Abstract
Purpose
The purpose of this study was to investigate the characteristics of patients managed for spinal tuberculosis at the orthopaedics department of a teaching hospital in Chongqing, China, between 2004 and 2010.
Methods
The study used a retrospective chart review. The epidemiology, clinical features, laboratory test results, imaging study findings, and treatment methods were recorded.
Results
The annual incidence of spinal tuberculosis was stable throughout the study period. There were 284 patients, 147 women and 137 men, with a mean age of 38.2 years. The majority of the lesions involved the thoracic spine (45.3%), followed by the lumbar spine (45.0%). Multiple level skip lesions were seen in 5.6% of cases. The erythrocyte sedimentation rate was normal in 26.8% of patients. The C-reactive protein (CRP) was normal in 30.2% of patients. Type A and type O were the most common blood types. Neurological involvement was seen in 21.8% of patients. Concomitant tuberculosis of the lung was seen in 73 (25.7%). The patients with middle school education and above account for 60.4% (102/169) in rural patients and 68.7% (79/115) in urban patients. Mean time from symptom onset to diagnosis was 18.0 months (range, three days to 360 months), and there was a significant difference between the rural patients (23.0 months) and the urban patients (10.7 months) (p = 0.001, t = −3.300). Surgical treatment was performed in 233 patients (82.0%). The preferred surgical procedure was radical anterior debridement, bone grafting and internal fixation (132 patients, 46.5%). There were 13 patients (4.2%) with anti-tuberculous chemotherapy drug allergy or toxicity, streptomycin anaphylaxis and toxicity in 12, and isoniazide anaphylaxis and toxicity in one. No mortality was related to spinal TB.
Conclusion
The annual incidence of spinal tuberculosis remained unchanged throughout the study period and most of the patients did not pay much attention to the disease and received timely treatment. Thus, we should strengthen the census and treatment of spinal tuberculosis in Southwest China.
Introduction
Tuberculosis (TB), more prevalent in immunocompromised persons, is an emerging international problem despite advances in the methods of diagnosis and treatment; it is still prevalent in developing countries and on the increase in developed ones [1, 2]. Skeletal involvement occurs in approximately 10% of all patients with extra-pulmonary TB [3]. There are a number of publications regarding spinal TB in other countries [4–6], but in China few studies on spinal TB have been conducted, and most of them focussed on diagnostic features [7, 8]. China has the second highest burden of tuberculosis (TB) in the world, registering 17% of global cases [19]. Hence, the purpose of this seven-year retrospective study was to characterise the clinical presentation, laboratory test results, imaging study findings and the treatment of patients with spinal TB in the teaching hospital between January 2004 and December 2010.
Materials and methods
Study site
Chongqing Municipality is a city of 31,442,300 located in southwest China, and the rural population accounted for 61.7% in 2009. According to the Fourth National TB Survey in 2000, the TB prevalence rate for Chongqing Municipality (including urban and rural areas) was 112.5 per 100,000. The smear positive TB prevalence rate was much higher in rural counties of Chongqing (173.0/ 100,000) than in the urban areas (81.1/100,000). The teaching hospital was located in Shapingba district (SPB), which is a core district located in the northwest of Chongqing city. In 2010, SPB had per capita average income of 19,288CNY and the per capita average income of Chongqing was 18,991CNY.
Patient survey
We retrospectively reviewed the medical records of patients admitted for spinal tuberculosis to the Orthopaedic Department of the Xin Qiao Hospital, Chongqing, China between January 2004 and December 2010. Diagnosis was established following full clinical, haematological and radiological examination supplemented by pathological examination of biopsy specimens. The following is routinely done for suspected tuberculosis of the spine: a full clinical history detailing any backache, neurological deficit, spinal deformity, loss of weight, general malaise, and present or previous history of pulmonary tuberculosis; physical examination of lungs, spine, abdomen, groin, flanks, and peripheral nervous system; erythrocyte sedimentation rate; tuberculin test; chest radiograph; plain spinal radiograph; CT scan of the affected and adjacent vertebrae if surgery is contemplated or a tumour is suspected; multiplanar MRI of the spine for detection and characterisation of cord compression. In cases of suspected tuberculosis of the spine when plain radiographs were normal, the following was also performed: ultrasound of paraspinal and psoas muscles for detection of abscesses; biopsy when indicated and during surgical decompression. Clinical and radiological response to empirical anti-tuberculosis treatment is considered a diagnostic clue. We abstracted the following information from each record: demographic characteristics including clinical manifestations, laboratory test results, findings from imaging studies, and treatment methods of the patients.
