Abstract
Objective. To assess the extent to which US colleges and schools of pharmacy are incorporating interprofessional education into their introductory pharmacy practice experiences (IPPEs), and to identify barriers to implementation; characterize the format, structure, and assessment; and identify factors associated with incorporating interprofessional education in IPPEs.
Methods. An electronic survey of 116 US colleges and schools of pharmacy was conducted from March 2011 through May 2011.
Results. Interprofessional education is a stated curricular goal in 78% of colleges and schools and consistently occurred in IPPEs in 55%. Most colleges and schools that included interprofessional education in IPPEs (70%) used subjective measures to assess competencies, while 17.5% used standardized outcomes assessment instruments. Barriers cited by respondents from colleges and schools that had not implemented interprofessional education in IPPEs included a lack of access to sufficient healthcare facilities with interprofessional education opportunities (57%) and a lack of required personnel resources (52%).
Conclusions. Many US colleges and schools of pharmacy have incorporated interprofessional education into their IPPEs, but there is a need for further expansion of interprofessional education and better assessment related to achievement of interprofessional education competencies in IPPEs.
Keywords: interprofessional education, interdisciplinary education, introductory pharmacy practice experiences, experiential education
INTRODUCTION
Interprofessional education is an essential component of the Institute of Medicine's recommendations for improving healthcare professions education.1 Despite formal recommendations supporting interprofessional education, successful development and implementation are challenging.2-5 Barriers include limited access to other health care disciplines, lack of adequate clinical training sites, lack of a faculty member to champion interprofessional education, lack of administrative support, insufficient resources for faculty development, lack of standardized assessment instruments, and attitudinal differences and scheduling conflicts among the participating disciplines.
As a result of the 2011 updates to the learning outcomes in the Accreditation Council for Pharmacy Education (ACPE) Accreditation Standards and Guidelines,6 the development and implementation of meaningful interprofessional education experiences has become a priority in many pharmacy education programs nationwide. Educators cannot assume that students will develop an appreciation of the differences among healthcare disciplines by simply training or working in the same patient care environment, simulation center, or skills laboratory. Interprofessional education must be an intentional collaborative effort among faculty members and students from multiple disciplines with the goal of training healthcare professionals to work as teams to ensure optimal patient-centered care.
Approaches to interprofessional education and the timing of interprofessional education in the pharmacy curriculum vary considerably among colleges and schools of pharmacy. For example, interprofessional education might include activities such as introductory seminars, a formal convocation event for all entering health science students, lecture-based courses, student-operated primary care assessment clinics for the underserved, a research training program, and/or an interprofessional objective structured clinical examination.7 The environment in which interprofessional education is offered at colleges and schools of pharmacy varies and usually depends on the setting, ie, some colleges and schools reside on campuses with multiple health professions training programs in an integrated academic health center, while others are standalone programs that may not be affiliated with a hospital or medical center. Interprofessional education activities can include multiple professions (eg, pharmacy, medicine, nursing, etc) and occur both early and late in health professions training. Interprofessional education has focused on the latter years of the pharmacy curriculum, and has been delivered primarily through advanced pharmacy practice experiences (APPEs). However, the 2006-2007 Professional Affairs Committee of the American Association of Colleges of Pharmacy (AACP) recommended that interprofessional education should occur in a variety of settings, including IPPEs.8
All US colleges and schools of pharmacy are required by ACPE to provide IPPEs,6 and these experiences represent one of the first opportunities to integrate interprofessional education in the pharmacy curriculum. It is unclear how commonly and in what form interprofessional education is being incorporated in IPPEs in colleges and schools of pharmacy. The primary objective of this study was to determine the extent to which interprofessional education occurs in IPPEs. Secondary objectives were to identify barriers to implementation; to characterize the format, structure, and assessment of interprofessional education in IPPEs; and to identify factors associated with colleges and schools incorporating interprofessional education in IPPEs.
METHODS
This project was developed as a component of AACP’s Academic Leadership Fellows Program. Institutional review board (IRB) approval was obtained from the IRB committees at the investigators’ institutions. An electronic survey instrument was developed to assess the extent to which US colleges and schools of pharmacy were incorporating interprofessional education into their IPPEs. The survey instrument was pretested at the investigators’ home institutions prior to dissemination. The survey data for this paper were collected and analyzed using the Qualtrics Research Suite (Qualtrics Labs, Inc., Provo, UT). A complete description of the survey instrument and a flowchart are available from the authors.
