Abstract
In the United States, racial-ethnic minorities experience disproportionately high rates of end stage renal disease, but they are substantially less likely to receive living donor kidney transplants (LDKT) compared with their majority counterparts. Minorities may encounter barriers to LDKT at several steps along the path to receiving LDKT including consideration, pursuit, completion of LDKT, and the post-LDKT experience. These barriers operate at different levels related to potential recipients and donors, health care providers, health system structures, and communities. In this review, we present a conceptual framework describing various barriers minorities face along the path to receiving LDKT. We also highlight promising recent and current initiatives to address these barriers, as well as gaps in initiatives, which may guide future interventions to reduce racial-ethnic disparities in LDKT.
Keywords: race, ethnicity, disparities, minority, organ donation, barriers to living kidney donation, living donor kidney transplantation
Introduction
In the United States (US), racial-ethnic minorities experience disproportionately high rates of end-stage renal disease (ESRD) but are far less likely to undergo kidney transplantation than Whites1–3. Despite long-standing recognition of the need to reduce racial-ethnic disparities in transplantation, relatively little progress in identifying effective mechanisms to narrow disparities has been made1–3. Living donor kidney transplantation (LDKT) represents the optimal therapy for many patients with ESRD, providing numerous clinical benefits compared to prolonged dialysis or deceased donor kidney transplantation, including better patient and graft survival and improved quality of life4–5. LDKT also allows potential transplant recipients to bypass the lengthy deceased donor kidney transplant waiting list and therefore is a promising strategy for improving access to transplantation1, 6–7. However, over the past decade, minority ESRD patients have been consistently less likely than their majority counterparts to receive LDKT1, 6–11, limiting the promise of this therapy to address inequities in access to kidney transplants.
Conceptual Framework: Barriers Limiting Minorities’ Access to LDKT
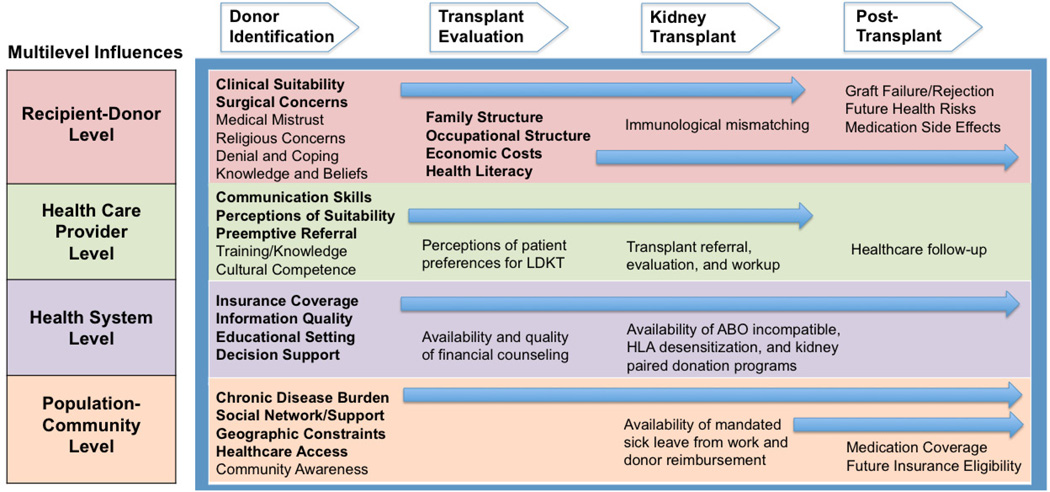
To inform the development of effective interventions to improve racial-ethnic Minorities’ access to LDKT, we must first elucidate barriers to living kidney donation and attempt to understand the mechanisms through which these barriers perpetuate disparities in access to LDKT. Studies suggest racial-ethnic minorities may encounter barriers at several steps along the path to successful LDKT, including during donor identification, transplant evaluation, and the kidney transplantation process itself12–32. Some minorities’ willingness to pursue LDKT may also be heavily influenced by their concerns about post-LDKT challenges. These barriers to LDKT may be attributable to multiple factors, including recipient and donor attitudes, beliefs, and clinical characteristics12–21; health care provider knowledge, attitudes and behaviors22–26; and population awareness, attitudes, and disease burden27–30. A unifying framework describing barriers to living kidney donation could assist ongoing efforts and inform the development of future strategies to overcome barriers to living kidney donation. In this paper, we present a conceptual framework (Figure 1) that contextualizes barriers identified along the path to LDKT. We also review recent and ongoing initiatives to overcome these barriers, and we identify opportunities for the development of new strategies to reduce racial-ethnic disparities in LDKT.
Figure 1.
