Abstract
Background:
The aims of this study was to analysis the current situation of malaria and to find the distribution of anopheline mosquitoes, as probable vectors of the disease, in Qom Province, central Iran.
Methods:
This study was carried out in two parts. First stage was data collection about malaria cases using recorded documents of patients in the Province health center, during 2001–2008. The second stage was entomological survey conducted by mosquito larval collection method in 4 villages with different geographical positions in 2008. Data were analyzed using Excel software.
Results:
Of 4456 blood slides, 10.9% out were positive. Most of cases were imported from other countries (90.4%), mainly from Afghanistan (56.5%) and Pakistan (16.3%). Slide positive rate showed a maximum of 16.9% and a minimum of 2.9% in 2008 and 2007, respectively. Plasmodium vivax was causative agent of 93.75% of cases, followed by P. falciparum (6.25%). More than 15 years old age group contained the most malaria reported cases (66.7%). Two Anopheles species, An. superpictus and An. claviger were collected and identified. This is the first report of Anopheles claviger in Qom Province.
Conclusion:
Malaria is in the control stage in Qom Province. The rate of local transmission is very low (only 1 case), shows Anopheles superpictus, as the main malaria vector of central part of Iran, can play its role in malaria transmission in the area.
Keywords: Malaria, Iran, Epidemiology
Introduction
Malaria is one of the most important infectious diseases in tropical and subtropical regions of the world. The last data show 225 million cases of malaria resulted to about 781000 death in 2009 (WHO 2010).
Malaria eradication program that started in 1956 in Iran changed to malaria control program from 1980, restricted the local transmission of this disease, so that at present it occurs only in 3 southeastern provinces of Sistan and Baluchistan, Hormozgan and Kerman Provinces and 95% of cases in 2007 reported from these provinces (Raeisi et al. 2009). Multiplicity of malaria vectors and their various behaviors, resistance of the main vector An. stephensi Liston as well as An. culicifacies to some insecticides, absence of suitable transportation roads to some remote villages, structure of living houses, socioeconomic conditions of people, immigration from malarious neighbor countries (Afghanistan and Pakistan) and some other operational problems are the present problems for malaria control program in Iran. According to the latest checklist of Iranian mosquitoes (Azari-Hamidian 2007) there are 28 Anopheles species in Iran, 7 out of them are well known as malaria vectors in the country: An. stephensi, An. culicifacies, An. fluviatilis and An. dthali in the southern part, An. maculipennis and An. sacharovi in north and north-west, and An. superpictus in central part, although it is distributed in nearly all parts of Iran, except for coastal area of Caspian Sea (Saebi 1987, Manouchehri et al. 1992, Edrissian 2006). During the 1994–95 an outbreak of Plasmodium vivax malaria appeared in the northwest parts of the country in Parsabad, Ardebil Province (Arshi et al. 2002, Edrissian 2006). Anopheles sacharovi was is responsible for malaria maintaining in this area (Yaghoobi-Ershadi et al. 2001). At present the disease in this area is under control. Besides, the risk of re-emergence of malaria exists in other parts of the country. Iran showed evidence of a sustained decrease in the number of cases, more than 50% since 2000, associated with wide scale implementation of malaria control activities and is classified in the pre-elimination phase of malaria (WHO 2010).
Qom Province located in the central plateau region of Iran, where have lower risk of malaria infection compare to southern/southeastern parts. Situation of this province increases its risk for malaria, because many passengers/pilgrims from malarious area visit this province and stay for sometime.
The aims of this study was to analysis the current situation of malaria and to find the distribution of anopheline mosquitoes, as probable vectors of the disease, in Qom Province, central Iran.
Materials and Methods
Study area
Qom is one of the 30 provinces of Iran, between 50° 06′–51 ° 58′ E and 34 ° 09′–35 ° 11′ N with 11,237 km2, covering 0.89% of the total area in Iran. It is in the northern part of the country, and its provincial capital is the city of Qom (Fig. 1). Based on the last census in 2005, this province had a population of approximately 2,000,000 out of which 91.2% resided in urban areas and 8.8% in rural vicinities. The province contains one city, five counties, nine rural districts, and 256 villages.