In December 2010, a pre-invitation e-mail to participate in the survey was sent to the director of experiential education at each of the 116 US colleges and schools of pharmacy that had obtained, at minimum, pre-candidate status as defined by ACPE.9 This pre-invitation alerted these individuals that they would be receiving a survey invitation in the near future and confirmed that all contacts’ e-mail addresses were correct. A second e-mail asking recipients to participate in the survey and containing a unique link to the survey instrument was sent in March 2011. Although participants’ responses were anonymous, the online survey system allowed investigators to identify and send reminder e-mails to non-responders. To improve the response rate, individuals who had not responded after multiple e-mail reminders had been sent were contacted by phone in mid-April 2011 and encouraged to participate. The survey was closed in late May 2011. In compliance with IRB requirements, respondents could elect to quit the survey process at any time or not answer 1 or more questions on the survey instrument.
A split logic survey design was used to stratify colleges and schools based on the survey question: “Does your school/college of pharmacy consistently incorporate interprofessional education into your IPPEs?” This survey question included the following definition of interprofessional education and provided a reference for the definition: “An educational approach in which two or more disciplines collaborate in the teaching-learning process with the goal of fostering interdisciplinary/interprofessional interactions that enhance the practice of both disciplines.”2
Colleges that indicated that they incorporated interprofessional education into their IPPEs were directed toward survey questions designed to gather information related to the structure and format of these IPPEs, such as whether the IPPE was a required or elective course, the format(s) of the IPPE, what other professions were involved as faculty members and students, whether there was an orientation prior to the IPPE, and the type(s) of student assessment used. The survey instrument also asked the respondents from these colleges and schools whether consistent incorporation of interprofessional education in IPPEs had involved any specific faculty development, or a champion in the faculty or administration.
Colleges and schools that indicated that they did not consistently incorporate interprofessional education into IPPEs were directed toward survey questions intended to identify possible barriers to implementation and resources that might be needed to implement interprofessional education in IPPEs. Demographic information about each college and school was obtained to help characterize differences between the colleges and schools that were incorporating interprofessional education into IPPEs and those that were not.
Data were summarized descriptively with means, frequencies, and percentages. Because all US colleges and schools were contacted and 82% responded, differences were deemed to be meaningful reflections of the environment for pharmacy education, so it was not necessary to focus on significant differences. However, p values for statistical tests are reported. Additionally, exploratory statistical analyses looking at factors related to having interprofessional education in IPPEs were completed. These analyses looked at the relationship between college and school characteristics and whether interprofessional education was included in IPPEs, using chi-square statistics to compare colleges and schools with interprofessional education in IPPE to those without interprofessional education in IPPE. Comparisons were made in terms of public or private, years established (< 2 years, 2-10 years, 11-20 years, > 20 years), number of students per class (< 100 students, 100-150 students, > 150 students), and number of professions on campus (2-3 professions, 4-6 professions, > 6 professions).
RESULTS
Ninety-five colleges and schools responded to the survey instrument, resulting in an 82% response rate. One college refused to complete the survey instrument and some respondents did not complete all questions. Forty-two (44%) private colleges and schools and 53 (56%) public colleges and schools responded. Approximately 65% of the responding colleges and schools were established more than 20 years ago. Interprofessional education was a stated curricular goal in 78% of the colleges and schools. Eight colleges and schools had no other health professions training programs represented on their campus, while 4 reported having more than 10 other health profession education programs on campus.
Characteristics of Colleges and Schools That Incorporate Interprofessional Education into IPPEs
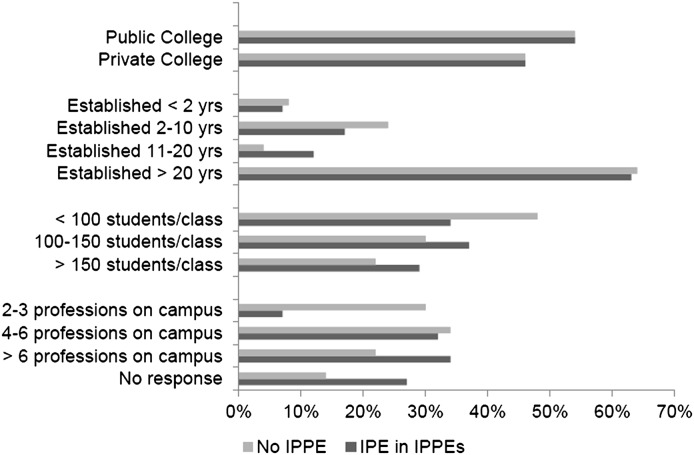
Of the 95 respondents who started the survey instrument and answered the first several survey questions, only 91 answered the question regarding whether their college consistently incorporated interprofessional education into IPPEs. Fifty (55%) respondents reported having interprofessional education in IPPEs at their colleges and schools, while 41 (45%) reported their colleges and schools did not currently have interprofessional education consistently incorporated into IPPEs. A difference was not observed in any of the characteristics of colleges and schools that reported having interprofessional education in their IPPEs compared with those that did not (Figure 1 and Table 1). Private and public colleges and schools were equally likely to have interprofessional education in IPPEs, and no differences were observed in colleges and schools that had been established for more than 20 years or less than 2 years (Figure 1). Some trends were observed, such as colleges and schools that had been established for 2-10 years were somewhat less likely to incorporate interprofessional education in their IPPEs, whereas colleges established for 11 to 20 years were more likely to incorporate interprofessional education in their IPPEs. Colleges and schools with fewer than 100 students per class were less likely to have interprofessional education in their IPPEs, while colleges and schools with more than 100 students per class were more likely to have interprofessional education in their IPPEs (Figure 1).
