Abstract
Purpose
Displaced type 2 lateral end clavicle fractures have a tendency to delayed union or non-union. Various methods of stabilisation of the displaced lateral end fractures are described. The increasing use of implants to fix such fractures also necessitates extensive dissection for implant retrieval. Adequate reduction and minimal tissue trauma during implant placement and removal would be ideal modalities for fixation of such fractures.
Methods
All displaced type 2 lateral end clavicle fractures fulfilling our inclusion criteria were reduced with a small anterosuperior incision. Anteroposterior drill holes were made in both the fragments and a nonabsorabable polyester suture was passed through. The fracture was reduced and fixed with transacromial smooth Kirshner wires. The suture was tied with the knot superiorly in a figure-eight manner. The arm was supported in an arm pouch for six weeks. The Kirshner wire was routinely removed after six weeks in an out-patient department. Clinico-radiological outcome was studied at six weeks, and monthly intervals thereafter until union.
Results
All 16 fractures united. The mean average age of patients was 36.25 years with a SD of 11.35. There was no loss of reduction even after removal of Kirshner wires at six weeks. The mean average time of union was 10.75 weeks with a SD of 3.92. All patients regained near normal range of motion, and the mean average constant score at the end of one year was 98.37 with a SD of 2.87. All patients returned to preinjury level by the one-year follow-up. The range of motion remained the same in those who were followed up in successive years. Skin impingement with bent Kirshner wires were noted in four cases. Kirshner wires backed out in one case before six weeks but there was no loss of reduction. Infection and Kirshner wire breakage were not noted in our series.
Conclusion
The clinico-radiological outcomes with our modified tension band fixation for displaced type 2 lateral end clavicle fractures were encouraging and comparable with earlier studies.
Introduction
Clavicle fractures are often treated conservatively. However, lateral end fractures need special attention, more so with the displaced variety. Based on Neer’s classification system, there are three types of fractures of lateral end of the clavicle [1]. Type 1 fractures are the stable fractures lateral to the coracoclavicular ligament attachment. Type 2 fractures are unstable fractures with damage to the coracoclavicular ligament causing a loss of ligamentous connection between the coracoid and the medial fragment. Type 3 fractures are the intra-articular fractures at the acromio-clavicular joint.
The fate of conservatively treated displaced type 2 fracture is either bony union, fibrous union or nonunion. The rate of nonunion is as high as 30% in the literature [1, 2]. Nonunion of the lateral end of the clavicle is painful and operative treatment has been suggested [3–5]. Several authors have recommended open reduction and internal fixation for type 2 fractures of the distal clavicle because of their tendency to slow healing and residual shoulder disability [6].
The ideal method of internal fixation remains controversial to date. However, a few series of coracoclavicular screws [7–9], tension bands [10–12], Kirshner wires [1, 13], hook plates [14, 15] and contoured locked and non locked plates [16–18] have been published with encouraging results in all series. Feared complications of open reduction and internal fixation (ORIF) include fixation failure, pin migration, refracture, malunion and extensive tissue dissection during hardware removal [12, 19].
Levy [20] described a minimally invasive suture fixation with good outcome, which obviates the need for implant removal. Badhe et al. [21] modified the Levy technique and mentioned tension band suturing for such displaced type 2 lateral end clavicle fractures with 100% union in their series. We share our results using modified tension band fixation of displaced type 2 fracture of the lateral end clavicle.
We favour minimal tissue dissection, rigid fixation with trans-acromial Kirshner wires and tensioning with non-absorbable polyester suture Ethibond (Johnson & Johnson). With our modified tension band fixation, we achieved encouraging results in a small cohort of 16 patients.
