Abstract
Objectives. To determine the extent of implementation of Institute of Medicine (IOM) recommendations for 5 core competencies within the doctor of pharmacy (PharmD) curricula in US colleges and schools of pharmacy.
Methods. A survey instrument that used IOM language to define each of the recommended competencies (patient-centered care, interdisciplinary teaming, evidence-based practice, quality improvement, and informatics) was sent to 115 US colleges and schools of pharmacy.
Results. Evidence-based practice and patient-centered care were the most widely implemented of the 5 core competencies (in 87% and 84% of colleges and schools, respectively), while informatics, interdisciplinary teaming, and quality improvement were implemented to a lesser extent (at 36%, 34%, and 29% of colleges and schools, respectively).
Conclusions. Significant progress has been made by colleges and schools of pharmacy for inclusion of IOM competencies relating to evidence-based practice and patient-centered care within curricula. However, the areas of informatics, interdisciplinary teaming, and quality improvement are lagging in inclusion.
Keywords: Institute of Medicine, competency, curriculum
INTRODUCTION
The Institute of Medicine (IOM) has highlighted the extent of harm caused by medical errors and other problems with healthcare quality and the need to transform healthcare to improve outcomes.1,2 The IOM recognized that a safer healthcare system could not be built without adequately trained health professionals.
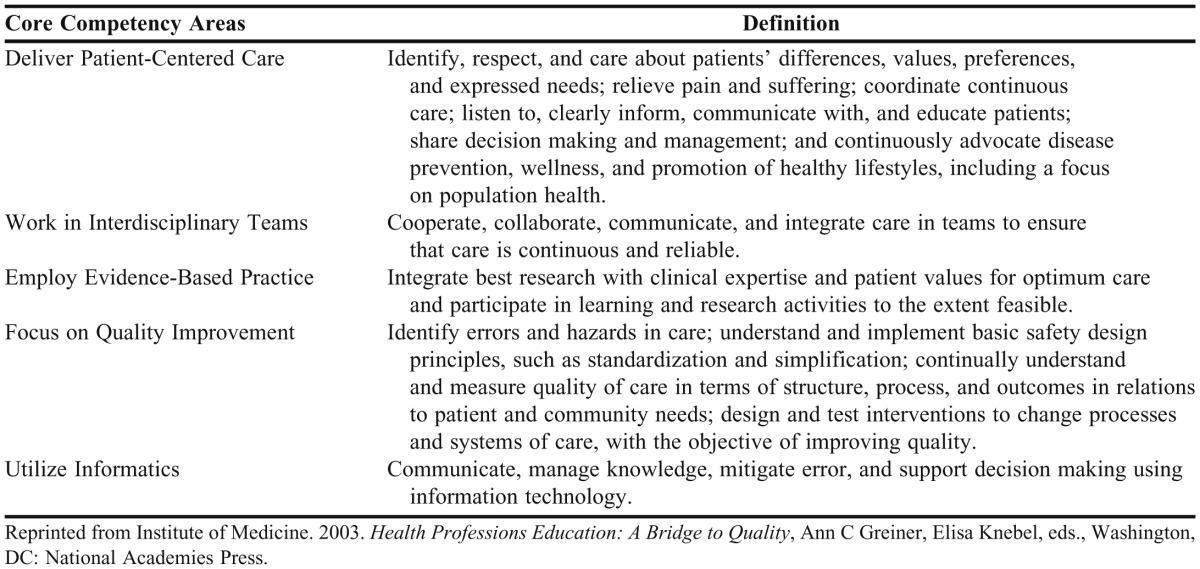
The IOM Report: Health Professions Education: A Bridge to Quality, published in 2003, emphasized changes in the education of health care professionals that are needed to improve the quality of health care in the United States.3 The report presented a vision that emphasized the importance of integrating 5 core competencies into health professions education to prepare professionals to meet the evolving needs of the health care system: patient-centered care, interdisciplinary teams, evidence-based practice, quality improvement, and informatics (Table 1).3
Table 1.
