Abstract
Objective. To determine student competency and confidence in the provision of diabetes care and satisfaction with incorporation of the American Pharmacist Association/American Association of Diabetes Educators (APhA/AADE) diabetes certificate program into the required doctor of pharmacy (PharmD) curriculum.
Design. Material from the diabetes certificate program was incorporated longitudinally into the third-year curriculum skills laboratory courses. Educational techniques used included self-study modules with case questions, lectures using the program’s slides and live seminar materials, and active-learning techniques including instructor-led modeling and role-playing exercises, small group activities, objective structured learning exercises (OSLE) using standardized patients, and a week-long diabetes simulation.
Evaluation. Students achieved a 100% pass rate on a diabetes certificate program examination and earned a mean score of 71.8 out of 100 points on a medication therapy management (MTM) objective structured clinical examination (OSCE). A student survey demonstrated high student confidence in their ability to provide diabetes care (mean scores 4.2 to 4.8) and satisfaction with the program (mean scores 4.5 to 4.8).
Conclusion. Longitudinal integration of a nationally recognized diabetes certificate program into the required PharmD curriculum produced satisfied students competent in providing diabetes pharmaceutical care.
Keywords: diabetes, diabetes certificate, disease management, assessment, American Pharmacists Association
INTRODUCTION
There is growing support within the pharmacy profession to require pharmacists to acquire specialized skills for chronic disease state management, which includes diabetes. It is difficult for community pharmacists to provide more than prescription dispensing and medication counseling. Pilot projects in pharmacist-delivered disease management services, patient coaching, and medication therapy management (MTM) have been successfully implemented.1-6
Without a sufficient number of pharmacists confident and competent in the delivery of specialized disease management and MTM services, advancement of the profession is unlikely. Colleges and schools of pharmacy have a responsibility to prepare students to meet future as well as current requirements of the profession. Achieving competency in specialized disease state management during pharmacy school would allow these future pharmacists to participate in advanced practice models upon entering practice. Provision of the American Pharmacist Association and American Association of Diabetes Educators (APhA/AADE) national diabetes certificate program as a required curricular component for student pharmacists could prepare them to provide diabetes pharmaceutical care. The certificate program fulfills the Accreditation Council for Pharmacy Education (ACPE) Standards 11 and 12 in that it uses active-learning strategies to promote patient-centered care and effective health and disease prevention.7
Pharmacists’ expert knowledge of medications and their ability to contribute to coordinated care models and MTM makes them a valuable asset in meeting health savings initiatives. Programs, such as the Minnesota MTM Care Program, the Asheville Project, and the Diabetes Ten City Challenge demonstrated improvement in diabetes care in addition to significant cost savings with pharmacist intervention.8-11 While not ubiquitous, payment for clinical pharmacy services is making the paradigm shift in pharmacies from product dispensing to service possible. Networks in which pharmacists provide specialized services to patients with diabetes require proof of the pharmacists’ training or competency. In some cases, board certification such as Board Certified Pharmacotherapy Specialist or Certified Diabetes Educator is required. In others, the pharmacist is only required to complete a recognized certificate program.4
Primarily targeting practicing pharmacists, certificate programs have been widely used to provide additional training for pharmacists to improve their knowledge and skills.12,13 The APhA/AADE certificate program, Pharmaceutical Care for Patients with Diabetes, is a nationally recognized program for pharmacists.14 In South Carolina, the APhA/AADE diabetes certificate program qualifies pharmacists to participate in the Palmetto Pharmacists Network (PPN).15 The PPN originated as the regional pharmacy network in South Carolina for the Diabetes Ten City Challenge in 2005, a program that resulted in improved clinical and economic outcomes and patient satisfaction.9
The literature documents diabetes elective courses and locally developed certificate programs that were embedded within the curriculum for a self-selected group of pharmacy students. Students improved their skills related to a broad range of diabetes topics.16,17 In addition, the literature describes the use of diabetes certificate programs to train practicing pharmacists.13 The pharmacists who received training had improved knowledge and confidence, were more likely to provide diabetes care, and subsequently more likely to document and bill for these services.
