Abstract
Purpose
The aim of this study was to identify factors which contribute to loss of reduction (LOR).
Methods
Outpatient records and initial, post-reduction (PR) and follow-up radiographs of patients with a distal radial metaphyseal fracture were reviewed to determine demographic factors; fracture characteristics (obliquity, comminution, intact ulna); three-point cast index (3PI); and initial, PR, and follow-up displacement (angulation and translation in the sagittal and coronal planes). Univariate and multivariate regression were used to identify significant risk factors for LOR.
Results
A total of 161 patients were included in our series (119 boys and 42 girls). Fifty-seven (35%) patients met the criteria for LOR. Multivariate logistic regression revealed that patients over 14 years old were 4.8 times more likely (p = 0.01) to lose reduction, and those with more than 10% PR translation in the sagittal plane were four times more likely (p = 0.03) to lose reduction. In younger patients, initial coronal translation and PR sagittal translation were independent risk factors. Patients with over 10% initial translation in the coronal plane were 2.4 times more likely (p = 0.01) to lose reduction, and those with over 10% PR translation in the sagittal plane were 2.7 times more likely (p = 0.03) to lose reduction. Three point cast index was not found to be a significant risk factor (1.64 vs. 1.57, p = 0.43).
Conclusion
Our study, the largest dedicated series of distal radial metaphyseal fractures, indicates that loss of reduction is common. Our analysis suggests that an anatomical reduction, which minimises residual translation, is the most important variable in preventing a loss of reduction.
Introduction
Distal forearm injuries are among the most frequently encountered orthopaedic injuries in the paediatric emergency department [1, 2]. The distal radius is the most common fracture site within forearm fractures, accounting for 20–30% of these fractures [3, 4]. Most of these fractures occur at the metaphysis [5].
Immediate closed reduction and cast immobilisation is the mainstay of management for the majority of these fractures [2, 6]. Some authors have reported good outcomes with non-operative management with few complications or long-term problems [7]; however, other authors have reported loss of reduction rates between 10% and 91%. In general, up to one third of cases will demonstrate late displacement [8, 9].
Risk of re-displacement is multifactorial [6]. Factors leading to re-displacement have been reported in the literature and can be broadly divided into three groups: (1) Fracture-related factors such as initial displacement, and increased obliquity of the fracture line [8, 10, 11]; (2) Treatment-related factors such as residual angulation after initial reduction and poor casting technique [10]; and (3) Patient-related factors such as muscle atrophy and resolution of initial soft tissue swelling while in the cast [5].
Some recent reports have advocated the routine use of percutaneous pin fixation as the initial treatment of high risk fractures [8, 9]. The aim of this study was to identify those fractures with a high risk of re-displacement and analyse the associated potential risk factors.
Material and methods
After Institutional Review Board approval, billing records were queried from January 1, 2006 to June 1, 2010 to identify children who were treated by closed reduction and casting in our Emergency Department for a displaced closed metaphyseal distal radius fracture.
Patients were included if they had sustained a bicortical, displaced metaphyseal distal radius fracture requiring reduction and cast immobilisation in our Emergency Department and had at least three weeks follow-up with complete radiographic and medical records. All reductions were performed under conscious sedation by orthopaedic staff using a C-arm to verify the reduction; a fibreglass cast was used in all cases. Diaphyseal, intra-articular, physeal, pathological, and open fractures were excluded as were patients whose initial displacement was treated at an outside institution. In addition, patients with incomplete radiographic or medical records were excluded.
A retrospective chart and radiographic review was performed using the hospital electronic medical records to obtain data regarding age, sex, mechanism of injury (fall below own height, fall above own height, sports related, etc.), length of follow-up, initial angulation and translation (AP and lateral), initial shortening, dorsal comminution, obliquity of fracture (higher angle among AP/lateral views), associated ulna fracture, post reduction residual angulation and translation (AP and lateral) and three-point cast index (3PI) that was calculated according to the formula of Alemdaroglu et al. [11]. The primary outcome used was presence of loss of reduction of the fracture during follow-up.
Loss of reduction (LOR) was defined as an angulation of 15° or more in the coronal plane for all ages and/or angulation in the sagittal plane up to 30° if more than five years of growth remaining and 5° less for each year less than five [18]. Additionally, all patients who were re-manipulated or had a closed reduction and percutaneously pinned before loss of reduction according to our definition were excluded.