Results
Demographics and epidemiology
During this seven-year period, 284 patients with spinal TB were identified, the annual incidence of spinal tuberculosis was stable throughout the study period (31–49 cases per year). Mean age was 38.2 years overall, 39.4 years in the 137 males and 37.0 years in the 147 females. Male to female ratio was 1.07 (Table 1). The largest number of patients fell in the 31–40 age group (30.6%). Mean time from symptom onset to diagnosis in the hospital was 18.0 months (range, three days–360 months), and 122 patients (43.0%) with mean time from symptom onset to diagnosis was more than 12 months. Rural patients accounted for 59.5% (169/284) and urban patients accounted for 40.5% (115/284). The patients with middle school education and above accounted for 60.4% (102/169) in rural patients and 68.7% (79/115) in urban patients. Mean time from symptom onset to diagnosis in the hospital was 23.0 months in rural patients and 10.7 months in urban patients; there was significant difference between the two groups (P = 0.001,t = −3.300). The average income of the patients in the study was 12,653 CNY over the seven years. There were 177 patients (62.3%) with worsening of their sickness during the course of disease. Risk factors consisted of alcohol abuse and/or smokers in 14 patients, diabetes in two patients, close contact with a person with tuberculosis in seven patients, and a history of tuberculosis in 36 (12.7%) patients. None of the patients were HIV-positive and none had a history of TNF-α antagonist therapy.
Table 1.
Demographic characteristics of 284 spinal tuberculosis patients
| Characteristics | Value |
|---|---|
| Age (years) | 38 (2–82) |
| Age distribution (years) | |
| <11 | 6 |
| 11–20 | 30 |
| 21–30 | 46 |
| 31–40 | 87 |
| 41–50 | 54 |
| 51–60 | 39 |
| >60 | 22 |
| Sex, M/F | 147/137 |
| Comorbidities, n | |
| Respiratory disease | 4 |
| Diabetes mellitus | 2 |
| Chronic kidney disease | 4 |
| Cardiovascular disease | 2 |
| Hepatitis B | 1 |
| Others | 2 |
| Duration of symptoms | 18.0 months (3 days – 360 months) |
| Rural patients | 23.0 months (20 days – 360 months) |
| Urban patients | 10.7 months (3 days – 120 months) |
| Worsening of sickness, % | 177, 62.3% |
Thirty-six patients had a previous history of TB, including spinal tuberculosis (17cases), pulmonary tuberculosis (11 cases), cervical lymph node tuberculosis (three cases), pleural tuberculosis (two cases), testicular tuberculosis (one case), epididymal tuberculosis (one case) and intestinal tuberculosis (one case). At the time of diagnosis, 95 patients (33.5%) had constitutional symptoms. Seventy-three patients (25.7%) had concomitant pulmonary TB. Ten cases had other extra-pulmonary site involvement, including tuberculosis of rib (three cases), tuberculosis of joint (three cases), renal tuberculosis (one case), epididymal tuberculosis (one case), pleural tuberculosis (one case) and cervical lymph node tuberculosis (one case).
Clinical presentation
Back pain was the most common clinical complaint (263 patients, 92.6%), followed by radicular pain (43 patients, 15.1%), numbness (39 patients, 13.7%), weakness (28 patients, 9.9%) and trouble walking (35 patients, 12.3%). In addition, presenting symptoms included nocturnal pain in 11 patients. A fever was present in 75 patients and weight loss (2–20 kg) in 46 patients (16.2%). At physical examination of the patients, tenderness was found in 214, percussion pain in 159, kyphosis in 81, mass in 23 and sinus in 15 (Table 2). Neurological deficit was classified according to the Frankel classification. The number of the patients with neurological deficit was 62 (21.8%): Frankel A in three patients, Frankel B in one patient, Frankel C in seven patients and Frankel D in 51 patients.