Evaluation of the incorporation of a nationally recognized diabetes certificate program into the required pharmacy curriculum has not been described. This paper describes implementation of such a program at the South Carolina College of Pharmacy (SCCP) and how it impacted student knowledge, skills, and confidence related to the pharmaceutical care of patients with diabetes. Specifically, the objectives of this study were:(1) to describe the integration of the APhA/AADE diabetes certificate program into required third-year pharmacy curriculum, (2) determine the impact of the certificate program on student competency in diabetes care, (3) determine the effect of the certificate program on student confidence in providing pharmaceutical care to patients with diabetes, and (4) determine student satisfaction regarding the delivery of the certificate program.
DESIGN
The APhA/AADE diabetes certificate program supports a patient-centered interdisciplinary approach to health care delivery.14 It is a comprehensive program that teaches medication therapy management as well as self-care instruction. The program is traditionally delivered in 3 parts: a Web-based self-study, online learning activities, and a 6-hour live seminar.
SCCP’s program fulfilled all of the APhA/AADE requirements as well as provided some supplemental learning experiences and assessments for students developed by skills laboratory instructors in order to integrate the certificate program into the third-year curriculum. Student participation in the APhA/AADE diabetes certificate program also fulfilled ACPE accreditation standards.7
Specific learning objectives for the SCCP program were consistent with those of the APhA/AADE for the diabetes certificate program. Students completing the program were expected to be able to: conduct a patient self-management assessment; design and implement a diabetes medication plan; and provide diabetes self-care instruction, including use of devices, products, and equipment. These learning objectives are congruent with the higher levels of Bloom’s taxonomy.18 Although the diabetes certificate program was implemented at all 3 campuses of SCCP, this study focuses on the experiences and outcomes of the MUSC campus.
As part of the college’s 4-year PharmD degree, third-year students complete 2 semester-long skills laboratory courses that cover diabetes care topics as well as other topics relevant to clinical pharmacy, advanced community pharmacy, and physical assessment skills. Students attend the live laboratory sessions 1 day each week, with approximately 25 students in each session. Several of the diabetes care topics that are delivered in the laboratories were also part of the certificate program requirements. The principle goal of this project was to deliver the APhA/AADE diabetes certificate program longitudinally in the practice skills laboratories while ensuring the program was harmonious with the material presented in the pharmacotherapy course.
Course coordinators and instructors were identified to deliver the diabetes certificate program. Instructors must have completed the certificate program and a train-the-trainer program. Two of the practice laboratory faculty members were already recognized by APhA as approved instructors so this expedited the first-year implementation of the curriculum.
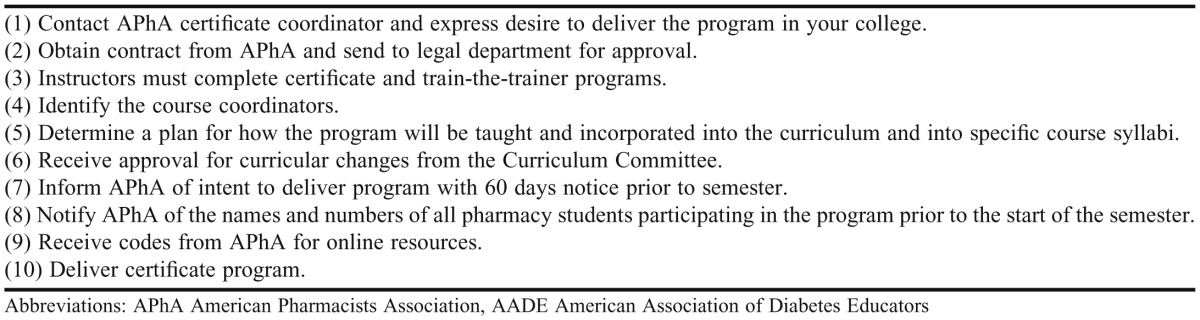
Laboratory instructors met with the instructors in the PCT course to collaborate and identify any discrepancies between the course content and the certificate program. A plan was created to deliver the curriculum in the fall and spring semesters. After approval for the certificate program was obtained by the SCCP Curriculum Committee, APhA was then informed of a start date for certificate delivery. The APhA provided special codes for each student to use for access to their online resources. A summary of the initial steps of incorporating the program into the curriculum is provided in Table 1.
