Abstract
Objective. To determine and describe the nature and extent of medication adherence education in US colleges and schools of pharmacy.
Methods. A mixed-methods research study was conducted that included a national survey of pharmacy faculty members, a national survey of pharmacy students, and phone interviews of 3 faculty members and 6 preceptors.
Results. The majority of faculty members and students agreed that background concepts in medication adherence are well covered in pharmacy curricula. Approximately 40% to 65% of the students sampled were not familiar with several adherence interventions. The 6 preceptors who were interviewed felt they were not well-informed on adherence interventions, unclear on what students knew about adherence, and challenged to provide adherence-related activities for students during practice experiences because of practice time constraints.
Conclusions. Intermediate and advanced concepts in medication adherence, such as conducting interventions, are not adequately covered in pharmacy curriculums; therefore stakeholders in pharmacy education must develop national standards and tools to ensure consistent and adequate medication adherence education.
Keywords: medication adherence, curriculum, medication
INTRODUCTION
The effectiveness of medications depends largely on patients’ adherence to a prescribed medication regimen.1 Although patients’ medication-taking behaviors vary, most only adhere to their regimens approximately 50% of the time, and half stop taking medication for a chronic illness after 1 year.2-5 When patients do not adhere to their regimens, they are at increased risk for hospitalizations, emergency department visits, worsening disease, and poorer quality of life.6-10 Medication non-adherence costs the United States $290 billion per year in unwarranted health care spending and results in an increased incidence of preventable illness and death.1,11
Medication non-adherence is a significant public health concern and has received attention from various stakeholders including the National Council on Patient Information and Education (NCPIE), Agency for Healthcare Research and Quality, The New England Healthcare Institute, the Pharmacy Quality Alliance (PQA), and the National Consumers League. Multi-stakeholder involvement in this issue brought about a national campaign in 2011, “Script Your Future,” to improve consumer awareness of the importance and value of medication adherence and to encourage and increase practitioner efforts to discuss adherence with their patients.12 Additionally, US health care reform policies such as coordinated care (eg, accountable care organizations) and new payment models will rely on the appropriate use of medications. Pharmacists will be required to implement adherence strategies and improve outcomes in practice to receive outcomes-based health care payment.
Over the last 50 years, we have learned much about medication adherence, including epidemiologic factors, predictors of medication non-adherence, and barriers and interventions to improve medication adherence.1 The extent to which academic medicine and pharmacy and educators in the allied health professions have transferred this knowledge and experience to students is less clear. The World Health Organization (WHO) recommends that healthcare professionals be trained in adherence assessment.1 NCPIE, a coalition working to advance communication with patients about appropriate medication use, convened a stakeholder panel of experts to address medication non-adherence. The panel created a consensus on 10 national priorities with the greatest potential to improve medication adherence.13 NCPIE addresses the need for multidisciplinary curriculum development on medication adherence, including pharmacy school curricula, that focuses on increasing public awareness of the adherence problem and implementing solutions. PQA, an organization that focuses on the improvement of medication use across health care settings, has developed metrics to evaluate the impact of pharmacy-level interventions on patient medication adherence.14
Pharmacists are accountable for patients’ medication-taking behavior and future pharmacy graduates need to be prepared to detect, monitor, and intervene to improve patients’ medication adherence. There is a paucity of literature describing the extent to which pharmacy educators teach students about medication adherence. Only 22% of 50 pharmacy colleges and schools surveyed indicated having assessment instruments to evaluate students’ skills related to promoting medication adherence to patients.15 Only 18% had students work with patients to schedule medication doses, tailor therapy, and establish cues to remind them to take their medicine; 12% had educational content focused on determining patient motivation to adhere to a medication regimen; and 8% taught students interventions to improve patients’ medication adherence.
The Accreditation Council for Pharmacy Education’s (ACPE) standards for pharmacy colleges and schools discuss the importance of “optimal medication therapy outcomes and patient safety,” but there is no direct mention of medication adherence, how adherence affects patient outcomes, or the severity of the problem.16 The American Association of Colleges of Pharmacy (AACP) Center for the Advancement of Pharmaceutical Education developed a 2004 recommendation that students should be able to assess a patient’s previous adherence to medication, identify social and behavioral issues associated with non-adherence, and discover different methods within pharmacy to improve adherence.17 The National Association of Boards of Pharmacy (NABP) is also committed to medication adherence as it relates to their mission in “developing, implementing, and enforcing uniform standards for the purpose of protecting the public health.”18 NABP specifically mentions adherence in the first of their 3 competency statements that form the foundation of the North American Pharmacist Licensure Examination (NAPLEX). Specifically, NABP states that the NAPLEX examinee should be able to “identify, present, and address methods to remedy medication non-adherence, misuse, or abuse.”19
Given the importance of the topic to various pharmacy and other stakeholders, the primary objective of this study was to obtain a more detailed description of the nature and extent of medication adherence education in US colleges and schools of pharmacy.
