Abstract
Background:
The aim of this study was that the past five years data were collected to analyze the situation of malaria and health facilities in this area for better understanding malaria problem and to find solutions.
Methods:
In this retrospective study data of the last 5 years were obtained from health center of Bandar Abbas, published papers and reports, weather forecasting organization of the city and annual reports of Hormozgan official authorities. An excel databank was created and analysis was conducted using this software.
Results:
According to the national health system, Bandar Abbas also has referral net work system from periphery to the district health center. The maximum and minimum Annual Parasitic Index (API) were observed in 2005 (1.31) and 2008 (0.17), respectively. The prevalence of cases in villages was more than city, except for 2008. More than 97.6% of indigenous malaria cases were caused by Plasmodium vivax, although P. falciparum, P. ovale and mix infection were also reported. Anopheles stephensi, An. dthali and An. fluviatilis are the main malaria vectors in rural area, while only the first species is distributed in the urban area.
Conclusion:
According to results and many variables including API, Bandar Abbas is divided in two strata. From the situation analysis of Bandar Abbas it is postulated that the main activities of this district could be accuracy of data, and malaria vector control.
Keywords: Malaria stratification, Iran
Introduction
Malaria disease is a worldwide problem that can be found in vast area of the world, where great portions of population are at risk. Unfortunately number of people lost their live because of this disease, and still it is one of the main problems in global health. The disease is transmitted by a variety of female Anopheline mosquitoes (WHO 2009).
Iran is one of the countries that face this problem. Before starting any malaria control program in Iran about 60% of population of the country was living in endemic areas with 30 to 40% malaria morbidity (Edrissian 2006). Iran has been classified into four different strata according to the epidemiology of the disease (Raeisi et al. 2004). At present, malaria problem in Iran is mostly concentrated in southern part. More than 90% of cases are reported from Sistan and Baluchistan, Kerman and Hormozgan Provinces in south-east of the Country (Moosa-Kazemi et al. 2007). It is unstable with two seasonal peaks mainly in spring and autumn. Outbreaks due to P. vivax usually occur after rainy season (Manouchehri et al. 1992). In this part of the country six anopheline mosquitoes including Anopheles culicifacies, An. stephensi, An. dthali, An. fluviatilis, An. superpictus are known proven vectors. Anopheles pulcherrimus was mentioned as suspected malaria vector (Jalali-Moslem 1956, Manouchehri et al. 1972, Eshghi et al. 1976, Manouchehri et al. 1992, Zahirnia et al. 2001, Edrissian 2006). The national strategy on malaria was revised in 2006, with the goal of eliminating of Plasmodium falciparum malaria in 3–4 yr and only introduced cases of P. falciparum might occur, further reducing the number of autochthonous P. vivax malaria in a period of 7 yr. In the third stage of the new strategy, the objective will be a drastic reduction of local transmission of P. vivax in the residual and active malaria foci. At the end of the third stage only 500–700 autochthonous cases could be reported in the country per year.
Reported studies in 2008 show that out of 11460 malaria cases of Iran, 8% was due to P. falciparum, while 90% were infected by P. vivax (Minsitry of Health 2008). In WHO malaria report 2009, Iran showed evidence of a sustained decrease in the number of cases associated with wide scale implementation of malaria control activities. This country is classified as in the pre-elimination stage (WHO 2009).
The aim of conducting a situational analysis is to systematically understand the malaria epidemiology of an area in a very short space of time and the health status, system and resource available for controlling the disease. In succession to planning to go to the district, there is need to use of the information that is already available and analyzing in such a way to understand the problems. The main objective of the situational analysis is to collect the data from respective references such as: health network office, hospital, health centers, communities, metrology department and others for conducting anti-malarial measures.
Bandar Abbas is the most important seaport of Iran in northern part of the Persian Gulf. This city has thousands of passengers from different parts of Iran, as well as shipmen and immigrants from malarious areas of different countries. Regarding to favorable conditions for malaria transmission, the city can be an important focus for the disease in southern Iran. The aim of this study was that the past five years data were collected to analyze the situation of malaria and health facilities in this area for better understanding malaria problem and to find solutions.