Patients and methods
This prospective study was conducted at the Civil Service Hospital of Nepal from 2008 to 2011 with a minimum of one-year follow up. Neer’s type 2 displaced fracture of less than three weeks duration of an adult volunteer having controlled medical comorbidities at time of admission were included in this study. Preoperative assessment with anteroposterior X-ray of clavicle was undertaken in all patients. All operations were done in the beach chair position by author LR. A small incision of about 3 cm was made anterosuperiorly centering over the fracture site. Cautery dissection was carried out to minimise bleeding from the subcutaneous plane onwards. Every care was taken not to disturb acromioclavicular ligaments. The fracture site was visualised, and the haematoma was curetted and washed. An anteroposterior drill hole was made with 2-mm drill bit on either side of the fracture. With the help of a suture passer a 2-0 PROLENE (Johnson & Johnson) was passed in a figure-eight configuration. One end of the prolene suture was then tied in the middle of a no 5 Ethibond and was made to pass through the drill hole pulling the other end. This technique passed double strands of Ethibond suture to provide reasonable strength. The fracture was reduced with the help of a clamp and fixed with two 1.8-mm transacromial Kirshner wires and reduction was evaluated with an image intensifier. The Ethibond suture was tied in a figure-eight manner keeping the knot superiorly (Fig. 1a–c). The tip of the Kirshner wire was bent and buried inside the skin. The wound was irrigated and closed in layers. Postoperatively, the arm was supported in an arm pouch for six weeks. Pendulum exercises were commenced from the third postoperative day. Passive flexion and extension was started from the seventh day. However, supported gradual abduction was started after suture removal on the 14th postoperative day. Routine retrieval of the Kirshner wire was done on the sixth postoperative week at the out-patient department (OPD) under local anaesthesia, after which active shoulder movement was allowed. Clinico-radiological follow-up was done in the sixth postoperative week and at a monthly interval until union, and six-monthly evaluation was done after established union. We confirmed union with two plane radiographs, anteroposterior and axillary view of shoulder. Cortical continuity in three cortices, medullary cavity reconstitution, no increase in fracture line gap in consecutive radiographs, and a nontender fracture site clinically were considered evidence of union at fracture site (Figs. 2a–c, 3a–e).
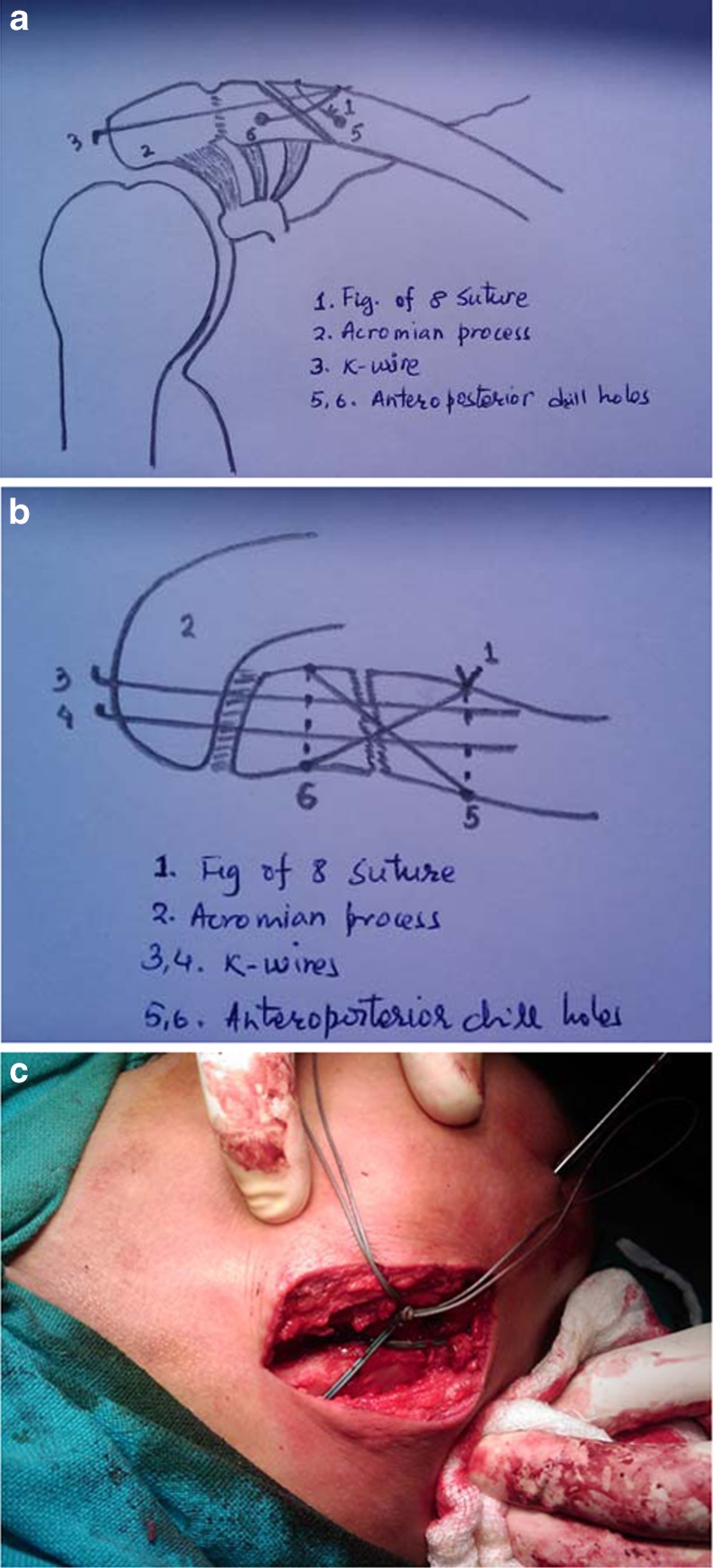
Fig. 1.