METHODS
The study consisted of 3 parts: (1) a national Web-based survey of faculty members at colleges and schools of pharmacy, (2) a national Web-based survey of student chapters of 2 national pharmacy organizations, Phi Delta Chi (PDC) and the National Community Pharmacists Association (NCPA), and (3) conference calls with a convenience sample of pharmacy preceptors and faculty members.
In the first part of the project, researchers conducted a national Web-based survey to pharmacy faculty members on communication topics taught in US colleges and schools of pharmacy. This cross-sectional survey instrument was developed by the Western University of Health Sciences (WesternU) team, based on the Kimberlin study.15 The study purpose was to identify what communication topics were covered by pharmacy colleges and schools and how they were delivered and evaluated. There were only 2 items that specifically related to medication adherence. The first item asked respondents to indicate whether adherence topics (defined as barriers to adherence and encouraging patient participation in care) were taught as a part of a required or elective course. The second item asked faculty respondents to indicate how this adherence content was delivered (lecture, multimedia, live actors/modeling, practice, and/or case-based). An e-mail with a link to the electronic survey instrument was sent to 269 deans, department chairs, and/or curriculum chairpersons at US colleges and schools of pharmacy (e-mails were sent to more than 1 person at some colleges and schools). The survey was available for completion from December 2010 to March 2011. To achieve an excellent response rate, 3 Web-based reminders to complete the survey instrument were sent. The survey instrument was approved by the university’s institutional review board (IRB).
The second and third parts of the study were led by members of the National Community Pharmacists Association’s (NCPA) Advisory Council on Medication Adherence. These researchers developed a 9-item Web-based survey instrument to send to representatives at 71 student chapters of Phi Delta Chi pharmacy fraternity and 90 student chapters of NCPA. The researchers targeted 2 student organizations to increase the odds of receiving a response from each of the colleges and schools. SurveyMonkey (SurveyMonkey, Palo Alto, CA) was used to distribute the survey to PDC student chapters and SurveyGizmo (SurveyGizmo, Boulder, CO) was used to distribute the survey to NCPA student chapters. Chapter representatives were asked to have 1 third or fourth-year (P3 or P4) student from their chapter to complete the survey instrument, with preference to be given to P4 students because questions about the third year were included in the survey instrument. As an incentive, chapters that participated in the survey were entered into a random drawing to win free registration for their organization’s national meeting.
Because there was no prior research exploring specific adherence topics and how they were covered in curricula, all items were new and constructed for the study’s goals to gain a better description of specific topics covered in colleges and schools of pharmacy. Students were asked to provide online consent to participate before completing the survey instrument. There were 3 items asking respondents to use a 4-point Likert-scale to indicate to what extent a topic was taught: not taught, somewhat taught, moderately taught, or extensively taught. Another item asked respondents to indicate in which courses and years in the pharmacy curriculum adherence topics were covered. Respondents were also asked to describe how adherence topics were presented in the curriculum (eg, lecture, video, textbook/readings, guest speaker, role playing, written patient cases, and other).
Students were queried about the extent to which they engaged in adherence interventions during their introductory pharmacy practice experiences (IPPEs) and advanced pharmacy practice experiences (APPEs). Specifically, students indicated whether they had: (1) no opportunity to do any adherence-related interventions, (2) identified patient non-adherence but could not determine intervention, (3) identified patient non-adherence and planned intervention, and (4) intervened and followed up on a patient. Students could also choose “not applicable” if the opportunity to engage in adherence interventions was not available during their IPPEs and APPEs. Students were asked 4 brief background questions about the name of their college or school of pharmacy, location, type of university (public/private/other), type of pharmacy program (0-6, 2-4, undergraduate then PharmD degree, or accelerated PharmD degree), and in what year of the program the student was enrolled (P1-P4).
In the third part of the study, the NCPA Advisory Council on Medication Adherence developed a list of questions addressing the nature and extent of coverage of adherence topics in the pharmacy curriculum to ask a convenience sample of 6 community pharmacy preceptors (4 from independent pharmacies and 2 from chain pharmacies) and 3 pharmacy faculty members with adherence interests. The independent pharmacy preceptors were all active members of NCPA and the 2 preceptors at chain pharmacies were known to the authors through their preceptor service at their respective pharmacy schools.
These questions were administered during a scheduled conference call (2 group conference calls with preceptors and 1 group conference call with faculty members) conducted by a member of the research team. Consent to participate in the study was obtained prior to the call. The calls were recorded for purposes of transcription and review of key themes. Preceptor questions were focused on what activities students undertake during their practice experiences in the areas of detecting, monitoring, and intervening in medication non-adherence. Preceptors also were asked to what extent they thought students were competent to implement strategies to improve medication adherence. Finally, preceptors were asked to indicate what changes they would make in the pharmacy curriculum to better prepare students to engage in detecting, monitoring, and intervening in medication adherence of patients in community pharmacy practice.
