Abstract
A review of the literature relating to the use of virtual patients in teaching pharmaceutical care to pharmacy students was conducted. Only 7 articles met the inclusion criteria for the review and 4 of the studies were conducted in North America. Few articles identified by the review used virtual patient technology that was true-to-life and/or validated.
Keywords: virtual patient, pharmaceutical care, systematic review
INTRODUCTION
Pharmacists’ ability to communicate effectively with patients is paramount in the prevention and management of drug-therapy problems.1-3 The effective delivery of pharmaceutical care interventions requires not only sound clinical knowledge of medication, but also good communication skills to interact with patients and review their medication needs and use. Over a decade ago, the World Health Organization identified the ability to communicate effectively as a skill pharmacists must possess in support of their role,4 prompting pharmacy colleges and schools around the world to introduce communication skills as an integral part of the pharmacy curriculum. In contrast, most colleges and schools of Pharmacy in Brazil are yet to implement communication skills in their curricula, despite that the National Guidelines for Undergraduate Education in Pharmacy have included formal training in communication skills as an integral part of the pharmacy curriculum.5
In developed countries, recognition of the value of pharmacy in the prevention and management of drug-therapy problems has led to demonstrable efforts made by pharmacy colleges and schools to teach effective communication skills to students. Curriculum changes have incorporated training in communication skills, including the introduction of theoretical-practical disciplines, as well as the establishment of practice laboratories.6-9 Additionally, different methods of teaching communication skills to pharmacy students have been developed, including face-to-face, telephone, and e-mail interviews; analysis of audio and video tapes; and simulated patient methods in which actors played the role of patients or actual patients who were coached to present specific scenarios to pharmacists in order to teach and evaluate their patient assessment and interview skills.10-14
Over the last decade, use of virtual patient technology—from computer-based virtual reality programs to full-size lifelike simulators— emerged as a new method of training health care providers in clinical and communication skills. In pharmacy education, the virtual patient is a simulated patient, typically generated by a computer software program, and used to simulate realistic clinical scenarios.15 Teaching methods using virtual patient technology in health care education allow students to adopt the role of a health care provider in a safe environment where they can develop clinical and communication skills, such as patient assessment, interview skills, and information provision, without compromising the welfare of an actual patient. This can be achieved through the use of a range of virtual clinical scenarios applied to individual case-based assignments.16 Typically, students interact with a virtual patient, and during the process of assessment, propose some health care intervention, which is then recorded to complete the case. As computer-generated virtual patients are available on demand, students are able to practice their clinical and communication skills at any time.
An advantage of using virtual patients in the teaching of medication counseling compared to traditional teaching methods is the ability of the virtual patient to emulate the psychological state of the different types of patients that pharmacists encounter in the practice of pharmacy (eg, angry, anxious, ambivalent, passive, assertive, and persuasive).7 This not only allows future pharmacists to build realistic expectations of pharmacy practice, but also enhances trainees’ confidence in their medication-counseling skills, increasing their sense of self-efficacy in dealing with all types of patients.17
Virtual patient technology also can be used to assess student skills. Hubal and colleagues14 argue that the use of case studies involving any of the 3 types of patients (real, simulated, virtual) is the optimal way of assessing critical-thinking skills in students, compared to paper-based case studies. At least 94 medical schools in the United States and Canada use virtual simulated patients in their teaching programs, and 26 medical schools in the United States cooperate in resource sharing, standard setting, and other issues relevant to implementing effective simulated-patient programs.14 In addition, several interactive virtual patients software programs have been developed during the last 10 to 15 years.16 In pharmacy, the first study in which virtual patient technology was reported was published in the early 1990s.17 There are only a paucity of published studies in the area.
The standardized nature of virtual patient simulations also increases the validity of assessments, as each scenario is relatively consistent.15 The use of virtual patient technology allows students to develop their competencies (knowledge, skills, and attitudes) in providing care to patients.18 Therefore, it is important to use techniques such as virtual patient technology in teaching pharmacotherapy and pharmacist-patient communication skills, as virtual patients allow students to experience true-to-life situations and the knowledge and skills developed through these experiences have the long-term potential to optimize patient care. The aim of the current paper is to review the literature on the use of virtual patient technology in the teaching of pharmaceutical care to pharmacy students.