Table 1.
Steps for Incorporating the APhA/AADE Diabetes Certificate Program Into the Third-Year of a Doctor of Pharmacy Curriculum
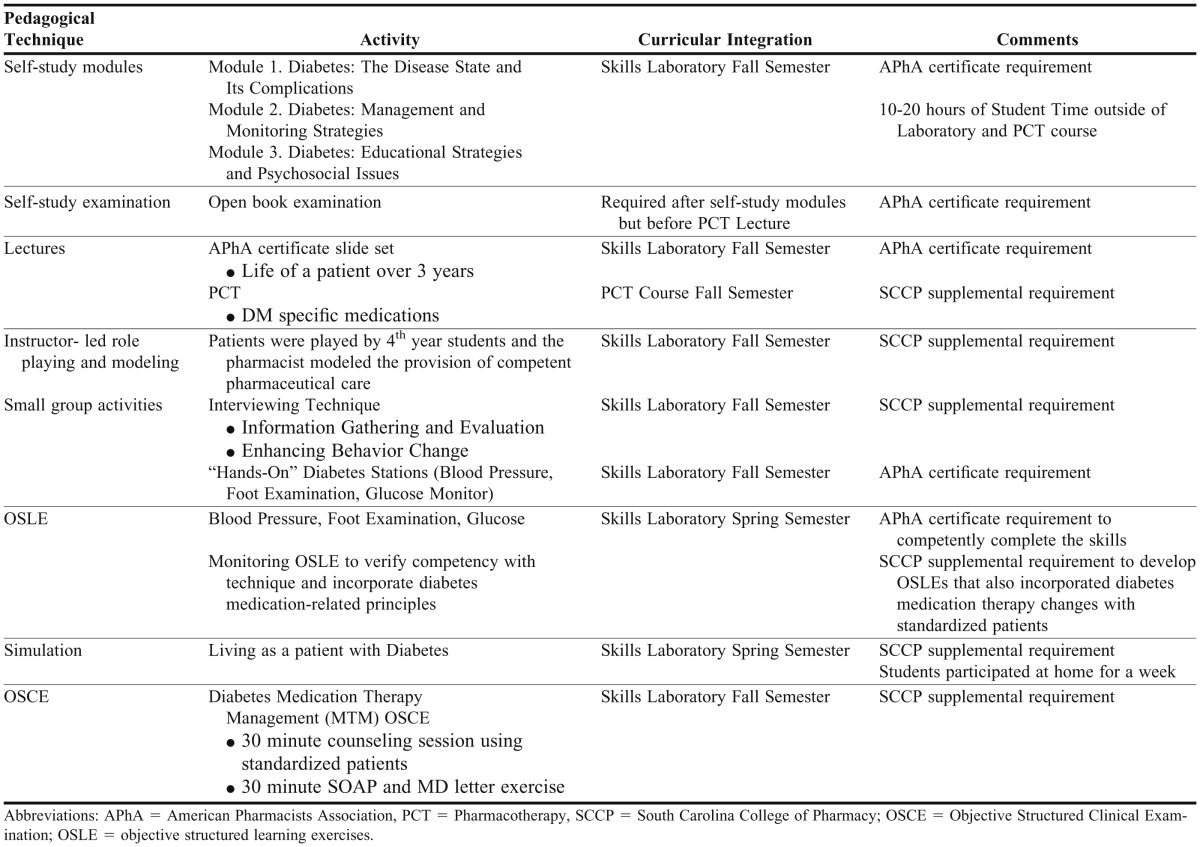
The majority of the required reading assignments, live seminar materials, and online examination were delivered in the fall semester. The “hands-on” skills competency assessments (blood glucose monitoring, etc) were completed in the spring semester (Table 2).