Table 2.
Clinical symptoms/signs and initial laboratory findings of 284 spinal tuberculosis patients
| Characteristics | Value |
|---|---|
| Clinical symptoms | |
| Back pain | 263 (92.6%) |
| Radicular pain | 43 (15.1%) |
| Numbness | 39 (13.7%) |
| Weakness | 28 (9.9%) |
| Trouble walking | 35 (12.3%) |
| Fever | 75 (26.4%) |
| Clinical signs | |
| Tenderness | 214 (75.4%) |
| Percussion pain | 159 (56.0%) |
| Kyphosis | 81 (28.5%) |
| Mass | 23 (8.1%) |
| Sinus | 15 (5.3%) |
| Hematological and biochemical data | |
| ESR (mm/hr) | 41.2 ± 30.0 |
| C-reactive protein (mg/L) | 26.4 ± 41.0 |
| Positive rate of TB-Ab | 21.2% |
Laboratory test results
Erythrocyte sedimentation rate is a routine investigation and in our study ranged from 1–145 mm/h. The mean ESR was 41.2 mm/h. The percentage of patients with ESR less than 20 mm/h was 26.8%. The percentage of patients with ESR more than 100 mm/h was 4.9%. The mean value of C-reactive protein (CRP) level at presentation was 26.4 mg/L. The C-reactive protein (CRP) was normal in 30.2% of patients. TB-Ab test in the blood found a positive rate of 21.2%, a weak positive rate of 36.5% and a negative rate of 42.3%. In blood type testing of 201 patients, type A was found in 69 patients, type O in 66 patients, type B in 43 patients, and type AB in 23 patients.
Imaging study findings
Image findings are summarised in Table 2. All patients received an X-ray examination. Computed tomography (CT) was the most frequently used imaging modality in evaluating spinal lesions (240 patients, 84.5%); 199 (70.1%) of these patients received magnetic resonance imaging (MRI). Radionuclide bone scanning was performed in 32 patients (11.3%), all of whom had foci of increased uptake.
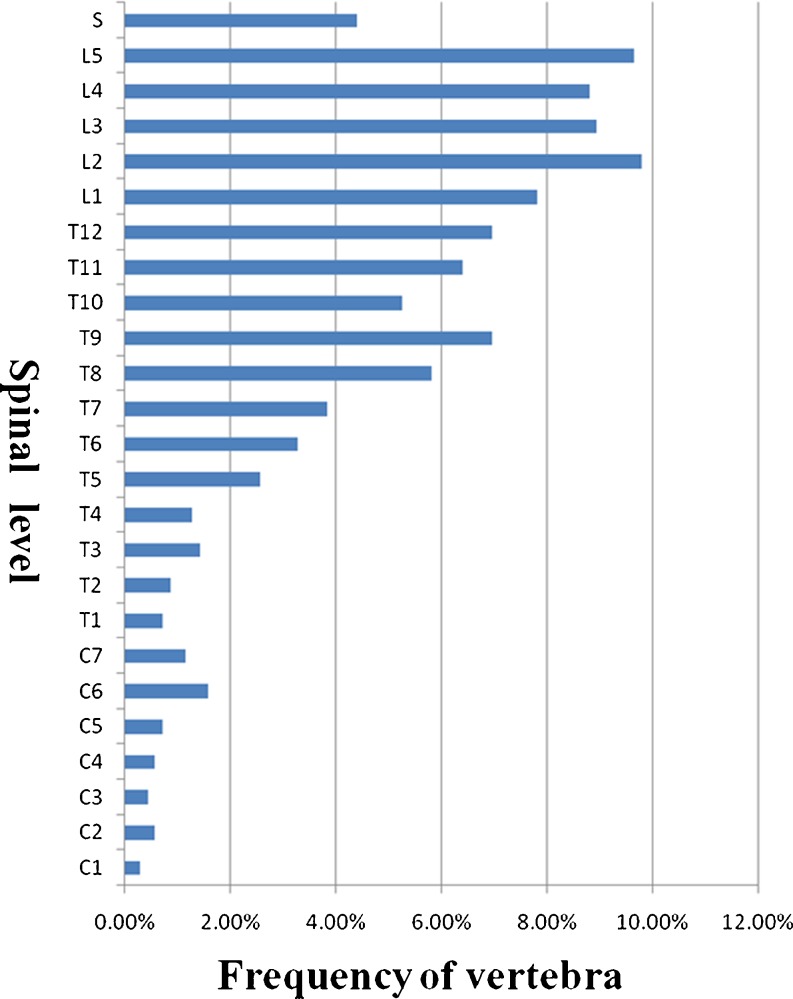
Through the imaging study, the 284 patients had 704 lesions, whereby the thoracic spine was the most commonly involved site (319, 45.3%), followed by the lumbar spine (317, 45.0%), while the cervical spine (37, 5.3%) and sacral spine (31, 4.4%) were less commonly involved (Fig. 1). The numbers of vertebral bodies involved per patient ranged between one and 14 (mean 2.5). A total of 26.8% of patients had three or more vertebral bodies involved. Multiple level skip lesions were seen in 5.6% of cases. The most common findings were disk space narrowing (visible on plain radiographs in 229 of the 284 patients), and there were 27 patients with disk space fusion. Abscesses were visible by CT and MRI in 112 of 284 patients (39.4%), including paraspinal abscess in 99, prevertebral abscess in ten and spinal abscess in six. Epidural compression was visible in 66 patients (23.2%). There were eight patients with pathological fracture caused by spinal tuberculosis (Table 3).