a Line diagram of shoulder anteroposterior view showing figure-eight suture and Kirshner wires. b Line diagram of shoulder top view showing figure-eight suture and two Kirshner wires. c Clinical photograph showing figure-eight suture with double strands of Ethibond
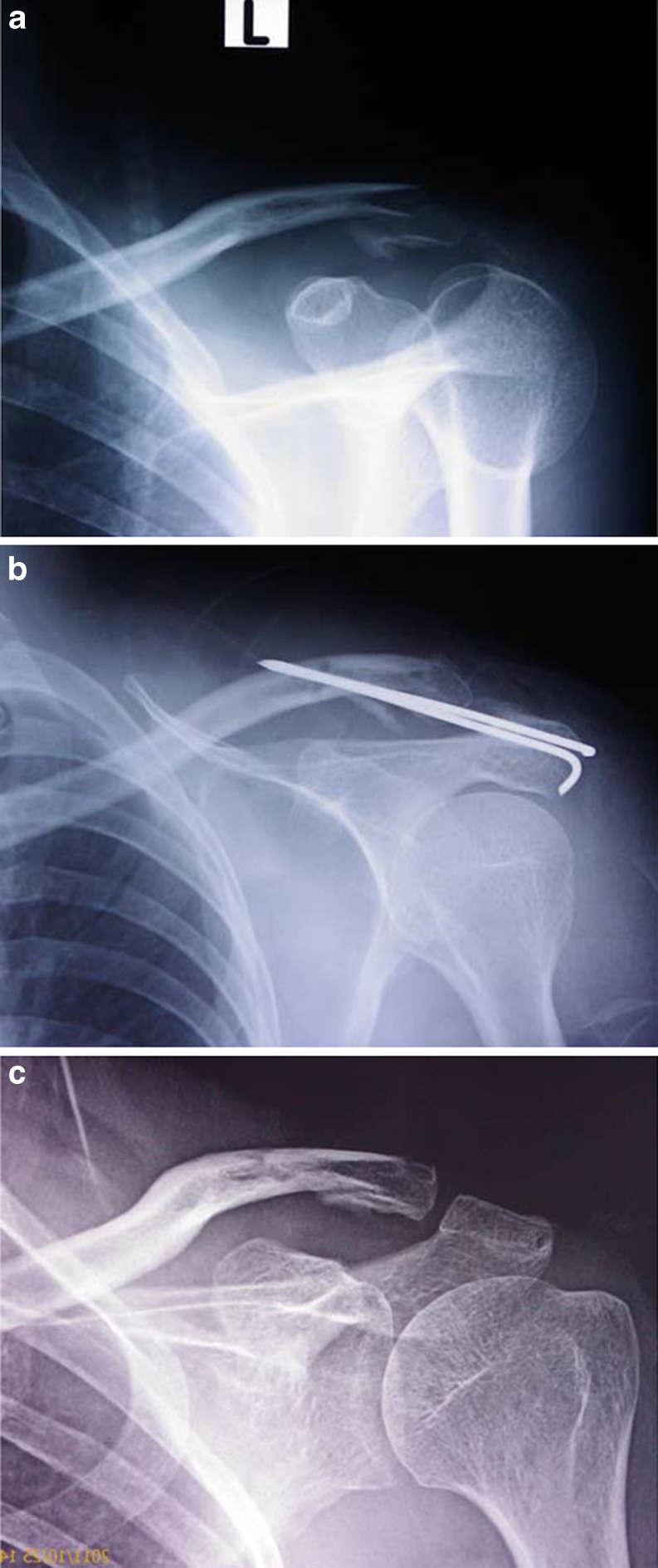
Fig. 2.