Multilevel Influences Contributing to Barriers to Living Kidney Donation for Racial-Ethnic Minorities at Each Stage of the LDKT Process
Barriers During Donor Identification
Recipient, Donor Level
Racial-ethnic minority ESRD patients may have knowledge deficits, concerns and attitudes which contribute to their increased difficulties identifying and approaching potential living kidney donors compared with their majority counterparts. Studies of African American and Hispanic patients have demonstrated their poor knowledge about the benefits of kidney transplantation and unmet concerns about surgical risks of LDKT for donors and recipients, which may hinder their willingness to approach potential donors13–14, 17, 33. Furthermore, African American potential recipients may experience high rates of psychological denial about the need for a kidney transplant14, 16, while Hispanic patients may be less likely to approach potential donors due to expectations that a relative would initiate an offer to donate13. As minorities consider pursuing LDKT, their concerns about graft failure and rejection rates, as well as potential health risks for living donors may also influence their willingness to identify and approach potential donors18, 20, 32. Additional barriers to donor identification for minority patients may include concerns about transplant medication costs (due to limited Medicare/insurance coverage) and potential medication side effects, as well as concerns about future financial risks, insurance eligibility, and medical coverage for their potential donors14, 35–36. Cultural biases and differences in family decision-making may also pose as additional barriers to identification of potential donors. Recent data suggest older African Americans may be less likely to participate in LDKT due to concerns regarding the impact of living donation upon burial/cremation and spiritual well-being after death for living donors19. Asian Americans have also demonstrated more negative attitudes toward organ donation than Whites, including stronger cultural and religious concerns about maintaining body integrity after death47. Additionally, differential rates of clinical suitability may reduce the availability of minority potential donors and lead to disparate rates of LDKT21.
Health Care Provider, Health System Levels
Health care providers’ perceptions of their patients’ suitability and preferences for LDKT appear to differ according to patient race-ethnicity and may be associated with lower rates of LDKT education and transplant referral for minority patients22–23. Additionally, lower rates of preemptive physician-patient and physician-family discussions about LDKT among minorities likely reflect these inherent biases24–25. A recent study found that general nephrologists who primarily serve African American patients reportedly spent less time providing patients with LDKT education and counseling than counterparts who serve proportionately fewer African American patients26. These differences in provider-patient interactions may, in part, reflect variations in provider communication skills and cultural competence, knowledge about LDKT, and perceptions of patient suitability and preferences for LDKT 22–26. Suboptimal quality of educational information about LDKT and lack of decision support regarding ESRD treatment options may serve as additional barriers to donor identification for minorities, but these issues have been poorly studied.
Population, Community Level
Currently, a majority of LDKT recipients receive kidneys donated by relatives or non-relatives emerging from recipients’ close social networks. Unfortunately, evidence suggests that the disproportionately high burden of chronic diseases, particularly diabetes and hypertension, within racial-ethnic minorities’ families and social networks may reduce the potential donor pool for many minority potential recipients 27–30. For example, clustering of ESRD and associated risk factors has been noted within African American families, and first- or second-degree relatives of ESRD patients are at increased risk for developing ESRD27. Suboptimal community awareness about the benefits of and need for LDKT, as well as poor access to health care may serve as additional barriers to living kidney donation13.
Barriers During Transplant Evaluation
Recipient, Donor Level
Although racial-ethnic minorities are less likely than Whites to complete the transplant evaluation process31, our understanding of specific barriers to successful completion of this integral step is limited. It is postulated that minority donor and recipients’ concerns about surgical risks of LDKT combined with higher rates of obesity, diabetes, and hypertension among potential donors may contribute to lower rates of minorities completing the transplant evaluation process21, 31. Alternatively, economic constraints, including less flexibility to leave work for extensive transplant workup and recovery may also contribute to disparate rates of completing transplant evaluation.
Health Care Provider, Health System Levels
Although not restricted to LDKT, delayed receipt of nephrology subspecialty care prior to renal replacement therapy initiation has been associated with lower transplant referral rates, higher rates of incomplete evaluations, and reduced access to transplantation48–49. In a similar manner to donor identification, health care providers’ perceptions of their patients’ suitability for LDKT (and their inherent biases about patients’ preferences for and adherence to medical therapies) may also lead to lower rates of transplant evaluation and higher rates of incomplete workups among minority potential recipients compared to Whites22–24. Additionally, emerging research suggests possible links between inadequate health literacy and poorer ESRD outcomes, such as higher patient mortality39 and lower rates of transplant evaluations38, 40. Notably, low health literacy has been shown to be highly prevalent among African American hemodialysis patients and may be associated with less access to kidney transplantation37–38. Further, average health literacy rates among Hispanic, African American, and American Indian/Alaska Native adults within the general population are reportedly lower than rates among Whites and Asian/Pacific Islanders41. Minimal availability and use of language and health literacy-appropriate educational resources about LDKT may contribute to minorities’ higher rates of incomplete LDKT workups. Existing educational resources about LDKT may also lack important information that could alleviate minorities’ concerns about the potential short-and long-term financial burden of LDKT14, 32.
