Abstract
Purpose
The object of this study was to investigate the in vivo function of the posterior cruciate ligament (PCL) in patients before and after a PCL-retaining total knee arthroplasty (TKA).
Methods
Eleven patients with advanced osteoarthritis (OA) of the knee were recruited. Magnetic resonance scans of each OA knee were obtained, and 3D computer models, including the femoral and tibial insertion areas of the anterolateral and posteromedial bundles of the PCL, were created. Before and after PCL-retaining TKA, dual fluoroscopic images of each knee were acquired during weight-bearing knee flexion. The images and computer models were used to reproduce the in vivo motion of the knee. The function of the PCL bundles was described in terms of elongation, elevation and deviation. Twenty-two healthy controls were also included as normal references.
Results
PCL bundles of the OA knees were overstretched during late knee flexion and orientated more medially throughout flexion compared with normal knees. After PCL-retaining TKA, PCL bundles were further overstretched during late flexion and changed from medially directed in normal and OA knees to almost sagittally directed, which may compromise function in controlling knee rotation.
Conclusions
The current PCL-retaining TKA systems and surgical techniques may not adequately re-establish normal biomechanics of PCL bundles after PCL-retaining TKA.
Introduction
Posterior cruciate ligament (PCL)-retaining total knee arthroplasty (TKA) has been widely used by many surgeons [20, 21, 24]. PCL retention is mainly based on the assumption that the retained PCL facilitates the femoral rollback and therefore increases range of motion (ROM) of the knee and moment arm of the quadriceps [6, 14]. However, various studies have found that knee kinematics and ROM after PCL-retaining TKA are significantly different from the native knee [4, 22, 23]. Many clinical studies show that postoperative outcomes, including ROM, stability, loosening rate, gait and patient satisfaction level are similar between patients receiving PCL-retaining TKA with or without the PCL [6, 13, 17]. The role of the PCL in the PCL-retaining TKA knees remains an important topic in TKA research [6, 13, 15]. Several in vitro studies show that PCL force cannot be restored to normal after PCL-retaining TKA [11, 13, 16]. For instance, Mahoney et al. found that the PCL was generally overtight in PCL-retaining TKA knees [13]. Incavo et al. found that in most cases, the PCL was either too tight or too loose after PCL-retaining TKA [7]. In vitro robotic studies revealed that the PCL forces in PCL-retaining TKA knees were significantly lower than those in the native knees [11, 16]. Several studies have investigated the in vivo biomechanics of the PCL in normal knees and found that the PCL undergoes not only changes in length, but also in orientation [3, 8, 18]. The function of the PCL in osteoarthritic (OA) knees and PCL-retaining TKA knees may be fundamentally different from that in healthy knees due to joint degeneration caused by the disease, change in articular surface geometry, and concomitant resection of the anterior cruciate ligament (ACL) in PCL-retaining TKA knees [15]. Therefore, quantifying the in vivo PCL function in OA knees before and after PCL-retaining TKA under physiological loading conditions is important to improve the TKA that retains the PCL. The object of this study was to investigate the in vivo function of the PCL in patients before and after a PCL-retaining TKA.
Patients and methods
Study design and patient demographics
Eleven patients with advanced medial-compartment knee OA were recruited in this study (average age 64 ± 7 years, range 51–73; average height 68.3 ± 3.9 in., range 61–73; average weight 208.2 ± 31.9 lb, range 155–265; six left and five right knees; Kellgren-Lawrence (KL) grade IV in seven knees and grade III in four knees). All patients had evidence of patellofemoral disease, and five had ACL deficiency at surgery. The preoperative average Knee Society Score (KSS) was 55.3 ± 12.9 (range,39–70), and the average functional KSS was 50.0 ± 19.6 (range,25–75). The preoperative average weight-bearing ROM of the OA knees was 102.8° ± 22.3° (extension/flexion,1.8° ± 5.2°/104.6° ± 20.4°), and the average varus deformity was 1.9° ± 2.8° (range 1.0°–7.8°). Further, 22 healthy controls studied in our previous investigation were included in this study as normal references (average age 31.4 ± 9.3 years, range 19–51; average height 67.9 ± 4.1 in., range 61–75; average weight 166.9 ± 31 lb, range 110–215). Prior to the study, Institutional Review Board approval was obtained, as was informed consent from each patient.