Fig. 1.
Position of Qom Province in Iran (left) and its geographical situation (right)
The climate of Qom Province varies between a desert and semi-desert climate, and comprises mountainous areas, foothills and plains. Due to being located near an arid region and far inland, it experiences a dry climate, with low humidity and scanty rainfall.
The minimum and maximum temperatures in 2008 were −1.9 in January and 37.4 in June, respectively. The annual rainfall in this year was 114.9 mm. Relative humidity was ranged between 10.2 in June and 79.3 in February (Iran Meteorological Organization).
Malaria information
All data about malaria cases during 2001–2008 were obtained from disease prevention unit, Qom Province health center. A databank was created in Excel software.
Entomological survey
In order to determine the anopheline mosquito fauna of Qom Province, 4 villages with different geographical positions and weather conditions were selected: Agholak (Qahan District), Ahmadabad (Dastjerd District), Rahjerd (Qomrood District) and Emamzadeh Esmail (Kahak District). Mosquito larval collection was conducted biweekly during April to November 2008, using dipping standard method of WHO. Larvae were collected from riversides which had small vegetation, and conserved in lactophenol medium. In the laboratory, the specimens were mounted in de Faure’s medium and identified using illustrated keys for Iranian mosquitoes (Shahgudian 1960, Azari-Hamidian and Harbach 2009).
Results
During the study period, 448 malaria cases were detected and reported in Qom Province. Out of them 420 cases were infected by Plasmodium vivax, while 28 cases were due to P. falciparum (Table 1). Based on recorded data only one case was due to local transmission and others were imported. This case was an Iranian man who lived close to 15 families of foreign religious sciences students. Most of cases observed among passengers who came to Qom from other countries (90.4%) and different parts of Iran for pilgrimage and also studying the religious sciences. Afghani patients had the highest rate of infection (56.5%), followed by Pakistani peoples (16.3%) and other nationalities such as Sudanese, Yemeni and so on (17.6%).
Table 1.
Malaria information in Qom Province, 2001–2008
| Years | At risk population | Nationality | Sex | Age groups | Species | Total slides | Total cases | API | ASPR | ABER | AVI | AFI | Residence place | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||||||||||