Defining the Institute of Medicine Five Core Competencies
Reports from several other professional and/or interdisciplinary expert groups, including the American Association of Colleges of Pharmacy (AACP) Curricular Change Summit, the Interprofessional Education Collaborative, the Council on Credentialing in Pharmacy, and the Lucian Leape Institute at the National Patient Safety Foundation, have emphasized the importance of incorporating the 5 core competencies into the education of health care professionals.4-7 The Accreditation Council for Pharmacy Education (ACPE) acknowledged the IOM report and incorporated the competencies into Standards 2007.8 In addition, Guidelines version 2.0 for ACPE Accreditation Standards 2007 highlight the importance of addressing the 5 core competencies, with a particular/specific focus on interprofessional education. The guidelines emphasize key areas, including patient safety and interprofessional team work, to better prepare graduates to work in collaborative health care teams.9
While ACPE, AACP, and other organizations have emphasized inclusion of these competencies within pharmacy curricula, the extent to which US colleges and schools of pharmacy have implemented the competencies into their PharmD programs was unknown. A literature search of MEDLINE, CINAHL and International Pharmaceutical Abstracts (IPA) from 1996 to October 2011 to identify existing reports on the inclusion of IOM competencies in pharmacy curricula was conducted using terms and synonyms for the 5 core competencies and the terms pharmacy education or pharmacy schools. Although some reports on attempts to include these competencies in pharmacy curricula were identified, no reports that assessed the inclusion of all 5 competencies were found.
Inclusion of informatics has been assessed to some degree within pharmacy curricula. An initial study retrieved data on pharmacy informatics from course titles and descriptions published on the public Internet Web sites of colleges and schools of pharmacy.10 These findings were used in a follow-up study to determine the extent of pharmacy informatics education and compliance with ACPE Standards 2007 for accredited pharmacy colleges and schools in the United States.11 This study identified current competencies in the area of pharmacy informatics while also proposing a foundational set of core competencies for teaching informatics.
Baseline information on integrating the science of safety into the PharmD curricula has been reported by a collaboration between AACP, the Food and Drug Administration and the American Pharmacists Association’s Pharmacy Services Support Center.12-15 The science of safety competencies are consistent with those recommended in the IOM report, Health Professions Education: A Bridge to Quality.3
In 2011, Kiersma and colleagues reported that the development of patient safety curricula in health professions curricula (medicine, pharmacy, nursing, and dentistry) has primarily been discipline-specific and that a variety of educational methods have been used.16 Interprofessional education has also been studied using structured interviews at 6 US colleges and schools of pharmacy to explore benefits, barriers, and strategies for implementation.17 A 2009 survey of 112 academic institutions, which addressed the extent to which IOM competencies were covered in the allied health professions education, found a strong desire to include these competencies and moderate to strong success in including all 5 core competencies.18
The purpose of the present study was to determine the level of inclusion of the 5 IOM competencies in PharmD curricula in US colleges and schools of pharmacy. The authors hope that the data gathered will help identify and improve the incorporation of all 5 of the competencies within pharmacy curricula.
METHODS
A 24-question survey instrument that used IOM language to define each of the competencies was developed. The IOM-related questions on the survey instrument were previously used in another study by one of the study investigators for a survey he conducted in colleges and schools of allied health.18 The survey items of the present study asked the extent to which each core competency was included within the PharmD curriculum; the extent of desire to include the competency; and if already included, how the competency was incorporated in the curriculum. The items on extent of inclusion and desired extent of inclusion used a Likert scale on which 1 indicated not at all and 5 indicated to a great extent. The scale for items on how the competency was included used a 4-point scale on which 1 indicated “standalone course,” 2 indicated “topic within course(s),” 3 indicated “integrated throughout curriculum,” and 4 indicated “not offered.” In addition, the survey instrument asked respondents to indicate to the best of their knowledge whether their college or school had ever used the 2003 IOM report, “Health Professions Education: A Bridge to Quality” in curricular planning and/or assessment? The same Likert scale, ranging from 1 indicating not at all to 5 indicating to a great extent was used. The survey instrument was reviewed and pretested by 3 faculty members experienced in survey research and pharmacy education at the Massachusetts College of Pharmacy and Health Sciences (MCPHS). Based on the feedback from the review and pretest, a few minor modifications were made to the demographic section of the survey instrument, but none to the IOM-related questions.
An e-mail distribution list of all colleges and schools of pharmacy was provided by AACP following approval by the MCPHS Institutional Review Board. In November 2010 the survey instrument was sent electronically to pharmacy practice chairs of 115 US colleges and schools of pharmacy (full or candidate status) to either complete or designate to an individual for online completion via Zoomerang. Follow-up e-mails with a link to the survey instrument were sent over the next 2 months. The survey responses were anonymous and only reported in aggregate form. Descriptive statistics were used for data analysis.
