- Nadim A, Seyedi-Rashti MA. A brief review of the epidemiology of various types of leishmaniasis in Iran. Acta Medica Iranica. 1971;8:99–106. [Google Scholar]
- Nadim A, Rashti AS, Faghih A. Epidemiology of cutaneous leishmaniasis in Iran: B. Khorassan. 3. Human infection. Bull Soc Pathol Exot Filiales. 1969;62(4):702–10. [PubMed] [Google Scholar]
- Oumeish OY. Cutaneous leishmaniasis: a historical perspective. Clin Dermatol. 1999;17(3):249–54. [PubMed] [Google Scholar]
- Razmjou S, Hejazy H, Motazedian MH, Baghaei M, Emamy M, Kalantary M. A new focus of zoonotic cutaneous leishmaniasis in Shiraz, Iran. Trans Roy Soc Trop Med Hyg. 2009;103:727–730. doi: 10.1016/j.trstmh.2008.12.013. [DOI] [PubMed] [Google Scholar]
- Reithinger R, Reithinger R, Mohsen M, Wahid M, Bismullah M, Quinnell RJ, Davies CR, Kolaczinski J, David JR. Efficacy of thermotherapy to treat cutaneous leishmaniasis caused by Leishmania tropica in Kabul, Afghanistan: a randomized controlled trial. Clin Infect Dis. 2005;40(8):1148–55. doi: 10.1086/428736. [DOI] [PubMed] [Google Scholar]
- Salimi M. A clinical and epidemiological comparison on the cutaneous leishmaniasis in the city and villages of Isfahan. Iranian J Publ Health. 2000;2(4):214–219. [Google Scholar]
- Talari SA, Shajari G, Talaei R. Clinical finding of cutaneous leishmaniasis as a new focus of Iran. Internet J Infec Dis. 2006;5(2) [Google Scholar]
- World Health Organization . Report of WHO Expert Committee, Technical Report Series. Vol. 793. Geneva, Switzerland: 1990. Control of leishmaniasis; p. 159. [PubMed] [Google Scholar]
- World Health Organization Report of WHO expert committee. The leishmaniasis, Who Technical Report Series. 1984;701:2–4. [PubMed] [Google Scholar]
- Yaghoobi-Ershadi MR, Hanafi-Bojd AA, Javadian E, Jafari R, Zahraei-Ramazani AR, Mohebali M. A new focus of cutaneous leishmaniasis caused by Leishmania tropica. Saudi Med J. 2002;23:291–4. [PubMed] [Google Scholar]