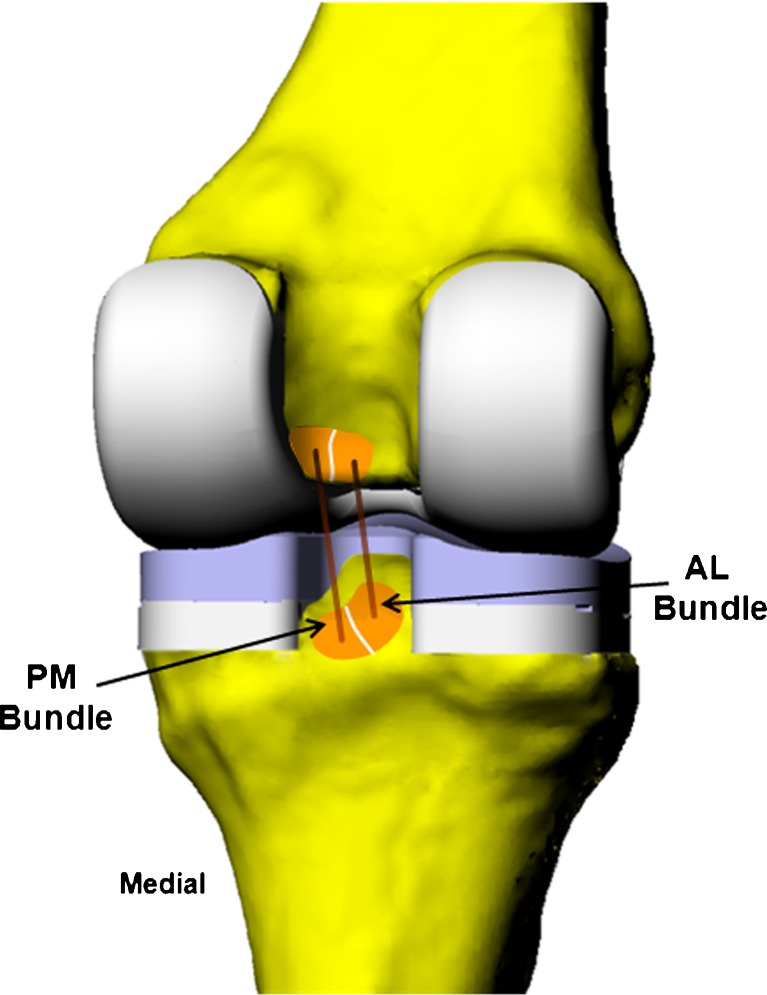
Before the scheduled operation, magnetic resonance (MR) scans of each OA knee were obtained using a 3.0-Tesla magnet (Siemens, Malvern, PA, USA) and fat-suppressed 3D spoiled gradient-recalled-echo sequence. Sagittal-plane image slices (1-mm spacing, resolution 512 × 512 pixels, field of view 180 × 180 mm) were then segmented using a 3D modelling software (Rhinoceros®, Robert McNeel and Associates, Seattle, WA, USA) to construct 3D models of the knee, including the tibia and femur. The attachment sites of the PCL on the femur and tibia were divided into the anterolateral (AL) and posteromedial (PM) bundle attachment sites by an experienced orthopaedic surgeon, and the area centroids of the bundle attachment sites were calculated (Fig. 1). Lines connecting the centroids of the corresponding bundle attachment sites on the femur and tibia represent the AL and PM bundles of the PCL. This technique has been used in previous studies in our laboratory to measure ligament kinematics [3, 8, 18].
Fig. 1.