LITERATURE SEARCH
A search was conducted of the following electronic databases: EBSCO, Embase, Latin American and Caribbean Center on Health Sciences Information (LILACS), Pubmed/Medline, Scientific Electronic Library Online (SciELO), and Scopus. The following combinations of search terms were used: virtual patient and pharmacist, virtual patient and pharmacy, and virtual patient and medication.
To study the literature on the use of virtual patients in pharmacy, we retrieved articles from all 6 databases that met the following criteria: original articles and reviews from experts, published from January 1960 to December 2009 in the English language, where virtual patients were used in the teaching of competencies (skills, knowledge, and attitudes) related to pharmacist-patient interactions. We excluded studies in which the use of virtual patients occurred outside the discipline of pharmacy.
Abstracts resulting from the initial online search were manually screened for relevance and eligibility for full-text retrieval. Articles indexed in 2 or more databases were considered only once.
The following categories of data were extracted from selected articles: (1) setting where virtual patients were used; (2) scenario of the virtual consultation (outpatient, community pharmacy, hospital pharmacy); (3) number of students who used the virtual patient tool; (4) year of the students’ degree; (5) student satisfaction with the virtual patient tool; (6) competencies assessed; (7) role of instructors; (8) program development; and (9) limitations.
FINDINGS
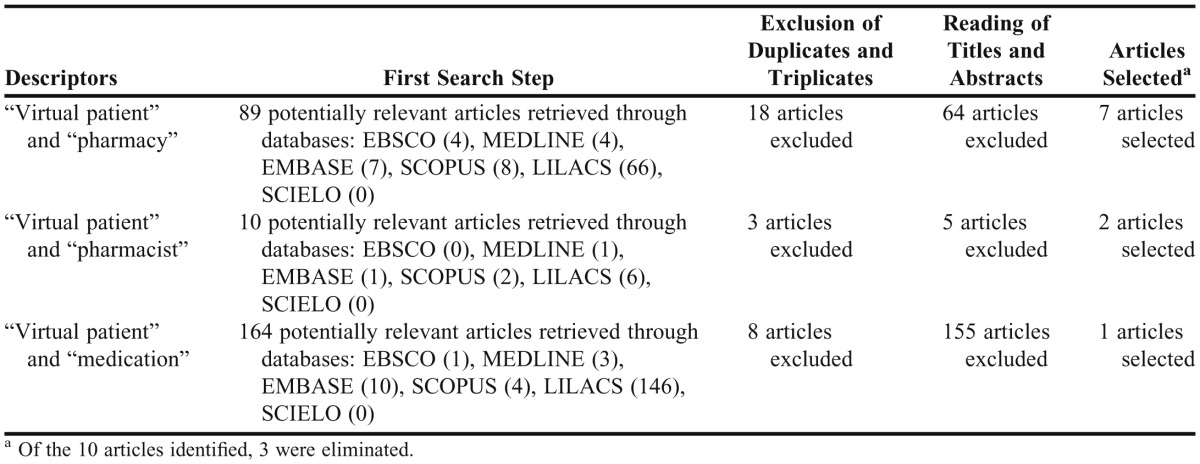
The literature search generated 72 articles using the terms virtual patient and pharmacy, 10 articles with the terms virtual patient and pharmacist, and 157 articles with the terms virtual patient and medication. Of these studies, only 7 met the inclusion criteria, and these 7 formed the study sample.
Table 1 shows the distribution of articles by database. All 7 articles selected were indexed in the Scopus database; 5 of them were indexed concurrently in Embase, 4 in LILACS, 3 in Medline, and 2 in the EBSCO database. None of the 7 was found in the SciELO database. Most excluded articles were indexed in the LILACS database.
Table 1.