Materials and Methods
Study area
Hormozgan Province covers an area of 71139.62 km2. It is located in south of Iran and north of the Persian Gulf. Bandar Abbas is the capital city of the province. It is located in southern part of this province between 54° 53′–56 ° 03′ E and 26 ° 53′–27 °31′ N on flat ground with an average altitude of 9 m above sea level. The nearest elevated area is Geno Mountain, 17 km north of Bandar Abbas. The city has a hot and humid climate. Maximum temperature in summers can reach up to 49° C while in winters the minimum temperature drops to about 5° C. The average of total annual rainfall was 118.44 mm during 2004–2008 and the mean annual relative humidity was 63.4% (www.weather.ir). In 2008 total population was 521657, from which 47% female and 53% male. About 77% of population of this district is living in urban area and 23% in rural area. Foreign population in this year was 15087 (Management and Programming Organization 2008).
Data collection
This study was a retrospective survey conducted using data obtained from health network of Bandar Abbas, as well as published documents on weather, population, history of malaria and previous studies on malaria in this area. The data bank was created in Excel software. Situation analysis and stratification was conducted based on the obtained data.
Results
Health system and general health profile
Health care and public health services in Iran are provided through a national wide net. This network consists of a referral system starting from primary care center in the periphery going through secondary hospital in the capital and tertiary hospital in major cities. The public sector provide primary, secondary and tertiary health services and some of these services such as prenatal care and vaccination are free of charge (Table 1). The private sector plays a significant role in the health care focused on secondary and tertiary health care in urban areas. There are also many non-governmental organizations acting in health issue in Iran. They provide activities in special field like children with cancer, diabetes and thalassemia.
Table 1.
Health facilities in Bandar Abbas, 2004–2008, Bandar Abbas County
| Health facilities | 2004 | 2005 | 2006 | 2007 | 2008 |
|---|---|---|---|---|---|
| Teaching hospitals | 2 | 4 | 4 | 4 | 4 |
| Total district hospitals | 11 | 10 | 10 | 10 | 11 |
| Private hospitals | 7 | 6 | 6 | 6 | 7 |
| Governmental hospitals | 4 | 4 | 4 | 4 | 4 |
| Urban health centers, polyclinics | 54 | 58 | 66 | 73 | 66 |
| Rural health centers | 21 | 21 | 17 | 23 | 19 |
| Health houses | 128 | 131 | 106 | 106 | 107 |
| Laboratories | 33 | 33 | 36 | 37 | 39 |
| Pharmacies | 36 | 32 | 42 | 45 | 46 |
There is one university for medical sciences education in Bandar Abbas and health network is working under vice chancellor for health. Bandar Abbas health facilities during our study period are showed in Table 1 (Management and Programming Organization 2004–2008).
Malaria situation
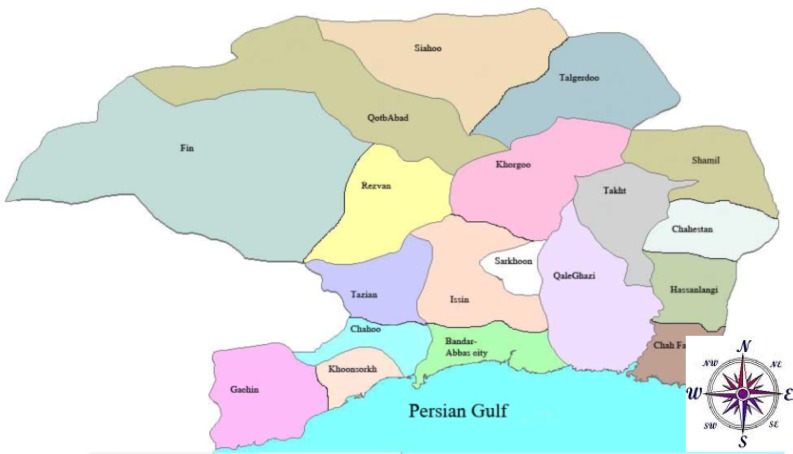
Cases: Based on our findings the malaria cases in Bandar Abbas City are mainly coming from rural areas and from other countries such as Afghanistan and Pakistan, but in rural area most of cases are due to local transmission. All these cases are diagnosed by taking blood and then examined microscopically, and then reported and treated in the public centers. All these activities are free of charge. Usually the cases from the health house reach the health centers within same day and about 80% of slide positive cases (slide examination take less 30 min) get treatment within 24 h according to national guideline. In those areas which are not covered by primary health care system, the anti-malaria activities carried by mobile team. The private sectors can investigate the cases but should refer them to the public sectors for treatment. Bandar Abbas is divided into 19 areas for malaria detection and treatment (Fig. 1).