Table 2.
Pedagogical Techniques and Activities Used for a Diabetes Certificate Program Incorporated Into the Third-Year Curriculum of a Doctor of Pharmacy Program
In the fall semester, students were responsible for reading the 3 online modules and completing the accompanying reinforcement exercises (approximately 10 to 20 hours of student reading time). Because of the large amount of reading, these modules served as the required reading and reference materials for both the pharmacotherapy course and the laboratory course. Requiring the same reading assignment for both classes was thought to minimize the perceived burden on the students. The students were also given 1 laboratory day off (3 direct contact hours) to work on the online modules. After the reading assignments, students were required to complete a self-study examination and achieve a 70% score (they could take it as many times as needed) before the live seminar material was presented in the pharmacotherapy and laboratory courses.
The instructors began delivering the certificate material in the skills laboratory 1 week after the diabetes pharmacotherapy lectures commenced. Delaying the presentations in the laboratory course provided the instructor with the opportunity to reinforce material learned in the pharmacotherapy course in an active-learning environment. The live seminar material, provided by APhA, was delivered via a slide presentation demonstrating the care of a patient from diagnosis through follow up over a 3-year period. Because of the small laboratory room and class size, instructors were able to incorporate supplemental activities to foster active learning in the areas of communication, knowledge, and “hands-on” skills. Delivery of the certificate program required only a 6-hour seminar, but 9 additional hours were spent in the laboratory sessions to deliver both required and supplemental material.
Using role play, the instructor modeled best practices for how to properly interview a patient and assess and solve medication-based problems. Students also received hands-on training in the following during the skills laboratory sessions: diabetes self-care instruction, subcutaneous injection techniques, blood pressure measurement, exercise, blood glucose monitors, meal planning, and comprehensive foot examination.
At the end of the semester, students completed the final examination for the certificate. Students were allowed 2 attempts to achieve at least the APhA’s required passing score of 70%.
Students were provided additional hands-on training during the skills laboratory course in the spring semester and then required to demonstrate appropriate performance of insulin injection, diabetic foot examination, blood pressure measurement, and blood glucose monitoring. At each station, laboratory instructors completed the assessments and documentation required by APhA. To further enhance these skills, students were given supplemental laboratory exercises that required them to complete OSLEs highlighting the delivery of “hands-on” diabetes patient education. In addition, students were required to participate in a week-long simulation where they had to live the life of a patient with diabetes.19 At the conclusion of the third-year, laboratory instructors collected all the required paperwork for each student and submitted it to APhA for their certificates.
Educational techniques used in the delivery of the certificate program were self-study modules with case questions and lectures covering required certificate slides and live seminar material, as well as active-learning techniques including instructor-led modeling and role-playing exercises, small group activities, objective structured learning exercises using standardized patients, and a week-long diabetes simulation. The self-study modules with learning-reinforcement exercises provided a foundation in the management of a patient with diabetes. The instructor-led role-playing exercises modeled the proper way a pharmacist should conduct a patient self-management assessment. Following each role-play, the instructor led an open discussion. Student-based small-group activities were used to foster self-learning and allowed students to provide each other with feedback for improvement. The OSLEs and diabetes simulation encouraged students to engage in active learning and allowed instructors to conduct performance-based assessments and provide feedback.
A variety of resources were needed to incorporate and deliver the curriculum for the APhA/AADE diabetes certificate program. Sixty to 85 additional hours of dedicated faculty time was required by the coordinator and 20 to 40 hours was required for additional instructor training and delivery. A 10 to 20 hour additional time commitment was required by the students. The equipment needed to teach the curriculum was the same as that for existing laboratories (glucose meters, test strips, lancing devices, insulin syringes, normal saline, monofilaments and blood pressure equipment). Although APhA discounted the fees for the certificate program, the cost to students was still significant. College administration built this cost into tuition fees. There were additional APhA fees required for faculty members who needed both the certificate training and the instructor level training. Costs were also incurred for standardized patients and resources needed to conduct the supplemental MTM OSCEs. This study was approved as exempt research by the Institutional Review Board at MUSC.