a X-ray anteroposterior view (left shoulder) showing displaced type 2 lateral end clavicle fracture. b Immediate post operative X-ray showing reduced fracture with transacromial Kirshner wire. The drill hole for figure-eight suture is well marked in both the fragments. c Well reduced and united fracture lateral end clavicle after Kirshner wire removal at six-months follow-up
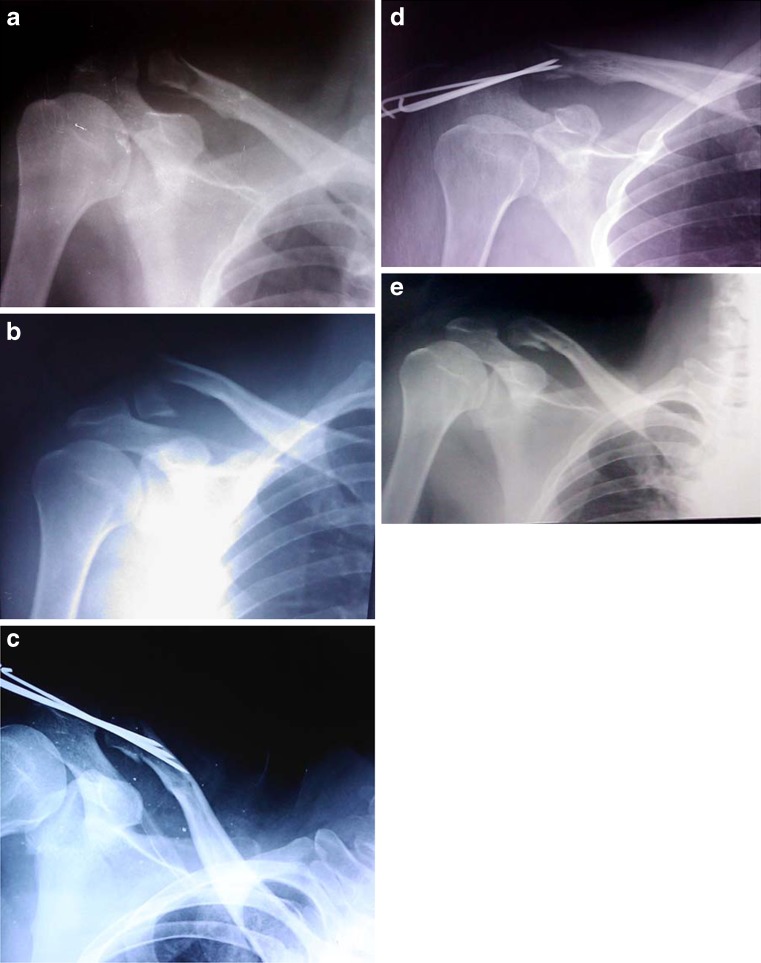
Fig. 3.
a X-ray anteroposterior view of right shoulder showing undisplaced type 2 lateral end clavicle fracture. Non-operative treatment was adopted initially. b Fracture displaced after two weeks of conservative treatment. c Immediate post operative X-ray showing reduced fracture. Tip of distal Kirshner wire was close to fracture site. Additional Kirshner wire was used to get secure cortical purchase. d All three Kirshner wires backed out at six weeks. Fracture is not yet united but the figure-eight suture still maintains the reduction. e Well reduced and united fracture at six-months follow-up
Results
Clinico-radiological outcomes are summarised in Table 1. All 16 fractures united clinically and radiologicaly. The mean average age of patients was 36.25 years with a SD of 11.35. The mean average time of union was 10.75 weeks with a SD of 3.92. All of them regained near normal range of motion, and the mean average constant score at the end of one year was 98.37 with a SD of 2.87. At the end of one year all patients had reached their pre-injury performance level. Range of movements at one year remained the same in those who were followed-up in successive years. There was no loss of fixation after removal of Kirshner wires at six weeks. In one of our cases, Kirshner wires backed out before six weeks but the reduction was maintained with the figure-eight suture. Wound related complications or infections were not reported in our series. However, skin impingement with bent Kirshner wires was noted in four cases. Return to sporting activities was only allowed after clinico-radiological union.