Fig. 1.
Malaria registration centers of Bandar Abbas, Hormozgan Province, Iran, Bandar Abbas County
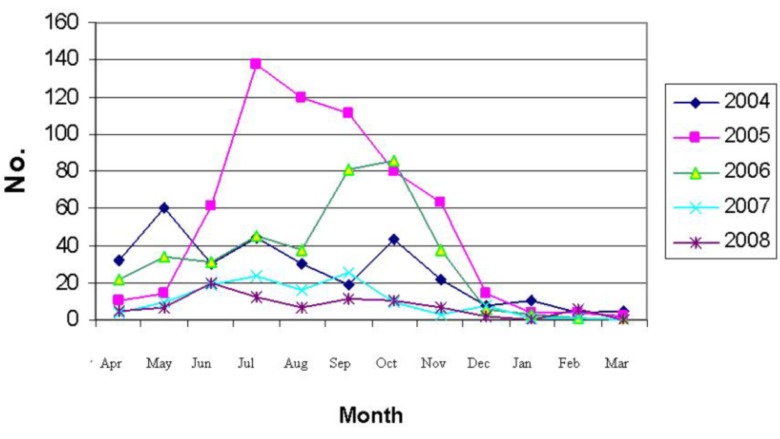
During 2004–2008 a total of 1519 cases were reported to be positive out of 140620 taken slides (Table 2). Most of cases were Iranian (79.3%). The disease morbidity increased up to 2005 and after that had a decreasing trend to 2008. Plasmodium vivax was the main causative agent of malaria in Bandar Abbas (97.69%), followed by P. falciparum (2.17%). There was also one mixed infection case and a report of malaria due to P. ovale detected in an African football player came to Bandar Abbas in 2008. Cases reported in rural area of Bandar Abbas (64.3%) were more than urban area (35.7%). Most of cases (70.7%) had over 14 yr old. Males (64.5%) were infected more than females (35.5%). The transmission season was mainly between April and November (Fig. 2).
Table 2.
Malaria information in Bandar Abbas County, Hormozgan Province, 2004–2008, Bandar Abbas County
| Years | At risk population | Nationality | Sex | Age groups | Species | Total slides | Total cases | API | SPR | ABER | Re-checked slides | Positive from re-checked | Residence place | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||||||||||||
| Iranian | Non-Iranian | Male | Female | <5 | 5–14 | 14< | P. vivax | P. falciparum | Mix | P. ovale | City | Village | |||||||||
| 2004 | 453658 | 160 | 147 | 243 | 64 | 7 | 60 | 240 | 309 | 1 | 0 | 0 | 41174 | 307 | 0.68 | 0.75 | 9.07 | 21414 | 28 | 147 | 160 |
| 2005 | 471816 | 556 | 64 | 362 | 258 | 28 | 166 | 426 | 609 | 11 | 0 | 0 | 34462 | 620 | 1.31 | 1.79 | 7.30 | 15465 | 26 | 164 | 456 |
| 2006 | 479040 | 355 | 30 | 213 | 172 | 35 | 118 | 232 | 378 | 7 | 0 | 0 | 27819 | 385 | 0.8 | 1.38 | 5.80 | 9203 | 17 | 110 | 275 |
| 2007 | 514450 | 95 | 24 | 81 | 38 | 4 | 20 | 95 | 116 | 3 | 0 | 0 | 17247 | 119 | 0.23 | 0.68 | 3.35 | 15078 | 32 | 53 | 66 |
| 2008 | 521657 | 38 | 50 | 81 | 7 | 3 | 4 | 81 | 75 | 11 | 1 | 1 | 19918 | 88 | 0.17 | 0.44 | 3.81 | 13260 | 11 | 68 | 20 |
| Total | -- | 1204 | 315 | 980 | 539 | 77 | 368 | 1074 | 1484 | 33 | 1 | 1 | 140620 | 1519 | -- | 1.08 | -- | 74420 | 114 | 542 | 977 |
API = Annual parasite incidence, SPR = Slide positive rate, ABER = Annual blood examination rate
Fig. 2.