EVALUATION AND ASSESSMENT
Assessment of the incorporation of the APhA/AADE diabetes certificate program focused on 3 areas: student competency in diabetes care, student confidence in diabetes care, and student satisfaction with the certificate program. Although the certificate program was incorporated on all campuses of SCCP, assessment methods and results are only reported for the MUSC campus (n = 79).
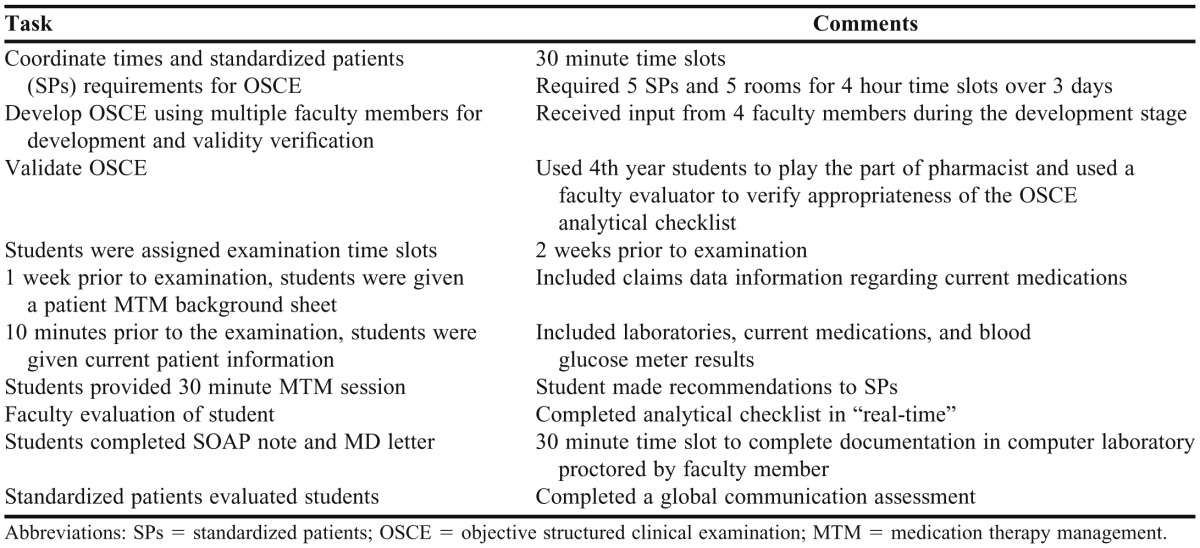
Student competency was assessed using 2 methods, the first of which was the required APhA/AADE diabetes certificate program written final examination. To further assess competency, students were required to also complete a diabetes MTM OSCE as part of their final skills laboratory grade in the fall semester. The OSCE, which was developed and validated by the laboratory instructors, incorporated all components of the certificate program and required the students to comprehensively apply their diabetes knowledge and care for a standardized patient (Table 3). Thirty minutes were allowed to complete the OSCE and 30 minutes to complete a SOAP (subjective, objective, assessment, plan) note. The OSCE was evaluated using a validated analytical checklist shown in Appendix 1. Students were required to achieve an overall score of 70% or greater on the OSCE to pass. Students who did not achieve a passing score on the OSCE were required to meet with the laboratory instructor to review the encounter and complete a reflection paper highlighting self-improvements they could make during future patient visits.
Table 3.