Demographic items were included in the survey instrument to determine the type and setting of the pharmacy college or school (private or public, whether it was part of a medical center, and the class size range of the first professional year PharmD class). The survey instrument also included the region in which the college or school was located, the title of the individual completing the survey instrument, and the role of the individual on their college's or school’s curriculum committee (if any).
RESULTS
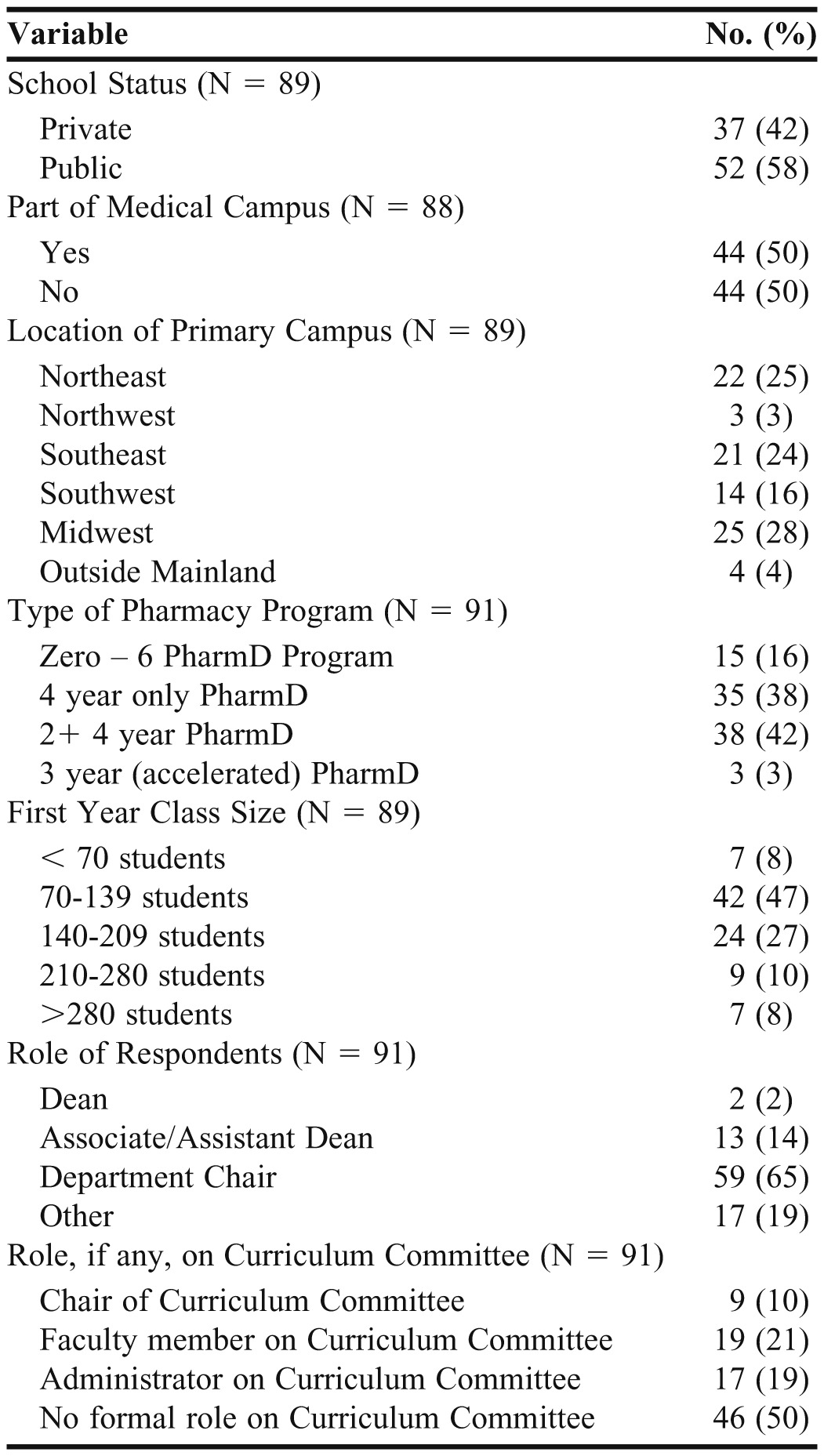
Representatives from 91 colleges and schools responded (79.1% response rate); however, not all respondents answered all questions (range of 88 to 91 respondents for the majority of questions). Of the total respondents, 58% were from public universities and 42% were from private institutions (Table 2), which is similar to the demographics of all US colleges and schools of pharmacy (54% public and 46% private institutions). The largest groups of respondents were from 2+ 4-year PharmD programs and 4-year only PharmD programs. Of the survey respondents, 50% were curriculum committee members at their college or school and 65% were department chairs.