Population, Community Level
Disparities in population disease burden and community resource allocation may also contribute to racial-ethnic differences in living kidney donation. For instance, historic differences in the racial composition of certain US geographic regions, such as in the Southeastern US are linked to well-documented differences in rates of chronic illnesses28–30. High rates of cardiovascular disease, hypertension, and diabetes in distinct regions of the Southeastern US where large populations of African American ESRD patients and their families reside may disproportionately limit the potential donor pool for this group compared with counterparts who reside in other US regions28–30. Transplant centers performing LDKT may also be more heavily concentrated in certain metropolitan regions. Data suggest African Americans living in rural areas may be less likely to receive transplants than their urban counterparts42. As evidenced by disproportionately lower kidney transplant rates in areas with higher degrees of poverty, minority patients and potential donors may also encounter more geographic and socioeconomic barriers to completing transplant workup43–45.
Barriers During Kidney Transplantation
Recipient, Donor Level
Racial-ethnic minorities who complete transplant evaluation and workup might encounter additional barriers to successful LDKT, such as human leukocyte antigen (HLA) sensitization and ABO incompatibility46. Lower rates of preemptive LDKT referrals for minority patients, which result in higher rates of dialysis initiation, might contribute to higher rates of anemia and transfusion leading to HLA sensitization and higher burden of medical complications for minorities that impede successful LDKT24.
Health Care Provider, Health System Levels
Limited availability of blood-type compatible LDKT and less minority participation in paired kidney exchange programs may also contribute to disparate rates of LDKT46.
Population, Community Level
A number of recent federal and state policies have been enacted to provide financial support to living donors, including mandated sick leave from work and reimbursement for some living donor-related expenses; however, evidence suggests this legislation has not yet translated to increased rates of LDKT50. The extent to which racial-ethnic minorities who are actively considering LDKT are aware of these policies is unclear. Less awareness of these policies among minorities could be associated with demonstrated financial concerns about the LDKT process.
Barriers After LDKT
Recipient, Donor Level
The long-term success of living kidney donation among minorities may be threatened by several factors. Current data suggest African American living donors may face increased risk of developing ESRD compared to Whites51,52. Low health literacy, which is highly prevalent among minority adults41, may be associated with suboptimal transplant self-care and lower levels of kidney function among LDKT recipients34, 40.
Provider, Structural Levels
Reduced health care access, including poor availability or utilization of routine follow-up medical care and less health insurance coverage may also lead to suboptimal long-term clinical outcomes for minority living donors. Currently in the US, most living donor-related expenses are covered by the recipient’s health insurance. Notably, a significant proportion of living donors in the US also lack health insurance coverage at the time of LDKT35. Poor access to health care may be particularly prevalent among younger minorities53, possibly resulting in inferior rates of long-term healthcare follow-up and poorer clinical outcomes compared to Whites.
Population, Community Level
Lower socioeconomic status, less access to healthy foods, and resource deprivation may also contribute to suboptimal post-LDKT outcomes within racially-segregated minority communities54–55. For instance, a recent study of US Renal Data System and US Census data found that transplant recipients living in predominantly African American neighborhoods have inferior post-transplant outcomes (i.e. patient mortality and graft loss) compared with recipients living in neighborhoods with a lower percentage of African Americans55.
Recent and Current Initiatives To Address Barriers To LDKT
A number of promising strategies to address barriers to living kidney donation at each stage of LDKT process currently exist (Table 1). We describe some of these initiatives, targeted at recipients and donors, health care providers and the health care system, and population and community factors.
Table 1.
Promising Initiatives to Address Barriers to Living Kidney Donation for Racial-Ethnic Minorities
| DONOR IDENTIFICATION INITIATIVES |
TRANSPLANT EVALUATION INITIATIVES |
KIDNEY TRANSPLANT INITIATIVES |
POST- TRANSPLANT INITIATIVES |
|
|---|---|---|---|---|
|
RECIPIENT-DONOR INITIATIVES |
|
|||
|
HEALTH CARE PROVIDER INITIATIVES |
|
|
|
|
|
HEALTH SYSTEM INITIATIVES |
|
|
|
|
|
POPULATION- COMMUNITY INITIATIVES |
|
Recipient, Donor Initiatives
Home, Community, and Clinic-Based Education: A randomized trial evaluating the effectiveness of a home and community-based educational intervention to address concerns about living kidney donation found that patients who received the intervention were more likely to have had living donor inquiries than those who received standard clinic-based education33. Similarly, an ongoing study to develop a program tailored to patients’ level of transplant readiness will evaluate the effectiveness of conducting this educational intervention within the in-center dialysis setting56. Social Network Engagement: Lower LDKT awareness and knowledge among families and existing social networks might also contribute to less LDKT among racial-ethnic minorities. Increased community awareness and involvement of social networks beyond immediate family members in educational efforts may help to overcome these barriers for minorities57. A new initiative to engage potential LDKT recipients’ families, friends, or associates as ‘champions’ to help potential recipients raise awareness within their social networks regarding their need for a donated kidney may represent a promising strategy to overcome minorities’ difficulties approaching potential donors58. Preemptive Transplant Education: A recent randomized trial evaluated the effectiveness of a culturally sensitive educational and behavioral intervention designed to improve preemptive transplant education. The study found that the intervention, which incorporated social worker visits, educational videos and booklets, increased the pursuit of LDKT among participants59. Another study highlighted the importance of quality of life and health benefits of LDKT when designing interventions to improve preemptive transplant education60. Financial Counseling: The incorporation of social workers and financial counselors within educational efforts has also been shown to reduce patients’ financial concerns regarding the LDKT process32.