Diabetes Medication Therapy Management OSCE Development and Delivery
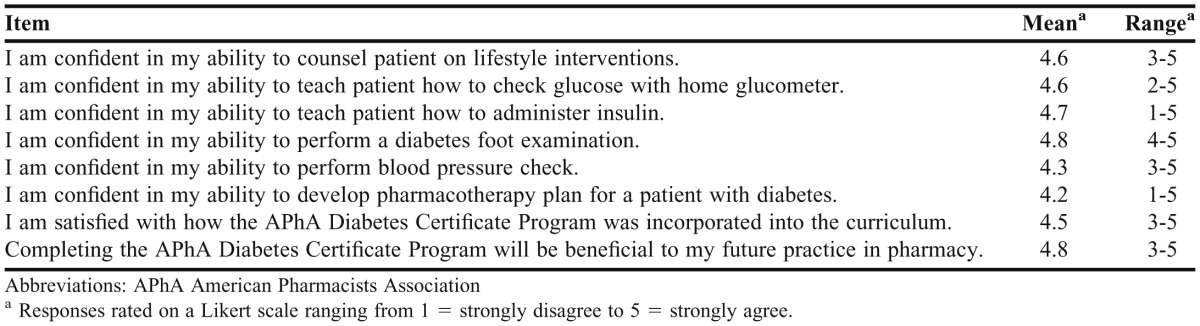
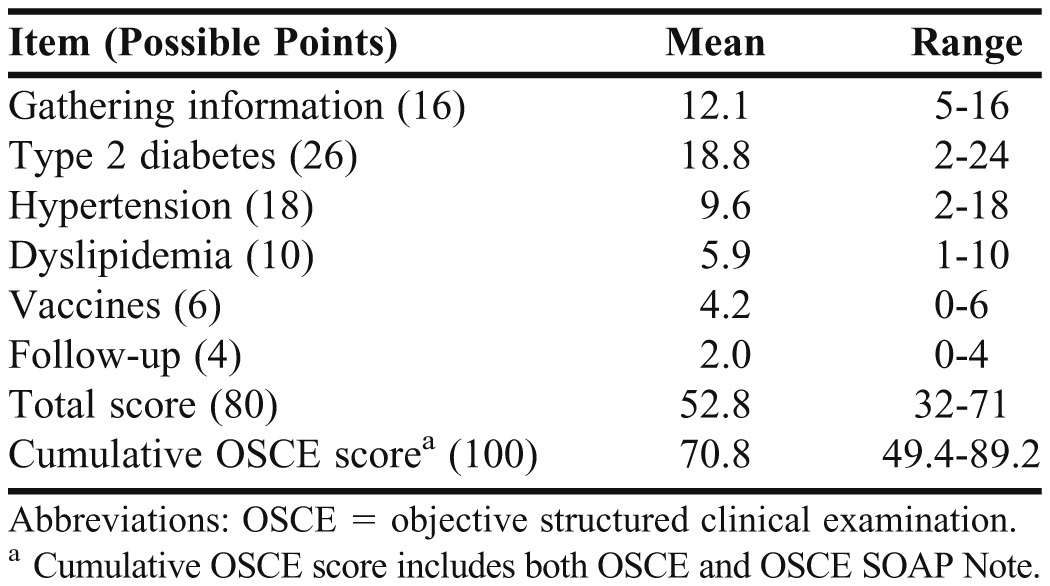
All students (n = 79) completed and passed the required written final examination and “hands-on” competencies for the APhA/AADE diabetes certificate program. Student competency based on the final diabetes MTM OSCE and SOAP note was passing with a mean score of 70.8 out of 100 possible points. The students performed with a mean of 52.8 out of a possible 80 points on the OSCE with the standardized patient. Additionally, students had a mean score of 17.2 out of a possible 28 points on the corresponding SOAP note. The students’ strongest performance areas on the OSCE were in gathering information from the patient, conducting diabetes counseling, and verifying/obtaining/documenting vaccine status (Table 4). Student confidence in the provision of diabetes care and student satisfaction with the incorporation of the APhA/AADE diabetes certificate program was assessed after completing both skills laboratories and all certificate requirements at the end of the spring semester in the third year. The instructors developed an 8-question survey instrument and incorporated feedback from other instructors and fourth-year students into a final version. Responses on the survey instrument were rated using a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree. The voluntary and anonymous survey instrument was administered using SurveyMonkey, Inc. (Palo Alto, CA). Statistical analyses were performed using Microsoft Excel database. Descriptive statistics were used to analyze student competency, confidence, and satisfaction data.