Malaria cases in different months of year during 2004–2008, Bandar Abbas, Hormozgan Province, Iran
Vectors
Previous studies in the area show that Hormozgan Province has five Anopheles vector species, the most important of them are Anopheles stephensi, An. fluviatilis and An. dthali.
Anopheles stephensi is the main malaria vector in Bandar Abbas region, mainly can be found in south urban part, flat and the coastal areas. It considers being endophilic, but biting outdoor during summer months. Its seasonal activity started at beginning of May reach the peak in August and gradually decrease up to December in the mountainous area, but in the coastal areas it is active all the year with two peaks one in the April–May and second in the August up to September (Manouchehri et al. 1976a). Another study reported the peak of activity in September in mountainous and October in coastal regions. This species is absent during the cold winter months, but has high density during spring and autumn in mountainous and coastal region, respectively (Vatandoost et al. 2006). The larva can be found in different bodies of water. In rural areas, it is found in pool streambeds at the margin of the streams, in the seepage and marshy area with gentle flow water, animal hoof print, and around the seepage marsh area (Vatandoost et al. 2004, Vatandoost et al. 2006). Sporozoite rates for An. stephensi were reported 0.2–1.8% from southern part of Iran (Jalali-Moslem 1956).
Anopheles dthali plays a secondary role as malaria vector in Bandar Abbas after An. stephensi. It is found mainly in Siahoo mountainous area, north of Bandar Abbas city. This Anopheles has two peaks of activity during autumn (December–February) and absent during cold winter and hot weather (June–August). The mosquito is resting outdoor in animal house as well as human dwelling (Vatandoost et al. 2007). In rural area of Bandar Abbas, the anthropophilic index and sporozoite rate in salivary glands for this species is reported 25% and 1.4%, respectively (Manouchehri et al. 1972).
The larvae of An. dthali are found in mineral water in high salinity with temperature of 13–28° C and pH of 6.9–8. The larva is most abundant in September and October which is the end of hot season in Bandar Abbas (Vatandoost et al. 2007).
Anopheles fluviatilis is also secondary vector with An. dthali, distributed in mountainous area from the east to west of Hormozgan Province. This species is exophilic, exophagic and zoophilic (Naddaf et al. 2003) with larval habitat in slow moving water on margin of river, stream with or without vegetation with high dissolved oxygen and pits around springs. The biting of this species on human bait started from 18.00 h and continued until 04.00 h, but most of bites on human and cow bait took place in the first half of the night, and there was no bite after 04.00 h (Manouchehri et al. 1975a). Seasonal activity of An. fluviatilis showed two peaks in November and May. This species was active throughout the night with one peak of blood meal, 22:00–23:00 h on animal and 24:00–01:00 h on human (Edalat and Moosa-Kazemi 2005). Sporozoite rate of this species is reported between 1.7–11% in south of Iran (Eshghi et al. 1976).