Figure 1.
Demographics based on offering of interprofessional education (IPE) in introductory pharmacy practice experiences (IPPEs). No significant differences were found between the number of colleges and schools with IPE in IPPEs and the number with no IPE in IPPEs (P > 0.05).
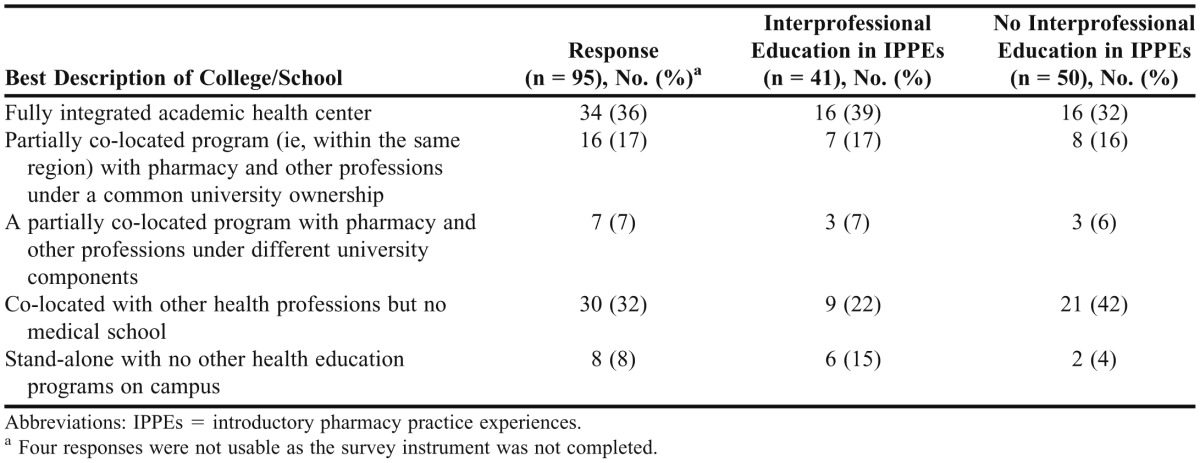
Table 1.
Incorporation of Interprofessional Education into Introductory Pharmacy Practice Experiences According to the Presence of Other Health Profession Educational Programs on Campus
Colleges and schools with more than 6 health professions education programs on campus were more likely to have interprofessional education in their IPPEs, whereas colleges and schools with 2 to 3 on campus were less likely. There were 19 colleges and schools that did not respond to the question regarding how many other health education professions education programs were on the same campus. Eight of these 19 were standalone colleges or schools of pharmacy with no other health professions education programs on campus. The 19 colleges that did not indicate how many other health professions education programs were on the same campus were more likely to have incorporated interprofessional education in their IPPEs. Table 1 shows that the 8 standalone colleges and schools with no other health professions education programs on campus were more likely to have interprofessional education in their IPPEs. Colleges and schools described as co-located with other health professions but not with a medical school were much less likely to have interprofessional education in their IPPEs (Table 1). However, colleges and schools of pharmacy that were educational components of a fully integrated academic health center were only modestly more likely to have interprofessional education in their IPPEs.
The non-pharmacy disciplines most likely to be involved as faculty members and students in IPPEs that incorporated interprofessional education were medicine and nursing, followed by physician assistants and other healthcare professions (Table 2). Other healthcare professions included public health, veterinary medicine, optometry, occupational therapy, chiropractics, dietetics, and others. Survey results indicate that more than two-thirds (n = 28, 68%) of IPPEs with interprofessional education included interactions with 2 or more other professions as students or faculty members, and 39% (n = 16) included interactions with 3 or more professions (Table 3).
Table 2.