Prior to the telephone interview, the 3 faculty members indicated that they did not have a thorough enough knowledge of the entire curriculum to give an accurate estimate of the extent to which adherence topics were covered, where such topics were taught in the curriculum, and how much time was spent on the different adherence topics. Therefore, 2 survey questions asking for this information were deleted from the interviews with the faculty members. The 3 faculty members provided feedback on whether various adherence topics should be required; how prepared they felt students were to detect, monitor, and intervene in medication non-adherence; and how competent they thought students were in implementing various intervention strategies. The 3 faculty members also identified possible opportunities to better prepare students to engage in adherence-related activities.
All survey data were entered in SPSS 18.0 (SPSS Inc, Chicago, IL) and analyzed using descriptive statistics such as medians and frequencies where appropriate. In a few cases, responses were received from both the Phi Delta Chi and NCPA student chapters of a college or school, and/or 2 or more responses were received from the Phi Delta Chi and/or the NCPA student chapter of a college or school. To ensure only 1 response from each college or school of pharmacy was included in the data analysis, we eliminated the second response if that response was from an individual in their first or second year as we believed that students in the third and fourth years of the program had more knowledge of the entire curriculum. If there were 2 responses from a third or fourth year student at a college or school, we used the response of the more senior student as that student was more likely to be able to answer the APPE questions. In cases where we received 2 or more responses from students in the same year at a college or school, we combined the responses and imputed the averaged score for the college or school. The conference call tapes were transcribed using the Cogi iPhone application (Cogi, Santa Barbara, CA). Student researchers categorized the key themes identified from the phone conversations. Both the student survey instruments and the scripts used during the conference calls were approved by multiple IRBs. (Copies of the survey instruments and the questions asked during the phone interviews are available by request from the corresponding author.)
RESULTS
One hundred ten survey responses were received from 92 different colleges and schools of pharmacy (representatives from 18 of the 92 colleges and schools completed the same survey instrument twice). A majority of faculty respondents (n = 99, 90%) indicated that curricular content/education on medication adherence was required by their college or school of pharmacy, and 1 respondent indicated the school included it as an area of focus within an elective course. Three respondents indicated either that the question was not applicable to their college or school, or that adherence was not covered in their program. A large number of respondents indicated that medication non-adherence was covered through lecture (n = 93), practice-based experiences (n = 74), or case-based problems (n = 60). A smaller number of respondents indicated that adherence was taught using multimedia resources (n = 29) or by live actors and/or modeling (n = 36).
The NCPA Advisory Council on Medication Adherence received 37 of the 71 survey instruments sent to PDC student chapters, and 58 of 90 survey instruments sent to NCPA student chapters. One or more survey instruments were received from 52 (43.7%) of the 119 accredited (full or candidate status) colleges and schools of pharmacy.20 Of the 52 colleges and schools represented, 56% (n = 29) were public and 44% (n = 23) were private. The types of pharmacy programs represented were: 0/6 PharmD programs (4), 2/4 PharmD programs (16), undergraduate degree then PharmD programs (2), accelerated PharmD programs (10), and other types of programs (2). Six (12%) of the survey respondents were fourth-year students, 28 (54%) were third-year students, 17 (33%) were second-year students, and 1 (2%) was a first-year student.
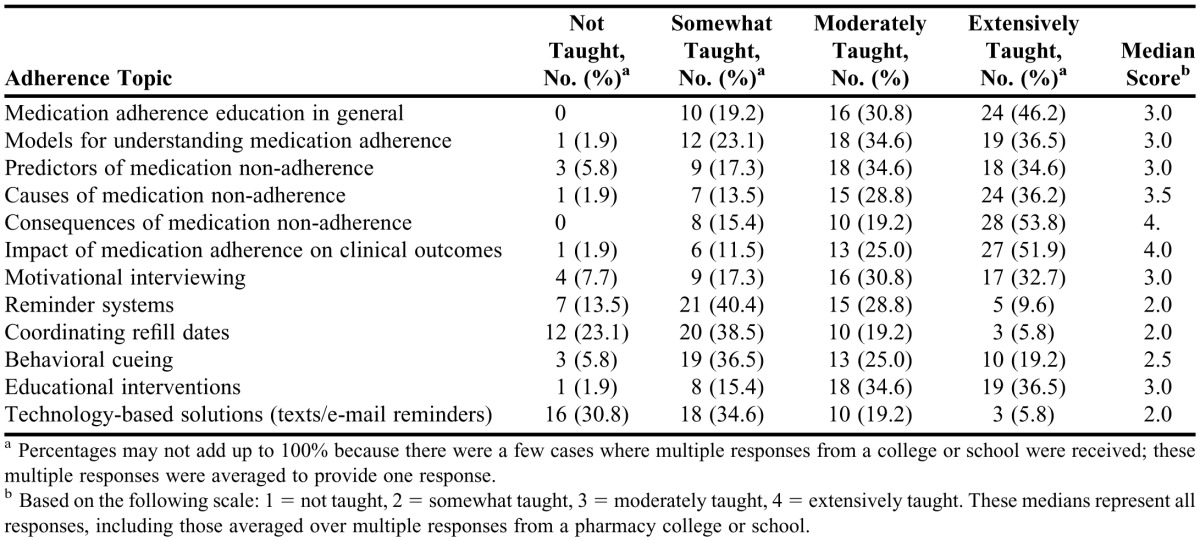
Approximately two-thirds (>70%) of the study sample was “moderately or extensively taught” background topics on medication adherence, including models for understanding adherence; predictors, causes, and consequences of medication non-adherence; and impact of medication adherence on clinical outcomes (Table 1). All of these background topics had a median score of 3 or higher on a 5-point scale, indicating the topics were “moderately or extensively taught.” On the 6 topics relating to adherence interventions, only 2 topics, motivational interviewing and educational interventions, had median scores of 3, indicating the topic was moderately taught. Over 50% of respondents indicated “not being taught at all” or “only somewhat taught” about reminder systems, coordinating refill dates, and technology-based solutions. Student responses were split with regard to behavioral cueing; half of the respondents were “not at all taught” or “somewhat taught” and the other half of respondents were “moderately or extremely taught” the topic.
