Abstract
Purpose
Short-stem hip arthroplasty preserves femoral bone stock which includes the femoral neck. This implies that the stem has to follow the anatomy of the femoral neck. Therefore, it has been questioned whether biomechanical reconstruction of the hip can be safely achieved with SHA.
Methods
Biomechanical reconstruction of the hip was analysed for 50 modular short-stem hip arthroplasties (SHA) and compared to 50 conventional total hip arthroplasties (THA). Biomechanical parameters were analysed on pre- and postoperative pelvic overviews and compared to those of the contralateral side.
Results
The position of the acetabular cup (vertical and horizontal hip centre of rotation) changed slightly and was comparable for both groups. Horizontal femoral offset increased more in SHA (6.2 mm) than in THA (2.0 mm). Compared to the contralateral side it was significantly greater after SHA (+3.6 mm) but almost balanced after THA (−0.2 mm). Limb length increased with both procedures (8.0 mm SHA, 9.1 mm THA), but showed a significantly greater discrepancy after SHA (3.3 mm) as compared to THA (1.3 mm). According to the different implant designs, the stem-shaft axis showed a wider varus-valgus range for SHA (6.2° varus to 8.8° valgus) than for THA (2.6° varus to 3.3° valgus).
Conclusion
Horizontal femoral offset increased more with modular SHA than with conventional THA, but was within a beneficial range. Restoration of limb length appears more difficult in SHA and has a tendency to prolong limb length, which is probably related to the higher femoral resection level. This should be taken into consideration when considering SHA for a patient as well as during implantation.
Introduction
Biomechanical reconstruction of the hip has a significant impact on the clinical outcome and survival of implants in hip replacement arthroplasty [1–7]. In order to achieve a proper restoration of the joint, it is essential for the surgeon to understand the key characteristics of an implant design.
Good clinical results have been reported for short-stem hip arthroplasty (SHA) [8–11], which was introduced several years ago, but only now is being performed in increasing numbers. However, little is known about the ability of SHA to reconstruct the limb length and the biomechanics of the hip [12]. This appears even more relevant for SHA, as several designs require a resection level under the femoral head to preserve the femoral neck, which is needed for a firm anchorage. This entails that the implant has to follow the given angle and torsion of the femoral neck [11]. Furthermore, the position of the implant is also partly determined by the height of the femoral resection level. As a consequence, it has been speculated that restoration of the limb length might be limited in SHA [13].
Therefore, the present study was designed to evaluate whether biomechanical restoration of the hip can reliably be achieved with SHA.
Material and methods
Patients and surgery
Fifty consecutive short-stem hip arthroplasties (SHA) with a modular implant design, which had a pre- and post-operative pelvic overview were analysed retrospectively. Surgery was performed from May 2006 to November 2008 at the orthopaedic department. All surgery was performed by three experienced senior surgeons (AF, FM, VJ) through a minimally invasive antero-lateral Hardinge approach in the supine position. For comparison, 50 consecutive total hip arthroplasties (THA), which were implanted during the same period of time, with one implant type and a pre- and post-operative pelvic overview, were analysed. The THA collective patients were operated via the same antero-lateral approach and by the same surgeons (AF, FM, VJ), or under their supervision.
Inclusion criteria for patients of both treatment groups were primary hip arthroplasty, and at least one pre- and one post-operative pelvic overview. Exclusion criteria were severe dysplasia (Crowe III-IV), joint infection, malignancy of the femur/pelvis, or a traumatic event. All implants were carefully templated pre-operatively and intra-operatively evaluated with fluoroscopy in two planes. The study was approved by the Ethics Committee of the University.