Disciplines Involved With Interprofessional Education in Introductory Pharmacy Practice Experiences (N = 41)a
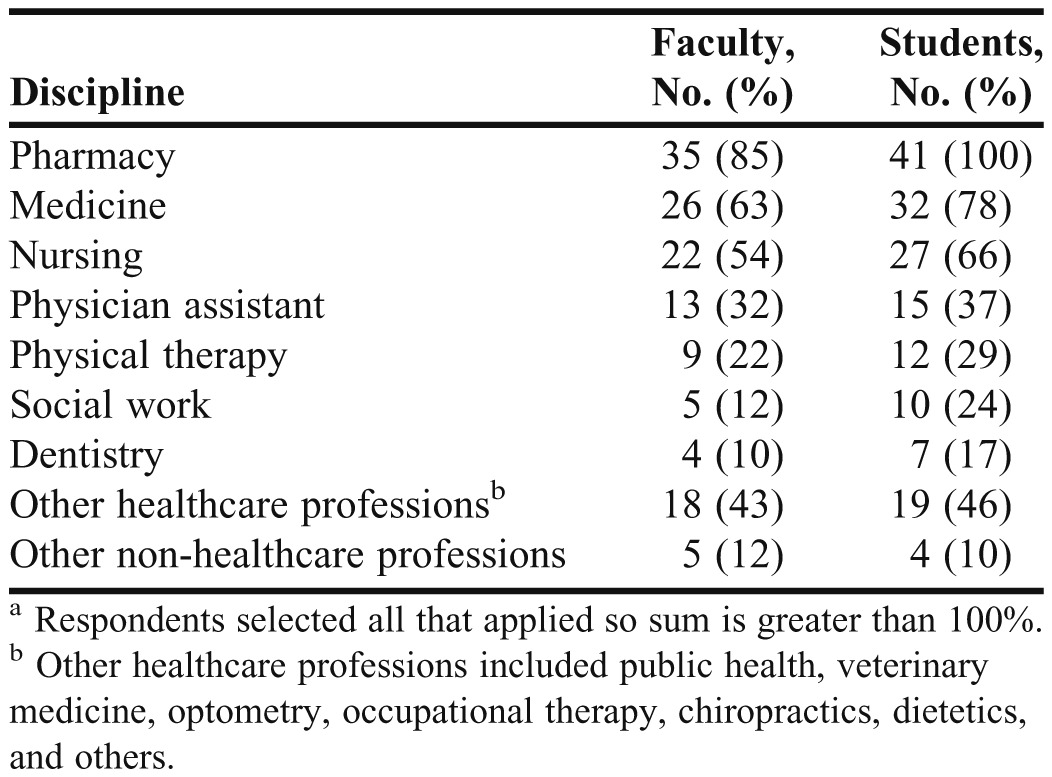
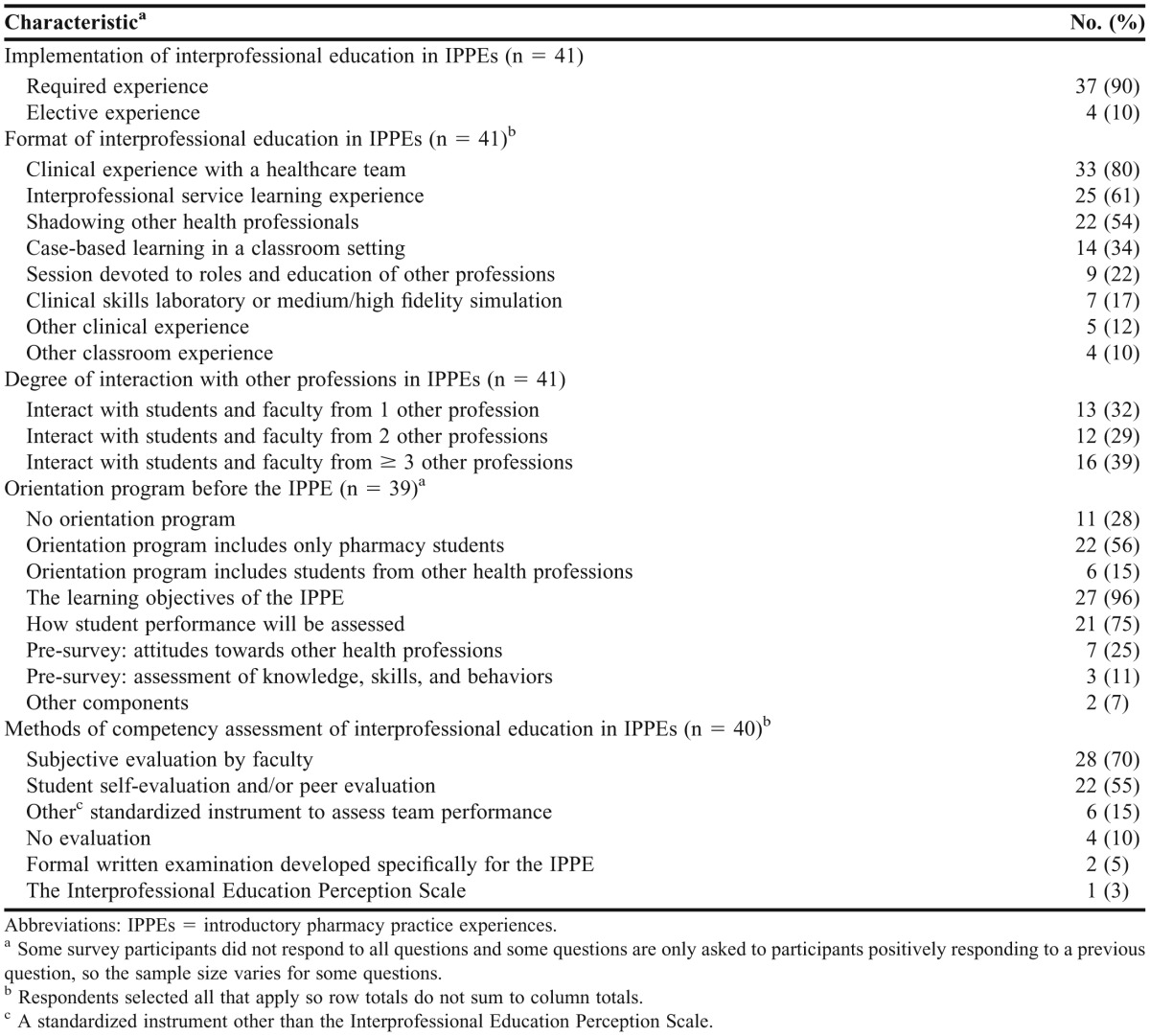
Table 3.
Structure, Scope, Orientation, and Assessment of Interprofessional Education in Introductory Pharmacy Practice Experiences at US Colleges and Schools
Structure, Scope, Orientation, and Assessment of Interprofessional Education in IPPEs
The survey instrument included questions regarding the structure, scope, orientation, and assessment of interprofessional education for the 41 colleges that indicated they consistently incorporated interprofessional education into IPPEs (Table 3). The majority of colleges and schools (90%) indicated that the IPPE that incorporated interprofessional education was a required experience. There were a range of interprofessional education formats with actual clinical experience with a healthcare team being the most common (80%), followed by interprofessional service learning (61%), shadowing other health professionals (54%), and case-based learning in a classroom setting (34%). Less common formats included classroom sessions devoted to roles and education of other professions (22%), clinical skills laboratories or simulations (17%), or other clinical or classroom experiences.
Nearly three-fourths of the respondents (72%) indicated that the IPPE in which interprofessional education was taught included an orientation program, though only a small percentage (15%) indicated that the orientation included students from health professions other than pharmacy (Table 3). Most colleges provided an orientation to the IPPE that included a description of the learning objectives (96%) and assessment methods (75%), but relatively few included a pre-IPPE survey of students' attitudes towards other professions (25%) or assessment of knowledge, skills, and behaviors relevant to interprofessional interactions, such as the Readiness for Interprofessional Learning Scale (RIPLS, 11%).10 Few respondents (3%) indicated using a standardized assessment instrument such as the Interprofessional Education Perception Scale11 (IEPS), a formal written examination developed specifically for the IPPE (5%), or other standardized instruments to assess team performance (15%). Most respondents used subjective assessments by faculty members (70%) or students (55%) as part of the competency assessment methods for the IPPE, and a small number of respondents (10%) used no form of evaluation.