Table 1.
Pharmacy Students’ Perspectives on Medication Adherence Topics Taught in the Doctor of Pharmacy Curriculum (N = 52)
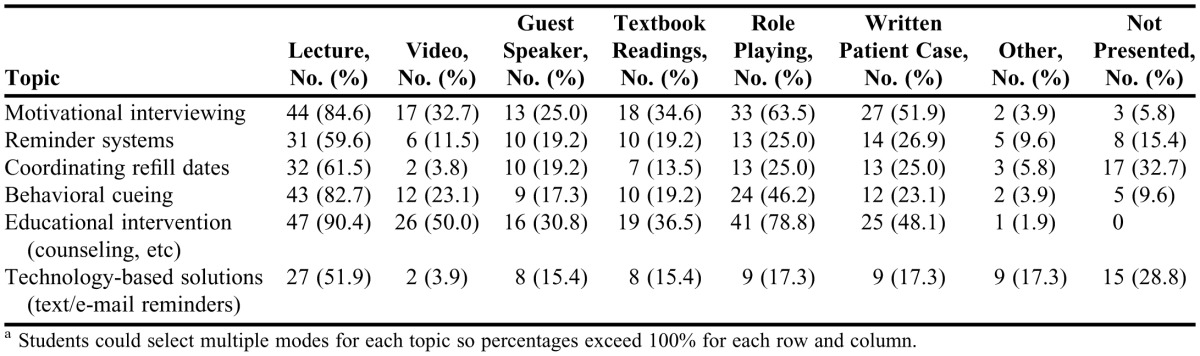
Table 2 shows the frequencies at which adherence topics are covered. Lecture was a common mode of instruction for all medication adherence topics. Motivational interviewing and educational intervention concepts were largely taught through role playing, written patient cases, videos, textbook readings, and guest speakers. Reminder systems and coordinating refill dates were largely taught through lecture, written patient cases, and role playing. Almost a third of the sample had not been taught how to coordinate refill dates. Behavioral cueing was largely presented via lecture, role playing and written patient cases. Technology-based solutions were primarily presented in lectures and about 29% of the sample indicated the topic was not presented at their college or school of pharmacy.
Table 2.
Modes of Teaching Medication Adherence Concepts in the Pharmacy Curriculum (n = 52)a
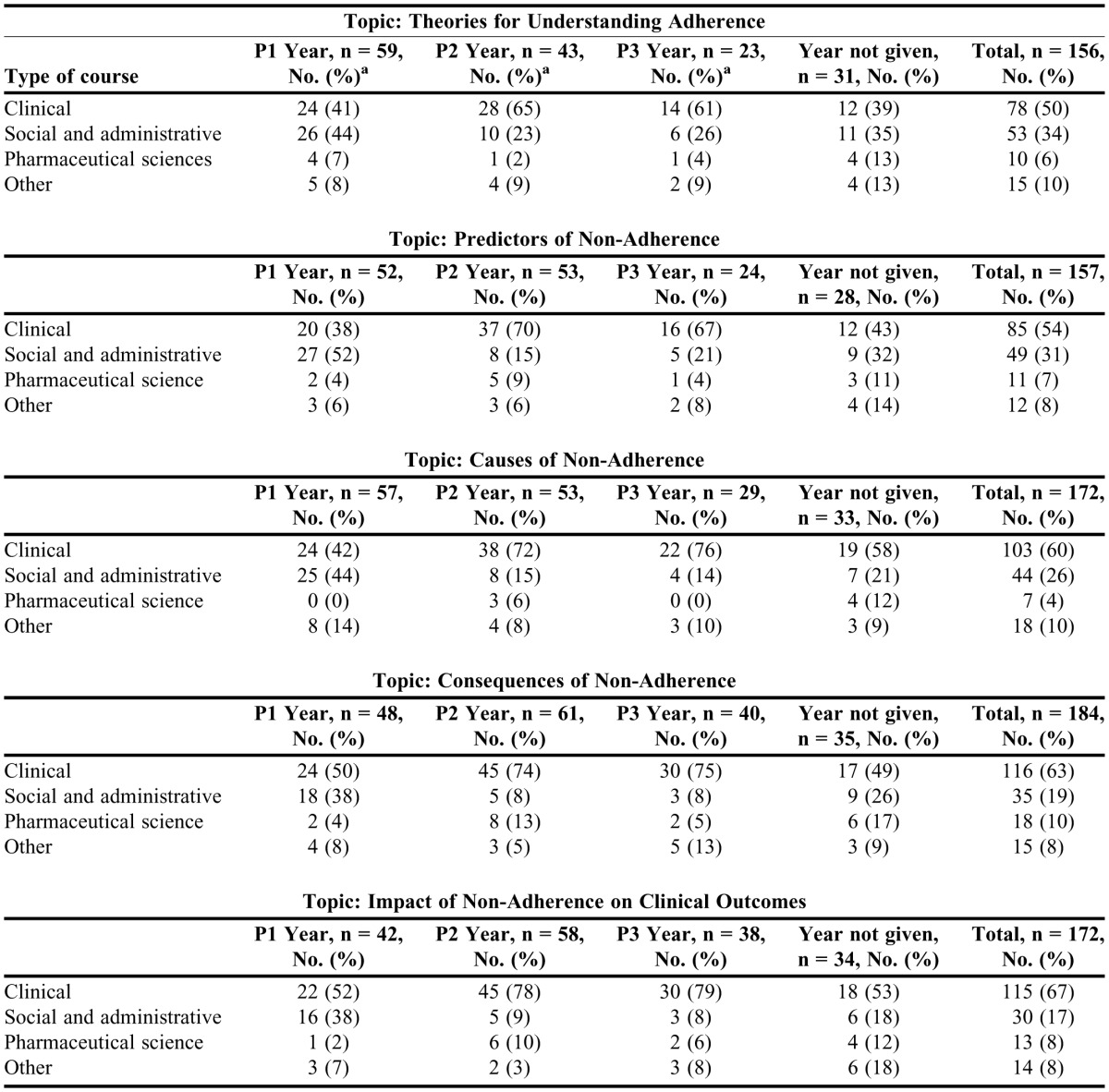
Table 3 shows responses to open-ended questions regarding which courses in the curriculum taught the adherence topics. Background adherence topics and the impact of medication adherence on clinical outcomes were presented mostly in clinical and social and administrative courses, with some content covered in pharmaceutical science and other courses throughout the curriculum. Examples of courses in which background concepts on adherence were taught are: Therapeutics/Pharmaceutical Care, Health Care Systems, Psychosocial Aspects of Health Care, Communications, and other courses on medication safety and self-care therapeutics. During the first year (P1), the majority of students were exposed to background topics on medication adherence in clinical and social administrative courses. During the P2 and P3 years, students were exposed to background topics on medication adherence mainly in their clinical courses.