Table 2.
Characteristics of Colleges and Schools of Pharmacy That Participated in a Survey Regarding Incorporation of Institute of Medicine Competencies in the Doctor of Pharmacy Curriculum
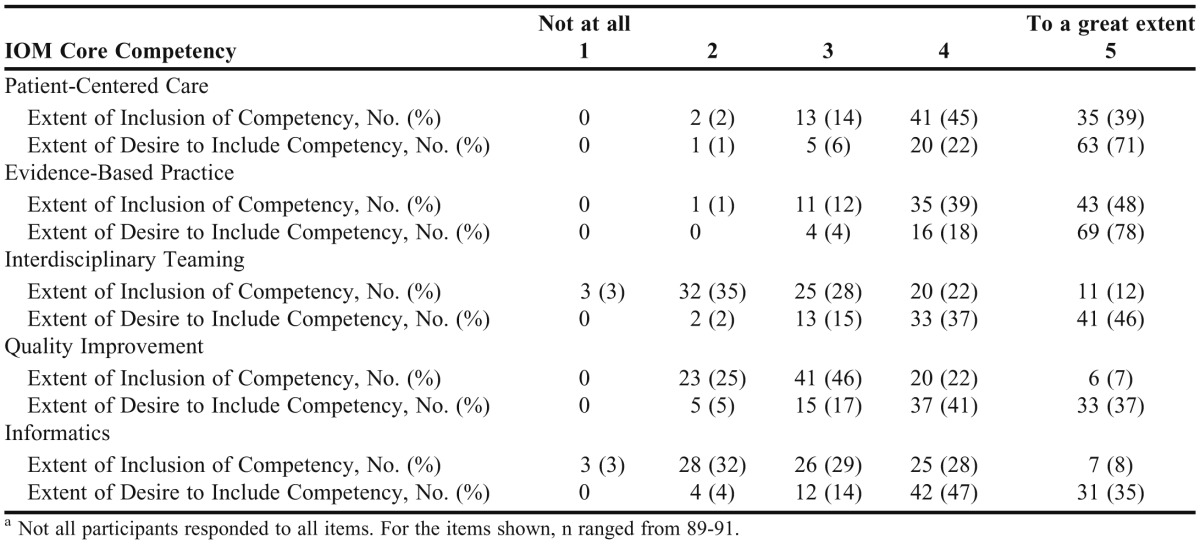
When combining the 2 highest possible survey scores of 4 and 5 (with 5 indicating “to a great extent”) evidence-based practice and patient-centered care were reported as the most widely implemented of the 5 core competencies (87% and 84%, respectively), with implementation of informatics, interdisciplinary teaming, and quality improvement to a lesser extent (36%, 34%, and 29% respectively). There was a high desire to integrate all IOM competencies into the PharmD curricula, and strong success in doing so with the evidence-based practice and patient-centered care competencies. For example, with regard to the items assessing colleges' and schools’ desired extent to include the competencies, again combining the two highest possible survey scores of 4 and 5 (with 5 indicating “to a great extent”) evidence-based practice and patient-centered care were reported at the top (96% and 93%, respectively), followed in decreasing order by interdisciplinary teaming (83%), informatics (82%), and quality improvement (78%). Data for each of the 5 competencies with respect to the level of implementation and the desire to implement the competency within the curriculum are provided in Table 3. Twenty percent of respondents indicated that the IOM report was used extensively at their college or school (combining scores of 4 and 5), 37% indicated a rating of 3, followed by 27% (rating of 2) and 16% with a rating of 1 (not at all).
Table 3.