Implants
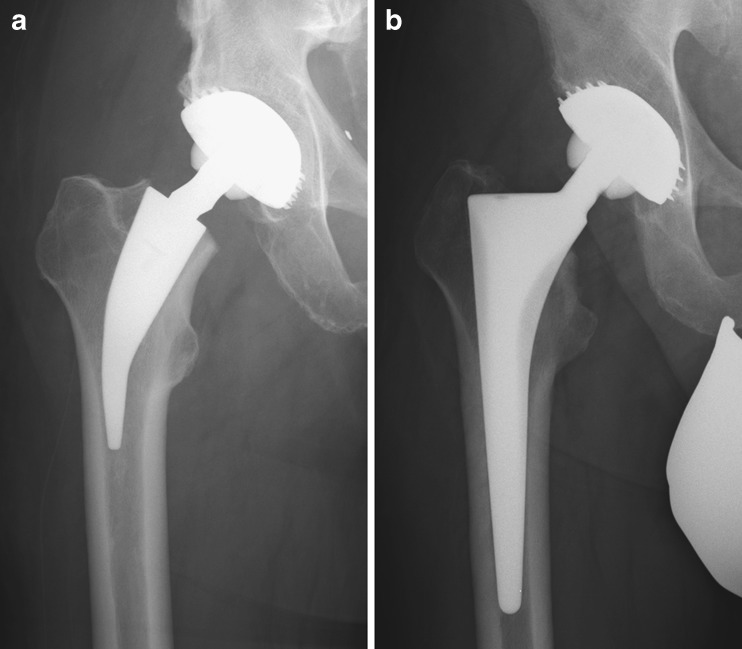
All patients with SHA received the same short-stem hip implant (Metha, BBraun Aesculap, Tuttlingen, Germany) in the modular version (Fig. 1a). The implant is available as a monoblock (CCD-angle 130°, 135°) or as a modular variant with cone adapters (CCD-angle 130°, 135° and 140°, all with 7.5° antetorsion, retrotorsion or neutral), with an implant size ranging from 0 to 7.
Fig. 1.
a Radiograph showing the SHA implant. b The THA implant
All patients with THA received the same conventional hip implant, which has a monoblock design with a CCD-angle of 140° (CR-stem, Implantcast, Buxtehude, Germany). The implant sizes range from 0 to 7 (Fig. 1b). In both groups, either a threaded or a press fit cup (Screwring or Plasmacup SC, BBraun Aesculap, Tuttlingen, Germany) was used. All patients received a ceramic femoral head (BBraun Aesculap, Tuttlingen, Germany), which is available in small, medium, large and extra-large sizes with 4-mm increments respectively.
Radiological evaluation
Biomechanical parameters were determined from a pre- and a postoperative pelvic overview. The radiographs were centred on the pubis with the patient in the supine position, the legs stretched and parallel, with 10–15° of internal rotation. All radiographs were acquired with the same digital X-ray apparatus and analysed with the digital planning software Endomap (both Siemens, Medical Solutions, Erlangen, Germany). The best reproduced pre- and postoperative radiograph was selected for each patient.
All measurements were performed by one of the authors (MB), in a blinded fashion and random order. The postoperative pelvic overviews were calibrated for size using the femoral head (size obtained from the operative notes). The pre-operative pelvic overview was calibrated using the distance between the teardrop lines, or the lowest points of the sacroiliac joints (length determined beforehand from the calibrated postoperative pelvic overview). Size consistency was validated by comparing the diameter of the contralateral femoral head, using the pre- and postoperative radiographs.
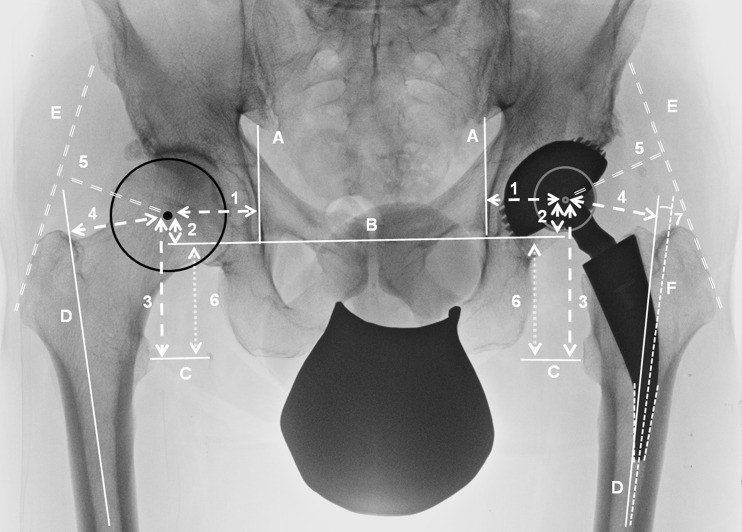
The following parameters were determined pre- and postoperatively for the arthroplasty side, as well as for the native contralateral side (only radiographs with unilateral hip arthroplasty), as previously described (Fig. 2) [14, 15]:
Vertical and horizontal femoral offset
Vertical and horizontal hip centre of rotation
Leg length
Abductor lever arm
Stem-shaft axis
Fig. 2.