Health Care Provider, Health System Initiatives
Enhanced Provider-Patient/Family Education: The Medicare Improvement for Patients and Providers Act of 2008 (MIPPA) aims to enhance timely provider-patient LDKT educational sessions and decision support for pre-ESRD patients61. Standardized Training for Non-Transplant Healthcare Professionals: Standardized education and training of health care providers not directly involved in the LDKT process (e.g. primary care providers and general nephrologists) could help to raise awareness of LDKT as a treatment option, reduce potential biases about patient suitability for LDKT22–23, enhance provider-patient LDKT communication, and increase rates of preemptive transplant referrals. The Medicare National Transplant Education Quality Improvement Initiative, which links dialysis facility quality measures to reimbursement, is one system-level intervention designed to improve rates of transplant education within in-center hemodialysis facilities61. Paired Kidney Donation, HLA Desensitization, and ABO-Incompatible Programs: Historically, high degrees of pre-sensitization and ABO-incompatibility have represented challenging immunological barriers to transplant among minority patients. However, wider adoption of paired kidney donation, HLA desensitization, and ABO-incompatible programs hold promise to overcome these challenges46.
Population, Community Initiatives
Increased “Neighborhood” Health: Population-level interventions to improve the general health of underserved communities may help to decrease the disproportionate burden of chronic disease among minority populations. Examples of such efforts include increasing the availability of fresh, nutritious foods54, enhancing access to safe public spaces for exercise and recreation, reducing exposure to potential environmental toxins65, and implementing community-based screening programs for kidney disease and related risk factors66. Satellite Transplant Centers: Although future work is needed to determine the extent to which geographic barriers contribute to racial disparities in access to LDKT, it is postulated that certain minority populations might face unique challenges accessing transplant centers based upon their geographic distributions. To this end, a recent initiative found that bringing satellite transplant clinics to rural areas helped to address geographic and socioeconomic barriers and resulted in increased rates of transplant referrals for patients living in the Southeastern US45. Federal and State Policies to Support Living Donors: Federal and state legislation to support living donors, such as the National Living Donor Assistance Program authorized by the Organ Donation and Recovery Improvement Act of 200467, and expanded Medicare coverage of immunosuppressant drugs may help to overcome potential financial barriers to LDKT.
Next Steps: Future Work Needed to Narrow LDKT Disparities
Our conceptual framework highlights areas where future work is needed to further elucidate racial-ethnic barriers along the path to successful LDKT and lends insight to the development of future strategies to improve living kidney donation for minorities.
Expansion of efforts to understand barriers to donor identification among a more diverse range of racial-ethnic minorities. To date, most studies identifying barriers to LDKT among racial-ethnic minorities have focused on potential recipient-related barriers occurring within the donor identification stage, particularly among African Americans and Hispanics. This work should be expanded to include studies of other minority groups such as Asians, Pacific Islanders, and American Indians/Alaska Natives who also experience disproportionately high rates of ESRD but are less likely to receive LDKT. More research is also needed to identify barriers to LDKT for potential living donors among all racial-ethnic groups.
Improved understanding of racial-ethnic minorities’ barriers to completing LDKT evaluation and workup. Work elucidating unique barriers that racial-ethnic minorities face in completing LDKT evaluation and workup could inform the development of effective interventions to overcome barriers in this phase of the LDKT process. Studies expanding our knowledge of how minority patients cope with advancing chronic kidney disease and studies further exploring the influence of family dynamics in diverse populations as related to rates of seeking transplants may be particularly helpful.
Culturally sensitive and health literacy-appropriate educational resources to improve minorities’ understanding of LDKT and transplant self-care. Because racial-ethnic minorities are disproportionately affected by inadequate health literacy, culturally sensitive educational interventions tailored to accommodate low health literacy could be particularly useful in improving potential recipients’, their families’, and their communities’ knowledge and awareness about the risks and benefits of LDKT. Efforts to incorporate the importance of medication adherence and self-care within transplant-related educational materials may also help to reduce racial-ethnic disparities in LDKT outcomes.
Improved characterization of racial-ethnic minorities’ long-term clinical risks with LDKT Efforts to accurately quantify the short-and long-term health and economic consequences of living donation for minority living donors are needed to ensure long-term donor safety and well-being and to better inform potential recipients and donors about the risks associated with their pursuit of LDKT. Comprehensive surveillance systems are needed to enhance tracking of long-term health outcomes for donors of all races and ethnicities.