Table 3.
Types of Courses in Which Medication Adherence Topics Were Covered in the Doctor of Pharmacy Curriculum According to Pharmacy Students
Almost 50% of students indicated that during their IPPEs, they had the opportunity to identify non-adherent patients and plan an intervention. Some students (13.5%) indicated that during their IPPEs they had the opportunity to identify non-adherent patients but not to perform an intervention. Other students (13.5%) reported they had the opportunity to intervene and follow-up on patients. Approximately 11.5% of the sample indicated they had no opportunity to do adherence-related activities during their IPPEs. The remainder of respondents indicated the question was not applicable or their experience did not fit in any of the categories. Using a coding scheme of 1 = no opportunity, 2 = identified non-adherent patient but could not determine intervention, 3 = identified non-adherent patient and planned intervention, and 4 = intervened and followed up with patient, the mean score on this item was 2.7 ± 0.9.
Only about 12% of the respondents were in their fourth year, thus, 50% of the sample indicated that the question was not applicable to them or that they had no opportunity to do adherence-related activities during their APPEs. Fifty percent reported participating in some medication adherence activities during APPEs. Of the 50% who responded, more than half (27%) indicated they had APPEs in which they had the opportunity to intervene and follow-up with patients. Approximately 21% indicated they could identify non-adherent patients; however, 11.5% of these individuals indicated they had identified non-adherent patients and planned an intervention, while the remainder (9.6%) had not planned an intervention. Using the same coding scheme, the APPE mean for this question was 3.2 ± 1.0.