Biomechanical parameters determined in pre- and postoperative radiographs after SHA and THA: 1 horizontal hip centre of rotation, 2 vertical hip centre of rotation, 3 vertical femoral offset, 4 horizontal femoral offset, 5 abductor lever arm, 6 limb length, 7 stem-shaft angle, A vertical teardrop line, B horizontal tear drop line, C midline lesser trochanter, D femoral shaft axis, Etangential line to the greater trochanter, F stem axis
Statistical analysis
Statistical analysis was performed using SigmaStat (Systat Software GmbH, Erkrath, Germany). Differences within each group (pre- and postoperative side, operated and contralateral side) were evaluated using a paired t-test. Comparison between THA and SHA was evaluated using an unpaired t-test. A p-value <0.05 determined significance.
Results
Patients and demographics
The SHA study collective was comprised of 50 implants (45 patients): 23 men and 22 women, with a mean age of 54 ± 12 years (20–71 years). Reasons for hip replacement were osteoarthritis in 40% (n = 20), avascular necrosis in 28% (n = 14), acetabular dysplasia in 28% (n = 14) and rheumatoid arthritis in 4% (n = 2) of the patients.
The THA study collective comprised of 50 implants (42 patients): 19 men and 23 women, with a mean age of 60 ± eight years (range 39–72 years). Reasons for hip replacement were osteoarthritis in 70% (n = 35), acetabular dysplasia in 22% (n = 11) and avascular necrosis in 8% (n = 4) of the patients.
Implants
For SHA, implants with a CCD-angle of 130° were used in 46% (n = 23), 135° in 54% (n = 27) and 140° in 0% (n = 0) of the cases. The mean cup size was 50.6 ± 3.4 mm (range 44–56 mm) with a head diameter of 28 mm in 10% (n = 5), 32 mm in 82% (n = 41), and 36 mm in 8% (n = 4) of the patients. Head length was short in 36% (n = 18), medium in 40% (n = 20) and large in 24% (n = 12) of the patients.
For THA, all 50 implants had a CCD-angle of 140°. The mean cup size was 51.0 ± 3.8 mm (range 44–64 mm) with a head diameter of 28 mm in 12% (n = 6), and 32 mm in 88% (n = 44) of the patients. Head length was short in 22% (n = 11), medium in 76% (n = 38), and large in 2% (n = 1) of the patients.
Radiological evaluation
Consistency of the pre- and postoperative radiographs
Comparing the diameter of the contralateral femoral head size, using the pre- and postoperative radiographs, revealed an excellent degree of consistency, with an average diameter of 46.3 ± 3.8 mm and 45.9 ± 3.8 mm (maximum error of 6.4%), respectively.
Horizontal femoral offset
After SHA, the mean horizontal femoral offset had significantly increased by 6.2 mm (p = 0.001), with 78% (39/50) of the cases showing an increase. Compared to the contralateral side, the horizontal femoral offset was significantly larger by 3.6 mm (p = 0.001). After THA, the mean horizontal femoral offset had increased significantly by 2.0 mm (p = 0.03), with 54% (27/50) of the cases showing an increase. Compared to the contralateral side, the horizontal femoral offset was, with −0.2 mm, almost equal and not significantly different (p = 0.87). The increase (p = 0.001) in the horizontal femoral offset, as well as the postoperative difference (p = 0.007), were significantly different between SHA and THA (Tables 1, 2 and 3).