Vector control
The past program for malaria eradication in Iran was based on vector control using very large quantities of DDT started in 1949 which resulted in dramatic reduction in malaria incidence. Vector population recovery happens mainly due to resistant to DDT in Anopheles stephensi as well as DDT lack of selectivity affecting target population of mosquito (Edrissian 2006). Therefore, other insecticide belongs to organophosphate, organochlorine, carbamate and pyrethroid were used in following years. However, extensive use of chemical insecticides against mosquito vectors for about four decades has resulted in resistance to DDT, dieldrin and malathion (Maouchehri et al. 1992, Edrissian 2006). Susceptibility tests of insecticides against adult mosquitoes using standard impregnated papers provided by WHO showed An. stephensi was resistance to DDT, dieldrin and malathion, while An. dthali and An. fluviatilis are susceptible (Mofidi et al. 1958, Mofidi et al. 1960; Manouchehri et al. 1975b, Manouchehri et al. 1976b, Vatandoost 2004; Vatandoost and Vaziri 2004; Vatandoost and Borhani 2004; Vatandoost et al. 2005). In recent studies, it was found that the field samples of An. stephensi from Bandar Abbas were resistant to DDT, dieldrin and fipronil, and susceptible to other insecticides including malathion in Bandar Abbas (Davari et al. 2006, Vatandoost et al. 2006,). There is also a newly report of tolerance to DDT and dieldrin from Kerman Province (Abai et al. 2008). Study on susceptibility status on An. fluviatilis to diagnostic dose of 10 insecticides including DDT 4%, dieldrin 4%, malathion 5%, fenitrothion 1%, propoxour 0.1%, bendiocarb 0.1%, permethrin 0.75%, deltamethrin 0.05%, lambda-cyhalothrin 0.05% and cyfluthrin 0.15% showed 100% mortality in all tests (Shahi et al. 2006). Evaluation of standard solutions of 5 larvicides against these 3 species from Bandar Abbas showed they were susceptible (Vatandoost et al. 2004, Vatandoost and Hanafi-Bojd 2005, Hanafi-Bojd et al. 2006).
Now the main measures in Iran for malaria vector control are: Indoor residual spraying using Lambda-cyhalothrin WP 10% and deltamethrin WP 10% in malarious areas, larviciding by Chlorpyrifos-methyl, Bacillus thuringiensis and some larvivorous fish like Aphanius dispar and Gambusia affinis and distributing LLINTs. At present, B. thuringiensis and larvivorous fish are using for larviciding in the area as well as impregnated mosquito nets. This measure have been welcomed by people at various level, it was been introduced in 2003 as ITNs and nowadays LLITNs are used in malarious areas of Iran (Moosa-Kazemi et al. 2007).
In Bandar Abbas district, the main measures for vector control are Indoor Residual Spraying (IRS), larviciding and LLITNs. During the period of our study, the vector control activity was restricted to some villages of mountainous area.
Treated mosquito nets were used in May 2005 as ITNs when epidemic started in the area, but now LLITNs are using (personal communications). They are distributed according to the following priorities: Villages without electricity, active foci and high population movement; villages with electricity, active foci and high population movement; villages with only one of the above mentioned factors; villages without electricity.
Larviciding using B. thuringiensis is another vector control measure in the area. It is also limited to the infected villages of mountainous area, north of Bandar Abbas. In addition some other measures are conducted for larval control.
Treatment and drug resistance
In Iran there is no recommended policy for chemoprophylaxis to the pregnant women and travelers. Quinine, chloroquine, fansidar, primaquine, artesunate, clindamycin, doxycychline and coartem are recommended for malaria treatment in Iran. They are used in different combinations based on severity of the disease, age of patient and Plasmodium type. There is also special recommendation for pregnant women (Saebi et al. 2006).
Several studies were carried out on drug resistant in the southern part of Iran. The results of studies during 1968–1976 (Manouchehri et al. 1973, Sutoso et al. 1978) by In vivo test showed that P. falciparum was sensitive to chloroquine, but in 1983 (Edrissian et al. 1985) In vivo and In vitro tests show chloroquine resistant with rate of 5.1% which increased to 51.1% by 1996 (Edrissian et al. 1999). This rate in Bandar Abbas was 32.5% in 1986, 64.8% in 1994–1996 and 68% to 84% by 1997 (Edrissian 2006).
Discussion
There was no considerable change in the number of health facilities during the study period (Table 1). The reduction of health houses that are the first step of the referral system is due to newly geographical changes that pass them to neighbor cities. There was a dramatic increase in malaria cases of 2005 compared to 2004. As showed in Table 2, during 2005–2006 the cases in rural area were more than two times higher than urban areas. There is a limited population movement in the rural area, so this epidemic occurred due to local transmission and this is attributed to the weakness of surveillance system in that years. As it can be seen in Table 2, the total slides taken decrease year by year. Also the amount of insecticides used during epidemic was very limited, e.g. only 400 kg of pyrethroid insecticides and 510 kg Bacillus thuringiensis as larvicide were applied during the epidemic of 2005 (Management and Programming Organization 2005), and the control program started after the first peak of the disease. We found that the entomological data in the area are poor and not enough and reliable for designing a control program. This careless may be due to case reduction in previous years as well as poor entomological data. After this epidemic, different control activities such as LLINTs, IRS and larviciding were strengthened parallel to case detection and treatment resulted to drop positive cases in the area, so that in 2008 the local transmission that usually occurs in rural area was about one third of reported cases in urban area. Reports of health services showed most of cases in Bandar Abbas City in this year were imported.