A typical 3D model after posterior cruciate ligament (PCL)-retaining total knee arthroplasty (TKA). Insertion areas of the PCL on the femur and tibia are determined based on magnetic resonance imaging slices and divided into two functional bundles: anterolateral (AL) and posteromedial (PM)
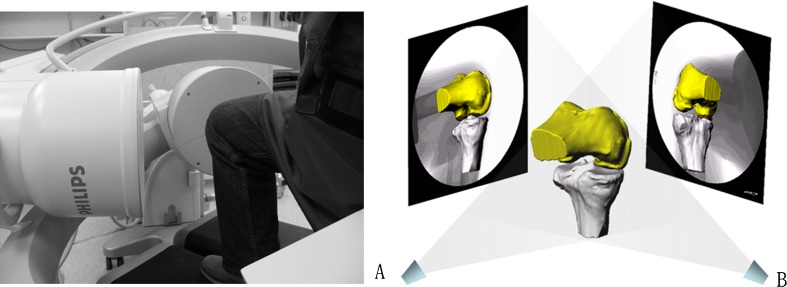
Then, the OA patients performed a weight-bearing single leg lunge from full extension to maximal flexion within the field of view of a dual fluoroscopic imaging system (Fig. 2). Patients slowly bent their knees and the two fluoroscopes captured the knee positions at 15° increments (monitored using a goniometer) from full extension to maximal flexion without altering the orientation of feet and torso. Afterwards, all patients received a high-flexion PCL-retaining TKA (NexGen CR-Flex, Zimmer, Warsaw, IN, USA). The TKA operations were performed by the same surgeon following standard procedures. In all instances, the extension–flexion gaps were well balanced without PCL recession.
Fig. 2.
a A patient performing the single leg lunge inside the dual fluoroscopic imaging system. b The virtual environment used to reproduce knee joint kinematics of each patient
After surgery (average 8 ± 2.5 months; range 7–15 months), all patients were recalled for postoperative tests and evaluated as clinically successful with no ligamentous laxity, pain or clinical complications. After PCL-retaining TKA, the average KSS was 90.6 ± 11.0 (range 60–100); average functional KSS was 85.9 ± 14.1 (range 70–100). Average weight-bearing ROM was 101.7° ± 15.1° (extension/flexion, −1.5° ± 6.2°/100.2° ± 15.5°). In vivo kinematics during weight-bearing knee flexion were obtained again using the same dual fluoroscopic imaging technique. The fluoroscopic images were imported into Rhino software to establish a virtual fluoroscopic setup (Fig. 2b). The 3D MR image-based models were then individually manipulated in six degrees of freedom (DOF) until they matched their projections on the dual fluoroscopic images captured during the actual weight-bearing activity (Fig. 2b). Thus, in vivo knee motion was represented by a series of 3D knee models at different flexion angles. The relative positions of the PCL attachment areas on the tibia and femur were also determined at each flexion angle. To measure PCL kinematics after TKA, the same preoperative knee models were used in to determine PCL kinematics [25].
Data analysis
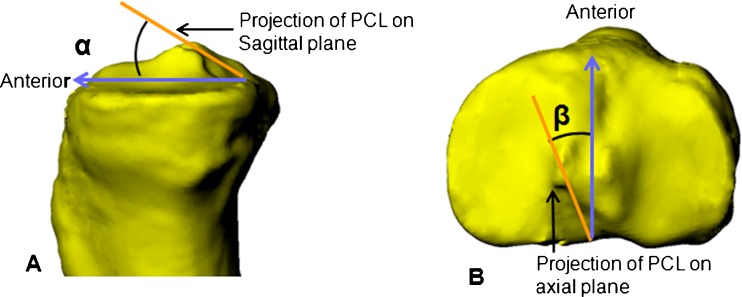
The length of each PCL bundle was defined as the length of the straight line connecting the centroids of the bundle attachment sites (Fig. 1) [18]. In the normal group, the length of each PCL bundle was measured at each flexion angle. Elongation of the bundle at different flexion angles was calculated as a percentage of its length at full extension. In the OA and PCL-retaining TKA knees, elongation of the bundles was calculated as a percentage of the length of the bundle of the preoperative OA knees at full extension [3, 18]. A coordinate system was created on the tibia to measure PCL bundle orientation [3, 18]. An orthogonal coordinate system was placed on the tibia, with the mediolateral axis obtained by projecting a line passing through the centre of the medial and lateral tibial plateaus onto a plane perpendicular to the tibial long axis. The centre of the medial/lateral tibial plateau was defined as the centroid of the closed curve formed by tracing the edges of the plateau. The midpoint of the tibial mediolateral axis was defined as the origin of the tibial coordinate system. The proximal–distal axis of the tibia was parallel to the tibial long axis. The tibial anteroposterior (AP) axis was defined to be perpendicular to the tibial mediolateral (ML) and proximal-distal (PD) axes. Knee flexion was defined as the angle between the femoral and tibial long axes projected onto the tibial sagittal plane. PCL bundle orientation was defined using elevation and deviation [3, 18], as shown in Fig. 3. Elevation was defined as the angle between the projection of the bundle on the sagittal plane and the AP axis of the tibia (Fig. 3a). Deviation was defined as the angle between the projection of the bundle on the transverse plane and the AP axis of the tibia (Fig. 3b). A medial deviation of the bundle was considered positive.