Fig. 1.
Distribution of spine tuberculosis for each vertebra
Table 3.
Imaging characteristics of 284 spinal tuberculosis patients
| Characteristics | Patients, n (%) |
|---|---|
| Location | |
| Cervical | 37 (5.3) |
| Thoracic | 319 (45.3) |
| Lumbar | 317 (45.0) |
| Sacral | 31 (4.4) |
| Skipped lesion | 16 (5.6) |
| Vertebra involved | |
| 1 | 39 (13.7) |
| 2 | 169 (59.5) |
| ≧3 | 76 (26.8) |
| Imaging findings | |
| Disc space involvement | 229 (80.6) |
| Paraspinal abscess | 99 (34.9) |
| Prevertebral abscess | 10 (3.5) |
| Spinal abscess | 6 (2.1) |
| Epidural compression | 66 (23.2) |
| Pathological fracture | 8 (2.8) |
Treatments
Of the 284 patients, 143 (50.4%) underwent some form of extramural hospital anti-tuberculosis treatment, including anti-tuberculous chemotherapy in 126 (which got worse in 11, slight improvement in 39, and got better in 76), surgical treatment and postoperative recurrence in 17.
After admission into the hospital, surgical treatment was performed in 233 patients (82.0%). Anterior debridement was performed in 15 patients (5.3%) with an average length of hospital stay for 40.6 days. Anterior debridement and bone grafting was performed in 45 patients (15.8%) with an average length of hospital stay for 34.6 days. Anterior debridement, bone grafting and internal fixation was performed in 132 patients (46.5%) with an average length of hospital stay for 27.4 days. Anterior debridement, bone grafting and posterior internal fixation was performed in 30 patients (10.6%) with an average length of hospital stay for 29.4 days. Posterior debridement, bone grafting and internal fixation was performed in 11 patients (3.9%) with an average length of hospital stay for 27.4 days. Among all the patients, there were six who underwent minimally invasive surgery, anterior decompression, bone grafting and posterior internal fixation using the Sextant system, while two patients underwent debridement with an endoscopic system. Fifty-one patients (18.0%) were treated nonsurgically.
There were 26 patients (9.2%) with drug allergy or toxicity, penicillin anaphylaxis in 13 patients, streptomycin anaphylaxis and toxicity in 11 patients, procaine anaphylaxis in three patients, novocaine anaphylaxis in three patients, lincomycin anaphylaxis in one patient, and isoniazide anaphylaxis and toxicity in one patient. The rate of anti-tuberculous chemotherapy anaphylaxis and toxicity was 4.2% (12/284).