Table 1.
Pre-operative radiological data on patients of both study groups. Data presented as mean (SD, range)
| Parameter | SHA (n = 50) | THA (n = 50) | p valuea |
|---|---|---|---|
| Horizontal femoral offset | 35.1 (±7.9, 18–53) | 37.9 (±6.6, 21–52) | 0.07 |
| Vertical femoral offset | 54.8 (±9.1, 33–71) | 55.2 (±7.4, 43–71) | 0.76 |
| Horizontal hip centre of rotation | 37.8 (±5.2, 24–47) | 34.2 (±5.7, 20–45) | 0.002 |
| Vertical hip centre of rotation | 16.7 (±4.1, 7–27) | 16.4 (±3.9, 9–29) | 0.73 |
| Abductor lever arm | 49.5 (±6.7, 36–65) | 47.8 (±6.0, 32–60) | 0.18 |
| Leg length | 38.0 (±10.5, (13–58) | 39.2 (±9.1, 21–58) | 0.53 |
SD standard deviation, SHA short-stem hip arthroplasty, THA total hip arthroplasty
a p value: SHA vs. THA
Table 2.
Biomechanical changes of the pre-operative hip compared to those of the post-operative hip. Data presented as mean (SD, range)
| Parameter | SHA (n = 50) | THA (n = 50) | p valuea |
|---|---|---|---|
| Horizontal femoral offset | +6.2 (±6.5, −6 to 24) | +2.0 (±6.1, -11 to 21) | 0.001 |
| Vertical femoral offset | +8.1 (±5.2, -1 to 26) | +8.8 (±5.9, -4 to 20) | 0.53 |
| Horizontal hip centre of rotation | −5.2 (±4.6, -16 to 6) | −3.5 (±4.9, -18 to 8) | 0.22 |
| Vertical hip centre of rotation | +0.2 (±3.3, -11 to 6) | −0.6 (±2.9, -8 to 7) | 0.10 |
| Abductor lever arm | −1.1 (±5.1, -11 to 9) | −0.4 (±6.7, -14 to 20) | 0.58 |
| Leg length | +8.0 (±6.2, -3 to 23) | +9.1 (±5.8, -4 to 20) | 0.34 |
SD standard deviation, SHA short-stem hip arthroplasty, THA total hip arthroplasty
a p value: SHA vs. THA
Table 3.
Biomechanical parameters on the operated hip compared to the native contralateral hip (unilateral hip arthroplasty). Data presented as mean (SD, range)
| Parameter | SHA (n = 45) | THA (n = 42) | p valuea |
|---|---|---|---|
| Horizontal femoral offset | +3.6 (±6.4, −8 to 18) | −0.2 (±6.4; −12 to 15) | 0.007 |
| Vertical femoral offset | +6.2 (±4.9, −3 to 17) | +4.6 (±5.2; −5 to 17) | 0.14 |
| Horizontal hip centre of rotation | −2.2 (±3.9, −12 to 5) | −1.1 (±3.0; −8 to 5) | 0.15 |
| Vertical hip centre of rotation | +2.4 (±4.5, −15 to 12) | +2.3 (±3.9; −6 to 10) | 0.92 |
| Abductor lever arm | −1.4 (±5.9, −14 to 15) | −1.9 (±5.5; −13 to 11) | 0.69 |
| Leg length | +3.3 (±5.3, −10 to 14) | +1.3 (±3.4; −7 to 9) | 0.03 |
SD standard deviation, SHA short-stem hip arthroplasty, THA total hip arthroplasty
a p value: SHA vs. THA
Vertical femoral offset
After SHA, the mean vertical femoral offset had significantly increased by 8.1 mm (p = 0.001), with 96% (48/50) of the cases showing an increase. Compared to the contralateral side, the vertical femoral offset was significantly larger by 6.2 mm (p = 0.001). After THA, the vertical femoral offset had significantly increased by 8.8 mm (p = 0.001), with 92% (46/50) of the cases showing an increase. Compared to the contralateral side, the vertical femoral offset was significantly larger by 4.6 mm (p = 0.001). The increase (p = 0.53) in the vertical femoral offset, as well as the postoperative difference (p = 0.14), were not significantly different between SHA and THA (Tables 1, 2 and 3).