Fig. 3.
Angles used to describe the orientation of the posterior cruciate ligament (PCL). a Elevation (α) is measured by projecting the long axis of the PCL onto the sagittal plane and measuring the angle relative to the anterior direction. b Deviation (β) is measured by the projection of the long axis of the PCL on the tibial plateau and measuring the angle relative to the anterior direction
Statistical analysis
A two-way analysis of variance (ANOVA) followed by Newman–Keuls post hoc test was used to analyse the differences of elongation, elevation and deviation of the PCL bundles between groups. A p value <0.05 was considered to be significant.
Results
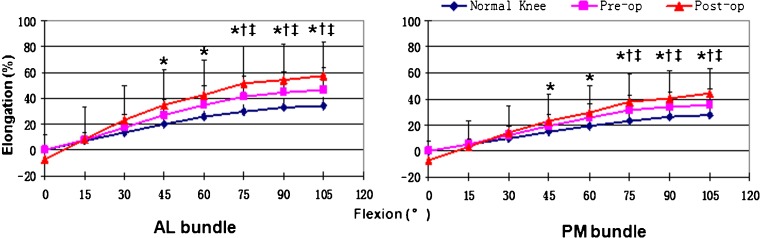
Elongation of the PCL bundles
The length of the AL bundle increased with increasing knee flexion in all three groups. Before 75° of knee flexion, elongation of the AL bundles was similar among groups. However, beyond 75° of flexion, elongation of the AL bundle in the PCL-retaining TKA knee was significantly greater than that in the OA knee and normal knees (p < 0.05) . A similar trend was observed in PM bundle elongation (Fig. 4).
Fig. 4.
Elongation of the posterior cruciate ligament (PCL) bundles. Length of the anterolateral (AL) and posteromedial (PM) bundle increased with increasing flexion in all three groups of knees. Beyond 75° of flexion, the elongation of the PCL bundles in the PCL-retaining total knee arthroplasty knee was significantly greater than that of the osteoarthritic knee and normal knee
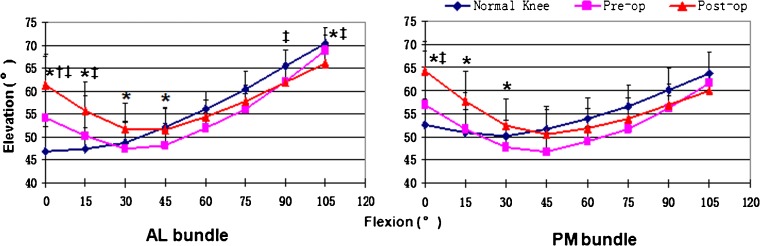
Elevation of PCL bundles
At full extension, the elevation of the AL bundle of the PCL-retaining TKA knees (61.3° ± 6.5°) was significantly larger than that of normal (46.8° ± 5.5°) and OA knees (54.1° ± 13.5°) (p < 0.05) . During knee flexion, elevation of the AL bundle of the normal knee was relatively constant up to 30° of flexion, and thereafter increased steadily with flexion. In the other two groups, however, the elevation angle kept decreasing until around 45° of flexion, and thereafter increased steadily with flexion. Beyond 45° of flexion, the elevation angles of the AL bundles in the three groups were generally similar. The similar trend was observed in the PM bundle elevation (Fig. 5).
Fig. 5.
Elevation of posterior cruciate ligament (PCL) bundles. Elevation angle of the anterolateral (AL) bundle was generally lower than that of the posteromedial (PM) bundle before 45° of flexion in all groups. However, after 45° of flexion, the elevation angle of the AL bundle increased dramatically and became greater than that of the PM bundle in all groups
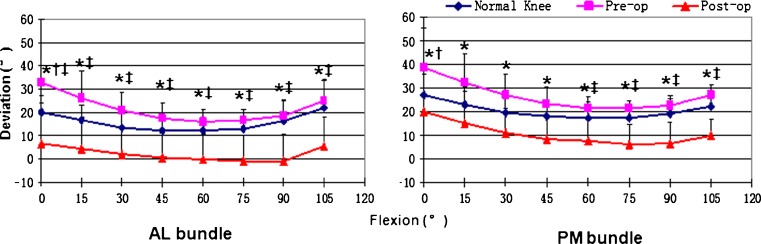
Deviation of PCL bundles
At full extension, the deviation angle of the AL bundle was 20.1° ± 7.0°, 32.7° ± 17.3° and 6.6° ± 17.6° for normal, OA and PCL-retaining TKA knees, respectively. Differences among groups were significant (p < 0.05). Throughout knee flexion, the AL bundle was oriented medially in both normal and OA knees. In contrast, the AL bundle oriented almost AP without medial deviation in PCL-retaining TKA knees (p < 0.05). A similar trend was observed in the PM bundle deviation (Fig. 6).