Table 1.
Clinico-radiological outcomes
| Patient number | Age (years) | Sex | Union time (weeks) | Follow-up (months) | ROM Fl/Abd/IR/ER | Pain | Strength (lbs) | Constant score | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 28 | M | 6 | 35 | 180/180/90/90 | None | 25 | 100 | * |
| 2 | 47 | M | 10 | 32 | 180/180/90/90 | None | 23 | 98 | |
| 3 | 31 | M | 6 | 31 | 180/180/90/90 | None | 25 | 100 | |
| 4 | 26 | M | 10 | 31 | 180/180/90/90 | None | 25 | 100 | |
| 5 | 29 | M | 10 | 28 | 180/180/90/90 | None | 25 | 100 | |
| 6 | 51 | F | 14 | 27 | 170/160/80/80 | None | 22 | 98 | * |
| 7 | 42 | M | 14 | 25 | 180/180/90/90 | None | 23 | 98 | |
| 8 | 46 | M | 10 | 20 | 180/180/90/90 | None | 25 | 100 | |
| 9 | 18 | M | 6 | 20 | 180/180/90/90 | None | 25 | 100 | |
| 10 | 36 | M | 10 | 20 | 180/180/90/90 | None | 23 | 98 | * |
| 11 | 52 | M | 18 | 17 | 170/160/90/85 | None | 14 | 89 | ** |
| 12 | 33 | M | 6 | 16 | 180/180/90/90 | None | 25 | 100 | |
| 13 | 26 | F | 10 | 15 | 180/180/90/90 | None | 25 | 100 | |
| 14 | 56 | F | 14 | 13 | 180/180/90/90 | None | 21 | 95 | |
| 15 | 25 | M | 10 | 13 | 180/180/90/90 | None | 24 | 98 | |
| 16 | 34 | M | 18 | 12 | 180/180/90/90 | None | 25 | 100 | * |
*Skin impingement with bent Kirshner wire
**Kirshner wire backed out before six weeks
Discussion
Fracture of the distal clavicle is less frequent than the more common middle third fractures. Type 2 fracture of distal clavicle has a high rate of delayed and nonunion [1, 2]. The rotational movement that occurs at the acromioclavicular joint is transferred to the fracture site, making the lateral end mobile, resulting in nonunion. Consequently, various surgical modalities have been advocated with various techniques of fixation with better outcomes [7–18]. Gaining control over such rotational movement with some sort of semi rigid to rigid fixation would prevent nonunion. Coracoclavicular reconstruction is generally not required as the ligaments are intact and attached to the distal clavicle. Anatomical alignment and prevention of rotation will suffice for such fractures to unite.
Rigid internal fixation between clavicle and coracoid or clavicle and acromian will fail, as it interferes with the normal rotational movement of the clavicle with relation to the coracoid and acromion. Furthermore, if the fracture unites with such procedures, implant removal must be before full mobilisation is started [7, 20, 22]. These fixations demand a second operation and extensive exposures for implant removal. The same is true with coracoclavicular reconstruction, which requires extensive exposure with soft tissue damage and risk of neurovascular injury.
Our method is a minimally invasive modified tension band fixation where tensile force is converted into compressive force with the help of non-absorbable sutures after anatomical reduction with transacromial Kirshner wires. We routinely remove Kirshner wires before full active mobilisation of the shoulder that eliminates the complication of a semi rigid type of fixation and fracture reduction is maintained by the non-absorbable suture. The fracture becomes sticky by the end of six weeks, and due to its intramembranous nature of ossification, union takes place if a conducive environment is provided. Radiological union appears to be delayed if single plane radiograph is considered. But two plane radiographs along with clinical evaluation gives fair estimation of union. Though the fracture line is visible in a few cases in the anteroposterior radiograph, the cortical continuity is seen in axillary views. Furthermore, a reconstituted medullary cavity, non-progressive fracture line gap and nontender fracture site give information about fracture union. We suggest CT scan in doubtful cases but routine use of CT scan to note union is not recommended. With our method, minimal dissection is required to reduce and pass non-absorbable sutures in a figure-eight manner. Transacromial Kirshner wires are passed under an image intensifier guidance to hold the fracture in an anatomical position. Removal of Kirshner wires is done under local anaesthesia in an out-patient procedure room. We keep the limb supported in an arm pouch for six weeks to make the patient aware that their shoulder needs protection and, secondly, so that the stress exerted by the hanging limb is guarded. Both these facts minimise undue stress at the healing bone. Results of our method of fixation are encouraging with this small cohort of 16 patients and comparable with other studies.