Barriers to Implementation of Interprofessional Education in IPPEs
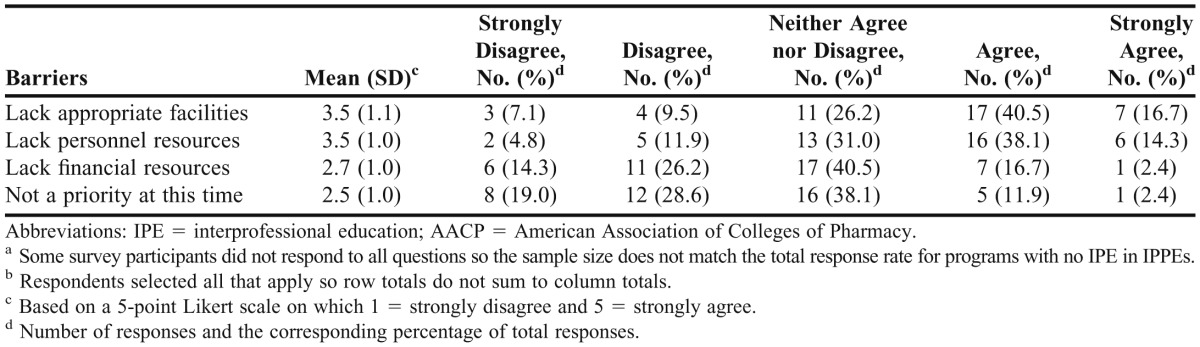
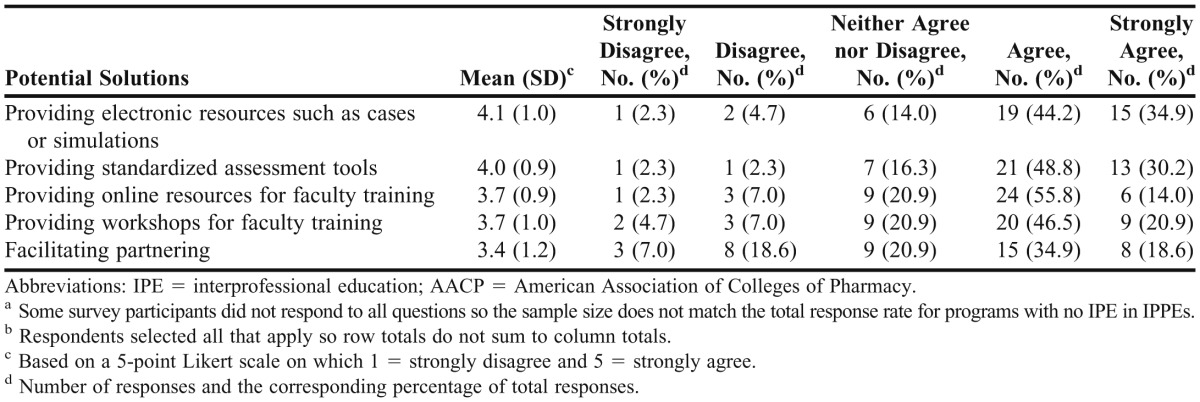
The survey instrument was designed to collect information regarding barriers to implementation from the respondents who answered that they were not consistently incorporating interprofessional education into IPPEs (Table 4). These respondents were also asked questions regarding the ways that AACP might assist with implementation of interprofessional education in IPPEs (Table 5). The most common barriers to implementation of IPPEs with interprofessional education were lack of access to a sufficient number of healthcare facilities with interprofessional education opportunities (57% agreed or strongly agreed) and the lack of required personnel resources (52% agreed or strongly agreed). Less than 20% of the respondents considered lack of required financial resources to be a barrier. A similar percentage of respondents indicated that interprofessional education in IPPEs was not a high priority at this time. The survey instrument allowed respondents to provide information regarding other barriers to implementation as free text responses. Seven respondents indicated that their institutions were in the early phases of implementing interprofessional education in IPPEs. Nine respondents indicated that there were logistical problems to implementation such as the structure of their IPPEs, time constraints, limited access to other health professions on campus, and limited interest from other healthcare education programs. Table 4 summarizes the resources that respondents thought would be useful in implementing interprofessional education in their IPPE programs. A large percentage suggested that AACP might assist implementation by providing electronic resources such as case-based studies and simulations (79%), standardized assessment instruments (79%), online resources for faculty training (70%), workshops for faculty training (67%), and by facilitating partnering with other healthcare education programs (54%).
Table 4.
Barriers to Implementation for US Pharmacy Programs That Have Not Incorporated Interprofessional Education into Introductory Pharmacy Practice Experiences (N = 42)a,b
Table 5.
Potential Solutions to Implementation for Programs That Have Not Incorporated Interprofessional Education Into Introductory Pharmacy Practice Experiences (N = 43)a,b
Factors Facilitating Interprofessional Education in IPPEs
The survey instrument was used to identify critical factors that may facilitate overcoming barriers to implementation of interprofessional education in IPPEs. Fifty-six percent of the respondents (n = 23) whose college or school consistently incorporated interprofessional education into IPPEs indicated their institutions had an administrative or faculty champion who has been critical in partnering programs. This person was often an upper-level administrator (87%) and/or faculty member (65%) in the college or school of pharmacy rather than an upper-level administrator in the academic health center (17%) or other health education program (22%), or a faculty member in another health education program (9%). Most institutions that incorporated interprofessional education into IPPEs did not have faculty development programs to support or reward faculty members participating in interprofessional education (90%).