Fig. 6.
Deviation of posterior cruciate ligament (PCL) bundles. The anterolateral (AL) and posteromedial (PM) bundles were oriented medially in both normal and osteoarthritic knees throughout knee flexion. In contrast, AL and PM bundles showed little or even no medial deviation in the PCL-retaining total knee arthroplasty knee
Discussion
The major findings of this study were that PCL bundles of OA knees showed greater elongation during late flexion and were orientated more medially throughout flexion compared with normal knees. After PCL-retaining TKA, PCL bundles showed further increase in elongation during late flexion, and the medial orientation of PCL bundles decreased substantially. Our data show that AL and PM bundles of the PCL elongated continuously with increasing flexion in all three groups, which was consistent with the previous in vitro studies reporting that the PCL force increased with flexion in both normal and PCL-retaining TKA knees [3, 8, 11, 16, 18]. Interestingly, our study found that elongation of PCL bundles in PCL-retaining TKA knees was significantly greater than those of normal and preoperative OA knees during late knee flexion, suggesting the PCL may have become tighter after PCL-retaining TKA at high flexion in this group of patients. Overstretching of the PCL was correlated to the reduced posterior femoral translation (femoral rollback) in the same patient group after PCL-retaining TKA [25]. Reduction of femoral rollback has also been observed in many previous studies of PCL-retaining TKAs [2, 23]. The possible explanation may be the so-called kinematic conflict that occurs in knee flexion, that is, the PCL tightens in high flexion angles and encourages femoral rollback, but the posterior lip of the dished tibial insert acts as a restraint against femoral rollback and results in kinematic conflict, with progressive tightening of the PCL [17].
Controversy exists about the PCL force in the PCL-retaining TKA knees, but it has been consistently reported that PCL force is not fully restored to normal after PCL-retaining TKA [7, 13]. Incavo et al. studied eight knees and found that the PCL was too tight in three knees and too loose in another three knees after PCL-retaining TKA [7]. Mahoney et al. tested eight knees and found that in most cases, the PCL was overtightened after PCL-retaining TKA [13]. Li et al. found that PCL force decreased after PCL-retaining TKA compared with normal knees [12]. Differences among these studies may be caused by the different loading conditions applied and the number of knees requiring PCL recession during the operation. Although the length measured in our study should not be directly used to calculate PCL forces, overstretching of the PCL observed in PCL-retaining TKA knees may limit further knee flexion or lead to ligament failure [13].
PCL is the primary restraint to the posterior translation of the tibia during knee flexion in healthy knees [9]. However, little is known about the relative role of the AL and PM bundles in the stabilisation function of the PCL in OA and PCL-retaining TKA knees. Our study shows that in all three groups, elevation of the AL bundle was relatively lower than that of the PM bundle before 45° of flexion, but after 45°, elevation of the AL bundle increased dramatically and was higher than that of the PM bundle. Our data suggests that during high flexion, the AL bundle restrains the proximal–distal translation and induces posterior femoral translation, whereas the PM bundle may be more efficient in resisting posterior tibial translation. The similar trend has also been observed in normal knees by other investigators [1, 3, 18]. Results demonstrate that both AL and PM bundles of the PCL are important in maintaining normal knee kinematics.