Progress Through the Stages of a Literature Search on Virtual Patient Technology
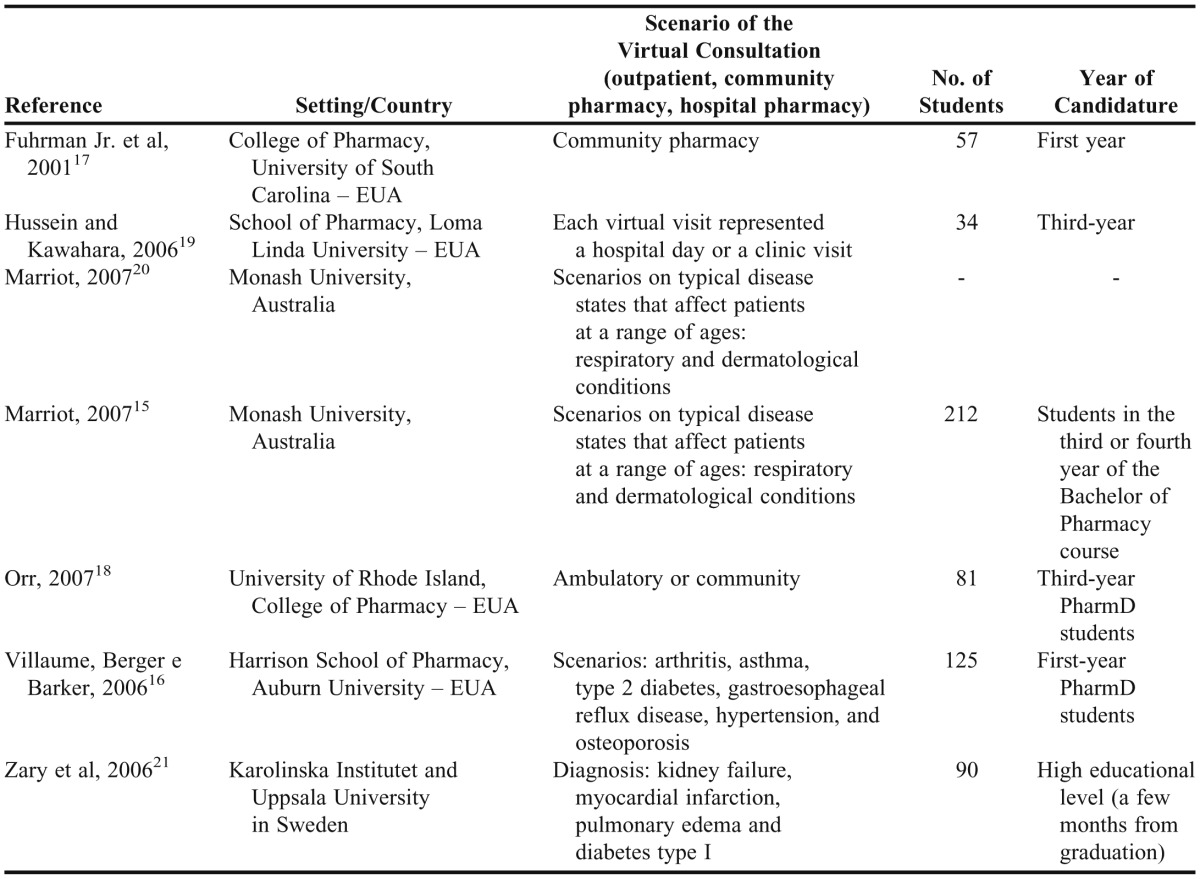
Of the studies in the final sample, 4 were conducted in North America,16-19 2 were conducted in Australia;16,20 and 1 in Europe21 (Table 2). None of the studies that met the inclusion criteria was conducted in Latin America, Africa, or Asia.
Table 2.