Discussion
This retrospective review of patients with spinal tuberculosis demonstrated that tuberculosis of the spine affects all age groups. The youngest patient was two years old and the oldest was 82. The mean age was 38.2. As in other reports [1, 2], our subjects were young people, with 65.8% of patients between 21 and 50 years of age. The largest number of patients was in the 31–40-year-old age group (30.6%). But Weng et al. [3] pointed out that their subjects in Taiwan were elderly, with 55% of patients over the age of 70 years.
Spinal tuberculosis is characteristically chronic and slowly progressive. Similar to other studies, back pain was the most common presenting symptom [1, 4]. Unlike pulmonary TB, spinal TB is seldom accompanied with symptoms such as fever, body weight loss or night sweating, and this was clearly demonstrated in our study. At the time of diagnosis, 95 patients (33.5%) had constitutional symptoms. Neurological deficits such as weakness, numbness, gait difficulties, and incontinence occurred less frequently [4]. Godlwana et al. [5] reported that 56% of their subjects presented with neurological deficits, in which 24% had complete paraplegia and 32% incomplete paraplegia. McLain et al. [6] reported that neurological deficits are common with long-standing thoracic and cervical involvement, and if untreated, neurological involvement may progress to complete and incomplete paraplegia. In our study, 21.8% of our subjects presented with neurological deficits, 1.1% had complete paraplegia and 20.8% incomplete paraplegia. The neurological deficits are common with thoracic (12.3%) and lumbar (7.4%) involvement.
Considerable variation in the duration of symptoms was also observed in the study, and this may be due to the insidious clinical course and nonspecific manifestations of spinal TB [4, 7]. The time from symptom onset to the diagnosis of spinal tuberculosis ranged from three days to four years in earlier studies [3, 8, 9] and varied from three days to 30 years in our population. Rural patients accounted for 59.5% and urban patients accounted for 40.5%. Patients with middle school education and above accounted for 60.4% in rural patients and 68.7% in urban patients in our study. Wang et al. [10] pointed out that middle school education and above accounted for 55.7% in the migrant patients and 62.9% in the resident patients in 2008. Mean time from symptom onset to diagnosis in the hospital was 23.0 months in rural patients and 10.7 months in urban patients; there was significant difference between the two groups. Long et al. pointed out that the knowledge and awareness of TB among the general public and in TB suspects was relatively poor. Migrants had significantly less knowledge about TB, possibly due to their lower education level and lower access to health education due to their marginal status in urban areas. Lack of TB knowledge was significantly associated with diagnostic delay in a regression analysis [10, 11]. Rural-to-urban migrants, who delay seeking care for symptoms suggestive of TB, are rendered particularly vulnerable to the limitations of the TB control system due to their low incomes, lack of health insurance and low awareness of TB and the free treatment policy [11].
Previous reports [5, 12] have indicated the thoracic region to be the most affected area in the vertebral column, followed by the lumbar region. These findings are similar to those found in our study. The sacral area is the least affected in the vertebral column with only 4.4% of cases. In contrast to the report by Schlesinger et al. [4], our patients had a more extensive disease state with tuberculosis abscess and epidural compression, whereby the tuberculosis abscesses were visible in 39.4% of the patients and the epidural compression in 23.2% of the patients. There were eight patients with pathological fracture caused by spinal tuberculosis. The different severity levels between this and previous studies may be due to the presence of nonspecific symptoms of spinal TB in the elderly and a delay in diagnosis. Analogous to other reports [3, 13], the percentage of combined spinal and pulmonary TB was 25.7% in this study. Similar to other results [2, 3], the thoracic and lumbar spines were nearly equally affected and contributed 90.3% of the spinal regions.