The study presented here shows that in the mediolateral direction, PCL bundles are oriented medially in normal knees, in line with previous studies [3, 18]. An oblique PCL produces rotation torque during flexion and acts as a guiding bundle in knee rotation [5]. After PCL-retaining TKA, however, PCL bundles change to be almost in a sagittal plane orientation. In other words, the PCL changed from the guiding bundle to a sagittal bundle [5]. Fuss et al. demonstrated that a sagittal bundle has no effect on knee rotation, even if it is constantly tight during flexion [5]. Reduced internal tibial rotation has been observed in both PCL-deficient knees and PCL-retaining TKAs [4, 9, 23] and may suggest PCL dysfunction in controlling rotation in PCL-retaining TKA knees in addition to the tibiofemoral articular geometry change after TKA. Earlier in vitro studies demonstrated that the ACL oriented medially, so that the ACL would provide resistance to lateral translation of the femur [10]. In ACL-deficient knees, a lateral shift of the femur was observed when compared with normal knees [10]. As the ACL is resected in a PCL-retaining TKA, the constraining function of ACL to lateral femoral shift is lost. This might result in lateral femoral translation.
There are limitations to this study: PCL bundle lengths were measured using the distance between their femoral and tibial attachment sites. The relative elongation of the two PCL bundles exceeded 20% in all three groups, which was larger than the ultimate strain of the PCL reported in the literature [19], indicating that the PCL was lax at full extension; that is, the distance between the attachment sites is less than the length of the PCL. Therefore, this distance should not be directly used to calculate in vivo PCL strain [3, 18]. The second limitation is that the study only represents results of one particular PCL-retaining implant. Future work will involve evaluation of other TKA designs. In addition, the study only evaluated knees with predominantly medial-compartment OA, and the PCL of the knees with other disease situations, such as lateral-compartment OA, should have different in vivo performance. Finally, we studied knee behaviour in a single leg-lunge activity. Future study should also examine knee functions during dynamic activities, such as gait.
In conclusion, our study shows the current PCL-retaining TKA systems and surgical techniques may not adequately re-establish normal biomechanics of PCL bundles after PCL-retaining TKA. Additional studies evaluating other TKA systems and other dynamic activities, such as gait, would be valuable.
Acknowledgments
This study was partially supported by an AEF grant from the Department of Orthopaedics, Massachusetts General Hospital. This study was also supported by the Fund of Science and Technology Commission of Shanghai (11QA1404100), Shanghai Municipal Health Bureau (XYQ2011024), and National Natural Science Foundation of China (30901517).
Conflict of interest
All authors disclose any financial and personal relationships with other people or organisations that could inappropriately influence (bias) this work.
References
- 1.Amis AA, Gupte CM, Bull AM, et al. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14:257–263. doi: 10.1007/s00167-005-0686-x. [DOI] [PubMed] [Google Scholar]
- 2.Casino D, Martelli S, Zaffagnini S, et al. Knee stability before and after total and unicondylar knee replacement: in vivo kinematic evaluation utilizing navigation. J Orthop Res. 2009;27:202–207. doi: 10.1002/jor.20746. [DOI] [PubMed] [Google Scholar]
- 3.Defrate LE, Gill TJ, Li G. In vivo function of the posterior cruciate ligament during weightbearing knee flexion. Am J Sports Med. 2004;32:1923–1928. doi: 10.1177/0363546504264896. [DOI] [PubMed] [Google Scholar]
- 4.Fantozzi S, Catani F, Ensini A, et al. Femoral rollback of cruciate-retaining and posterior-stabilized total knee replacements: in vivo fluoroscopic analysis during activities of daily living. J Orthop Res. 2006;24:2222–2229. doi: 10.1002/jor.20306. [DOI] [PubMed] [Google Scholar]
- 5.Fuss FK. Principles and mechanisms of automatic rotation during terminal extension in the human knee joint. J Anat. 1992;180(Pt 2):297–304. [PMC free article] [PubMed] [Google Scholar]
- 6.Hirsch HS, Lotke PA, Morrison LD. The posterior cruciate ligament in total knee surgery. Save, sacrifice, or substitute? Clin Orthop Relat Res. 1994;309:64–68. [PubMed] [Google Scholar]