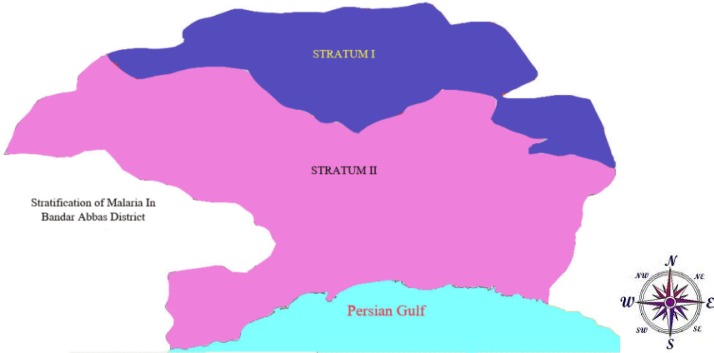
Major determinates of malaria stratification in Bandar Abbas were: geography, vector, water sources, population movement, people behavior and API. Stratification is done based on the above determinates which are illustrated in table 3 and fig 3. So Bandar Abbas were divided into two strata.
Table 3.
Stratification of malaria in Bandar Abbas, Hormozgan Province, Iran 2004–2008, Bandar Abbas County
| Variables | Stratum I | Stratum II |
|---|---|---|
| Geography | Mountainous | Coastal |
| Vector | An. stephensi An. dthali, An. fluviatilis | Mostly An. stephensi |
| Water source | Pools, rivers, and containers | Water pipe, rivers, swage |
| Population movement | No | Present |
| People behavior during transmission season | Sleeping out side | Sleeping in side |
| API | 1%< | <0.5% |
Fig. 3.
Malaria stratification in Bandar Abbas, Hormozgan Province, Iran 2004–2008, Bandar Abbas County
From the situation analysis of Bandar Abbas we found the main problems of this township are: inaccuracy of data and malaria vector control activities. For elimination of malaria in Bandar Abbas it is suggested to do the following activities: Proper case management by early detection and prompt treatment, routine evaluation of drug resistance, biweekly entomological survey during the transmission season in the high risk area, annual survey on susceptibility status of vectors to insecticides/larvicides, free distribution of the LLITNs to at risk groups including travelers and refugees, improving of housing condition at the rural areas, conducting training for entomological survey as larvicidal personnel, spraying workers and response team for epidemics, treatment of breeding site by effective larvicides and biological measures, participation of school children and community in environmental management by drainage and filling the major mosquito sources and small water resources, site selection (establishment of population away from reach of mosquitoes) and introduce of animal shelter between breeding site and human houses for exophilic mosquitoes, personal protection using insect repellents, early detection of epidemics and improvement of data collection, training of staff on computerization, data collection and excel management for updating malaria database, study the health aspect of any project by health authorities and anti malaria services and seek assistant to investigate advantages and benefits, evaluation of knowledge, attitude and practice of people in high risk area by KAP study, and training though mass media (TV, radio) and leadership (community leaders, schools, religious leaders).
Acknowledgments
This study is result of teamwork and field exercise study on malaria situation analysis and stratification, in the 12th International Diploma Course on Malaria Planning and Management, conducted during November 2009-January 2010 in WHO Regional Malaria Training Centre in Bandar Abbas, Southern Iran. We are thankful from the staff of this centre. We would like to thank Dr Masoodi, the director and Ms M Mehranzadeh the focal malaria person in Bandar Abbas health center for their kind collaboration and data providing. The authors declare that they have no conflicts of interest.