Erythrocyte sedimentation rate (ESR) elevation in patients with spinal tuberculosis is common [14–16], with mean reported values of 49 mm (range, 22–68 mm) [8] and 84.5 mm (range, 1–143 mm) [15]. In our study, erythrocyte sedimentation rate ranged from 1 to 145 mm/h, with a mean being 41.2 mm/h. A total of 26.8% of patients had a normal ESR of less than 20 mm/h and 4.9% had and ESR of more than 100 mm/h. ESR is a very sensitive but a highly non-specific test. We use it mostly to evaluate the disease activity during follow-up. Similarly, the mean value of C-reactive protein (CRP) level at presentation was 26.4 mg/l (range, 0.7–303 mg/l); 15.8% of patients had a normal CRP level of less than 8 mg/L. Mulleman et al. [16] pointed out that the CRP level of 23 patients with spinal tuberculosis ranged from 6 to 197 mg/l. The positive rate of TB-Ab test in the blood was 21.2%, thus the sensitivity for the diagnosis of spinal tuberculosis is low. There were no reports about the relationship between the ABO blood groups and spinal tuberculosis. In our study, type A comprises 34.3%, type O 32.8%, type B 21.4% and type AB 11.4%.
Anti-tuberculous chemotherapy remains the mainstay of therapy: 143 patients underwent some form of extramural hospital anti-tuberculosis treatment and 88.1% of them were treated through anti-tuberculous chemotherapy. In our study, the rate of anti-tuberculous chemotherapy drug anaphylaxis and toxicity was 4.2%, with streptomycin anaphylaxis and toxicity in 11, and isoniazide anaphylaxis and toxicity in one. So when patients are treated with anti-tuberculous chemotherapy, we should strengthen the monitoring to avoid serious adverse reaction. Surgery is reserved for patients with severe neurological deficit, severe kyphotic deformity, cervical spine tuberculous and severe pain (Table 4). Anterior, posterior and combined techniques as well as osteotomies and vertebral column resection have been described to correct spinal alignment and restore sagittal balance [17, 18]. Surgical treatment was performed in 233 patients (82.0%) of our population. Our choice of procedure depends on the site and level of vertebral involvement but generally it is radical anterior debridement, bone grafting and internal fixation.
Table 4.
Operation criteria of 233 patients with spinal tuberculosis in our population
| Operation criteria | Patients, n (%) |
|---|---|
| Compression and /or injury of the spinal cord, cauda or the nerve root | 81 (34.8%) |
| Severe spinal kyphosis and progressive spinal kyphosis | 67 (28.8%) |
| Regular anti-tuberculous chemotherapy with slight improvement or worsening | 30 (12.9%) |
| Large abscess; long-term non healing sinus; large sequestrum | 20 (8.6%) |
| Postoperative recurrence with sinus or spinal kyphosis | 15 (6.4%) |
| Cervical spinal tuberculosis and instability | 12 (5.2%) |
| Pathological fracture and instability | 8 (3.4%) |
Conclusions
The annual incidence of spinal tuberculosis remained unchanged throughout the study period. Tuberculosis remains a major public health problem. Before the disease can be treated, it must be recognised. Most of the patients did not pay much attention to the disease and receive timely treatment; thus, we should strengthen the census and treatment of spinal tuberculosis in Southwest China. Early initiation of an appropriate treatment regimen may reduce the need for surgical intervention.
Acknowledgments
We thank Dr. Xuke Wang for his help with the clinical data collection and statistical analyses carried out for this paper.
Contributor Information
Changqing Li, Phone: +86-236-8755608, FAX: +86-236-8755608, Email: younglee881@163.com.
Yue Zhou, Email: zhouyue_xinqiao@163.com.