- 7.Incavo SJ, Johnson CC, Beynnon BD, et al. Posterior cruciate ligament strain biomechanics in total knee arthroplasty. Clin Orthop Relat Res. 1994;309:88–93. [PubMed] [Google Scholar]
- 8.Li G, Defrate LE, Sun H, et al. In vivo elongation of the anterior cruciate ligament and posterior cruciate ligament during knee flexion. Am J Sports Med. 2004;32:1415–1420. doi: 10.1177/0363546503262175. [DOI] [PubMed] [Google Scholar]
- 9.Li G, Gill TJ, Defrate LE, et al. Biomechanical consequences of PCL deficiency in the knee under simulated muscle loads–an in vitro experimental study. J Orthop Res. 2002;20:887–892. doi: 10.1016/S0736-0266(01)00184-X. [DOI] [PubMed] [Google Scholar]
- 10.Li G, Papannagari R, Defrate LE, et al. Comparison of the ACL and ACL graft forces before and after ACL reconstruction: an in vitro robotic investigation. Acta Orthop. 2006;77:267–274. doi: 10.1080/17453670610046019. [DOI] [PubMed] [Google Scholar]
- 11.Li G, Zayontz S, Most E, et al. In situ forces of the anterior and posterior cruciate ligaments in high knee flexion: an in vitro investigation. J Orthop Res. 2004;22:293–297. doi: 10.1016/S0736-0266(03)00179-7. [DOI] [PubMed] [Google Scholar]
- 12.Li G, Zayontz S, Most E, et al. Cruciate-retaining and cruciate-substituting total knee arthroplasty: an in vitro comparison of the kinematics under muscle loads. J Arthroplasty. 2001;16:150–156. doi: 10.1054/arth.2001.28367. [DOI] [PubMed] [Google Scholar]
- 13.Mahoney OM, Noble PC, Rhoads DD, et al. Posterior cruciate function following total knee arthroplasty. A biomechanical study. J Arthroplasty. 1994;9:569–578. doi: 10.1016/0883-5403(94)90110-4. [DOI] [PubMed] [Google Scholar]
- 14.Matsuda S, Miura H, Nagamine R et al (1999) Knee stability in posterior cruciate ligament retaining total knee arthroplasty. Clin Orthop Relat Res 169–173 [DOI] [PubMed]
- 15.Matsuda S, Miura H, Nagamine R, et al. Knee stability in posterior cruciate ligament retaining total knee arthroplasty. Clin Orthop Relat Res. 1999;366:169–173. doi: 10.1097/00003086-199909000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Most E, Li G, Sultan PG, et al. Kinematic analysis of conventional and high-flexion cruciate-retaining total knee arthroplasties: an in vitro investigation. J Arthroplasty. 2005;20:529–535. doi: 10.1016/j.arth.2004.09.034. [DOI] [PubMed] [Google Scholar]
- 17.Pagnano MW, Cushner FD, Scott WN. Role of the posterior cruciate ligament in total knee arthroplasty. J Am Acad Orthop Surg. 1998;6:176–187. doi: 10.5435/00124635-199805000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Papannagari R, Defrate LE, Nha KW, et al. Function of posterior cruciate ligament bundles during in vivo knee flexion. Am J Sports Med. 2007;35:1507–1512. doi: 10.1177/0363546507300061. [DOI] [PubMed] [Google Scholar]
- 19.Race A, Amis AA. The mechanical properties of the two bundles of the human posterior cruciate ligament. J Biomech. 1994;27:13–24. doi: 10.1016/0021-9290(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 20.Rand JA, Trousdale RT, Ilstrup DM, et al. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85-A:259–265. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Scott RD. Would that it were so: save the PCL! Orthopedics. 2001;24:888–889. doi: 10.3928/0147-7447-20010901-29. [DOI] [PubMed] [Google Scholar]
- 22.Seon JK, Park JK, Jeong MS, et al. Correlation between preoperative and postoperative knee kinematics in total knee arthroplasty using cruciate retaining designs. Int Orthop. 2011;35:515–520. doi: 10.1007/s00264-010-1029-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siston RA, Giori NJ, Goodman SB, et al. Intraoperative passive kinematics of osteoarthritic knees before and after total knee arthroplasty. J Orthop Res. 2006;24:1607–1614. doi: 10.1002/jor.20163. [DOI] [PubMed] [Google Scholar]
- 24.Tsuji S, Tomita T, Hashimoto H, et al. Effect of posterior design changes on postoperative flexion angle in cruciate retaining mobile-bearing total knee arthroplasty. Int Orthop. 2011;35:689–695. doi: 10.1007/s00264-010-1060-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yue B, Varadarajan KM, Moynihan AL, et al. Kinematics of medial osteoarthritic knees before and after posterior cruciate ligament retaining total knee arthroplasty. J Orthop Res. 2011;29:40–46. doi: 10.1002/jor.21203. [DOI] [PubMed] [Google Scholar]