Analysis was performed on the entire cohort as well as a subgroup analysis on patients aged under 11 years and 11 years or more. This cutoff point was chosen based on the senior author’s experience.
Statistical analysis
Univariate and multivariate statistical analysis was performed with LOR being the outcome of interest. When a risk factor was a continuous variable with normal distribution, the Student’s t-test for unpaired samples was used with equal variances not assumed. When the risk factor was continuous and the distribution of that variable was not normal, the Mann–Whitney U test was used to test the hypothesis that the variables came from similar distributions versus the alternative that the distributions were different. Chi squared tests were performed for dichotomous or categorical variables. In cases where fewer than 20 per cell were present, Yates correction for continuity was employed, and in cases where less than five were present in any cell, the Fisher’s exact test was used. Multivariate binary logistic regression was used to adjust for any potential confounder which was found on univariate logistic regression to have a significance of 0.10 or less. A backward likelihood ratio method was used to eliminate variables, starting at the least significant, and progressing until removal of any further variables caused a change in the likelihood ratio which was significant at the 0.10 level or less. Following this, continuous variables were dichotomized using a receiver operator characteristics analysis to determine what the optimum cutoff was in our data. Then the multivariate analysis was re-analysed using the dichotomous version of the variable. All statistics were calculated with SPSS version 16.0 (SPSS Inc., Chicago, IL).
Results
A total of 161 patients had their closed reductions and casting performed at our centre and met the inclusion criteria (119 boys and 42 girls) with a mean of 10.2 years of age. There were 94 patients in the under 11 years of age group (61 boys and 33 girls) with an average of 7.7 years of age, and 67 patients in the over 11 years of age group (58 boys and nine girls) with an average of 13.6 years of age. All patients were followed up until radiographic union with a mean follow-up of 2.8 months (range, 0.7–14.5 months).
During the treatment period, 57 of 161 patients met criteria for loss of reduction (35%). In patients over 11 years of age, 22 patients of 67 lost reduction (32.8%) and within the under 11 years of age group, 35 of 94 lost reduction (37.2%).
Based on univariate logistic regression analysis within the entire group of patients, initial angulation and translation in the coronal plane, residual translation in the coronal plane, initial translation and residual translation in the sagittal plane and initial shortening were significantly different between those who did and did not lose reduction (Table 1). Dorsal comminution (p = 0.308), mechanism of injury (p = 0.626), an intact ulna (p = 0.255) and 3PI (p = 0.43) were not found to be significant risk factors. Patients with an intact ulna showed higher residual translation in the sagittal plane after closed reduction than those with a fractured ulna (14.1% vs. 7.5%; p = 0.0041). Multivariate logistic regression revealed initial translation in the coronal plane as an independent risk factor for LOR (13% vs 27% , p = 0.007).
Table 1.
Univariate analysis of potential risk factors for loss of reduction in the entire group of patients
| Variable | Non-redisplaced | Redisplaced | p value | ||
|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | ||
| Age | 10.22 | 8.24–12.2 | 10.09 | 8.11–12.07 | 0.83 |
| Obliquity (degrees) | 11.64 | 9.93–13.35 | 13.28 | 11.19–15.37 | 0.153 |
| Initial angulation (AP) | 8.5 | 6.92–10.08 | 11.16 | 9.30–13.02 | 0.008* |
| Initial angulation (Lat) | 19.53 | 17.27–21.79 | 20.54 | 17.74–23.33 | 0.549 |
| Initial translation (AP) | 12.74 | 8.3–17.17 | 26.8 | 19.88–33.72 | < 0.0001* |
| Initial translation (Lat) | 38.84 | 30.28–47.40 | 58.52 | 48.9–68.15 | 0.002* |
| Initial shortening (%) | 25.84 | 17.3–34.38 | 44.5 | 32.89–56.10 | 0.003* |
| PR angulation (AP) | |||||
| PR angulation (Lat) | 6.61 | 5.71–7.51 | 8.03 | 6.77–9.29 | 0.075 |
| PR translation (AP) | 6.12 | 3.94–8.3 | 10.82 | 7.66–13.98 | 0.004* |
| PR translation (Lat) | 8.4 | 5.68–11.11 | 14.13 | 10.42–17.83 | 0.003* |
| 3 point index | 1.64 | 1.51–1.77 | 1.57 | 1.40–1.75 | 0.430 |
PR post-reduction, AP antero-posterior view (coronal plane), Lat lateral view (sagittal plane)
Angulations were measured in degrees; translation and shortening in percentage
*p ≤ 0.05 (statistically significant)
In children over 11 years of age, initial and residual translation in the sagittal plane as well as age were identified as risk factors based on univariate analysis. Sex (p = 0.999), an intact ulna (p = 0.607), mechanism of injury (p = 0.920) and 3PI (1.35 vs. 1.25; p = 0.404) were not statistically significant. Multivariate logistic regression revealed that age and residual translation in the sagittal plane were both independent risk factors for LOR (Fig. 1). Patients with age 14 years and over were 4.8 times more likely to lose reduction and patients with residual translation in the sagittal plane of 10% or more were four times more likely to lose reduction (Table 2).