| Iranian | Non-Iranian | Male | Female | <5 | 5–14 | 14< | P. vivax | P. falciparum | Mix | City | Village | |||||||||
| 2001 | 917080 | 15 | 136 | 83 | 68 | 29 | 43 | 79 | 149 | 2 | 0 | 972 | 151 | 0.00016 | 0.155 | 0.0010 | 0.153 | 0.002 | 105 | 46 |
| 2002 | 942045 | 9 | 105 | 59 | 55 | 15 | 36 | 63 | 97 | 17 | 0 | 815 | 114 | 0.00012 | 0.139 | 0.0008 | 0.119 | 0.020 | 56 | 58 |
| 2003 | 967193 | 4 | 47 | 36 | 15 | 4 | 5 | 42 | 45 | 6 | 0 | 741 | 51 | 0.00005 | 0.068 | 0.0007 | 0.060 | 0.008 | 43 | 8 |
| 2004 | 991993 | 3 | 54 | 47 | 10 | 0 | 3 | 54 | 57 | 0 | 0 | 661 | 57 | 0.00005 | 0.086 | 0.0006 | 0.085 | 0 | 45 | 12 |
| 2005 | 1018997 | 4 | 18 | 16 | 6 | 1 | 0 | 21 | 22 | 0 | 0 | 233 | 22 | 0.00002 | 0.094 | 0.0002 | 0.094 | 0 | 18 | 4 |
| 2006 | 1046737 | 3 | 16 | 17 | 2 | 0 | 6 | 13 | 19 | 0 | 0 | 500 | 19 | 0.00002 | 0.038 | 0.0004 | 0.038 | 0 | 4 | 15 |
| 2007 | 1074475 | 4 | 8 | 8 | 4 | 1 | 1 | 10 | 10 | 2 | 0 | 404 | 12 | 0.00001 | 0.029 | 0.0003 | 0.024 | 0.005 | 12 | 0 |
| 2008 | 1102948 | 1 | 21 | 20 | 2 | 2 | 3 | 17 | 21 | 1 | 0 | 130 | 22 | 0.00002 | 0.169 | 0.0001 | 0.161 | 0.008 | 21 | 1 |
| Total | --- | 43 | 405 | 286 | 162 | 52 | 97 | 299 | 420 | 28 | 0 | 4456 | 448 | -- | -- | -- | -- | -- | 304 | 144 |
API = Annual Parasite Incidence, ASPR = Annual Slide Positive Rate, ABER = Annual Blood Examination Rate
AVI = Annual Vivax Incidence, AFI = Annual Falciparum Incidence
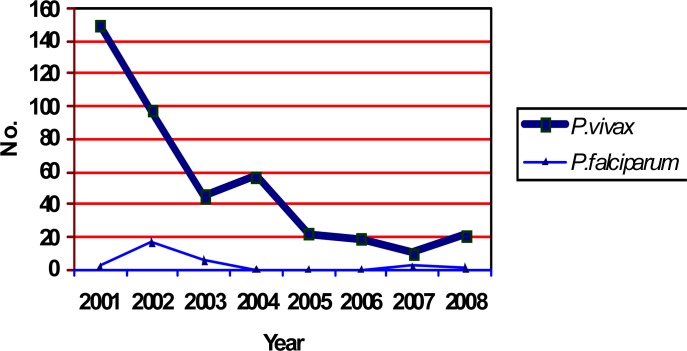
Reported cases were higher in males (63.8%) than females (36.2%). Analysis of cases based on age showed 11.6%, 21.6% and 66.8% were in 0–4, 5–15 and more than 15 yr old age groups, respectively. Most of cases were reported in August and September. Plasmodium vivax was dominant parasite species and the trend of the disease had a decreasing pattern (Fig. 2).
Fig. 2.
Malaria cases based on parasitic species, Qom province, 2001–2008
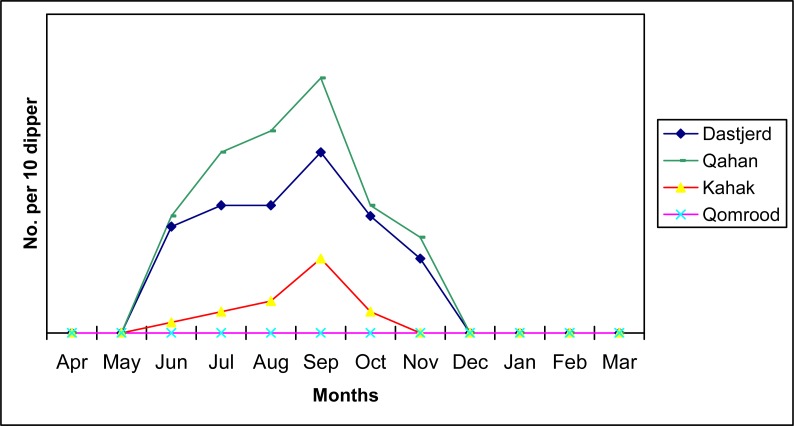
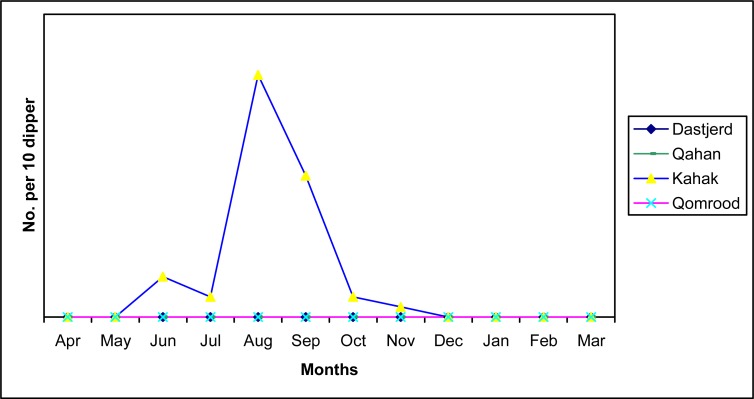
During April–November 2008, a total of 223 Anopheles larvae were collected and identified from collection stations. Anopheles claviger was dominant species (78.9%) and An. superpictus had the second frequency (21.1%). The activity of these species started from June and finished at December with a peak at September for An. claviger (Fig. 3) and August for An. superpictus (Fig. 4). Anopheles claviger is more distributed than An. superpictus in Qom Province, and found in three rural districts of Dastjerd, Qahan and Kahak, while An. superpictus was only collected from Kahak. In Qomrood District we found only Culicinae larvae.