Table 4.
Pharmacy Students’ Scores on an Objective Structured Clinical Examination After Completing the APhA Diabetes Certificate Programa
Seventy students (response rate 89%) completed the anonymous online survey instrument. Students’ mean scores on the confidence questions ranged from 4.2 to 4.8. Students’ mean score for their satisfaction with the longitudinal incorporation of the APhA/AADE diabetes certificate program into the PharmD curriculum was 4.5 and their mean score regarding benefits of the program to future pharmacy practice was 4.8. Many students provided additional comments expressing how useful the program was, and how much of an impact it would have on their future pharmacy practice (Table 5).
Table 5.
Survey of Pharmacy Students’ Confidence and Satisfaction After Completing the APhA Diabetes Certificate Program (N = 70)
DISCUSSION
This paper discusses incorporation of the APhA/AADE diabetes certificate program into a required PharmD curriculum. The 24-hour (6-hour seminar and 18-hour self-study) certificate program was restructured and integrated longitudinally into the third-year pharmacy curriculum. In addition to the certificate program requirements, supplemental instruction and assessments were provided to students in skills laboratories to enhance learning. The addition of the APhA/AADE diabetes certificate program to the curriculum contributed to student competency in the provision of diabetes pharmaceutical care. Student confidence in diabetes knowledge, skills, and management also were increased and they were highly satisfied with the program.
Incorporating the APhA/AADE diabetes certificate program into the required pharmacy curriculum was a novel approach that went beyond simply teaching the provided materials to students. Previous studies reported diabetes care electives or home-grown certificate programs aimed at smaller groups of students or practicing pharmacists.12,13,16,17 We report incorporation of a nationally recognized program into the required curriculum for third-year PharmD students at our college. We describe a longitudinal model and a step-by-step guide for incorporating the program, which can serve as a model for other colleges of pharmacy planning to implement a similar curriculum. The program produced students competent in diabetes pharmaceutical care and certified in the APhA/AADE program. Additional assessment methods included an OSCE to determine student application of knowledge gained from the program in a MTM session using standardized patients. Student confidence in diabetes knowledge, skills, and attitudes was high after completion of the program. Finally, students were highly satisfied with the program and believed it will positively benefit future pharmacy students. Conceptually, incorporating the APhA/AADE diabetes certificate program into the pharmacy curriculum would better prepare future pharmacists to participate in diabetes practice models upon graduation and licensure, and that would ultimately advance the profession.
A significant limitation to implementing this program was the time and resources needed. Students were required to complete on average 18 hours of self-study time to meet APhA/AADE diabetes certificate program requirements. Although many of the requirements, including completion of online modules and readings, were incorporated longitudinally into skills laboratories and the pharmacotherapy course, students had to invest many hours outside of class to successfully complete the course. The faculty time commitment increased as skills laboratories were restructured to include components of the APhA/AADE diabetes certificate program. The program was also resource-intensive, requiring the necessary supplies to provide diabetes pharmaceutical care (eg, blood glucose monitors, syringes). Additionally, incorporation of the OSCE required use of standardized patients who were trained and paid by the hour. Students incurred an additional fee ($95) to complete the certificate program. Finally, assessing changes in student confidence and competence using either a pre/post or randomized controlled study design would have strengthened the results, but would have required additional time and resources.
CONCLUSION
Incorporating the APhA/AADE diabetes certificate program longitudinally into a required pharmacy curriculum allowed for all pharmacy students to be recognized providers in a national certificate program. After completion of the program, students were competent and confident providers of diabetes pharmaceutical care. Students were highly satisfied with the certificate program and it can serve as a model for other pharmacy colleges and schools to help advance the profession.