Characteristics of the Study Sample Related to the Use of Virtual Patient Methods from 1960 to 2009
All 7 studies were related to the teaching of pharmacy practice in the educational setting, with 1 study being multidisciplinary,21 covering the disciplines of pharmacy, medicine, and dentistry. The study reported by Marriot20 simply described the development and implementation of a computer software program for producing virtual patients, with a later study complementing this initial one by addressing the use and application of the tool by pharmacy students.15
The majority of virtual patient tools used standardized clinical cases involving chronic illness and reflected true-to-life professional practice scenarios simulating patient care in the community,17 outpatient setting,18 and hospital pharmacy.19 Four of the 7 studies did not state the location of patient care. However, 4 of the 7 articles described the clinical scenarios used.15,16,20,21
Regarding the reported number of students who used the virtual patient tool, sample sizes ranged from 3419 to 212 students.15 Virtual patients were typically used to teach students through the third year of the pharmacy curriculum.15,19
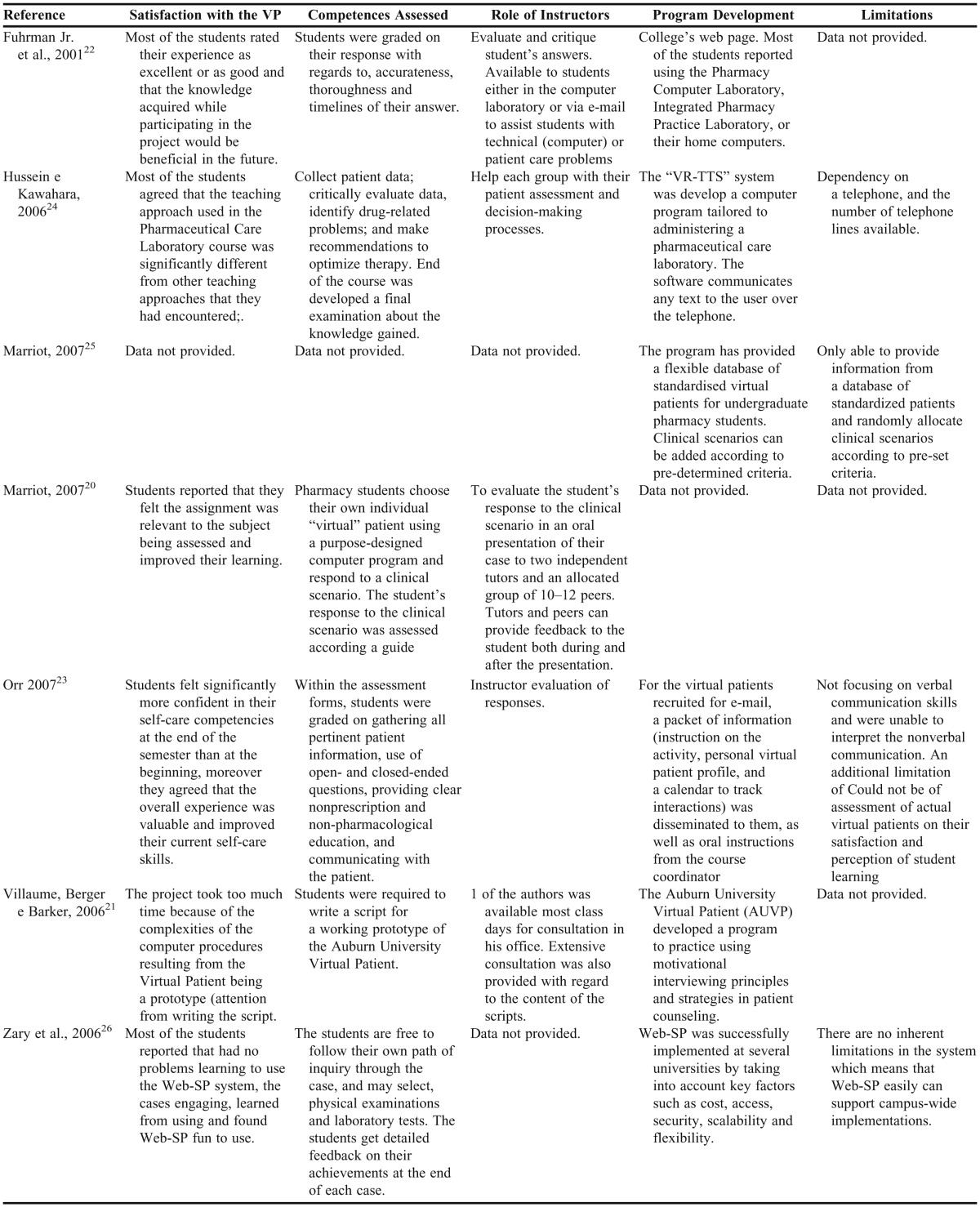
Evaluation of teaching methods using virtual patient technology was typically conducted by providing participating students with questionnaires to determine their satisfaction with the virtual patient experience, the program’s perceived value, and usability of the virtual patient tools (Appendix 1). Student assessment of the use of virtual patient technology took place in computer laboratories and at universities,19 via the Web,15,17,20,21 e-mail,18 and within computer programs.16,17 In one study, students assessed their patients from their computer at home by logging into the virtual patient database page on the college’s Web site.17 In addition, the studies assessed students’ competencies in pharmaceutical care interventions and in learning, and their ability to solve clinical cases.15-19,21 In all 7 studies, students reported a high degree of satisfaction with the virtual patient exercise and found it to be stimulating, innovative, and highly applicable to the practice of pharmacy.