Fig. 3.
Monthly activity of Anopheles claviger larvae in Qom province, 2008
Fig. 4.
Monthly activity of Anopheles superpictus larvae in Qom province, 2008
Discussion
In the entomological survey we found An. superpictus and An. claviger were active in the study area. Saebi (1987) reported only An. superpictus from Qom area, so this is the first report of An. claviger for Qom fauna. A study on malaria situation in Kashan City, close to Qom reported three anopheline mosquitoes, An. superpictus, An. claviger and An. molticolor in that area (Doroudgar et al. 1999). The Human Blood Indexes (HBIs) in An. superpictus in Iran was reported 4.9 (Edrissian et al. 1985). This show An. superpictus has antropophilic behavior, although it is an exophilic species. This species is introduced as malaria vector in central plateau of Iran and can play its role in local transmission of malaria in Qom Province under favorite conditions. The activity peak of this Anopheles in the area is the same with malaria disease occurrence. So it can be an alarm for malaria transmission in the area. Natural sporozoite infections of An. claviger have been recorded in Syria, Cyprus, Mesopotamia, and Taranto in Italy (Muir and Keilany 1972). More studies are recommended on this species in Iran to clear its antropophilic index and probable role in malaria transmission.
Results of this survey show malaria is at control stage in Qom Province, like many other provinces of the country. Trend of this disease was decreased up to 2007, but increased after that in 2008 (Fig. 2). Although all reported cases in this province were imported, the history of malaria in this province shows one indigenous case in 2004. Annual parasite index (API) decreased from 0.00016 in 2001 to 0.00001 in 2007, while annual blood examination rate (ABER) is also decreased from 0.0010 to 0.0003 during this period (Table 1). This show the surveillance system is not alert and only passive slides were taken. This may be due to low importance of malaria in Qom Province. Most of patients were non-Iranian, so it is recommended to take blood slide from all foreign students that mainly came from endemic countries for malaria, to improve the surveillance system of malaria detection and treatment.
Qom Province has thousands passengers from all parts of the country as well as other countries like Afghanistan, Pakistan, Yemen, Sudan, Djibouti and other malarious countries, so imported cases can play their role as malaria parasite reservoirs in the area and local transmission can occurs in suitable conditions.
Results of this study show only 0.2% of recorded cases were due to local transmission. Survey on the epidemiology of malaria in Kashan Province, bordered with Qom, showed 95% of positive cases were Afghani immigrants (Doroudgar et al. 1999). A similar study in Hamadan Province, western of Iran, shows 2.56% of reported cases during a 20 yr period were due to local transmission (Fallah et al. 2003). In addition, in Mazandaran Province, northern Iran, during 1999–2003; 13.7% of cases had no history of travel to other parts of the country (Najafi et al. 2006). Results of a demographic study on malaria in Kohgiloye and Boyer Ahmad Province, west of Iran, showed 62.7% of cases were local Iranian peoples (Moshfe et al. 2003). This shows local transmission is occurred in this province, maybe due to favorable conditions for malaria vectors in that area.