DISCUSSION
The complexity of the health care system requires that professionals from a wide range of disciplines work together to care for patients. Undoubtedly, pharmacy students in every US college and school of pharmacy encounter physicians, medical students, nurses and nursing students, and other health professionals during practice experiences. Nevertheless, simply working together does not necessarily provide insight into the roles, responsibilities, and perspectives of others, nor does it always provide the development of skills needed to effectively communicate and work as a team. Interprofessional education should involve direct interactions that foster collaboration and interprofessional interactions to improve the practice of each discipline. Insight into the roles and responsibilities of other professions should help pharmacy students better understand how they can and should fit into new and expanded patient care roles. These abilities may be developed through a variety of learning opportunities, including IPPEs.
As pharmacy education has incorporated practice experiences throughout the curriculum, it makes sense that interprofessional education should be a part of IPPEs. Nevertheless, the extent to which this is occurring has not been previously described. More than half of the colleges and schools that responded to this survey had incorporated interprofessional education into IPPEs, while others were in the planning stages. The age or size of the college or school did not appear to have influenced their ability to develop early interprofessional education experiences. Perhaps the accreditation requirements for enhanced interprofessional education in the pharmacy curriculum will provide the impetus for all colleges and schools of pharmacy to incorporate interprofessional education into IPPEs as a part of these expanded experiences.
Colleges and schools of pharmacy in the United States operate in a variety of settings. Buring and colleagues describe 5 models for pharmacy colleges and schools based on their association with other healthcare educational programs.12 In 2009, only 31 pharmacy colleges and schools were situated in an academic health center; our survey had 34 colleges that indicated they were associated with a fully integrated academic health center. While this setting would be expected to be the most likely to foster interprofessional activities, this was not the case with regard to IPPEs. Moreover, the number of health professions located on the same campus was not a factor in the development of interprofessional education in IPPEs. Three-fourths of the colleges and schools without other health professions on their campuses were incorporating interprofessional education into IPPEs. While this may seem counterintuitive, these standalone colleges may have needed to be proactive in their development of interprofessional education or in the development of educational partnerships with nearby healthcare educational programs. It will be important to explore the approaches used by these colleges and schools in future studies.
Assessment is an important component of education and is still evolving in the area of interprofessional education. Few programs included standardized assessments of interprofessional education in IPPEs. The most commonly used assessments for interprofessional education, RIPLS and IEPS, focus on student perceptions about their own professions, as well as other professions.10,11 With only 1 college indicating that the IEPS was used, increased use of standardized assessment instruments to measure the effectiveness of interprofessional experiences should be encouraged by the academy. An expert panel developed core competencies in 4 domains for interprofessional collaborative practice: values/ethics for interprofessional practice, roles/responsibilities, interprofessional communication, and teams and teamwork.13 These competencies had not been published at the time this survey was conducted; however, they highlight the ongoing evolution of interprofessional education. Methods for assessment of student development and achievement of these interprofessional competencies throughout the health science curricula are not well established and represent another area for future research in interprofessional education. The enhanced use of objective assessment of interprofessional education activities could facilitate the dissemination of knowledge related to best practices in this area and demonstrate the importance of interprofessional education in healthcare professional training. Workshops and programs on the implementation and assessment of interprofessional education in IPPEs offered by organizations such as AACP would likely catalyze expanded incorporation of these activities across healthcare education curricula.