Five of the reviewed studies used preceptors during the exercise to answer students’ questions regarding the virtual patient environment, including how to access sources of information necessary for solving clinical cases. Preceptors also evaluated student responses and collected feedback.15-19 The other 2 studies did not include preceptors.16,21
The reviewed studies differed in the reporting of limitations:18-20 some studies did not mention limitations16,17or reported having no limitations.21 Hussein and Kawahara reported that dependency on telephones for communication and having too few telephone lines available were limitations.19 Marriott reported limitations resulting from the small number of standardized patients and clinical scenarios from which to choose.20
DISCUSSION
Most of the 7 studies reviewed here that involved use of virtual patients were carried out in the United States, reflecting the pioneering of this country in relation to virtual patient methods in the teaching of pharmacy, with studies dating back to the late 1990s.22 Since completion of this literature review in December 2009, additional US studies have been published.23-26 The next step would be for these methods to be disseminated to a greater number of countries and for formal evaluation studies to be conducted, which may assist in the development of essential competencies in pharmacy students.
Virtual patient studies that used chronic disease scenarios may have assisted students in understanding the clinical aspects of risk-management and continuity of care. The health care literature emphasizes the importance of health care students, including pharmacy students, undergoing specific training using a technological approach, such as using virtual patient software programs, to ensure the provision of high quality care to patients with chronic disease.21,23,27-31 Therefore, the introduction of virtual patients to pharmacy education can potentially offer an effective method for teaching students, posing a challenge to current pharmacy educators to master and adopt these methods.
The studies demonstrated how using virtual patients impacted the clinical and communication skills of the students in their study samples, but most were not able to generalize their results beyond their sample.25,32 There is a need for more studies on the use of virtual patient technology to be conducted using a broader population of pharmacy students to validate its use as an effective teaching tool.
In the 7 studies reviewed, virtual patients were used in the teaching pharmaceutical care from the first year of an undergraduate pharmacy degree program to the third year of a doctor of pharmacy degree program.15-21 The use of computer technology in pharmacy education is broad and used in disciplines other than pharmacy practice, such as pharmacokinetics, dispensing, calculations, and clinical therapeutics.28-31,33 Similarly, the use of virtual patients can be broadened to encompass all aspects of pharmacy training, becoming an essential tool in pharmacy education and an integral part of student assessment.
With the worldwide increase in the adoption of pharmaceutical care practices, satisfaction with virtual patient methods in the area is an important performance indicator of educational program effectiveness. Therefore, assessment of student satisfaction with the use of virtual patients is necessary to identify its strengths and weaknesses and to improve virtual patient teaching methods.34 Students in the 7 studies found that virtual patients were an interactive and dynamic tool that assisted them in understanding disease states and managing drug therapy regimens, and that allowed them to apply what they had learned in classroom lectures to realistic situations.15-21 These findings corroborate those of Benedict and colleagues, who reported that the simulations in which virtual patients were used strongly supported by students and were effective teaching tools when used to supplement more traditional instructional formats (eg, lectures).34 Therefore, in designing future studies, researchers should consider the assessment of student satisfaction with virtual patient tools as a measurement that will lead to the expanded use of virtual patients in the teaching of pharmaceutical care.
This review found that there is a paucity of studies involving virtual patients, suggesting an under use of these methods in pharmaceutical education. Health care education is going through fundamental changes in relation to students’ skills and approaches to learning. In schools of medicine, virtual educational tools have been widely used and are considered important resources for teaching clinical skills31 (diagnostic and treatment) and communication skills.35,36 This training method is also commonly implemented in other health care professions education, including nursing37 and dentistry.38 Our findings suggest that pharmacy as a discipline may be lagging behind other health care disciplines in the use of virtual patient technology for teaching students clinical and communication skills. Pharmacy educators do not appear to be capitalizing on the congruence between computerized virtual patient approaches to teaching and the level of comfort graduate students have with virtual technology.