Although the probability of local transmission of malaria in Qom Province is very low, it is not impossible. So we recommend improving the surveillance system for case detection and treatment by active slide preparing among foreign students of religious sciences as well as pilgrims coming from malarious countries.
Acknowledgments
The authors would like to thank Dr A Akbari, Dr A Abbasi, Dr B Mahmoudi and Mrs F Abedi Astaneh their kind assistance and help. This study was financially supported by Deputy of Research, Qom University of Medical Sciences. The authors declare that they have no conflicts of interest.
References
- Arshi Sh, Sadeghi H, Mohebali M, Sezavar SH, Javan-Roozegar A, Emdadi D, Sepahram V, Amini-Sani N. Malaria epidemiology in Ardabil Province, 1999–2000. Ardabil University Journal. 2002;2(5):28–33. [Google Scholar]
- Azari-Hamidian S. Checklist of Iranian mosquitoes (Diptera: Culicidae) J Vec Ecol. 2007;32(2):235–242. doi: 10.3376/1081-1710(2007)32[235:coimdc]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Azari-Hamidian S, Harbach RE. Keys to the adult females and fourth-instar larvae of the mosquitoes of Iran (Diptera: Culicidae) Zootaxa. 2009;2078:1–33. [Google Scholar]
- Doroudgar A, Dehghani R, Hooshyar H, Sayyah M. Epidemiology of Malaria in Kashan. J Med Faculty Guilan Univ Med Sci. 1999;8(31–32):52–58. [Google Scholar]
- Edrissian GhH. Malaria in Iran: Past and present situation. Iranian J Parasitol. 2006;1(1):1–14. [Google Scholar]
- Edrissian GhH, Manouchehri AV, Hafizi A. Application of enzymelinked immunosorbent assay (ELISA) for determination of the human blood index in anopheline mosquitoes collected in Iran. J Am Mosq Control Assoc. 1985;1(3):349–352. [PubMed] [Google Scholar]
- Fallah M, Mirarab SA, Jamalian SF, Ghaderi A, Zolfaghari A. Epidemiology of Malaria in Hamadan Province during a 20 year period, 1980–2001. J Behbood. 2003;17(7):36–44. [Google Scholar]
- Manouchehri AV, Zaim M, Emadi AM. A review of malaria in Iran, 1957–1990. J Am Mosq Control Assoc. 1992;8:381–385. [PubMed] [Google Scholar]
- Moshfe A, Abolghasem Hosseini Sh, Karimi Z. Demographic pattern of malaria in Kohgiloyeh and Boyerahmad Province in 1996–2003. J Armaghan Danesh. 2003;8(31):27–39. [Google Scholar]
- Muir DA, Keilany M. Anopheles claviger Meigen as a malaria vector in Syria. 1972. p. 757. WHO/Mal/72.
- Najafi N, Ghasemian R, Farahmand M. Epidemiology of Malaria in Mazandaran Province during 1999–2003. J Mazandaran Univ Med Sci. 2006;50(15):125–132. [Google Scholar]
- Raeisi A, Nikpoor F, Ranjbar Kahkha M, Faraji L. The trend of malaria in I.R.Iran from 2002 to 2007. Hakim Res J. 2009;12(1):35–41. [Google Scholar]
- Saebi ME. 1987. Morphological study on anopheline larvae and their distribution in Iran [PhD dissertation]. School of Public Health, Tehran University of Medical Sciences, Iran.
- Shahgudian ER. A key to the anophelines of Iran. Acta Med Iran. 1960;3:38–48. [PubMed] [Google Scholar]
- WHO . World Malaria Report 2010. World Health Organization; Geneva: 2010. p. 203. [Google Scholar]
- Yaghoobi-Ershadi MR, Namazi J, Piazak N. Bionomics of Anopheles sacharovi in Ardebil Province, northwestern Iran during a larval control program. Acta Trop. 2001;78:207–215. doi: 10.1016/s0001-706x(01)00080-8. [DOI] [PubMed] [Google Scholar]