References
- Abai MR, Mehravaran A, Vatandoost H, Oshaghi MA, Javadian E, Mashayekhi M, Mosleminia A, Piyazak N, Edallat H, Mohtarami F, Jabbari H, Rafi F. Comparative performance of imagicides on Anopheles stephensi, main malaria vector in a malarious area, southern Iran. J Vector Borne Dis. 2008;45(4):307–312. [PubMed] [Google Scholar]
- Davarai B, Vatandoost H, Ladonni H, Shaeghi M, Oshaghi MA, Basseri HR, Enayati AA, Rassi Y, Abai MR, Hanafi-Bojd AA, Akbarzadeh K. Comparative efficacy of different imagicides against different strains of Anopheles stephensi in the malarious areas of Iran, 2004–2005. Pakistan J Biolog Sci. 2006;9(5):885–892. [Google Scholar]
- Edalat H, Moosa-Kazemi SH. Ecology of Anopheles fluviatilis, the main malaria vector in southern part of Iran, and its role in the epidemiology of malaria. Proceedings of the Fifth International Conference on Urban Pests; 2005 July 10–13; Singapore. 2005. pp. 503–504. [Google Scholar]
- Edrissian GH. Malaria past and present situation in Iran. Iranian J Parasitol. 2006;1(1):1–14. [Google Scholar]
- Eshghi N, Motabar M, Javadian E, Manouchehri AV. Biological features of Anopheles fluviatilis and its role in the transmission of malaria in Iran. Trop Geog Med. 1976;28:41–44. [PubMed] [Google Scholar]
- Jalali-Moslem G. History of malaria and its control in Iran until 1955. Institute of Parasitology and Malariology, Tehran University, Tehran, Iran. Publ No. 1956;225:82–92. [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Jafari R. Susceptibility status of Anopheles dthali and An. fluviatilis to commonly used larvicides in an endemic focus of malaria, southern Iran. J Vect Borne Dis. 2006;43:34–38. Http://www.weather.ir. [PubMed] [Google Scholar]
- Management and Programming Organization Statistical annually report of Hormozgan Province, 2004. 2008. p. 566.
- Management and Programming Organization Statistical annually report of Hormozgan Province, 2004. 2007. p. 594.
- Management and Programming Organization Statistical annually report of Hormozgan Province, 2004. 2006. p. 614.
- Management and Programming Organization Statistical annually report of Hormozgan Province, 2004. 2005. p. 588.
- Management and Programming Organization Statistical annually report of Hormozgan Province, 2004. 2004. p. 550.
- Manouchehri AV, Zaim M, Emadi AM. A review of malaria in Iran, 1957–1990. J Am Mosq Control Assoc. 1992;8:381–385. [PubMed] [Google Scholar]
- Manouchehri AW, Janbakhsh B, Eshghi N, Motabar M. Ecology of Anopheles stephensi Liston in southern Iran. Trop Geog Med. 1976a;28:228–232. [PubMed] [Google Scholar]
- Manouchehri AV, Janbakhsh B, Rohani F. Studies on the resistance of Anopheles stephensi to Malathion in Bandar Abbas, Iran. Mosq News. 1976b;36(3):320–322. [Google Scholar]
- Manouchehri AW, Djanbakhsh B, Eshghi N. The biting cycle of Anopheles dthali, An. fluviatilis and An. stephensi in southern Iran. Trop Geog Med. 1975a;28:224–227. [PubMed] [Google Scholar]
- Manouchehri AV, Zaini A, Javadian E. Resistance of Anopheles culicifacies Giles to DDT in Baluchistan Province, southern Iran, 1974. Mosq News. 1975b;35:314–316. [Google Scholar]
- Manouchehri A, Ghiasseddin M, Shahgudian ER. Anopheles dthali Patton, 1905, a new secondary vector in southern Iran. Annals Trop Med Parasitol. 1972;66(4):537–538. doi: 10.1080/00034983.1972.11686857. [DOI] [PubMed] [Google Scholar]
- Mofidi Ch, Samimi B, Eshghi B, Ghiassedin M. Institute of Parasitology and Malariology, Tehran University; Tehran, Iran: 1958. Further studies of anopheline susceptibility to insecticide in Iran, result of Bosvine and Nash Method. Publ. 585/7. [Google Scholar]