Neer reported 100% union with Kirshner wire fixation and suggested displaced fracture should be stabilised for better results [1]. Kona et al. reported 52.6% success rate with Kirshner wires [13]. Eskola et al. reported 95.6% success rate with two Kirshner wires [5]. Loosening of Kirshner wires, migration, undue stress during active mobilisation, back out, and breakage are known complications with Kirshner wires fixation. We addressed a few of such complications by removing Kirshner wires before active mobilisation. Even after removal of Kirshner wires, reduction is maintained by figure–eight suture.
Edward et al. [23], Yamaguchi et al. [9], and Ballmer et al. [7] reported 100% success rate in their series with Bosworth coracoclavicular fixation. Screw cut-out and peri-implant fracture are possible complications of Bosworth screw fixation. The implant removal demands deep tissue dissection and anaesthesia.
Coracoclavicular reconstruction using a dacron graft has yielded 100% success rate in a series by Goldberg et al. [24]. However, the nature of surgical dissection is more traumatic than other minimally invasive techniques. Stabilisation with a clavicular hook plate has yielded a success rate of up to 88% and 12% nonunion in a series of 18 patients by Tambe et al. [25]. Acromion osteolysis has been reported in 30% with such hook plates. Acromion osteolysis has also been reported by Nadarajah et al. [22] with the hook plate. However, Lee at al. [26] described the advantageous role of hook plate fixation in their comparative study between hook plate and tension band. Andersen et al. [27] reported 94% union rate with precountered superior locking plate fixation for displaced distal clavicle fractures. Peri-implant fracture has been reported in one case and infected nonunion in the other in their study. However, they required additional surgical techniques for anatomical reduction in the form of suture augmentaion with coracoid, anchor suture fixation or coracoclavicular screws in half of their cases resulting in wider surgical exposures.
Levy [20] described single figure-eight suture fixation with PDS suture with a success rate of 100%. Though alignment is secured, rotational stress during mobilisation may weaken suture fixation. Their technique has been modified by Badhe et al. [21], that consists of two figure-eight sutures with non absorbable polyester. However, the distal fragment is often too small to make two drill holes.
Our method of fixation allows stable fixation with Kirshner wires and figure-eight suturing using non-absorbable suture material, which jointly provides compression at the fracture site. Early removal of Kirshner wires allows active mobilisation without the fear of implant related complications at the cost of maintained reduction with non-absorbable suture after six weeks. Although the results of our small cohort of 16 patients are encouraging, we need to further observe a larger number of patients. More prospective studies with a larger population will definitely establish its role in type 2 displaced clavicle fractures.
Acknowledgments
Conflict of interest
No conflict of interest exists.
References
- 1.Neer CS. Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 2.Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am. 2004;86-A(4):778–782. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Neviaser JS. The treatment of fractures of the clavicle. Surg Clin North Am. 1963;43:1555–1563. doi: 10.1016/s0039-6109(16)37144-4. [DOI] [PubMed] [Google Scholar]
- 4.Zenni EJ, Jr, Krieg JK, Rosen MJ. Open reduction and internal fixation of clavicular fractures. J Bone Joint Surg Am. 1981;63(1):147–151. [PubMed] [Google Scholar]
- 5.Eskola A, Vainionpaa S, Patiala H, Rokkanen P. Outcome of operative treatment in fresh lateral clavicular fracture. Ann Chir Gynaecol. 1987;76(3):167–169. [PubMed] [Google Scholar]
- 6.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86:1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br. 1991;73:291–294. doi: 10.1302/0301-620X.73B2.2005158. [DOI] [PubMed] [Google Scholar]