Extent of Inclusion and Desire to Include Institute of Medicine Core Competencies in the Doctor of Pharmacy Curriculum at Colleges and Schools of Pharmacy, N = 91a
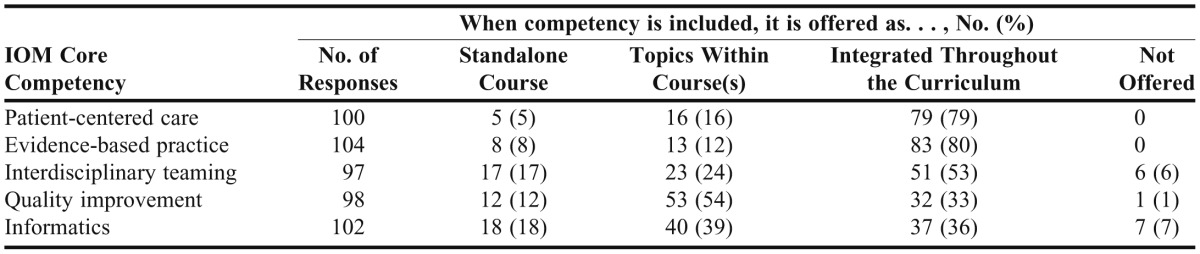
When content addressing the competencies within the PharmD curriculum was included in the colleges and schools of pharmacy curricula, respondents indicated that evidence-based practice and patient-centered care were most often integrated throughout the curriculum (80% and 79%, respectively). Quality improvement and informatics were the exceptions. With quality improvement, 54% of respondents indicated that quality improvement was offered as a topic within course(s), while 33% indicated it was integrated through the curriculum, and 12% indicated it was a standalone course. While 36% of responding institutions integrated informatics throughout the curriculum, 39% offered it as a topic within a course(s), and 18% offered it as a standalone course. Fifty-three percent of colleges and schools integrated interdisciplinary teaching within the curriculum, 24% offered it as a topic within a course(s), and 17% offered it as a standalone course. The format in which each competency was offered within the PharmD curricula is provided in Table 4 (some respondents provided multiple answers regarding format of inclusion).
Table 4.
Format in Which Institute of Medicine Competencies Are Offered in the Doctor of Pharmacy Curriculum at Colleges and Schools of Pharmacy
DISCUSSION
This study provides information on the incorporation of all 5 IOM competencies within PharmD curricula at US colleges and schools of pharmacy. While the findings of this study indicate that significant progress has been made on inclusion of evidence-based practice and patient-centered care competencies within the PharmD curricula, inclusion of the following areas is lagging: informatics (36%); interdisciplinary teaming (34%); and quality improvement (29%). These competencies are vital to reforming health professions education with the common goal of improving quality and better meeting patient needs.3 While the pharmacy profession has endorsed these changes, as in other health professions, several challenges exist for educators on various organizational levels in design, implementation, and assessment of educational experiences related to these competencies.
The strong desire to incorporate the IOM competencies within PharmD curricula is not surprising given the requirements of the ACPE Accreditation Standards.8,9 While the desire to incorporate each of the 5 core competencies was high (96% for evidence-based practice to 78% for quality improvement), the rates of actual inclusion of the core competencies within PharmD curricula was significantly lower for informatics (82% desire to include vs. 36% included), interdisciplinary teaming (83% desire to include vs. 34% included), and quality improvement (78% desire to include vs. 29% included). This study did not include questions to identify barriers to incorporation of IOM competencies within PharmD curricula. It would be valuable to examine factors that may hinder a program’s incorporation of the 5 IOM core competencies and to identify possible solutions. Previous studies in the areas of pharmacy informatics,10,11 interprofessional education,17 and the science of safety12-16 have noted challenges and deficiencies in pharmacy education within these areas and future research should build upon these findings.