Horizontal hip centre of rotation
After SHA, the mean horizontal hip centre of rotation was significantly medialized by 5.2 mm (p = 0.001), and was more medial in 88% (44/50) of the cases. Compared to the contralateral side, the horizontal hip centre of rotation was significantly more medial by 2.2 mm (p = 0.001). After THA, the horizontal hip centre of rotation was postoperatively medialized by 3.5 mm (p = 0.001), and was more medial in 72% (36/50) of the cases. Compared to the contralateral side, the horizontal hip centre of rotation was significantly more medial by 1.1 mm (p = 0.02). The increase (p = 0.21) in the horizontal femoral offset, as well as the postoperative difference (p = 0.92), were not significantly different between SHA and THA.
Vertical hip centre of rotation
After SHA, the vertical hip centre of rotation did not change significantly. The mean position was 0.2 mm more proximal (p = 0.71), with 48% (24/50) of the cases being more proximal. Compared to the contralateral side, the mean vertical hip centre of rotation was significantly more proximal by 2.4 mm (p = 0.001). After THA, the vertical hip centre of rotation did not change significantly. The mean position was 0.6 mm more distal (p = 0.14), with 46% (26/50) of the cases being more distal. Compared to the contralateral side, the mean vertical hip centre of rotation was significantly more proximal by 2.3 mm (p = 0.001). The changes (p = 0.100) in the vertical hip centre of rotation, as well as the postoperative differences (p = 0.15), were not significantly different between SHA and THA.
Abductor lever arm
After SHA, the mean abductor lever arm did not change significantly. It decreased by 1.1 mm (p = 0.15), with 56% (28/50) of the cases showing a decrease. Compared to the contralateral side, the abductor lever arm was shorter by 1.4 mm, which was not significant (p = 0.11). After THA, the mean abductor lever arm did not change significantly. It decreased by 0.4 mm (p = 0.67), with 44% (22/50) of the cases showing a decrease. Compared to the contralateral side, the abductor lever arm was significantly shorter by 1.9 mm, which was significant (p = 0.03). The changes (p = 0.58), as well as the postoperative differences (p = 0.69) in the abductor lever arm, were not significantly different between SHA and THA.
Leg length
After SHA, the leg length increased significantly by 8.0 mm (p = 0.001), with 92% (46/50) of the cases showing an increase. Compared to the contralateral side, the leg length was significantly longer by 3.3 mm (p = 0.001). After THA, the leg length increased significantly by 9.1 mm (p = 0.001), with 88% (44/50) of the cases showing an increase. Compared to the contralateral side, the leg length was significantly longer by 1.3 mm (p = 0.02) (Tables 1, 2 and 3). The increase in limb length was not significantly different (p = 0.34) between SHA and THA. In contrast, the postoperative limb difference was significantly different (p = 0.03).
Stem-shaft axis
The mean stem-shaft axis for SHA was 0.5° ± 3.5° of a varus position. Of the SHA stems, 58% (n = 29) were placed in a neutral position (±3°), 24% (n = 12) in a varus position (mean 5.1° ± 1.4°; max 8.8°) and 18% (n = 9) in a valgus position (mean 4.6° ± 0.9°; max 6.2°).
The mean stem-shaft axis for THA was 0.1° ± 1.2° of a varus position. Of the THA stems, 98% (n = 49) were placed in a neutral position (±3°), with one implant (2%) showing a varus position of 3.3°. The difference in the stem-shaft axis was not significantly different between SHA and THA (p = 0.32).
Discussion
Good results in hip arthroplasty not only depend on a firm anchorage, but also on a precise biomechanical reconstruction of the hip [2, 5, 6, 16–18]. Little is known about the ability to reconstruct the biomechanics of the hip for SHA [12], which is why this study compared the results of SHA to those of THA.