- 8.Macheras G, Kateros KT, Savvidou OD, Sofianos J, Fawzy EA, Papagelopoulos PJ. Coracoclavicular screw fixation for unstable distal clavicle fractures. Orthopedics. 2005;28:693–696. doi: 10.3928/0147-7447-20050701-18. [DOI] [PubMed] [Google Scholar]
- 9.Yamaguchi H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop. 1998;22:366–368. doi: 10.1007/s002640050279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bezer M, Aydin N, Guven O. The treatment of distal clavicle fractures with coracoclavicular ligament disruption: a report of 10 cases. J Orthop Trauma. 2005;19:524–528. doi: 10.1097/01.bot.0000164593.04348.e5. [DOI] [PubMed] [Google Scholar]
- 11.Chen CH, Chen WJ, Shih CH. Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma. 2002;52:72–78. doi: 10.1097/00005373-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Shin SJ, Roh KJ, Kim JO, Sohn HS. Treatment of unstable distal clavicle fractures using two suture anchors and suture tension bands. Injury. 2009;40:1308–1312. doi: 10.1016/j.injury.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 13.Kona J, Bosse MJ, Staeheli JW, Rosseau RL. Type II distal clavicle fractures: a retrospective review of surgical treatment. J Orthop Trauma. 1990;4(2):115–120. doi: 10.1097/00005131-199004020-00002. [DOI] [PubMed] [Google Scholar]
- 14.Haidar SG, Krishnan KM, Deshmukh SC. Hook plate fixation for type II fractures of the lateral end of the clavicle. J Shoulder Elbow Surg. 2006;15:419–423. doi: 10.1016/j.jse.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Klein SM, Badman BL, Keating CJ, Devinney DS, Frankle MA, Mighell MA. Results of surgical treatment for unstable distal clavicular fractures. J Shoulder Elbow Surg. 2010;19:1049–1055. doi: 10.1016/j.jse.2009.11.056. [DOI] [PubMed] [Google Scholar]
- 16.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40:236–239. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 17.Kaipel M, Majewski M, Regazzoni P. Double-plate fixation in lateral clavicle fractures—a new strategy. J Trauma. 2010;69:896–900. doi: 10.1097/TA.0b013e3181bedf28. [DOI] [PubMed] [Google Scholar]
- 18.Yu C, Sun YH, Zhao CQ, Shi DW, Wang Y. Treatment of distal clavicle fracture with distal radius volar locking compression plate. Chin J Traumatol. 2009;12:299–301. [PubMed] [Google Scholar]
- 19.Brouwer KM, Wright TC, Ring DC. Failure of superior locking clavicle plate by axial pull-out of the lateral screws: a report of four cases. J Shoulder Elbow Surg. 2009;18:e22–e25. doi: 10.1016/j.jse.2008.05.042. [DOI] [PubMed] [Google Scholar]
- 20.Levy O. Simple, minimally invasive surgical technique for treatment of type 2 fractures of the distal clavicle. J Shoulder Elbow Surg. 2003;12:24–28. doi: 10.1067/mse.2003.128564. [DOI] [PubMed] [Google Scholar]
- 21.Badhe SP, Lawrence TM, Clark DI. Tension band suturing for the treatment of displaced type 2 lateral end clavicle fractures. Arch Orthop Trauma Surg. 2007;127(1):25–28. doi: 10.1007/s00402-006-0197-3. [DOI] [PubMed] [Google Scholar]
- 22.Nadarajah R, Mahaluxmivala J, Amin A, Goodier DW. Clavicular hook-plate: complications of retaining the implant. Injury. 2005;36(5):681–683. doi: 10.1016/j.injury.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: a case for fixation. Injury. 1992;23(1):44–46. doi: 10.1016/0020-1383(92)90125-C. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR. Type II fractures of the distal clavicle: a new surgical technique. J Shoulder Elbow Surg. 1997;6:380–382. doi: 10.1016/S1058-2746(97)90006-9. [DOI] [PubMed] [Google Scholar]
- 25.Tambe AD, Motkar P, Qamar A, Drew S, Turner SM. Fracture of distal third of the clavicle treated by hook plate. Int Orthop. 2006;30(1):7–10. doi: 10.1007/s00264-005-0019-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee YS, Lau MJ, Tseng YC, Chen WC, Kao HY, Wei JD. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33(5):1401–1405. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andersen JR, Willis MP, Nelson R, Mighell MA. Precontoured superior locked plating of distal clavicle fractures: a new strategy. Clin Orthop Relat Res. 2011;469(12):3344–3350. doi: 10.1007/s11999-011-2009-5. [DOI] [PMC free article] [PubMed] [Google Scholar]