This study found different approaches to incorporating IOM competencies within PharmD curricula. With regard to evidence-based practice and patient-centered care competencies, the curriculum integrative approach seems logical as it enables students to apply the recommended competencies to various areas of content and scenarios within the PharmD curriculum, including experiential education. However, depending on the course design and delivery methods, standalone courses may provide the opportunity to focus on topics in greater depth, and can be connected to other relevant content and scenarios. While beyond the scope of this study, the sequencing of courses as it relates to incorporation of IOM core competencies is key to delivering competency-based education. As students progress through the PharmD curriculum, it is important to adequately prepare them with the necessary knowledge, attitude, and skills prior to integrated experiential learning whereby they can practice and demonstrate mastery of learning outcomes. Regardless of the format used, it is important to incorporate hands-on, interactive experiences to develop competent future practitioners. Moreover, if health care professionals are to “cooperate, collaborate, communicate, and integrate care in teams to ensure that care is continuous and reliable,” they should practice these skills together while they are students. There are significant benefits of interprofessional education but there are hurdles that must be overcome to advance the goals in this area. Health professions educators have the added challenge of variability within the experiential setting, which necessitates a quality assurance procedure to facilitate students’ achievement of competencies in all pharmacy practice experiences within a program.9
Although IOM language was used in the survey items to define each of the recommended competencies, this did not ensure construct validity. Because this survey instrument asked colleges and schools of pharmacy about the inclusion of and desire to incorporate IOM core competencies, which are emphasized in the ACPE accreditation standards and by other organizations, there may have been a tendency for responders to overestimate their responses for the inclusion or desire to include the core competencies within PharmD curricula (a phenomenon similar to the Hawthorne Effect), resulting in a potential confounding bias in this study. However, the lower ratings for the inclusion of IOM competencies related to informatics, interdisciplinary teaming, and quality improvement (36%, 34%, and 29%, respectively) compared to evidence-based practice and patient-centered care (87% and 84%, respectively) suggest otherwise. Also, participants were informed that the survey instrument was anonymous and respondents’ answers were not assessed, graded, or compared to one another, making the Hawthorne-like effect less likely. Notably, with self-administered survey instruments, the wording of questions as well as the rating scale used can be misinterpreted by respondents. The respondents were asked the extent to which these competencies were incorporated within the PharmD curriculum. We assumed that the responses were based on both the pre-clinical and experiential components of the PharmD curriculum as the survey instrument specified the PharmD program (rather than singling out one aspect of the PharmD curriculum) and included questions regarding the format of inclusion in the PharmD curriculum (ie, standalone course(s), topics within courses, and integration within the curriculum). Another limitation of this study is that it did not gather information about colleges’ and schools’ assessments of whether content related to the 5 IOM competencies was being appropriately included in the curriculum. While it was beyond the scope of this study, it is an important area for future research.
As colleges and schools of pharmacy address the dynamic changes within the profession in the context of the evolving health care system, it will be important to collaborate with other health professions in a unified mission to reform health care education. Educators and practitioners within the different health professions should seek opportunities to work together to design and assess educational experiences that support the IOM competencies. Previously published works by pharmacy colleagues in the areas of informatics,10,11 interprofessional education,17,19 and the science of safety12-15, 20 are beneficial to colleges and schools of pharmacy as they advance their curricular goals. An expert panel report, “Core Competencies for Interprofessional Collaborative Practice,” provides further insight into the IOM core competency on interprofessional teamwork and its interrelationships with the other 4 IOM core competencies.4 The panel identified 4 interprofessional competency domains: Values/Ethics for Interprofessional Practice, Roles/Responsibilities, Interprofessional Communication, and Teams and Teamwork.4 Each of the 4 domains contains a set of more specific competency statements. This report, which is sponsored by the Interprofessional Educational Collaborative, will support the common vision of health professional organizations to better prepare health profession students to practice or deliver patient care in collaborative health care teams.4
CONCLUSIONS
While significant progress has been made for inclusion of IOM competencies relating to patient-centered care and evidence-based practice in the pharmacy curricula, the areas of informatics, interdisciplinary teaming, and quality improvement are lagging in inclusion. The findings of this study identify areas for improvement by colleges and schools of pharmacy, while more broadly pointing to the need for the profession to have a more unified commitment to incorporation of the IOM competencies. The variation in the findings underscores the importance for identifying possible areas of unnecessary variation and for exploring opportunities at national levels for further guidance on incorporation of IOM competencies within pharmacy and health professions curricula. It will be valuable for pharmacy programs with successful models for incorporating the IOM competencies within curricula to share their experiences within the health professions.
ACKNOWLEDGEMENTS
The authors thank Dr. Michael Montagne, Senior Associate Dean, School of Pharmacy and Dr. William McCloskey, Interim Chair, Department of Pharmacy Practice at MCPHS-Boston for their expert review of this manuscript. The authors acknowledge the contributions of Erinda Spiro who placed the questionnaire into the Zoomerang software, emailed it to the participants, and provided technical assistance with software questions.