Semeraro and colleagues39 emphasized the importance of preceptors in familiarizing students with the use of virtual patient scenarios to practice and improve their clinical knowledge and communication skills. Some of the studies reported that preceptors assisted students in the patient decision-making process within the virtual clinical scenario.19 In addition, preceptors provided feedback on students’ performance during virtual counseling sessions and the strengths and weaknesses of using virtual patient technology to teach students.15,18 However, none of the studies in the review assessed whether the preceptors’ input had any influence on how well students performed in the virtual scenarios. Future studies should assess whether preceptors influence student outcomes when using virtual patient technology.
Two reviews found that there is a number of technologies that can be used in the teaching of clinical competencies, including telephone, e-mail, analysis of audio and video tapes, and Web pages, as well as computer software.10,11 Advantages of Internet-based virtual patient programs include their portability and realism.19 Limitations of virtual patient programs in pharmacy include the limited number of computer animations and interactions scenarios available.18,20 More sophisticated graphics and multimedia (sound, animation, text, and avatars of patients) need to be created to enhance human interactions with virtual patients and learning.
Despite the many advantages of using virtual patient technology in pharmacy education, a significant limitation identified in this review was the lack of virtual patients seeming true to life and the inability of virtual patients to provide additional unscripted information in response to students’ questions.15-21 Also, some pharmacy students did not focus on their verbal communication skills when interacting with virtual patients. Also, using virtual patients in patient encounters did not afford students practice in interpreting patients’ nonverbal communication.18 Moreover, the 7 studies did not assess the reliability of knowledge and skills acquired through use of virtual patient technology. Pharmacy educators must remember that virtual patient technology has yet to be validated as an effective learning tool for teaching pharmaceutical care.
This review is not without limitations. Only the keywords virtual patient, pharmacist, pharmacy, and medication were used. The use of other relevant key terms, such as pharmaceutical education and pharmaceutical teaching, did not lead to different results. Investigators did not search the International Pharmaceutical Abstracts (IPA) and Education Resources Information Center (ERIC) databases, which index specific journals that are not included in any other database. Consequently, some studies that would have met inclusion criteria may have been left out of the review.
CONCLUSION
Virtual patient technology has the potential to be an innovative and effective educational tool in pharmacy education, particularly for optimizing the teaching of pharmaceutical care. There are few published articles in the area and few validated virtual patient tools. Also, there are few virtual patient scenarios involving chronic diseases; lack of variability in the level of complexity of virtual patient scenarios; and lack of understanding of the influence preceptors have on students’ learning from virtual patient technology.
More resources need to be invested in the development of realistic, virtual patient technology specifically for teaching pharmacy at the graduate and undergraduate levels. Also, the technology needs to be tested in various countries to allow for internal and external validation of the programs as effective teaching tools.
Appendix 1. Characteristics of the Virtual Tools and Student Performance Were Analyzed From 1960 to 2009
REFERENCES
- 1.Berger K, Eickhoff C, Schulz M. Counselling quality in community pharmacies: implementation of the pseudo customer methodology in Germany. J Clin Pharm Ther. 2005;30(1):45–57. doi: 10.1111/j.1365-2710.2004.00611.x. [DOI] [PubMed] [Google Scholar]