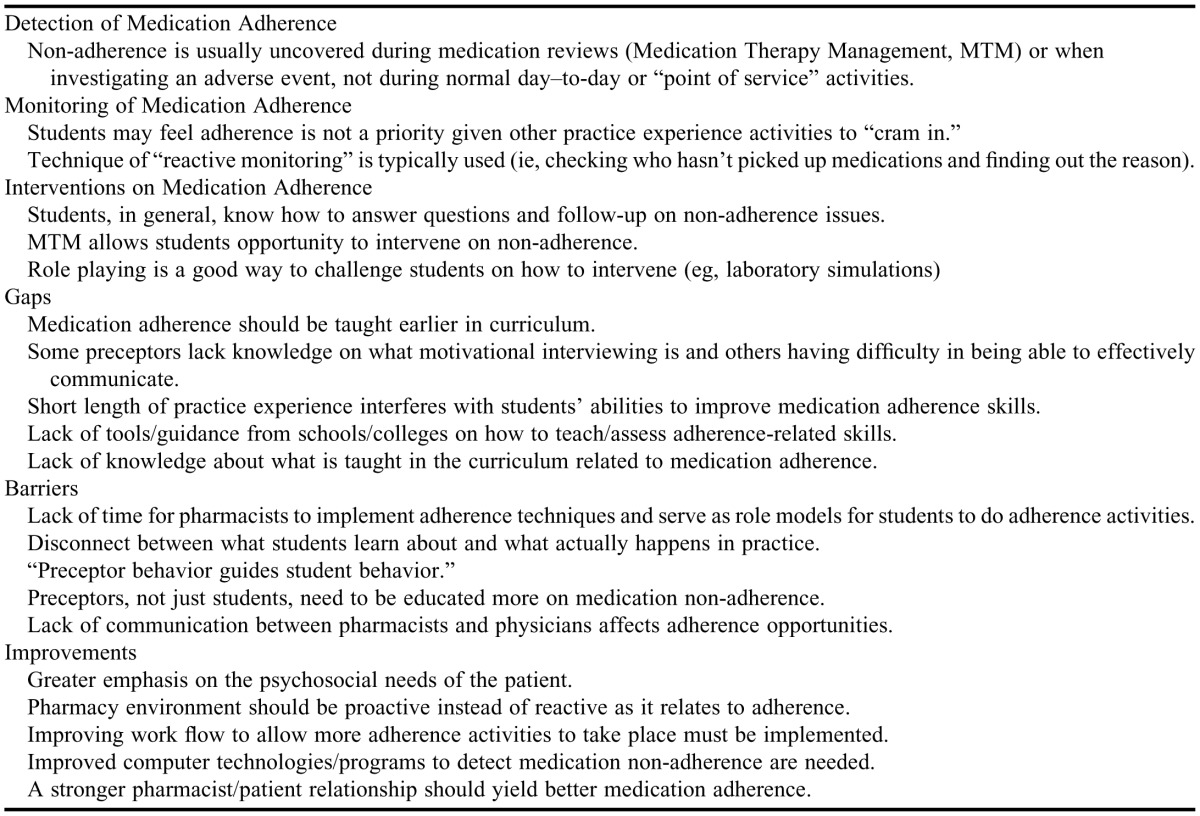
Table 4 lists the general themes that arose during the telephone conversations with the 3 preceptors. While most points reflected concerns about students’ educational experiences while on an APPE, some of the comments reflected on the broader challenges faced by community pharmacists to more fully and consistently care for their patients. Preceptors indicated consistent medication monitoring could yield opportunities to detect medication non-adherence but this was not seen as a priority for students and preceptors given the time constraints associated with point-of-service care and other practice experience activities. Preceptors, in general, believed that students have the skills to handle patient questions and follow-up on medication non-adherence, but do not have enough time to improve their skills given the short length of practice experiences.
Table 4.
Summary of Preceptor Comments From Telephone Interviews (N = 6)
The preceptors felt they lacked knowledge about the medication adherence curriculum taught to students in the classroom such as key interventions and communication approaches to improve adherence. They expressed a need for greater communication with colleges and schools on how to teach and assess medication adherence-related skills and how to make learning in the classroom optimally reflect the realities of practice. Preceptors felt their lack of education and time to do adherence interventions was not serving as a good model for students on how to engage in adherence interventions. They suggested that better computer technology and workflow designs could assist pharmacists and students in more consistently and proactively detecting, monitoring, and intervening on medication non-adherence.
The 3 faculty members who were interviewed agreed that background topics on medication adherence are important and should be integrated throughout the PharmD program, both in required and elective courses. This integration could be achieved through the development of active-learning techniques such as role-playing exercises. One faculty member highlighted the value of pharmacy faculty members joining students on practice experiences to facilitate and support medication adherence principles. Faculty members also indicated the need for better balance in the curriculum on instructing students to think about patients at both the individual and population levels. From their perspective, barriers to the development of a national pharmacy curriculum on medication adherence are resources and curriculum flexibility. Two solutions that were suggested were to implement adherence concepts and applications into a structured component of the experiential program and to create more efficiency in how adherence topics are interwoven in the curriculum.