References
- 1.Turgut M. Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev. 2001;24(1):8–13. doi: 10.1007/PL00011973. [DOI] [PubMed] [Google Scholar]
- 2.Pertuiset E, Beaudreuil J, Liote F, et al. Spinal tuberculosis in adults. A study of 103 cases in a developed country, 1980–1994. Med (Baltimore) 1999;78(5):309–320. doi: 10.1097/00005792-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Weng CY, Chi CY, Shih PJ, et al. Spinal tuberculosis in non-HIV-infected patients: 10 year experience of a medical center in central Taiwan. J Microbiol Immunol Infect. 2010;43(6):464–469. doi: 10.1016/S1684-1182(10)60072-2. [DOI] [PubMed] [Google Scholar]
- 4.Schlesinger N, Lardizabal A, Rao J. Tuberculosis of the spine: experience in an inner city hospital. J Clin Rheumatol. 2005;11(1):17–20. doi: 10.1097/01.rhu.0000152144.91206.0c. [DOI] [PubMed] [Google Scholar]
- 5.Godlwana L, Gounden P, Ngubo P, et al. Incidence and profile of spinal tuberculosis in patients at the only public hospital admitting such patients in KwaZulu-Natal. Spinal Cord. 2008;46(5):372–374. doi: 10.1038/sj.sc.3102150. [DOI] [PubMed] [Google Scholar]
- 6.McLain RF, Isada C. Spinal tuberculosis deserves a place on the radar screen. Cleve Clin J Med. 2004;71(7):534–549. doi: 10.3949/ccjm.71.7.537. [DOI] [PubMed] [Google Scholar]
- 7.Cormican L, Hammal R, Messenger J, et al. Current difficulties in the diagnosis and management of spinal tuberculosis. Postgrad Med J. 2006;82(963):46–51. doi: 10.1136/pgmj.2005.032862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fam AG, Rubenstein J. Another look at spinal tuberculosis. J Rheumatol. 1993;20(10):1731–1740. [PubMed] [Google Scholar]
- 9.Kim NH, Lee HM, Suh JS. Magnetic resonance imaging for the diagnosis of tuberculous spondylitis. Spine (Phila Pa 1976) 1994;19(21):2451–2455. doi: 10.1097/00007632-199411000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Wang Y, Long Q, Liu Q, et al. Treatment seeking for symptoms suggestive of TB: comparison between migrants and permanent urban residents in Chongqing, China. Trop Med Int Health. 2008;13(7):927–933. doi: 10.1111/j.1365-3156.2008.02093.x. [DOI] [PubMed] [Google Scholar]
- 11.Long Q, Li Y, Wang Y, et al. Barriers to accessing TB diagnosis for rural-to-urban migrants with chronic cough in Chongqing, China: a mixed methods study. BMC Health Serv Res. 2008;8:202. doi: 10.1186/1472-6963-8-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar R, Chandra A. Gluteal abscess: a manifestation of Pott’s disease. Neurol India. 2003;51(1):87–88. [PubMed] [Google Scholar]
- 13.Al-Saleh S, Al-Arfaj A, Naddaf H, et al. Tuberculosis arthritis: a review of 27 cases. Ann Saudi Med. 1998;18(4):368–369. doi: 10.5144/0256-4947.1998.368. [DOI] [PubMed] [Google Scholar]
- 14.Alothman A, Memish ZA, Awada A, et al. Tuberculous spondylitis: analysis of 69 cases from Saudi Arabia. Spine (Phila Pa 1976) 2001;26:E565–E570. doi: 10.1097/00007632-200112150-00020. [DOI] [PubMed] [Google Scholar]
- 15.Dharmalingam M. Tuberculosis of the spine-the Sabah experience. Epidemiology, treatment and results. Tuberculosis (Edinb) 2004;84(1–2):24–28. doi: 10.1016/j.tube.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 16.Mulleman D, Mammou S, Griffoul I, et al. Characteristics of patients with spinal tuberculosis in a French teaching hospital. Joint Bone Spine. 2006;73(4):424–427. doi: 10.1016/j.jbspin.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 17.Issack PS, Boachie-Adjei O (2011) Surgical correction of kyphotic deformity in spinal tuberculosis. Int Orthop. doi:10.1007/s00264-011-1292-9 [DOI] [PMC free article] [PubMed]
- 18.Ma YZ, Cui X, Li HW et al (2011) Outcomes of anterior and posterior instrumentation under different surgical procedures for treating thoracic and lumbar spinal tuberculosis in adults. Int Orthop. doi:10.1007/s00264-011-1390-8 [DOI] [PMC free article] [PubMed]
- 19.World Health Organization (2004) Global tuberculosis control. WHO Report, Geneva, Switzerland, p 22