- 2.Lyra Jr. DP, Rocha CE, Abriata JP, Gimenes FRE, Gonzalez MM, Pelá IR. Influence of pharmaceutical care intervention and communication skills on the improvement of pharmacotherapeutic outcomes with elderly Brazilian outpatients. Ther Clin Risk Manag. 2007;3:989–998. doi: 10.1016/j.pec.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Mackellar A, Ashcroft DM, Bell D, James DH, Marriott J. Identifying criteria for the assessment of pharmacy students’ communication skills with patients. Am J Pharm Educ. 2007;71(3):Article 50. doi: 10.5688/aj710350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO, World Health Organization. Vancouver; Canada: The role of the pharmacist in the healthcare system: preparing the future pharmacist, curricular development: WHO/PHARM/97. Report of a WHO Consultive. 27-29 August, 1997. [Google Scholar]
- 5.CNE. Conselho Nacional de Educação. Diretrizes Nacionais para o Ensino da Graduação em Farmácia de 2002 (National Guidance for the Undergraduate Teaching of Pharmacy, Brazil 2002). Diário Oficial da União. Brasília, Seção 1, p. 9. [Google Scholar]
- 6.Almeida Neto AC, Benrimoj SI, Kavanagh DJ, Boakes RA. Novel educational training program for community pharmacists. Am J Pharm Educ. 2000;64(3):302–307. [Google Scholar]
- 7.Chereson RS, Bilger R, Mohr S, Wuller C. Design of a Pharmaceutical Care laboratory: A survey of practitioners. Am J Pharm Educ. 2005;69(1):19–24. [Google Scholar]
- 8.Lust E, Moore FC. Emotional intelligence instruction in a pharmacy communications course. Am J Pharm Educ. 2006;70(1):Article 6. doi: 10.5688/aj700106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gallimore C, George AK, Brown MC. Pharmacy students’ preferences for various types of simulated patients. Am J Pharm Educ. 2008;72(1):Article 4. doi: 10.5688/aj720104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mesquita AR, Lyra Jr. DP, Brito GC, Balisa-Rocha BJ, Aguiar PM, de Almeida Neto AC. Developing communication skills in pharmacy: a systematic review of the use of simulated patient methods. Patient Educ Couns. 2010;78(2):143–148. doi: 10.1016/j.pec.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Shah B, Chewning B. Conceptualizing and measuring pharmacist-patient communication: a review of published studies. Res Social Adm Pharm. 2006;2(2):153–185. doi: 10.1016/j.sapharm.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 12.James D, Nastasic S, Horne R, Davies G. The design and evaluation of a simulated-patient teaching programme to develop the consultation skills of undergraduate pharmacy students. Pharm World Sci. 2001;23(6):212–216. doi: 10.1023/a:1014512323758. [DOI] [PubMed] [Google Scholar]
- 13.Austin Z, Gregory P, Tabak D. Simulated patients vs. standardized patients in objective structured clinical examinations. Am J Pharm Educ. 2006;70(5):119. doi: 10.5688/aj7005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hubal RC, Kizakevich PN, Guinn CI, Merino KD, West SL. The virtual standardized patient: simulated patient-practitioner dialog for patient interview training. Stud Health Technol Inform. 2000;70:133–138. [PubMed] [Google Scholar]
- 15.Marriot JL. Use and evaluation of “virtual” patients for assessment of clinical pharmacy undergraduates. Pharm Educ. 2007;7(4):341–349. [Google Scholar]
- 16.Villaume WA, Berger BA, Barker BN. Learning motivational interviewing: scripting a virtual patient. Am J Pharm Educ. 2006;70(2):Article 33. doi: 10.5688/aj700233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fuhrman Jr. LC, Buff WE, Eaddy M, Dollar M. Utilization of an integrated interactive virtual patient database in a web-based environment for teaching continuity of care. Am J Pharm Educ. 2001;65(3):271–275. [Google Scholar]
- 18.Orr KK. Integrating virtual patients into a self-care course. Am J Pharm Educ. 2007;71(2):Article 30. doi: 10.5688/aj710230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hussein G, Kawahara N. Adaptive and longitudinal pharmaceutical care instruction using an interactive voice response/text-to-speech system. Am J Pharm Educ. 2006;70(2):Article 35. doi: 10.5688/aj700237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marriot JL. Development and implementation of a computer-generated “virtual” patient program. Pharm Educ. 2007;7(4):335–340. [Google Scholar]