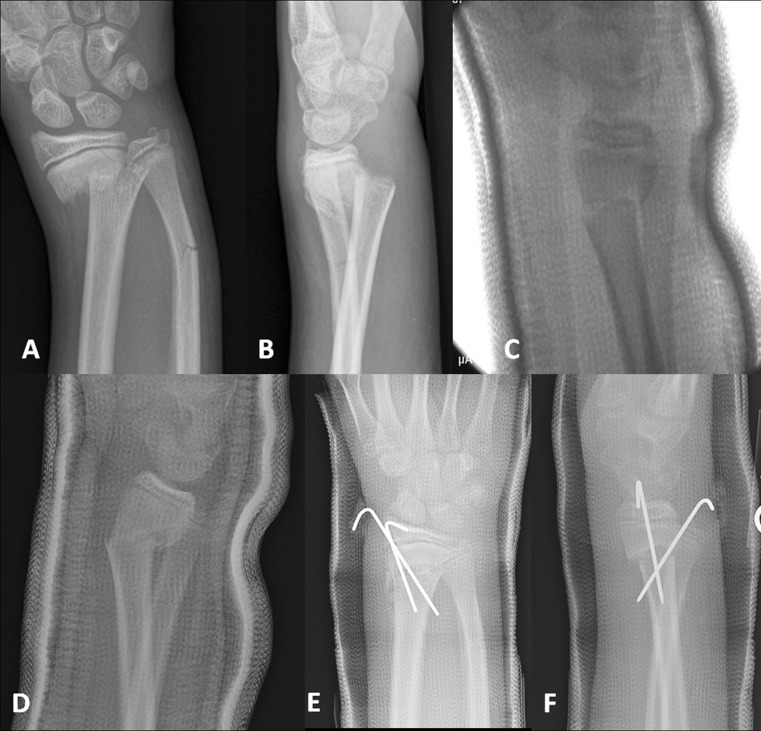
Fig. 1.
A 15-year-old boy who suffered a fall onto his outstretched hand while doing sport-related activities presented to the emergency room with right wrist deformity, swelling, pain and functional limitation. Closed reduction and casting was performed. A Initial PA view of the right wrist showing a distal metaphyseal radius fracture with a broken ulna. There is radial displacement of the distal fragment. B Initial lateral view of the right wrist showing a distal metaphyseal radius fracture with a broken ulna. There is dorsal displacement and some shortening of the distal fragment. C Post-reduction lateral view. There is a residual translation of about 14% of the diameter of the proximal fragment. D Lateral view, two weeks after initial closed reduction and casting. There is an angulation of about 39 degrees. Closed reduction and pinning was performed. E PA view follow-up X-ray after closed reduction and pinning. F Lateral view follow up X-ray after closed reduction and pinning
Table 2.
Odds ratios for a simple model predicting failure based on re-displacement criteria after closed reduction and casting of a distal metaphyseal radius fracture in children over 11 years of age
| Variable | Odds ratio | 95% CI | p value |
|---|---|---|---|
| Age (14+ vs 0–13) | 4.8 | (1.6,14.1) | 0.01 |
| PR translation (lat)(10% vs 0–9%) | 4 | (1.3,11.9) | 0.03 |
PR post-reduction, Lat lateral view (sagittal plane)
Translation was measured in percentage
*p ≤ 0.05 (statistically significant)
In children under 11 years of age, initial and residual translation both in the coronal plane as well as initial shortening and residual translation in the sagittal plane were identified as risk factors based on univariate analysis. Sex (p = 0.999), an intact ulna (p = 0.518), and mechanism of injury (p = 0.985) were not statistically significant. These results are similar to those of the entire group, because the majority of patients are in this subgroup. Multivariate logistic regression revealed that initial translation in the coronal plane and residual translation in the sagittal plane were both independent risk factors for LOR (Table 3). Patients with initial coronal translation 10% or more were 2.4 times more likely to lose reduction, and patients with residual sagittal translation ≥10% were 2.7 times more likely to LOR. Note that in both subgroups residual sagittal translation is an independent risk factor for LOR.