Improved cultural competency and strengthened communication among medical professionals Strategies to help medical professionals identify their unconscious biases regarding patient suitability and preferences for LDKT may help to improve minorities’ referral rates. Improving provider competence in communicating with racial-ethnic minority patients and families may also help to enhance the informed consent process and lessen minorities’ mistrust of the LDKT process. Strengthened communication between transplant, dialysis, and primary care providers, as well as educational support from a multidisciplinary team of health professionals (e.g. nurses, physicians, pharmacists, nephrologists, surgeons) may also help to overcome existing barriers to living kidney donation.
Community-based collaboration to enhance trust, awareness, and support for LDKT. Sustained and meaningful collaborations between medical-transplant professionals, religious leaders, and community organizations may help to foster patient and family trust in healthcare providers’ recommendations for LDKT and raise awareness and social support for those considering LDKT within minority communities.
Improved support for living donors post-donation follow up: To reduce donor concerns regarding post-transplant follow-up, policymakers should consider methods to enhance medical follow-up for living donors through increased access to health insurance coverage and primary care providers.
Conclusions
Significant work has been done to identify barriers faced by racial-ethnic minorities in their pursuit of LDKT, and several initiatives have emerged to address these barriers. However, many of these initiatives are relatively new. Thus, evidence of long-term effectiveness and optimal methods for implementing and disseminating these strategies are not yet clear. Rigorously designed studies that demonstrate the effectiveness of promising interventions to address specific barriers racial-ethnic minorities face along the path toward LDKT may guide policy makers, clinicians, and patients to utilize these interventions more broadly. Partnerships between patient advocacy groups, health care providers, and community organizations should be developed and leveraged to ensure the long-term sustainability of effective interventions.
Summary Points.
Racial-ethnic minorities may encounter barriers to living kidney donation at distinct steps in the transplant process including during donor identification, transplant evaluation, surgery and post-transplantation.
Determinants of living kidney donation operate at contextual levels beyond just the potential recipient or donor.
Strategies that address barriers to living kidney donation at the level of the potential recipient, donor, health care provider, health care system and/or community network are currently under investigation.
Rigorously designed clinical trials that test the effectiveness of promising interventions are needed to guide broader dissemination and adoption.
Additional studies are needed to address low rates of living kidney donation within less-studied racial and ethnic groups (e.g., Asians, Hispanics, American Indians/Alaska Natives, Pacific Islanders).
Acknowledgments
Funding Sources: Ms. Purnell was supported by grant 5F31DK08484003 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH), Bethesda, MD. Dr. Hall was supported by grant K23DK087900 from the NIDDK of the NIH and the Norman Coplon extramural grant program of Satellite Healthcare. Dr. Boulware was supported by grants K23DK070757 and R01DK079682 from the NIDDK of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: There are no affiliations or financial involvement with any organization or entity with a direct financial interest in the subject matter or materials discussed in the manuscript. The authors have no financial or nonfinancial conflict to disclose.
References
- 1.U.S. Renal Data System, USRDS 2009. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2009. Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. [Google Scholar]
- 2.Eggers PW. Racial differences in access to kidney transplantation. Health Care Financing Review. 1995;17(2):89–103. [PMC free article] [PubMed] [Google Scholar]
- 3.Powe NR, Boulware LE. The uneven distribution of kidney transplants: Getting at the root causes and improving care. Am J Kidney Dis. 2002;40(4):861–863. doi: 10.1053/ajkd.2002.36562. [DOI] [PubMed] [Google Scholar]
- 4.Jofre R, Lopez-Gomez JM, Moreno F, Sanz-Guajardo D, Valderrabano F. Changes in quality of life after renal transplantation. Am J Kidney Dis. 1998;32(1):93–100. doi: 10.1053/ajkd.1998.v32.pm9669429. [DOI] [PubMed] [Google Scholar]
- 5.Cecka M. Clinical outcome of renal transplantation. Factors influencing patient and graft survival. Surg Clin North Am. 1998;78:133–148. doi: 10.1016/s0039-6109(05)70639-3. [DOI] [PubMed] [Google Scholar]
- 6.United Network for Organ Sharing. Organ Procurement and Transplantation Network Data: Kidney Transplants in the US, 1988–2011. [Accessed May 2011]; Available at http://optn.transplant.hrsa.gov/latestData/rptData.asp.