- Mofidi Ch, Samimi B. Institute of Parasitology and Malariology, Tehran University; Tehran, Iran: 1960. Resistance of Anopheles stephensi to dieldrin. Publ. 650. [Google Scholar]
- Moosa-Kazemi SH, Vatandoost H, Raeisi A, Akbarzadeh K. Deltamethrin Impregnated Bed Nets in a Malaria Control Program in Chabahar, Southeast Baluchistan. I.R. Iran, Iranian J Arthropod-Borne Dis. 2007;1(1):43–51. [Google Scholar]
- Minsitry of Health and Medical Education . Annual report of malaria control department 2008. CDC; IR Iran: 2008. p. 50. [Google Scholar]
- Naddaf SR, Oshaghi MA, Vatandoost H, Asmar M. Molecular characterization of the Anopheles fluviatilis species complex in Iran. Eastern Med Health J. 2003;9(3):257–265. [PubMed] [Google Scholar]
- Raeisi A, Shahbazi A, Ranjbar M, Shoghli A, Vatandoost H, Faraji L. National strategy plan for malaria control (I. R. Iran, 2004–2008) Ministry of Health and Medical Education of Iran Publication. 2004:72. [Google Scholar]
- Saebi E, Ranjbar M, Nabavi M, Salehi M, Raeisi A, Rigwald P, Lobraz J, Keshavarz H, Nateghpour M, Shahbazi A, Jamshidi M, Faraji L. National malaria treatment guideline in I.R. Iran. 2006. p. 32. Diseases Management Center, Ministry of Health, and Medical Education. Seda Publ Center.
- Shahi M, Vatandoost H, Abaei MR, Hanafi-Bojd AA. Susceptibility of Anopheles fluviatilis James to different insecticides in Bandar Abbas township, 2003. Hormozgan Med J. 2006;10(4):321–328. [Google Scholar]
- Vatandoost H, Shahi M, Hanafi-Bojd AA, Abai MR, Oshaghi MA, Rafii F. Ecology of Anopheles dthali Patton in Bandar Abbas. Iranian J Arthropod-Borne Dis. 2007;1(1):21–27. [Google Scholar]
- Vatandoost H, Oshaghi MA, Abaie MR, Shahi M, Yaaghoobi F, Baghaii M, Hanafi-Bojd AA, Zamani G, Townson H. Bionomics of Anopheles stephensi Liston in the malarious area of Hormozgan Province, southern Iran, 2002. Acta Trop. 2006;97:196–203. doi: 10.1016/j.actatropica.2005.11.002. [DOI] [PubMed] [Google Scholar]
- Vatandoost H, Shahi M, Abai MR, Hanafi-Bojd AA, Oshaghi MA, Zamani G. Larval habitats of main malaria vectors in Hormozgan Province and their susceptibility to different larvicides. South-east Asian J Trop Med Pub Hlth. 2004;35(2):22–25. [PubMed] [Google Scholar]
- Vatandoost H, Mashayekhi M, Abaie MR, Aflatoonian MR, Hanafi-Bojd AA, Sharifi I. Monitoring of insecticides resistance in main malaria vectors in a malarious area of Kahnooj District, Kerman Province, southeastern Iran. J Vector Borne Dis. 2005;42:100–108. [PubMed] [Google Scholar]
- Vatandoost H, Hanafi-Bojd AA. Current resistant status of Anopheles stephensi Liston to different larvicides in Hormozgan Province, southeastern Iran. Pakistan J Biolog Sci. 2005;8:1568–1570. [Google Scholar]
- Vatandoost H, Vaziri VM. Larvicidal activity of neem tree extract (Neemarin) against mosquito larvae in the Islamic Republic of Iran. Eastern Med Health J. 2004;10:573–578. [PubMed] [Google Scholar]
- Vatandoost H, Borhani N. Susceptibility level and irritability of synthetic pyrethroids against main malaria vectors in the endemic areas of Iran. Acta Med Iran. 2004;42:247–255. [Google Scholar]
- WHO . World malaria report 2009. WHO Press, World Health Organization; Geneva: 2009. p. 66. [Google Scholar]
- Zahirnia AH, Taherkhani H, Vatandoost H. Observation of malaria sporozoite in Anopheles culicifacies (Diptera: Culicidae) in Ghasreghand District, Sistan and Baluchistan Province. Hakim. 2001;4:149–153. [Google Scholar]