On the acetabular side, the vertical hip centre of rotation did not change significantly either after SHA or THA, with a more proximal position for both groups when compared to the contralateral side (2.4 mm SHA; 2.3 mm THA). Similarly, two studies have reported only slight changes in the vertical hip centre of rotation after THA, with a more proximal position of 1.4 mm and 3.3 mm compared to the contralateral side [14, 19]. And after SHA with the Proxima short-stem, a more proximal cup position of 1.4 mm has previously been reported [10].
The horizontal hip centre of rotation was significantly medialized in both groups and was more medial compared to the contralateral side (2.2 mm SHA, 1.1 mm THA). A more medial cup position has also been reported after SHA (0.9 mm) [10] and THA (1.0 mm–3.1 mm) [14, 19, 20]. This is considered beneficial, as it affects the abductor lever arm positively and also leads to lower joint reaction forces [2, 18]. Overall, the position of the acetabular component was similar in both treatment groups, which enabled us to make a direct comparison of the femoral reconstruction.
On the femoral side, the horizontal femoral offset increased for both treatment groups, but with a clearly greater increase in SHA. Compared to the contralateral side, it was significantly greater in the SHA group (3.6 mm), but was almost balanced in the THA group (−0.2 mm). A study of the MiniHip short-stem also reported an increase of 2.8 mm in the horizontal femoral offset, however, without comparing the data to the contralateral side [12]. For the Proxima short-stem, Kim et al. reported postoperatively a smaller horizontal femoral offset of −0.6 mm compared to the contralateral side [10]. Although different study collectives and surgeons probably contributed to the varying results, the differences can also be attributed to the different short-stem implants with different shapes, shaft-neck angles and modular or non-modular designs. Furthermore, the varus or valgus position of most SHA implants is more variable than for THA implants [12, 21], which also influences the horizontal femoral offset [21].
For THA, a wide range in postoperative horizontal femoral offset has also been reported, with most studies describing a postoperative increase [7, 14, 19–21]. Compared to the contralateral side, a balanced or even moderately increased horizontal femoral offset is often striven for, as this seems to offer a favourable outcome in terms of a better range of motion [3, 22], an increased stability with a reduced risk of dislocation, and less wear [3, 5, 6, 16, 18]. However, less wear only seems to apply if the horizontal femoral offset is not increased by more than 5 mm compared to the native femoral offset [6]. And, one study even reported a higher failure rate for stems using a very high offset version [23].
An increase in the horizontal femoral offset correlates positively with the strength of the abductor muscles [1–3, 7], which can be estimated from radiographs by measuring the abductor lever arm [7]. Although the femoral offset increased for both treatment groups, the abductor lever arm decreased slightly in the THA (−0.4 mm) and in the SHA (−1.1 mm) groups. This contradictory finding can be explained by the increased limb length in both collectives, which results in a reduced measurement of the abductor lever arm.
Restoration of the limb length is an important goal in hip arthroplasty. In both groups the limb length was pre-operatively shorter on the side of arthroplasty, but increased thereafter. However, compared to the contralateral side, the postoperative limb length discrepancy was more pronounced in SHA (3.3 mm) than in THA (1.3 mm). Similarly, for the same SHA implant (Metha), Confalonieri et al. and Lavzoic et al. reported on a postoperative limb difference of about +4 mm to +8 mm, despite using navigation in many of the procedures [13, 24]. This tendency to increase limb length in SHA is very likely related to the higher resection level at the femoral neck. The Proxima short-stem, which requires a lower resection level compared to the Metha stem, has also reported a postoperative limb difference of +3.1 mm [10]. The difference of +3.3 mm in our SHA group is significantly more than that of our THA group (+1.3 mm) and also greater than that of most other THA studies (−1.1 mm to +2.6 mm) [7, 14, 19, 20]. Altogether, these results suggest that neck-preserving SHA has a tendency to prolong limb length, which should be taken into consideration when selecting an implant for a patient, as well as during implantation.