- 7.Agency for Healthcare Research and Quality. Rockville, MD: US Department of Health and Human Services, Agency for Healthcare Research and Quality; 2008. Feb, 2007 National Healthcare Disparities Report. AHRQ Pub. No.08-0041. [Google Scholar]
- 8.Gore JL, Danovitch GM, Litwin MS, Pham PT, Singer JS. Disparities in the utilization of live donor kidney transplantation. Am J Transplant. 2009;9:1124–1133. doi: 10.1111/j.1600-6143.2009.02620.x. [DOI] [PubMed] [Google Scholar]
- 9.Hall YN, Sugihara JG, Go AS, Chertow GM. Differential mortality and transplantation rates among Asians and Pacific Islanders with ESRD. J Am Soc Nephrol. 2005;16:3711–3720. doi: 10.1681/ASN.2005060580. [DOI] [PubMed] [Google Scholar]
- 10.Young CJ, Gaston RS. African Americans and renal transplantation: Disproportionate need, limited access, and impaired outcomes. Am J Med Sci. 2002;323:94–99. doi: 10.1097/00000441-200202000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Sequist TD, Narva AS, Stiles SK, Karp SK, Cass A, Ayanian JZ. Access to renal transplantation among American Indians and Hispanics. Am J Kidney Dis. 2004;44:344–352. doi: 10.1053/j.ajkd.2004.04.039. [DOI] [PubMed] [Google Scholar]
- 12.Weng FL, Reese PP, Mulgaonkar S, Patel AM. Barriers to living donor kidney transplantation among black or older transplant candidates. Clin J Am Soc Nephrol. 2010;5(12):2338–2347. doi: 10.2215/CJN.03040410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alvaro EM, Siegel JT, Turcotte D, Lisha N, Crano WD, Dominick A. Living kidney donation among Hispanics: a qualitative examination of barriers and opportunities. Prog Transplant. 2008;18(4):243–250. doi: 10.1177/152692480801800406. [DOI] [PubMed] [Google Scholar]
- 14.Boulware LE, Hill-Briggs F, Kraus ES, et al. Identifying and addressing barriers to African American and non-African American families’ discussions about preemptive living related kidney transplantation. Prog Transplant. 2011;21:97–105. doi: 10.1177/152692481102100203. [DOI] [PubMed] [Google Scholar]
- 15.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients' preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341(22):1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 16.Lunsford SL, Simpson KS, Chavin KD, et al. Racial differences in coping with the need for kidney transplantation and willingness to ask for live organ donation. Am J Kidney Dis. 2006;47:324–331. doi: 10.1053/j.ajkd.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 17.Waterman AD, Stanley SL, Covelli T, Hazel E, Hong BA, Brennan DC. Living donation decision making: recipients’ concerns and educational needs. Prog Transplant. 2006;16:17–23. doi: 10.1177/152692480601600105. [DOI] [PubMed] [Google Scholar]
- 18.Boulware LE, Ratner LE, Sosa JA, Cooper LA, LaVeist TA, Powe NR. Determinants of willingness to donate living related and cadaveric organs: identifying opportunities for intervention. Transplantation. 2002;73:1683–1691. doi: 10.1097/00007890-200205270-00029. [DOI] [PubMed] [Google Scholar]
- 19.Purnell TS, Powe NR, Troll M, Wang NY, LaVeist TA, Boulware LE. Age and racial/ethnic differences in willingness to donate live kidneys in the United States. Paper presented at: American Public Health Association Annual Meeting; October 31, 2011; Washington, DC. [Google Scholar]
- 20.Boulware LE, Ratner LE, Sosa JA, Tu AH, Nagula S, Simpkins CE, et al. The general public's concerns about clinical risk in live kidney donation. Am J Transplant. 2002;2:186–193. doi: 10.1034/j.1600-6143.2002.020211.x. [DOI] [PubMed] [Google Scholar]
- 21.Gaylin DS, Held PJ, Port FK, et al. The impact of comorbid and sociodemographic factors on access to renal transplantation. JAMA. 1993;269:603–608. [PubMed] [Google Scholar]
- 22.Ayanian JZ, Cleary PD, Keogh JH, Noonan SJ, David-Kasdan JA, Epstein AM. Physicians' beliefs about racial differences in referral for renal transplantation. Am J Kidney Dis. 2004;43:350–357. doi: 10.1053/j.ajkd.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 23.Ghahramani N. Perceptions of patient suitability for kidney transplantation: a qualitative study comparing rural and urban nephrologists. Paper presented at: American Transplant Conference; 20011 May 1–4; Philadelphia PA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kasiske BL, Snyder JJ, Matas AJ, Ellison MD, Gill JS, Kausz AT. Preemptive kidney transplantation: The advantage and the advantaged. J Am Soc Nephrol. 2002;13:1358–1364. doi: 10.1097/01.asn.0000013295.11876.c9. [DOI] [PubMed] [Google Scholar]
- 25.Boulware LE, Meoni LA, Fink NE, Parekh RS, Kao WH, Klag MJ, Powe NR. Preferences, knowledge, communication, and patient-physician discussion of living kidney transplantation in African American families. Am J Transplant. 2005;5(6):1503–1512. doi: 10.1111/j.1600-6143.2005.00860.x. [DOI] [PubMed] [Google Scholar]