Table 3.
Odds ratios for a simple model predicting failure based on re-displacement criteria after closed reduction and casting of a distal metaphyseal radius fracture in children under 11 years of age
| Variable | Odds ratio | 95% CI | p value |
|---|---|---|---|
| Initial translation (AP) (10% vs 0–9%) | 2.4 | (1.0, 6.3) | 0.01 |
| PR translation (lat) (10% vs 0–9%) | 2.7 | (1.1, 7.1) | 0.03 |
Translation was measured in percentage
PR post-reduction, Lat lateral view (sagittal plane), AP antero-posterior view (coronal plane)
*p ≤ 0.05 (statistically significant)
Of the 57 patients (35 over 11 years and 22 11 years and over) who lost reduction, seven were re-manipulated and casted without pinning (four over 11 years and three 11 years and over), and 22 underwent repeat closed reduction and pinning (eight under 11 years and 14 11 years and over). In 28 patients, the deformity was accepted (23 less than 11 years and five 11 years or more).
Discussion
Closed manipulation and casting is the accepted treatment of displaced metaphyseal distal radius fractures in children [12, 13]; however, the rate of re-displacement of these fractures after initial closed reduction and casting is high. A wide range of re-displacement rates has been reported in the literature, ranging from 24% to 45.8% [9–11, 14, 15]. A 35% re-displacement rate was found in our series, with a higher re-displacement rate within the older cohort. It is important to note that multiple definitions for re-displacement have been used due to the lack of consensus on what constitutes unacceptable reduction, and this fact should be taken into account when interpreting these results.
Previous studies on this fracture type have shown that initial displacement [8–11, 15, 16], failure to achieve a complete reduction [8, 10, 13, 17], distal radius fracture with or without an ulna fracture [9, 11, 17, 18], age [19], obliquity of the fracture [8, 9] and poor casting [8] are significant risk factors for loss of reduction in this age group.
Widmann et al. [19] found that complete metaphyseal distal radius fractures were at higher risk for LOR, and 50% of these fractures in children over ten years of age lose initial reduction. In our series, we found that increased age in the older cohort was an independent risk factor for LOR; patients 14 years old or more were 4.8 times more likely to lose reduction. This finding is important to take into account when treating older children as they have a reduced potential for remodeling [20].
Several authors agree that initial fracture displacement is an important risk factor for LOR [8–11, 13, 15, 16], with the theory that rupture of the periostium results in a lack of restraint [15]. Displacement greater than 50% of the diameter of the bone at the fracture site has been described as a risk factor for LOR [15, 16]. Zamzam et a. [11] reported that patients with a complete initial displacement of the fracture were 24.7 times more likely to lose reduction. Our findings agree with this as initial translation in the coronal plane ≥10% of the bone diameter is an increased risk for LOR for patients in the under 11 years of age cohort.
A perfect anatomical reduction is one of the most widely accepted factors preventing re-displacement [10]. According to Alemdaroglu et al. [8], an incompletely reduced fracture is five times more likely to re-displace than those anatomically reduced. Roy et al. [17] reported that fractures reduced to less than 50% apposition required re-manipulation more frequently. In our series, an incompletely reduced fracture was also found to be an independent risk factor for LOR in both cohorts. The risk for LOR was four times higher in the older cohort and 2.7 times within the younger ones.
A properly padded and moulded cast minimises the risk of re-displacement [21]. In order to assess the quality of casting, several casting indices have been described such as the cast index [6], padding index [21], gap index [22], Canterbury index [21] and the three-point index [8]. Alemdaroglu et al. [8] found that the three-point index was superior to the other radiographic indices with regard to prediction of re-displacement. This index is based on the basic principle of moulding the cast using the Charnley three-point fixation principle [13]. This index involves complex calculations and was not found to have a significant effect on the risk of re-displacement in our study, and we feel that could have a bearing on its practical application. We also noted that the values found either in the non re-displaced group or re-displaced group were higher than those described by Alemdaroglu et al. [8]. This could be explained by the fact that all patients in our study received fibreglass casts, which are more difficult to mould than when plaster of Paris is used, leaving wider gaps between the fiberglass and the skin.