The stem-shaft axis showed a wider range of varus-valgus position in the SHA group than in the THA group. This has been similarly reported by Kamada et al. [21] for the Mayo short-stem and is related to the different anchorage philosophy of the double-tapered SHA stem compared to that of a conventional THA stem [11]. Although Kamada et al. reported a better abductor muscle strength for the varus than for the valgus position after SHA [21], the preferable position and the acceptable range are still not known and require further research [9].
This study has some limitations. First, modular necks are supposed to improve the biomechanical reconstruction of the hip [25, 26]. In this study, the modular SHA implant did not show better results as compared to the monoblock THA implant. However, we were not able to analyse the anteversion or retroversion of the stem from the plane radiographs. Also, we did not compare a modular versus a non-modular SHA design. Further studies are required to evaluate these issues. Second, patients were not randomized. This was due not only to the retrospective study design, but also to the different selection criteria for THA and SHA (especially age and bone quality). Third, analysis from plane radiographs can potentially include deviations. However, consistency between the pre- and post-operative radiographs was very good with a maximum error of 6.4%.
In summary, hip arthroplasty with a modular SHA implant increased the horizontal femoral offset more than a monoblock THA implant, but within a beneficial range. In contrast, restoration of the limb length seems to be more challenging with SHA, as it tends to prolong limb length, which is probably related to the higher resection level at the femoral neck.
Acknowledgement
The first author gratefully thanks Nora Goudsouzian for the careful proofreading of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Kiyama T, Naito M, Shinoda T, Maeyama A. Hip abductor strengths after total hip arthroplasty via the lateral and posterolateral approaches. J Arthroplasty. 2010;25(1):76–80. doi: 10.1016/j.arth.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Asayama I, Chamnongkich S, Simpson KJ, Kinsey TL, Mahoney OM. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20(4):414–420. doi: 10.1016/j.arth.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 3.McGrory BJ, Morrey BF, Cahalan TD, An KN, Cabanela ME. Effect of femoral offset on range of motion and abductor muscle strength after total hip arthroplasty. J Bone Joint Surg Br. 1995;77(6):865–869. [PubMed] [Google Scholar]
- 4.Erceg M. The influence of femoral head shift on hip biomechanics: additional parameters accounted. Int Orthop. 2009;33(1):95–100. doi: 10.1007/s00264-008-0544-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bourne RB, Rorabeck CH. Soft tissue balancing: the hip. J Arthroplasty. 2002;17(4 Suppl 1):17–22. doi: 10.1054/arth.2002.33263. [DOI] [PubMed] [Google Scholar]
- 6.Little NJ, Busch CA, Gallagher JA, Rorabeck CH, Bourne RB. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin Orthop Relat Res. 2009;467(11):2895–2900. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lecerf G, Fessy MH, Philippot R, Massin P, Giraud F, Flecher X, Girard J, Mertl P, Marchetti E, Stindel E. Femoral offset: anatomical concept, definition, assessment, implications for preoperative templating and hip arthroplasty. Orthop Traumatol Surg Res. 2009;95(3):210–219. doi: 10.1016/j.otsr.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Briem D, Schneider M, Bogner N, Botha N, Gebauer M, Gehrke T, Schwantes B. Mid-term results of 155 patients treated with a collum femoris preserving (CFP) short stem prosthesis. Int Orthop. 2011;35(5):655–660. doi: 10.1007/s00264-010-1020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lerch M, von der Har-Tran A, Windhagen H, Behrens BA, Wefstaedt P, Stukenborg-Colsman CM (2011) Bone remodelling around the Metha short stem in total hip arthroplasty: a prospective dual-energy X-ray absorptiometry study. Int Orthop. Sep 21 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 10.Kim YH, Kim JS, Park JW, Joo JH. Total hip replacement with a short metaphyseal-fitting anatomical cementless femoral component in patients aged 70 years or older. J Bone Joint Surg Br. 2011;93(5):587–592. doi: 10.1302/0301-620X.93B5.25994. [DOI] [PubMed] [Google Scholar]