- 26.Balhara K, Kucirka L, Jaar B, Segev D. Race, age, and insurance status are associated with duration of kidney transplant counseling provided by non-transplant nephrologists. Paper presented at: American Transplant Conference; 20011 May 1–4; Philadelphia PA. [Google Scholar]
- 27.Freedman BI, Spray BJ, Tuttle AB, Buckalew VM. The familial risk of end-stage renal disease in African Americans. Am J Kidney Dis. 1993;21(4):387–393. doi: 10.1016/s0272-6386(12)80266-6. [DOI] [PubMed] [Google Scholar]
- 28.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 29.Barker LE, Kirtland KA, Gregg EW, Geiss LS, Thompson TJ. Geographic distribution of diagnosed diabetes in the US. A diabetes belt. Am J Prev Med. 2011;40(4):434–439. doi: 10.1016/j.amepre.2010.12.019. [DOI] [PubMed] [Google Scholar]
- 30.Mujib M, Zhang Y, Feller MA, Ahmed A. Evidence of a “heart failure belt” in the Southeastern United States. Am J Cardiol. 2011;107:935–937. doi: 10.1016/j.amjcard.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reeves-Daniel A, Adams PL, Assimos D, et al. Impact of race and gender on live kidney donation. Clin Transplant. 2009;23:39–46. doi: 10.1111/j.1399-0012.2008.00898.x. [DOI] [PubMed] [Google Scholar]
- 32.Lunsford SL, Shilling LM, Chavin KD, et al. Racial differences in the living kidney donation experience and implications for education. Prog Transplant. 2007;17:234–240. doi: 10.1177/152692480701700312. [DOI] [PubMed] [Google Scholar]
- 33.Rodrigue JR, Cornell DL, Kaplan B, Howard RJ. A randomized trial of a home-based educational approach to increase live donor kidney transplantation: effects in blacks and whites. Am J Kidney Dis. 2008;51:663–670. doi: 10.1053/j.ajkd.2007.11.027. [DOI] [PubMed] [Google Scholar]
- 34.Gordon EJ, Ladner DP, Caicedo JC, Franklin J. Disparities in kidney transplant outcomes: a review. Semin Nephr. 2010;30(1):81–89. doi: 10.1016/j.semnephrol.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ommen ES, Gill JS. The system of health insurance for living donors is a disincentive for live donation. Am J Transplant. 2010;10:747–750. doi: 10.1111/j.1600-6143.2009.02994.x. [DOI] [PubMed] [Google Scholar]
- 36.Yang RC, Thiessen-Philbrook H, Klarenbach S, Vlaicu S, Garg AX. Insurability of living organ donors: a systematic review. Am J Transplant. 2007;7:1542–1551. doi: 10.1111/j.1600-6143.2007.01793.x. [DOI] [PubMed] [Google Scholar]
- 37.Green JA, Mor MK, Shields AM, et al. Prevalence and demographic and clinical associations of health literacy in patients on maintenance hemodialysis. Clin J Am Soc Nephrol J Am Soc Nephrol. 2011;6:1354–1360. doi: 10.2215/CJN.09761110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grubbs V, Gregorich SE, Perez-Stable EJ, Hsu CY. Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol. 2009;4:195–200. doi: 10.2215/CJN.03290708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cavanaugh KL, Wingard RL, Hakim RM, et al. Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol. 2010;21:1979–1985. doi: 10.1681/ASN.2009111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Devraj R, Gordon EJ. Health literacy and kidney disease: toward a new line of research. Am J Kidney Dis. 2009;53:884–889. doi: 10.1053/j.ajkd.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 41.Kutner M, Greenberg E, Jin Y, Paulsen C. Washington, DC: National Center for Education Statistics; The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy (NCES 2006-483). U.S. Department of Education. [Google Scholar]
- 42.O’Hare AM, Johansen KL, Rodriguez RA. Dialysis and kidney transplantation among patients living in rural areas of the United States. Kidney Int. 2006;69:343–349. doi: 10.1038/sj.ki.5000044. [DOI] [PubMed] [Google Scholar]
- 43.Volkova N, McClellan W, Klein M, et al. Neighborhood poverty and racial differences in ESRD incidence. J Am Soc Nephrol. 2008;19:356–364. doi: 10.1681/ASN.2006080934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hall YN, O’Hare AM, Young BA, Boyko EJ, Chertow GM. Neighborhood poverty and kidney transplantation among US Asians and Pacific Islanders with end-stage renal disease. Am J Transplant. 2008;8:2402–2409. doi: 10.1111/j.1600-6143.2008.02413.x. [DOI] [PubMed] [Google Scholar]
- 45.Gibney EM, Wolf J, Zayas C, et al. Bringing transplantation to recipients: Effect of satellite outreach clinics on access to transplantation services. Paper presented at: American Transplant Conference; 2011 May 1–4; Philadelphia, PA. [Google Scholar]
- 46.Warren DS, Montgomery RA. Incompatible kidney transplantation: lessons from a decade of desensitization and paired kidney exchange. Immunol Res. 2010;47(1–3):257–264. doi: 10.1007/s12026-009-8157-y. [DOI] [PubMed] [Google Scholar]
- 47.Alden DL, Cheung AHS. Organ donation and culture: a comparison of Asian American and European American beliefs, attitudes, and behaviors. J App Soc Psych. 2000;30:293–314. doi: 10.1111/j.1559-1816.2000.tb02317.x. [DOI] [PubMed] [Google Scholar]