- 21.Zary N, Johnson G, Boberg J, Fors UG. Development, implementation and pilot evaluation of a Web-based virtual patient case simulation environment – Web-SP. BMC Med Educ. 2006;6:1–10. doi: 10.1186/1472-6920-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sherouse GW, Chaney EL. The portable virtual simulator. Int J Radiat Oncol Biol Phys. 1991;21(2):475–482. doi: 10.1016/0360-3016(91)90799-a. [DOI] [PubMed] [Google Scholar]
- 23.Benedict N. Virtual patients and problem-based learning in advanced therapeutics. Am J Pharm Educ. 2010;74(8):Article 143. doi: 10.5688/aj7408143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ricciotti HA, Hacker MR, De Flesco LD, Dodge LE, Huang GC. Randomized, controlled trial of a normal pregnancy virtual patient to teach medical students counseling skills. J Reprod Med. 2010;55(11-12):498–502. [PubMed] [Google Scholar]
- 25.Heinrichs WL, Youngblood P, Harter P, Kusumoto L, Dev P. Training healthcare personnel for mass-casualty incidents in a virtual emergency department: VED II. Prehosp Disaster Med. 2010;25(5):424–432. doi: 10.1017/s1049023x00008505. [DOI] [PubMed] [Google Scholar]
- 26.Benedict N, Schonder K. Patient simulation software to augment an advanced pharmaceutics course. Am J Phar Educ. 2011;75(2):Article 21. doi: 10.5688/ajpe75221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loke SK, Tordoff J, Winikoff M, McDonald J, Vlugter P, Duffull S. SimPharm: How pharmacy students made meaning of a clinical case differently in paper- and simulation-based workshops. Br J Educ Tech. 2010;42(5):1–10. [Google Scholar]
- 28.Hayton WL, Collins PL. STELLA: Simulation software for pharmokinetic software. Am J Pharm Educ. 1991;55:131–134. [Google Scholar]
- 29.Ramanathan M, Chau RI, Straubinger RM. Integration of Internet-based technologies as a learning tool in a pharmaceutical calulations course. Am J Pharm Educ. 1997;61(2):141–148. [Google Scholar]
- 30.Thompson JE. Development and use of an interactive database management system for simulated patient care experiences for pharmacy students. Am J Pharm Educ. 1994;58(3):324–332. [Google Scholar]
- 31.Chisholm MA, Dehoney J, Poirier S. Development and evaluation of a computer assisted instructional program in an advanced pharmacotherapeutics course. Am J Pharm Educ. 1996;60(4):365–369. [Google Scholar]
- 32.Triola M, Feldman H, Kalet AL, Zabar S, Kachur EK, Gillespie C, Anderson M, Griesser C, Lipkin M. A Randomized trial of teaching clinical skills using virtual and live standardized patients. J Gen Intern Med. 2006;21(5):424–429. doi: 10.1111/j.1525-1497.2006.00421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mestrovic A, Stanicic Z, Hadziabdic MO, Mucalo I, Bates I, Duggan C, Carter S, Bruno A. Evaluation of Croatian community pharmacists’ patient care competencies using the general level framework. Am J Pharm Educ. 2011;75(2):Article 36. doi: 10.5688/ajpe75236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.BC College & Institute Student outcomes. Understanding student satisfaction. Issue paper 2003;3:1-4. http://admin.selkirk.bc.ca/research/documents/issue_satisfaction%5B1%5D.pdf. Accessed March 24, 2012.
- 35.Stevens A, Hernandez J, Johnsen K, et al. The use of virtual patients to teach medical students history taking and communication skills. Am J Surg. 2006;191:806–811. doi: 10.1016/j.amjsurg.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 36.Deladisma AM, Johnsen K, Raij A, et al. Medical student satisfaction using a virtual patient system to learn history-taking communication skills. Stud Health Technol Inform. 2008;132:101–105. [PubMed] [Google Scholar]
- 37.Effken JA, Brewer BB, Patil A, Lamb GS, Verran JA, Carley K. Using OrgAhead, a computational modeling program, to improve patient care unit safety and quality outcomes. Int J Med Inform. 2005;74(7-8):605–613. doi: 10.1016/j.ijmedinf.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Sanders C, Kleinert HL, Boyd SE, Herren C, Theiss L, Mink J. Virtual patient instruction for dental students: can it improve dental care access for persons with special needs? Spec Care in Dentist. 2008;28(5):205–213. doi: 10.1111/j.1754-4505.2008.00038.x. [DOI] [PubMed] [Google Scholar]
- 39.Semeraro F, Frisoli A, Bergamasco M, Cerchiari EL. Virtual reality enhanced mannequin (VREM) that is well received by resuscitation experts. Resuscitation. 2009;80(4):489–492. doi: 10.1016/j.resuscitation.2008.12.016. [DOI] [PubMed] [Google Scholar]