The role of an intact ulna remains controversial. Proctor et al. [10] and Alemdaroglu et al. [8] did not find a broken ulna to be a significant risk factor for LOR; however, Zamzam et al. [11] described that an associated ulnar fracture was a risk factor for LOR. Gibbons et al. [18] found that isolated distal radius fractures were more unstable and prone to re-angulation than were distal radial fractures associated with an ulnar fracture. In our series, we did not find an intact ulna to be a significant risk factor for LOR; however, we did find that patients with an intact ulna had a higher residual translation (sagittal plane) after reduction than those with a fractured ulna. This confirms that these fractures are more difficult to reduce [17], and may enhance other potential risk factors for LOR.
Fractures of the distal radius usually heal promptly, nonunion is uncommon, and some degree of displacement can be accepted because of the excellent remodelling potential that will occur [20]. Authors have described 0.8–1° of correction per month [23–25].
Closed reduction and pinning has been recommended by some authors in high risk patients for LOR [11, 16, 18] based on the fact that a visible deformity can be seen, which worries the parents and creates anxiety. This anxiety could be greater if an additional reduction is needed because of the need for further general anaesthesia and the diminished trust after failure of the initial treatment [9]. Arguments for closed reduction percutaneous pinning (CRPP) include: a better maintenance of reduction [9], fewer follow-up X-rays [25] and a low rate of complications [11, 18]. However, the long-term functional outcome of a re-displaced distal radius fracture has not yet been clarified. Do et al. [7] found that in the group with residual angulation, the average time for remodelling was four months, and all those patients had full range of motion and were back to normal activities without restrictions. However, the mean age was 9.2 years and the oldest was 14 years of age. Miller et al. [14] found no difference in terms of functional outcome when closed reduction and casting was compared to closed reduction and pinning.
Limitations of this study include its retrospective nature and lack of sufficient follow-up to evaluate remodelling and the functional outcomes of patients whose loss of reduction was accepted without re-manipulation and or pinning.
Regardless of these limitations, this study, the largest dedicated series of distal radial metaphyseal fractures, indicates that loss of reduction is common. Our analysis suggests that an anatomical reduction, which minimises residual translation, is the most important variable in preventing loss of reduction. Fractures at highest risk of re-displacement were those presented in patients 14 years old or older with a residual translation in the sagittal plane 10% or more, and in these closed reduction and pinning after failed closed reduction and casting could be an option.
Acknowledgments
Conflict of interest statement
The authors declare that they have no conflict of interest.
References
- 1.Galano GJ, Vitale MA, Kessler MW, Hyman JE, Vitale MG. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop. 2005;25:39–44. doi: 10.1097/00004694-200501000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Pershad J, Williams S, Wan J, Sawyer JR. Pediatric distal radial fractures treated by emergency physicians. J Emerg Med. 2009;37:341–344. doi: 10.1016/j.jemermed.2008.08.030. [DOI] [PubMed] [Google Scholar]
- 3.Bae DS. Pediatric distal radius and forearm fractures. J Hand Surg Am. 2008;33:1911–1923. doi: 10.1016/j.jhsa.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez-Merchan EC (2005) Pediatric fractures of the forearm. Clin Orthop Relat Res 432:65–72 [PubMed]
- 5.Pretell Mazzini J, Rodriguez Martin J. Paediatric forearm and distal radius fractures: Risk factors and re-displacement-role of casting indices. Int Orthop. 2010;34(3):407–412. doi: 10.1007/s00264-009-0904-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones K, Weiner DS. The management of forearm fractures in children: A plea for conservatism. J Pediatr Orthop. 1999;19:811–815. doi: 10.1097/00004694-199911000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Do TT, Strub WM, Foad SL, Mehlman CT, Crawford AH. Reduction versus remodeling in pediatric distal forearm fractures: A preliminary cost analysis. J Pediatr Orthop B. 2003;12:109–115. doi: 10.1097/00009957-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Alemdaroglu KB, Iltar S, Cimen O, Uysal M, Alagoz E, Atlihan D. Risk factors in redisplacement of distal radial fractures in children. J Bone Joint Surg Am. 2008;90:1224–1230. doi: 10.2106/JBJS.G.00624. [DOI] [PubMed] [Google Scholar]