DISCUSSION
This investigation used multiple data sources to assess and describe the nature and extent of medication adherence education and experiential training in US colleges and schools of pharmacy. This is the first known study to attempt to understand the depth and breadth to which pharmacy students are trained in understanding and intervening on medication non-adherence. There were several key findings. First, 90% of the respondents in the national study indicated that adherence topics were a required part of their college or school’s curriculum, Although this suggests that these institutions were covering the topic in some form, the survey instrument did not explore what specific adherence topics were covered and how consistently they were taught throughout the curriculum. However, the student surveys conducted by the NCPA Advisory Council on Medication Adherence as part of this study provided some answers to these questions.
Our second key finding was that there is a gap in the medication adherence instruction covered in colleges and schools of pharmacy. While a majority of students reported that many adherence topics related to the nature and extent of the problem (models for understanding adherence, predictors, causes, and consequences of medication non-adherence, and impact of medication adherence on clinical outcomes) were moderately or extensively taught in their program, there was a large percentage of students who reported either not being taught or being only somewhat exposed to different adherence intervention strategies. This suggests that the adherence instruction that the colleges and schools of pharmacy in the WesternU survey reported covering is primarily background information on the medication adherence problem. Educational interventions and motivational interviewing are the only intervention strategies to which students reported having been moderately or extensively exposed (ie, counseling patients on their medications). This lack of intervention training may contribute to why, on average, there was a mix of respondents who had the opportunity to plan and follow-up on an adherence intervention during their IPPEs and APPEs.
The gap noted in the education of pharmacy students about conducting medication adherence interventions demonstrates the need for colleges and schools of pharmacy to develop national standards for medication adherence education and a toolbox of curricular content to help in the consistent and integrated implementation of those standards. During the phone interviews, a faculty member suggested that an adherence toolbox that would teach a set of principles and encourage faculty members to apply the principles in various courses using different instructional modes should be developed. Faculty members and preceptors could use these tools to train both students and practitioners on key adherence strategies. WHO first stated the urgent need for an adherence counseling toolkit that is adaptable for different socioeconomic settings in 2003.1 It is difficult to envision pharmacists as part of a multidisciplinary solution to improve medication adherence that is prepared for future industry requirements if they are not adequately equipped with effective strategies to resolve patient barriers to adherence.
The third and fourth key findings emerged during the telephone interviews with community pharmacy preceptors and pharmacy faculty members. The third key finding was that preceptors reported not feeling entirely well informed about medication adherence interventions themselves, being inadequately informed on what students know about medication adherence, and lacking the educational tools to consistently facilitate adherence detection, monitoring, and intervention. They expressed the need for greater guidance from colleges and schools of pharmacy on how to teach and assess adherence-related skills. One faculty member expressed similar concerns and suggested pharmacy faculty members needed to be more involved in the experiential learning of students, such as coming to experiential sites and showing applications of concepts taught in the classroom.
Preceptors faced challenges in consistently facilitating adherence-related activities during practice experiences, such as time constraints and other realities of daily practice. Because of these limitations, they were concerned that they were not modeling ideal adherence promotion behaviors for students. If students do not see preceptors consistently and effectively detecting, monitoring, and intervening on medication non-adherence, they may perceive these activities as not as critical as others and be less inclined to engage in them. The findings from the conversations with the preceptors provide additional evidence that students appear to be inadequately and inconsistently exposed to intervention strategies for medication non-adherence, both in the classroom and experiential settings.
Given the significant impact of medication adherence on the lives of patients and the severity of the medication non-adherence problem, pharmacy education groups must come together and ensure a common thread is woven throughout curriculum and national curriculum standards. The authors suggest that ACPE give strong consideration to the addition of language and content in the PharmD accreditation standards regarding adherence concepts and tools as part of their curriculum and IPPE/APPE experiences. Such language would facilitate a national effort toward consistency in medication adherence knowledge and behaviors that will better prepare students to address non-adherence in practice.
There are a few limitations to this investigation. To improve response rates among students in the project conducted by the NCPA Advisory Committee, multiple efforts were made to extend the deadline for survey instrument completion and an incentive for participation was offered. Future research could determine if a larger representation of students across more colleges and schools of pharmacy would yield findings similar to those of the present study. Also, the study involved a small convenience sample of preceptors and faculty members. Because of these 2 limitations, we may not be able to generalize our findings to other colleges and schools of pharmacy. A future study involving more preceptors and faculty members could be conducted to confirm our findings. We are uncertain as to the accuracy of the student data because of possible poor recall of content covered in past years. In recalling past events (especially events that occurred over several years), respondents may have underestimated or overestimated the coverage of an adherence topic. We also encouraged students to consult with students enrolled in later years of the program in hopes that their input would result in a more comprehensive response that more accurately represented the respondent’s college or school of pharmacy. While the current research asked students to report the degree to which they were exposed to a topic, a future study could assess what students actually know about the background on medication adherence and interventions to use with non-adherent patients. While the brief survey instrument was field tested for face and content validity among a group of students prior to administration, there is the possibility that survey items may not have been clear, leading to some misinterpretation of what was being requested.