REFERENCES
- 1.Kohn LT, Corrigan JM, Donaldson MS, editors. Institute of Medicine. ToErr is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.Institute of Medicine. Crossing the quality chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 3.Greiner AC, Knebel E, editors. Institute of Medicine. Health Professions Education: A Bridge to Quality. Washington, DC: National Academies Press; 2003. http://www.iom.edu/Reports/2003/Health-Professions-Education-A-Bridge-to-Quality.aspx. Accessed May 5, 2012. [Google Scholar]
- 4.Interprofessional Education Collaborative Expert Panel. Core Competencies for InterprofessionalCollaborative Practice: Report of an Expert Panel. Washington, D.C: Interprofessional Education Collaborative; 2011. [Google Scholar]
- 5.Jungnickel PW, Kelley KW, Hammer DP, Haines ST, Marlowe KF. Addressing competencies for the future in the professional curriculum. Am J Pharm Educ. 2009;73(8):Article 156. doi: 10.5688/aj7308156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Report of the Lucian Leape Institute Roundtable on Reforming Medical Education. Unmet Needs: Teaching Physicians to Provide Safe Patient Care. 2010. http://www.npsf.org/wp-content/uploads/2011/10/LLI-Unmet-Needs-Report.pdf. Accessed May 5, 2012.
- 7.Council on Credentialing in Pharmacy. Scope of Contemporary Pharmacy Practice: Roles, Responsibilities, and Functions of Pharmacists and Pharmacy Technicians. Washington DC; February 2009. www.pharmacycredentialing.org/ccp/Contemporary_Pharmacy_Practice.pdf. Accessed May 5, 2012.
- 8.Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (ACPE Standards 2007). Chicago, IL; 2006. https://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed May 5, 2012.
- 9.Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Guidelines Version 2.0 for Standards 2007. Effective February 14, 2011. http://www.acpe-accredit.org/standards/default.asp. Accessed May 5, 2012.
- 10.Flynn AJ. The current state of pharmacy informatics education in professional programs at US colleges of pharmacy. Am J Pharm Educ. 2005;69(4):Article 66. [Google Scholar]
- 11.Fox BI, Karcher RB, Flynn A, Mitchell S. Pharmacy informatics syllabi in doctor of pharmacy programs in the US. Am J Pharm Educ. 2008;72(4):Article 89. doi: 10.5688/aj720489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holdford DA, Warholak TL, Strum-West D, Bentley JP, Malone DC, Murphy JE. A baseline evaluation of the integration of the “Science of Safety” into the curriculum of the doctor of pharmacy degree in US colleges and schools of pharmacy. American Association of Colleges and Schools of Pharmacy; 2010. http://www.aacp.org/resources/research/Pages/FDACollaboration.aspx. Accessed May 5, 2012.
- 13.Holdford DA, Warholak TL, Strum-West D, Bentley JP, Malone DC, Murphy JE. Teaching the Science of Safety in US colleges and schools of pharmacy. Am J Pharm Educ. 2011;75(4):Article 77. doi: 10.5688/ajpe75477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.West-Strum D, Basak R, Bentley JP, et al. The Science of Safety curriculum in US colleges and schools of pharmacy. Am J Pharm Educ. 2011;75(7):Article 141. doi: 10.5688/ajpe757141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Warholak TL, Holdford DA, West D, Debake DL, Bentley JP, Malone DC, Murphy JE. Perspectives on educating pharmacy students about the Science of Safety. Am J Pharm Educ. 2011;75(7):Article 142. doi: 10.5688/ajpe757142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kiersma ME, Plake KS, Darbishire PL. Patient safety instruction in US health professions education. Am J Pharm Educ. 2011;75(8):Article 162. doi: 10.5688/ajpe758162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith KM, Scott DR, Barner JC, DeHart RM, Scott JD, Martin SJ. Interprofessional education in six US colleges of pharmacy. Am J Pharm Educ. 2009;73(4):Article 61. doi: 10.5688/aj730461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blagg JD. Descriptive analysis of level of implementation in allied health educational institutions of IOM recommended core competencies. Internet JAllied Health SciPract. 2009;7(4):1–9. http://ijahsp.nova.edu/articles/vol7num4/blagg.htm. Accessed May 5, 2012. [Google Scholar]
- 19.Buring SM, Bhushan A, Broeseker A, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. 2009;73(4):Article 59. doi: 10.5688/aj730459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fassett WE. Key performance outcomes of patient safety curricula: root cause analysis, failure mode and effects analysis, and structured communication skills. Am J Pharm Educ. 2011;75(8):Article 164. doi: 10.5688/ajpe758164. [DOI] [PMC free article] [PubMed] [Google Scholar]