REFERENCES
- 1.American Pharmacists Association and the National Association of Chain Drug Stores Foundation. Core elements of an MTM service model version 2.0. J Am Pharm Assoc. 2008;48(3):341–353. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 2.Choe MH, Mitrovich S, Dubay D, et al. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11(4):253–260. [PubMed] [Google Scholar]
- 3.Clifford R, Davis W, Batty K, Davis T. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes. Diabetes Care. 2005;28(4):771–776. doi: 10.2337/diacare.28.4.771. [DOI] [PubMed] [Google Scholar]
- 4.Leal S, Glover J, Herrier R, Felix A. Improving quality of care in diabetes through a comprehensive pharmacist based disease management program. Diabetes Care. 2004;27(12):2983–2984. doi: 10.2337/diacare.27.12.2983. [DOI] [PubMed] [Google Scholar]
- 5.Glenn ZM, Simmons ML, West CP, Schmidt AM. Advantages of a pharmacist-led diabetes education program. US Pharm. 2005;11:52–61. [Google Scholar]
- 6.McCord AD. Clinical impact of a pharmacist-managed diabetes mellitus drug therapy management service. Pharmacotherapy. 2006;26(2):248–253. doi: 10.1592/phco.26.2.248. [DOI] [PubMed] [Google Scholar]
- 7.Accreditation Council for Pharmacy Education. Accreditation standards. http://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed April 22, 2012.
- 8.Garrett D, Bluml B. Patient self-management program for diabetes: first-year clinical, humanistic, and economic. J Am Pharm Assoc. 2005;45(2):130–137. doi: 10.1331/1544345053623492. [DOI] [PubMed] [Google Scholar]
- 9.Fera T, Bluml B, Ellis W. Diabetes ten city challenge: final economic and clinical results. J Am Pharm Assoc. 2009;49(3):52–60. doi: 10.1331/JAPhA.2009.09015. [DOI] [PubMed] [Google Scholar]
- 10.Isetts BJ, Schondelmeyer SW, Artz MB, et al. Clinical and economic outcomes of medication therapy management services: the Minnesota experience. J Am Pharm Assoc. 2008;48(2):203–211. doi: 10.1331/JAPhA.2008.07108. [DOI] [PubMed] [Google Scholar]
- 11.Cranor CW, Bunting BA, Christensen DB. The Asheville Project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc. 2003;43(1):173–184. doi: 10.1331/108658003321480713. [DOI] [PubMed] [Google Scholar]
- 12.Smith JL. Planning and implementation of certificate programs in pharmacy: a review of six programs in the literature. Am J Pharm Educ. 2001;65(2):155–158. [Google Scholar]
- 13.Plake KS, Chesnut RJ, Biebighauser S. Impact of a diabetes certificate program on pharmacists’ diabetes care activities. Am J Pharm Educ. 2003;67(4):Article 116. [Google Scholar]
- 14.American Pharmacists Association. http://www.pharmacist.com/AM/Template.cfm?Section=Pharmaceutical_Care_for_Patients_with_Diabetes. Accessed April 22, 2012.
- 15.Palmetto Pharmacists Network. http://www.scrx.org/displaycommon.cfm?an=1&subarticlenbr=86. Accessed April 22, 2012.
- 16.Westberg SM, Bumgardner MA, Brown M, Frueh J. Impact of an elective diabetes course on student pharmacists' skills and attitudes. Am J Pharm Educ. 2010;74(3):Article 49. doi: 10.5688/aj740349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryan GJ, Foster KT, Unterwagner W, Haomiao J. Impact of a diabetes certificate program on PharmD students' knowledge and skills. Am J Pharm Educ. 2007;71(5):Article 84. doi: 10.5688/aj710584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bloom BS, editor. Taxonomy of Educational Objectives. The Classification of Educational Goals. Handbook I: Cognitive Domain. New York, NY: McKay; 1956. [Google Scholar]
- 19.Delea D, Shrader S, Phillips C. A week-long diabetes simulation for pharmacy students. Am J Pharm Educ. 2010;74(7):Article 130. doi: 10.5688/aj7407130. [DOI] [PMC free article] [PubMed] [Google Scholar]