- 11.Morrey BF, Adams RA, Kessler M. A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000;82(7):952–958. doi: 10.1302/0301-620X.82B7.10420. [DOI] [PubMed] [Google Scholar]
- 12.Jerosch J, Grasselli C, Kothny PC, Litzkow D, Hennecke T (2011) Reproduction of the anatomy (offset, CCD, leg length) with a modern short stem hip design—a radiological study. Z Orthop Unfall. Apr 12 [Epub ahead of print] [DOI] [PubMed]
- 13.Confalonieri N, Manzotti A, Montironi F, Pullen C (2008) Leg length discrepancy, dislocation rate, and offset in total hip replacement using a short modular stem: navigation vs conventional freehand. Orthopedics 31(10 Suppl 1) [PubMed]
- 14.Silva M, Lee KH, Heisel C, Rosa MA, Schmalzried TP. The biomechanical results of total hip resurfacing arthroplasty. J Bone Joint Surg Am. 2004;86-A(1):40–46. doi: 10.2106/00004623-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Traina F, De Fine M, Tassinari E, Sudanese A, Calderoni PP, Toni A (2011) Modular neck prostheses in DDH patients: 11-year results. J Orthop Sci 16(1):14–20 [DOI] [PubMed]
- 16.Sakalkale DP, Sharkey PF, Eng K, Hozack WJ, Rothman RH. Effect of femoral component offset on polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 2001;388:125–134. doi: 10.1097/00003086-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Yamaguchi T, Naito M, Asayama I, Ishiko T. Total hip arthroplasty: the relationship between posterolateral reconstruction, abductor muscle strength, and femoral offset. J Orthop Surg (Hong Kong) 2004;12(2):164–167. doi: 10.1177/230949900401200205. [DOI] [PubMed] [Google Scholar]
- 18.Bicanic G, Delimar D, Delimar M, Pecina M. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop. 2009;33(2):397–402. doi: 10.1007/s00264-008-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Girard J, Lavigne M, Vendittoli PA, Roy AG. Biomechanical reconstruction of the hip: a randomised study comparing total hip resurfacing and total hip arthroplasty. J Bone Joint Surg Br. 2006;88(6):721–726. doi: 10.1302/0301-620X.88B6.17447. [DOI] [PubMed] [Google Scholar]
- 20.Loughead JM, Chesney D, Holland JP, McCaskie AW. Comparison of offset in Birmingham hip resurfacing and hybrid total hip arthroplasty. J Bone Joint Surg Br. 2005;87(2):163–166. doi: 10.1302/0301-620X.87B2.15151. [DOI] [PubMed] [Google Scholar]
- 21.Kamada S, Naito M, Nakamura Y, Kiyama T (2011) Hip abductor muscle strength after total hip arthroplasty with short stems. Arch Orthop Trauma Surg 131(12):1723–1729 [DOI] [PubMed]
- 22.Massin P, Geais L, Astoin E, Simondi M, Lavaste F. The anatomic basis for the concept of lateralized femoral stems: a frontal plane radiographic study of the proximal femur. J Arthroplasty. 2000;15(1):93–101. doi: 10.1016/S0883-5403(00)91337-8. [DOI] [PubMed] [Google Scholar]
- 23.Thien TM, Karrholm J. Design-related risk factors for revision of primary cemented stems. Acta Orthop. 2010;81(4):407–412. doi: 10.3109/17453674.2010.501739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lazovic D, Dunai F, Zigan R (2010) The impact of navigation on a modular short stem prosthesis. J Bone Joint Surg (Proceedings) 92-B (SUPP_IV):523–552 d
- 25.Traina F, Clerico M, Biondi F, Pilla F, Tassinari E, Toni A. Sex differences in hip morphology: is stem modularity effective for total hip replacement? J Bone Joint Surg Am. 2009;91(Suppl 6):121–128. doi: 10.2106/JBJS.I.00533. [DOI] [PubMed] [Google Scholar]
- 26.Traina F, De FM, Biondi F, Tassinari E, Galvani A, Toni A. The influence of the centre of rotation on implant survival using a modular stem hip prosthesis. Int Orthop. 2009;33(6):1513–1518. doi: 10.1007/s00264-008-0710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]