- 48.Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey AS, Powe NR. The timing of specialist evaluation in chronic kidney disease and mortality. Ann Intern Med. 2002;137:479–486. doi: 10.7326/0003-4819-137-6-200209170-00007. [DOI] [PubMed] [Google Scholar]
- 49.Cass A, Cunningham J, Snelling P, Ayanian JZ. Late referral to a nephrologist reduces access to renal transplantation. Am J Kidney Dis. 2003;42:1043–1049. doi: 10.1016/j.ajkd.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 50.Boulware LE, Troll MU, Plantinga LC, Powe NR. The association of state and national legislation with living kidney donation rates in the United States: A National Study. Am J Transplant. 2008;8:1451–1470. doi: 10.1111/j.1600-6143.2008.02266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Taler SJ, Gillespie B, Ibraim H, et al. Renal and Lung Living Donors Evaluation (RELIVE) Study Group. Predictors of end-stage renal disease in live kidney donors at three US kidney transplant centers. Paper presented at: American Transplant Conference; 2011 May 1–4; Philadelphia, PA. [Google Scholar]
- 52.Doshi M, Garg AX, Gibney E, Parikh C. Race and renal function early after live kidney donation: an analysis of the United States Organ Procurement and Transplantation Network Database. Clin Transplant. 2010;24:E153–E157. doi: 10.1111/j.1399-0012.2010.01209.x. [DOI] [PubMed] [Google Scholar]
- 53.Hall YN, Rodriguez RA, Boyko EJ, Chertow GM, O’Hare AM. Characteristics of uninsured Americans with chronic kidney disease. J Gen Intern Med. 2009;24(3):917–922. doi: 10.1007/s11606-009-1028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hosler AS, Rajulu DT, Fredrick BL, Ronsani AE. Assessing retail fruit and vegetable availability in urban and rural underserved communities. Prev Chronic Dis. 2008;5(4):A123. Epub 2008 Sept 15. [PMC free article] [PubMed] [Google Scholar]
- 55.Chakkera H, Szalacha L, Rodriguez R, Noble B, O’Hare A. Relationship between residential area racial composition and outcomes after kidney transplantation. Paper presented at: American Transplant Conference; 2011 May 1–4; Philadelphia, PA. [Google Scholar]
- 56.Waterman AD, Hyland SS, Goalby C, Robbins M, Dinkel K. Improving transplant education in the dialysis setting: the “explore transplant” initiative. Dialysis & Transplantation. 2010;39(6):236–241. [Google Scholar]
- 57.Clark CR, Hicks LS, Keogh JH, Epstein AM, Ayanian JZ. Promoting access to renal transplantation: the role of social support networks in completing pre-transplant evaluations. J Gen Intern Med. 2008;23:1187–1193. doi: 10.1007/s11606-008-0628-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Segev DL. The Living Donor Champion Program. [Accessed July 2011]; Available at: http://www.hopkinsmedicine.org/transplant/Patient/LDCProgram.
- 59.Boulware LE, Ephraim P, Hill-Briggs F, et al. Effectiveness of educational and behavioral interventions to improve pursuit of pre-emptive living-related kidney transplantation: the Talking about Live Kidney Donation (TALK) study. Paper presented at: American Transplant Conference; 2011 May 1–4; Philadelphia, PA. [Google Scholar]
- 60.Hayes R, Waterman AD. Improving preemptive transplant education to increase living donation rates: reaching patients earlier in their disease adjustment process. Prog Transplant. 2008;14:251–256. doi: 10.1177/152692480801800407. [DOI] [PubMed] [Google Scholar]
- 61.The Library of Congress. Medicare Improvement for Patients and Providers Act of 2008 (H.R. 6331) [Accessed July 2011]; Available at http://thomas.loc.gov/cgi-bin/bdquery/z?d110:H.R.6331.
- 62.Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, Smarth C, Jenckes MW, Feuerstein C, Bass EB, Powe NR, Cooper LA. Cultural competence: A systematic review of health care provider educational interventions. Med Care. 2005;43:356–373. doi: 10.1097/01.mlr.0000156861.58905.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wesson DE. Is the ethnic disparity in CKD a symptom of dysfunctional primary care in the US? J Am Soc Nephrol. 2008;19:1249–1251. doi: 10.1681/ASN.2008050478. [DOI] [PubMed] [Google Scholar]
- 64.Morena G, Rodriguez MA, Lopez GA, Bholat MA, Dowling PT. Eight years of building community partnerships and trust: the UCLA family medicine community-based participatory research experience. Acad Med. 2009;84(10):1426–1433. doi: 10.1097/ACM.0b013e3181b6c16a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sallis JF, Bauman A, Pratt M. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15(4):379–397. doi: 10.1016/s0749-3797(98)00076-2. [DOI] [PubMed] [Google Scholar]
- 66.National Kidney Foundation. The Kidney Early Evaluation Program (KEEP) [Accessed July 2011]; Available at http://www.kidney.org/news/keep/KEEPabout.cfm.
- 67.National Living Donor Assistance Center. Program background. [Accessed July 2011]; Available at www.livingdonorassistane.org/theprogram/background.aspx.