CONCLUSIONS
While the pharmacy curriculum covers the concepts of medication adherence to some extent, students are at best only somewhat exposed to intervention strategies, making application of key adherence strategies a significant deficiency in pharmacy students’ educational experience. Our findings suggest that the following action steps are necessary to embed adherence as a core competency in pharmacy school curriculum and ensure its application in practice: integrating medication adherence concepts and interventions throughout the curriculum and experiential education, embedding medication adherence education into national standards for pharmacy education, and developing a toolkit that is a national resource for students and preceptors on adherence intervention strategies. These steps are critical to prepare future pharmacists to actively detect, monitor, and intervene in cases of medication non-adherence.
ACKNOWLEDGMENTS
The authors would like to thank Professors Jon Schommer, Dale Christensen, and Todd Brown, and several community pharmacy preceptors for their helpful comments during the data collection process.
REFERENCES
- 1.Sabaté E. World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. [PubMed] [Google Scholar]
- 2.Sackett D, Haynes R, editors. Compliance with Therapeutic Regimens. Baltimore, MD: John Hopkins University Press; 1979. [Google Scholar]
- 3.Avorn J, Monette J, Lacour A, et al. Peristence of use of lipid-lowering medications- a cross-national study. JAMA. 1979;279(18):1458–1462. doi: 10.1001/jama.279.18.1458. [DOI] [PubMed] [Google Scholar]
- 4.Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288(4):1455–1461. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- 5.Solomon DH, Avorn J, Katz JN, et al. Compliance with osteoporosis medications. Arch Intern Med. 2005;165(20):2414–2419. doi: 10.1001/archinte.165.20.2414. [DOI] [PubMed] [Google Scholar]
- 6.Grymonpre R, Mitenko P, Sitar D, Aoki F, Montgomery P. Drug-associated hospital admissions in older medical patients. J Am Geriatr Soc. 1988;36(12):1092–1098. doi: 10.1111/j.1532-5415.1988.tb04395.x. [DOI] [PubMed] [Google Scholar]
- 7.Maronde R, Chan L, Larsen F, Strandberg L, Laventurier M, Sullivan S. Underutilization of antihypertensive drugs and associated hospitalization. Med Care. 1989;27(12):1159–1166. doi: 10.1097/00005650-198912000-00007. [DOI] [PubMed] [Google Scholar]
- 8.National Council on Patient Information and Education (NCPIE) Talk About Prescriptions Month Newsletter. Washington, DC: National Council on Patient Information and Education; 1990. [Google Scholar]
- 9.Prince B, Goetz C, Rihn T, Olsky M. Drug-related emergency department visits and hospital admissions. Am J Hosp Pharm. 1992;49(7):1696–1700. [PubMed] [Google Scholar]
- 10.Sokol M, McGuigan K, Verbrugge R, Epstein R. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2008;43(6):521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 11.New England Healthcare Institute (NEHI) Thinking Outside of the Pillbox: A System-Wide Approach to Improving Patient Medication Adherence for Chronic Disease. Cambridge, MA: New England Healthcare Institute; 2009. [Google Scholar]
- 12.Script Your Future. National Consumers League. http://www.nclnet.org/health/106-prescription-drugs/234-ncls-medication-adherence-campaign. Accessed November 25, 2011.
- 13.National Council on Patient Education and Information (NCPIE) Enhancing prescription medication adherence: a national action plan. http://www.talkaboutrx.org/documents/enhancing_prescription_medicine_adherence.pdf. Accessed May 18, 2018.
- 14.Pharmacy Quality Alliance. Measures. http://www.pqaalliance.org/measures.htm. Accessed April 30, 2012.
- 15.Kimberlin CL. Communicating with patients: skills assessment in US colleges of pharmacy. Am J Pharm Educ. 2006;70(3):Article 67. doi: 10.5688/aj700367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Accreditation standards and guidelines for the professional program leading to the doctor of pharmacy degree. Accreditation Council on Pharmacy Education. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed April 30, 2012.
- 17.Educational outcomes. 2004 Center for the Advancement of Pharmaceutical Education, American Association of Colleges of Pharmacy. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed May 18, 2012. [Google Scholar]
- 18.NABP mission statement. National Association of Boards of Pharmacy (NABP). http://www.nabp.net/about/. Accessed April 30, 2012.
- 19.NAPLEX blueprint. National Association of Boards of Pharmacy (NABP). http://www.nabp.net/programs/examination/naplex/naplex-blueprint/. Accessed April 30, 2012.
- 20.Academic pharmacy’s vital statistics. American Association of Colleges of Pharmacy (AACP). http://www.aacp.org/about/Pages/Vitalstats.aspx. Accessed April 30, 2012.