For those colleges that have not yet implemented interprofessional education into their IPPE curriculum, it does not appear that it is because of a lack of interest. Only 6 colleges indicated that it was not a priority. Rather, respondents indicated the need for facilities and trained personnel were the greatest perceived barriers. These are among the major barriers previously described.2-5 However, there is also a demonstrated need for assistance by professional organizations such as AACP. Respondents reported needs in the areas of faculty and resource development, and cited the need for assessment instruments to facilitate the implementation of interprofessional education. While individual professions may work separately to promote the development of faculty members involved with interprofessional education, they must ensure that training of educators for interprofessional education occurs in collaboration with faculty members from other professions. A shared understanding of the content and process of interprofessional education is an important next step in facilitating widespread implementation of interprofessional education.13
As is common in survey research, a 100% response rate was not obtained. This precludes applying the results of our survey to all US colleges and schools of pharmacy without qualification. However, the approximately 80% response rate obtained does provide clear insights into the current state of interprofessional education in IPPEs and allows us to make a number of conclusions that can be applied to most colleges and schools of pharmacy. Accurate responses to questions regarding interprofessional education in IPPEs required that the respondent have extensive knowledge of the activities within and outside their college or school. Although directors of experiential education were the intended respondents and likely to be the most knowledgeable about the areas surveyed, someone other than the individuals invited may have been more knowledgeable regarding interprofessional education-related activities taking place at their institution. This might be the case with respondents who were relatively new to their position, and therefore, not fully aware of interprofessional education-related activities throughout the curriculum. Additionally, a small number of respondents reported that several survey questions were unclear; therefore, responses provided to those or other questions may not have accurately portrayed the situation at that college or school. “Survey fatigue” could also be a reason for lack of response to the survey invitation or to some survey items. Finally, the release of the 2011 ACPE Accreditation Standards and Guidelines that mandate the inclusion of interprofessional education into pharmacy curricula could have positively impacted the number of responses in the study that favored the use of interprofessional education in IPPEs.6
CONCLUSIONS
The incorporation of interprofessional education in IPPEs is a major curricular goal for most US colleges and schools of pharmacy. For those colleges and schools that are in the planning stages of implementation, the lack of appropriate facilities and personnel resources is a major barrier. Accordingly, upper-level administrative support and encouragement is deemed critical to facilitate the implementation of these activities. Although a considerable number of colleges and schools had incorporated interprofessional education into IPPEs, few used standardized assessment instruments to evaluate the curricular outcomes of these activities. The academy should encourage research and development of instruments to assess meaningful outcomes of interprofessional education in IPPEs to demonstrate the value of these early practice experiences in healthcare education.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the guidance and support of the AACP staff through the Academic Leadership Fellows Program for facilitating this work, specifically Dr. Robert A. Kerr and Mr. Bradford E. Miller. We also wish to thank the technical support staff at Qualtrics who provided valuable advice during the development of the survey instrument.
REFERENCES
- 1.Greiner AC, Knebel E, editors. Health Professions Education: A Bridge to Quality. A Report of the Committee on the Health Professions Education Summit, Institute of Medicine. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Page RL, Hume AL, Trujillo JM, et al. ACCP White paper: interprofessional education: principles and application. A framework for clinical pharmacy. Pharmacotherapy. 2009;29(3):145e–164e. [Google Scholar]
- 3.Buring SM, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009;73(4):Article 59. doi: 10.5688/aj730459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gardner SF, Chamberlin GD, Heestand DE, Stowe CD. Interdisciplinary didactic instruction at academic health centers in United States: attitudes and barriers. Adv Health Sci Educ Theory Pract. 2002;7(3):179–190. doi: 10.1023/a:1021144215376. [DOI] [PubMed] [Google Scholar]
- 5.Smith KM, Scott DR, Barner JC, DeHart RM, Scott JD, Martin SF. Interprofessional education in six US colleges of pharmacy. Am J Pharm Educ. 2009;73(4):Article 61. doi: 10.5688/aj730461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Chicago, IL: Accreditation Council for Pharmacy Education; 2011 Feb. 57 p. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed 23 May 2012. [Google Scholar]
- 7.Odegard PS, Robins L, Murphy N, et al. Interprofessional initiatives at the University of Washington. Am J Pharm Educ. 2009;73(4):Article 63. doi: 10.5688/aj730463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kroboth P, Crismon LM, Daniels C, et al. Getting to solutions in interprofessional education: report of the AACP 2006-2007 Professional Affairs Committee. Am J Pharm Educ. 2007;71(6):Article S19. [Google Scholar]
- 9.Accreditation Council for Pharmacy Education. Application for precandidate status for organizations developing a doctor of pharmacy degree program. Chicago, IL: Accreditation Council for Pharmacy Education; 2008 Jan. 44 p. https://www.acpe-accredit.org/pdf/application_for_seeking_preaccreditation_%202008_final.pdf. Accessed April 25, 2012. [Google Scholar]
- 10.Reid R, Bruce DA, Allstaff K, McLernon D. Validating the readiness for interprofessional learning scale (RIPLS) in the postgraduate context: are health care professionals ready for IPL? Med Educ. 2006;40(5):415–422. doi: 10.1111/j.1365-2929.2006.02442.x. [DOI] [PubMed] [Google Scholar]
- 11.Luecht RM, Madsen MK, Taugher MP, Petterson BJ. Assessing professional perceptions: design and validation of an interdisciplinary education perception scale. J Allied Health. 1990;19(2):181–191. [PubMed] [Google Scholar]
- 12.Buring SM, Bhushan A, Brazeau G, Conway S, Hansen L, Westberg S. Keys to successful implementation of interprofessional education: learning location, faculty development, and curricular themes. Am J Pharm Educ. 2009;73(4):Article 60. doi: 10.5688/aj730460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, DC: Interprofessional Education Collaborative; 2011. 2011. [Google Scholar]