- 9.Leemput W, Ridder K. Distal metaphyseal radius fractures in children: Reduction with or without pinning. Acta Orthop Belg. 2009;75:306–309. [PubMed] [Google Scholar]
- 10.Proctor MT, Moore DJ, Paterson JM. Redisplacement after manipulation of distal radial fractures in children. J Bone Joint Surg Br. 1993;75:453–454. doi: 10.1302/0301-620X.75B3.8496221. [DOI] [PubMed] [Google Scholar]
- 11.Zamzam MM, Khoshhal KI. Displaced fracture of the distal radius in children: Factors responsible for redisplacement after closed reduction. J Bone Joint Surg Br. 2005;87:841–843. doi: 10.1302/0301-620X.87B6.15648. [DOI] [PubMed] [Google Scholar]
- 12.Bae DS, Flynn JM, Frick SL, Noonan KJ (2009) The operative management of pediatric upper extremity fractures, forearm and wrist injuries. American Academy of Orthopaedic Surgeons Annual Meeting, February, Las Vegas, NV
- 13.Sharma S, Bowe D, Walters SJ, Flowers MJ. Dorsal cortical comminution as a predictor of redisplacement of distal radius fractures in children. Injury. 2011;42(2):173–177. doi: 10.1016/j.injury.2010.07.409. [DOI] [PubMed] [Google Scholar]
- 14.Miller BS, Taylor B, Widmann RF, Bae DS, Snyder BD, Waters PM. Cast immobilization versus percutaneous pin fixation of displaced distal radius fractures in children: A prospective, randomized study. J Pediatr Orthop. 2005;25:490–494. doi: 10.1097/01.bpo.0000158780.52849.39. [DOI] [PubMed] [Google Scholar]
- 15.Mani GV, Hui PW, Cheng JC. Translation of the radius as a predictor of outcome in distal radial fractures of children. J Bone Joint Surg Br. 1993;75:808–811. doi: 10.1302/0301-620X.75B5.8376446. [DOI] [PubMed] [Google Scholar]
- 16.Choi KY, Chan WS, Lam TP, Cheng JC. Percutaneous kirschner-wire pinning for severely displaced distal radial fractures in children. A report of 157 cases. J Bone Joint Surg Br. 1995;77:797–801. [PubMed] [Google Scholar]
- 17.Roy DR. Completely displaced distal radius fractures with intact ulnas in children. Orthopedics. 1989;12:1089–1092. doi: 10.3928/0147-7447-19890801-09. [DOI] [PubMed] [Google Scholar]
- 18.Gibbons CL, Woods DA, Pailthorpe C, Carr AJ, Worlock P. The management of isolated distal radius fractures in children. J Pediatr Orthop. 1994;14:207–210. doi: 10.1097/01241398-199403000-00014. [DOI] [PubMed] [Google Scholar]
- 19.Widman R WP, Reeves S (1994) Complications of closed treatment of distal radius fractures in children. Edited by America, A. M. o. t. P. O. S. o. N., Miami, FL
- 20.Hove LM, Brudvik C. Displaced paediatric fractures of the distal radius. Arch Orthop Trauma Surg. 2008;128:55–60. doi: 10.1007/s00402-007-0473-x. [DOI] [PubMed] [Google Scholar]
- 21.Bhatia M, Housden PH. Re-displacement of paediatric forearm fractures: Role of plaster moulding and padding. Injury. 2006;37:259–268. doi: 10.1016/j.injury.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Malviya A, Tsintzas D, Mahawar K, Bache CE, Glithero PR. Gap index: A good predictor of failure of plaster cast in distal third radius fractures. J Pediatr Orthop B. 2007;16:48–52. doi: 10.1097/01.bpb.0000236232.57269.ec. [DOI] [PubMed] [Google Scholar]
- 23.Friberg KS. Remodelling after distal forearm fractures in children. III. Correction of residual angulation in fractures of the radius. Acta Orthop Scand. 1979;50:741–749. doi: 10.3109/17453677908991304. [DOI] [PubMed] [Google Scholar]
- 24.Friberg KS. Remodelling after distal forearm fractures in children. II. The final orientation of the distal and proximal epiphyseal plates of the radius. Acta Orthop Scand. 1979;50:731–739. doi: 10.3109/17453677908991303. [DOI] [PubMed] [Google Scholar]
- 25.Friberg KS. Remodelling after distal forearm fractures in children. I. The effect of residual angulation on the spatial orientation of the epiphyseal plates. Acta Orthop Scand. 1979;50:537–546. doi: 10.3109/17453677908989801. [DOI] [PubMed] [Google Scholar]